Abstract
AIM
To evaluate the surgical outcome of congenital upper eyelid coloboma repair.
METHODS
All patients underwent complete ophthalmic and general examination before going to surgery, and then examination under anesthesia was performed to assess the site and size of eyelid defect, conjunctival involvement. The status of cornea and ocular motility with forced duction test was also being noted. The surgical procedure was performed according to the size of defect.
RESULTS
Out of 21 cases of congenital upper eyelid coloboma, 18 occurred in isolation with upper eyelid medial defect, 13 were bilateral and 5 were unilateral. Others were associated with Goldenhar syndrome and CHARGE syndrome with bilateral upper lid medial defects. All patients were presented for surgical corrections during age of 2.5-4.0 years except one that presented at 25 years of age. Cosmetically surgical results were acceptable, except one that was already presented with opaque corneal.
CONCLUSION
In this study, overall surgical results were satisfactory except one that was presented late with compromised cornea.
Keywords: coloboma, upperlid congenital, surgical outcome
INTRODUCTION
The word coloboma is Greek (Koloboma) meaning mutilated or curtailed and refers to a congenital malformation that occurs in about 1:10 000 births, in which ocular structures are incompletely formed due to failure of the embryonic optic fissure to fuse[1]. The resultant gap, notch or hole may involve different structures, including the eyelid, iris, lens, ciliary body, choroids, optic nerve or retina, causing mild to severe vision loss. The fronto nasal and maxillary processes of an embryo are formed at the 4th week of life and continue their structural differentiation until 8 to 9 weeks. Any form of disturbance that occurs during this embryological period (4 to 9 weeks) can affect the formation of normal eyelid[2]. Although the exact cause of congenital eyelid coloboma remains uncertain, several theories like it is a form of facial cleft[3], and intrauterine factors such as amniotic band, inflammation, decreased placental circulation, mechanical influences, or abnormal vascular system have been suggested to be factors involved in eyelid coloboma[3],[4].
A defect in the eyelid margin was first described in 1585 by Jacques Guillemeau[5]. Various systems for classification of eyelid colobomas have been described[6]-[8]. Jackson et al[6] reclassified the lid anomalies in 1988 as cryptophthalmos and eyelid colobomas. Eyelid colobomas are most commonly triangular in shape with the base at the eyelid margin. It is usually located on the medial half of the upper eyelid or laterals half of the lower eyelid and can vary in size form a small indentation of the eyelid to near absence of the entire eyelid. Eyelid coloboma is rare and commonly occurs as an isolated finding. However, they have been reported to occur as part of a multisystem syndrome. These include Goldenhar[9],[10]. Teacher-Collins[11], Delleman syndromes[12] and frontonasal dysplasia[13]. Other less common association include Fraser[14] and nasopalpebral lipoma coloboma syndromes[15], and a new un-named syndrome described by Balei et al[16] consisting of upper eyelid coloboma, hypertolorism, hypospadias and hearing loss.
The eyelid coloboma usually presents with exposure keratopathy due to poor Bell's phenomenon. So it requires immediate attention[2], otherwise the cornea inevitably ulcerates and the eye becomes blind[17],[18]. Management of these cases involves providing corneal protection, surgical repair of the eyelid defect and any associated ocular and systemic anomalies, and monitoring visual development[2].
MATERIALS AND METHODS
Subjects
Twenty-one patients for this study were selected from outpatient department of Ophthalmology, Liaquat University of Medical & Health Sciences Eye Hospital, Hyderabad from October 2008 to June 2009. Only patients of age ranged from one year to 25 years with upper eyelid coloboma were included in the study. Patients older than 25 years of age and with lower eyelid coloboma were excluded from the study. All patients underwent complete ophthalmic and general medical examination before going to surgery and all data were recorded on a printed profroma. At the time of initial visit all mothers were interviewed regarding the term of delivery, their exposure to drugs and infections diseases during pregnancy and the heritance of the coloboma. Then all patients were referred to pediatric specialist for general medical examination to exclude the systemic disease. During general ophthalmic examination position of eye ball, Bell's phenomenon and any facial deformity were also noted. All patients then went examination under anaesthesia (EUA) to assess the site and size of the eyelid defect, conjunctival involvement, status of the cornea and ocular motility with forced duction tests was also noted. Before repairing eyelid coloboma, the horizontal defects were measured by gently pulling the edges of the eyelid defects. Then the vertical defects were measured from the lash line to the apex of the defect, as one fourth's, one third's, half's or more then half's the eyelid size.
