Abstract
AIM
To report the study on radiofrequency ablation technique for eradication of palpebral margin neoplasm and its clinical effects.
METHODS
One hundred and six cases with the palpebral margin neoplasm were performed surgical removal with radiofrequency ablation technique. The 1-2 months postoperative follow-up was investigated and the lost cases were excluded from statistics. The continuing follow-up lasted about 6-16months.
RESULTS
One hundred cases underwent one treatment and 6 cases underwent two treatments. Six cases were missed. All the cases followed up healed well without pigmentation or scar left, nor eyelash loss or palpebral margin deformation. No case was recurrent.
CONCLUSION
Radiofrequency ablation has significant efficiency in eradicating the palpebral margin neoplasm.
Keywords: radiofrequency ablation, palpebral margin neoplasm
INTRODUCTION
People who were troubled by the palpebral margin neoplasm for its poor appearance on the face have been always looking for a suitable procedure to ablate it. Commonly it was removed by the general surgery. However, because of its location, the palpebral margin, the general surgery usually had to face some risks and difficulties, such as postoperative palpebral margin defect or deformation. The radiofrequency ablation technique was widely used in the minimal invasive procedure. For example, it was used to eradicate supraventricular arrhythmia in heart diseases, and to ablate renal tumors, protrusion of intervertebral disc, prostatic hyperplasia and tumors. It had many advantages in excising the pathological tissues, such as high precision, easily isolating the tissues, and rapidly forming a covering layer on the surface of the wound after the procedure. With the electrode improved, radiofrequency ablation technique can be used to eradicate the palpebral margin neoplasm. It could get the high precision in the micrographically controlled excision. Having been successfully used to eradicate 106 cases with the palpebral margin neoplasm, the radiofrequency ablation technique has been proved to be an effective new therapeutic method.
MATERIALS AND METHODS
Subjects
There were 106 cases with the palpebral margin neoplasm aged 18-89 years, including 43 males and 63 females. The average age was (45.2±17.5) years. Their neoplasm included the following 8 kinds of diseases: 5 cases with cysts of sebaceous gland, 2 cases with papilloma, 15 cases with fibroma, 3 cases with angioma, 35 cases with verruca, 8 cases with seborrheic keratosis, 29 cases with pigmented nevus and 9 others. The others involved postoperative residues of hordeolum, palpebral margin nevus residues, postoperative residues of papilloma, and epiblepharon. Generally, the neoplasm was classified into 5 types by the size, which were: very small, ≤1mm; small, ≤2mm; middle, ≤=3mm; large, ≤4mm; very large, >4mm. The visual fields of 22 patients were affected by the neoplasm. The course of the diseases lasted about 0.5-600 months. The average was 113.4±145.5 months.
Methods
To start the surgery, first the skin was carefully disinfected with 20g/L lodophor solution, and then was carried out topical anesthesia with 50g/L lidocaine. The operator wore the magnifier and then precisely directed the electrode of the radiofrequency ablation apparatus at the palpebral margin neoplasm. The neoplasm was eradicated from the center to the edge with the separating layers and point-removed methods until palpebral margin was reached. During the procedure, it was observed if there were leftovers. It was also checked whether the palpebral margin was smooth or not. Usually the wound surface should be coagulated at the same time. The procedure would last 10-20 minutes. After the surgery, the patients were reminded to keep the wound surface clean until the scab fell off and the wound naturally healed up. The postoperative follow-up of 1-2 months was made and the residues were removed if available. If the second surgery was performed, the continuing follow-up would be carried out for 6-16months until the therapeutic effect was stable. The outcomes fell into 4 categories: 1) Failed: the neoplasm was almost unchanged; 2) Effective: 2/3 of the neoplasm disappeared; the residue was less than 1/3 or patients had recurrence in 6 months; 3) Marked improvement: the neoplasm disappeared with a defect<1mm on the palpebral margin; 4) Recovered: the neoplasm completely disappeared with the normal palpebral margin; No visible scars were left; no recurrence happened in 6 months after the surgery.
RESULTS
Among 106 cases, a total of 100 cases underwent one treatment (5 missed, 91 recovered, 1 had marked improvement, 3 effective), while 6 cases underwent the second treatment with 1 missed and 5 recovered. With the radiofrequency ablation technique, the wound surface had no pain and formed the scabs on the second day after the surgery which usually fell off in 7 days before it healed. No case was involved with infection. During the postoperative follow-up of 6-16months, no case showed the tendency of malignant transformation. All the cases followed were healed up well to the recovery level. That is, no recurrence, smooth palpebral margin without any deformation or visible scars, no ingrowing or damaged eyelashes, no madarosis, no corneal epithelium damaged, and no pigmentation. There were very few side effects.