Surgical Procedure
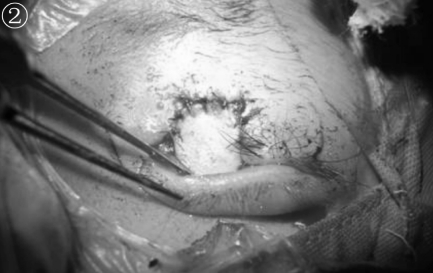
All surgeries were performed by a single surgeon. The defects one fourth's or upto one third's the eyelid were repaired by direct closure (Figure 1). The edges of the defects were refreshed with sharp incisions and precise anastomosis was performed by bringing lid margins together and by using two layer approximations of the tarsus and skin. Then lateral canthotomy or cantholysis was carried out to minimize the horizontal tension of the lid. The defect more than one third's or upto half's the eyelid were repaired with Cutler Beard procedure (Figures 2, 3). In this procedure a full thickness lower eyelid flap was advanced into the defect of upper eyelid by passing it behind the remaining lower eyelid margin.
Figure 1. Direct closure of bilateral upper lid medial two thirds full thickness coloboma.
Figure 2. Cutler beard procedure.
Figure 3. Cutler beard procedure,CHARGE syndrome.
RESULTS
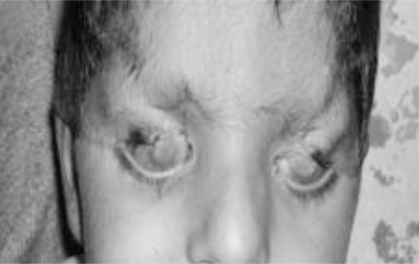
In this study, 16 patients were male and 5 were female. There was no history of immature birth of any case. Age of patients ranged from 2.5 to 4.0 years (median 3 years), only one patient had late presentation that was 25 years of age (Figure 4). Out of 21 cases 13 presented with bilateral upper lid medial defect as isolated coloboma (Figures 5, 6). Five cases presented with left upper lid medial defect as isolated coloboma. Three cases presented with systemic association. Out of three one patient had the problem of exposure keratopathy (Figure 7) and poor Bell's phenomenon with bilateral upper lid medial defect. Systemic association of one case was Goldenhar syndrome with unilateral upper lid medial defect and of another was CHARGE syndrome (Figure 8) with bilateral upper lid medial defect symblepheron was found in two cases that have systemic association. Cosmetically overall surgical results (Table 1) were acceptable with good eyelid closure and there was no exposure keratopathy, except one case that was already partially opaque when referred to us.
Figure 4. Direct closure of left upper lid less than medial one fourth full thickness coloboma.
Figure 5. Direct closure of bilateral upper lid medial one fourth full thickness coloboma.
Figure 6. Bilateral upper lid medial two thirds full thickness coloboma.
Figure 7. Bilateral upper lid medial one third full thickness coloboma.
Figure 8. CHARGE syndrome, bilateral upper lid medial two third thickness coloboma.
Table 1. Clinical data of patients & surgical procedure.
| N | Sex | Age(yr) | Occular features | Systemic features | Surgical procedure |
| 1 | M | 3.0 | • Bilateral upper lid medial one third's full thickness coloboma | • Depigmented skin around the mouth | • Direct closure of lid with canthotomy and cantholysis |
| • Poorly formed eye brows. | • Vertical Hairy growth | • Symplepherectomy | |||
| • Bilateral superior symblepheron | |||||
| • Poor Bell's phenomenon | |||||
| • Bilateral corneal opacities | |||||
| 6 | M | 3.5 | • Bilateral upper lid medial one forth's full thickness coloboma | - | • Direct closure of lid |
| 3 | F | 3.0 | • Bilateral upper lid medial one forth's full thickness coloboma | • Direct closure of lid | |
| 1 | F | 2.5 | • Left upper lid less than medial full thickness coloboma | • Goldenhar Syndrome Left hemifacial atrophy. Left cleft upper lip. and palate | • Direct closure of lid |
| • Repair of cleft lip & papate. By general plastic surgery | |||||
| 4 | M | 4.0 | • Bilateral upper lid medial two third's full thickness coloboma | • Direct closure of lid with cantholysis | |
| 1 | M | 3.0 | • Bilateral upper lid medial two third's full thickness coloboma with sympblepheron | • CHARGE syndrome | • Culter Beared rocedure Symplepheronectomy |
| 4 | M | 4.0 | • Left upper lid less than medial one forth's full thickness coloboma | • Direct closure of lid | |
| 1 | F | 25 | • Left upper lid less than medial one forth's full thickness coloboma | • Direct closure of lid |
DISCUSSION
Eyelid colobomas are, rare and occur as an isolated finding[19]. However they have been reported to occur as a part of multiple ocular and systemic anomalies[2],[9]-[16],[20]. In our series only two patients have systemic anomalies of Goldenhar and CHARGE syndrome. None of patients had iris coloboma, cataract, glaucoma, strabismus, retinal coloboma or iris atrophy. Corneal protection and cosmesis are common indications for repairing the eyelid defects and its treatment depend on the size of defect[12]. The corneal tolerance to exposure is excellent in young children because they have a good Bell's phenomenon[2], hence corneal protection can usually be achieved with addition of lubricants. Therefore, it may often be safe to delay the repairing of the small defect till the eyelid tissue available for reconstruction[14]. In our study, all patients referred for repairing the lid defects after 2.5 to 4.0 and 25 years of age. However early surgical intervention may be necessary in patients with large defect or poor Bell's phenomenon[2],[21].
Most of the surgeons like to repair with direct closure[2], Tenzel procedure[15] and Cutler Beard's procedure[16], the defects of one fourth's, one third's and upto half's the eyelid respectively. In present study most of the patients of coloboma pretended with size of one fourth to one third eyelid and all were repaired with direct closure followed by canthotomy or cantholysis. Only one case of more than one thirds the eye lid was treated with cutler Beard's procedure. In our study the overall results of direct closure with canthotomy or cantholysis were satisfactory cosmetically except one case that presented late with compromised cornea. The result of cutler Beard procedure was acceptable and this eyelid sharing procedure involves occlusion of the eye for a long duration. This occlusion during critical period of visual development has been reported potentially amblyogenic[17]. But we did not found such problem after sharing procedure. If the congenital upper eyelid coloboma is not treated at the critical time period, it may lead to great threat to vision even blindness due to exposure keratopathy and it may also be a blemish later in life. So the surgical intervention should be performed as soon as possible with guarded prognosis because the amblyopia may be the pit fall as results of eyelid sharing procedure.
REFERENCES
- 1.Pagon RA. Ocular coloboma. Surv Ophthalmol. 1981;25(4):223–236. doi: 10.1016/0039-6257(81)90092-8. [DOI] [PubMed] [Google Scholar]
- 2.Seath LL, Choo CT, Fong KS. Congenital upper lid colobomas management and visual outcome. Ophthal Plast Reconstr Surg. 2002;18(3):190–195. doi: 10.1097/00002341-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Tessier P. Symposium on Plastic Surgery in the Orbital Region. St. Louis: CV Mosby; 1980. Anatomical classification of facial, cranoi-facial and latero facial clefts. [Google Scholar]
- 4.Roper Hall MJ. Proceedings of the Second International Symposium in Plastic and Reconstructive Surgery of the Eye and Adnexa. St. Louis: CV Mosby; 1967. Congenital coloboma of the lids; pp. 316–321. [Google Scholar]
- 5.Duke-Elder S, Cook C. Normal and abnormal development. In: Duke-Elder S, editor. System of Ophthalmology. Vol. 14. St. Louis: C.V. Mosby Co; 1963. pp. 313–317. [Google Scholar]
- 6.Jackson IT, Shaw KE, del Pinal Matorras F. A new feature of the ablepharon macrostomia syndrome: zygomatic arch absence. Br J Plast Surg. 1988;41(4):410–416. doi: 10.1016/0007-1226(88)90084-7. [DOI] [PubMed] [Google Scholar]
- 7.Collin JRO. Congenital upper lid coloboma. Aust N Z J Ophthalmol. 1986;14(4):313–317. doi: 10.1111/j.1442-9071.1986.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 8.Mustarde JC. Ophthalmic Plastic and Reconstructive Surgery. Vol. 2. St. Louis: C. V. Mosby Co; 1987. Congenital soft tissue deformities; p. 1238. [Google Scholar]
- 9.Gorlin RJ, Jue K L, Jacobson U, Gold Schmidt E. Oculoauriculovertebral dysplasia. J Pediatr. 1963;63:991–999. doi: 10.1016/s0022-3476(63)80233-4. [DOI] [PubMed] [Google Scholar]
- 10.Sugar HS. The oculoauriculovertebral dysplasia syndrome of Goldenhar. Am J Ophthalmol. 1966;62:678–682. doi: 10.1016/0002-9394(66)92193-3. [DOI] [PubMed] [Google Scholar]
- 11.Coulon MR, Satala FC. Congenital eyelid anomalies. In: Albert DM, Jakobeic FA, editors. Principles and Practice of Ophthalmology: Clinical Practice. Philadlphia, Pa: WB Sauders Co; 1994. pp. 1693–1702. [Google Scholar]
- 12.Delleman JW, Oothuys JWE. Orbital cyst in addition to congenital cerebral and focal derma malformations: a new entity? Clin Genet. 1981;19(3):191–198. doi: 10.1111/j.1399-0004.1981.tb00695.x. [DOI] [PubMed] [Google Scholar]
- 13.Sedano HO, Cohen MM, Jr, Jirsek J, Jirasek J. Frontonasal dysplasia. J Pediatr. 1970;76(6):906–913. doi: 10.1016/s0022-3476(70)80374-2. [DOI] [PubMed] [Google Scholar]
- 14.Thomas IT, Frias JL, Felix V, Sanchez de Leon L, Hernandez RA, Jones MC. Isolated and syndromic cryptophthalmos. Am J Md Genet. 1986;25(1):85–98. doi: 10.1002/ajmg.1320250111. [DOI] [PubMed] [Google Scholar]
- 15.Bock-Kunz Al, Lyan DB, Singhal UK. Nasopalpebral lipoma-coloboma syndrome. Arch Ophthalmol. 2000;118(12):1699–1700. [PubMed] [Google Scholar]
- 16.Balci S, Kayik Cioglu A, Dagli AS. Two brothers with hypospadias, hypertelorism, upper lid coloboma and mixed type hearing loss: a new syndrome. Clin Genet. 1998;54(5):440–442. doi: 10.1111/j.1399-0004.1998.tb03761.x. [DOI] [PubMed] [Google Scholar]
- 17.Rougier Y, Tessier P, Hervouet F, Woillez M, Lekieffre M, Derome P. Paris: Masson; 1977. Chirurgie plastique orbito-palpebrale. [PubMed] [Google Scholar]
- 18.Duke Elder. Part 1. Vol. III. London: Kimpton; 1966. System of Ophthalmology; pp. 231–-4, 298-300; Vol III, part 2 835-840, 878. [Google Scholar]
- 19.Adegbehingbe BO, Olabanji, Adeoye AO. Isolated bilateral upper lid coloboma: a case report. Niger J Med. 2005;14(2):224–226. doi: 10.4314/njm.v14i2.37186. [DOI] [PubMed] [Google Scholar]
- 20.Wu-Chen WY, Christiasen SP, Berry SA, Engel WK, Fray KJ, Summers CG. Ophthalmic manifestations of Wolf- Hirschhorn syndrome. J AA POS. 2004;8(4):345–348. doi: 10.1016/j.jaapos.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Hoyama E, Lmawararut V, Malhotra R, Muecke J, Selva D. Tarsomarginal grafth in upper eyelid coloboma repair. J AAPOS. 2007;11(5):499–501. doi: 10.1016/j.jaapos.2007.04.011. [DOI] [PubMed] [Google Scholar]