Typical Cases
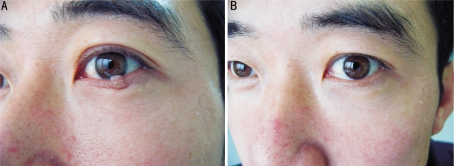
Case 1: Verruca on the left lower palpebral margin
A 32-year-old man presented with a verruca on the left lower palpebral margin, size: 4mm×6mm (Figure 1A). At one month after the first operation, the verruca on the left lower palpebral margin was completely eradicated (Figure 1B). The patient kept intact palpebral structure and had no eyelash loss. The 8-month postoperative follow-up showed that the curative effect was stable.
Figure 1. Verruca on the left lower palpebral margin.
A: before the operation, the size of verruca was 4mm×6mm; B: one month after the operation, verruca was completely removed
Case 2: Pigmented nevus on the left upper palpebral margin
A 36-year-old woman presented with pigmented nevus on the left upper palpebral margin, size: 6mm×3mm (Figure 2A). After the first operation, the pigmented nevus on the left upper palpebral margin was completely eradicated (Figure 2B). The patient kept intact palpebral structure and had no eyelash loss. The 8-month postoperative follow-up showed that the curative effect was stable.
Figure 2. Pigmented nevus on the left upper palpebral margin.
A: before the operation, the size of nevus was 6mm×3mm; B: eight months after the operation, nevus was completely removed
DISCUSSION
Palpebral margin, an arc-shaped structure on the eyelid, plays an important role in people's appearance. Any slight palpebral margin deficiency or deformation could affect the facial beauty. Therefore its requirements for the precision of the ablating technique are very strict. Palpebral margin is the transition area from the skin to the mucosa, where the neoplasm occurs more often. Traditionally palpebral margin neoplasm is removed by the general surgery[1], which usually brings lots of risks especially with a verdant practitioner, such as inappropriate stitching of wound, corneal reaction from the sutures, ingrowing eyelashes, deformation of the surgical scars and so on. All these could affect the facial cosmetology and cause lots of undesirable effects. So, it is urgent to find a safe and effective way to ablate the palpebral margin neoplasm. Radiofrequency ablation technique is an approach by which the electromagnetic wave is transmitted via electrode to vibrate the molecules of the contacted tissues, and thus tissues are coagulated. Only ablating the contacted tissues, it almost does no harm at all to those untouched tissues such as eyes. Because its ablating accuracy is easier to control, the potential surgical risks are significantly reduced. In addition, during the surgery procedure the practitioner does not need to wear protective spectacles, which makes the visual field clearer and the operation more convenient. As a result, its precision can be further enhanced. For some palpebral margin lesions operated under the surgery magnifier, the ablating precision could reach a very high level.
As for radiofrequency ablation technique, different methods could be employed or chosen according to the situations of the diseases. Radiofrequency ablation apparatus has two types of electrodes, the punctate shape and the plane shape, which are respectively for the lesion tissues of homologous shape[2],[3]. Thus the precision could be improved dramatically with the least damage to the nearby tissues such as eyelashes. For instance, the palpebral margin pigmented nevus could be eradicated by the punctate shaped electrode, the palpebral margin papilloma eradicated from the bottom through plane shaped electrode, the palpebral margin verrucae eradicated by separating the layers, and the palpebral margin sebaceous cyst eradicated from the wall or from the inside content. All these operations could help the treatments succeed to the greatest extent, which reduced the damage of the normal nearby tissues to the lowest level. Furthermore, none of wounds needed to be stitched up. Therefore it would make the operation much easier. Radiofrequency ablation technique had the least damage in eradicating the palpebral margin neoplasm.
The former research has discussed the efficiency of using high-power ultrapulse CO2 laser to remove the palpebral margin neoplasm. It showed that 2 cases fully recovered after the corneal injury had been treated and 10 cases had eyelash loss on the wound surface[4]. Other researches reported that using laser in palpebral plastic operation could increase the tendency of dried eye which usually happened at 1 week to 4 months after the surgery. Some even could cause exposed keratitis or hypophasis which required further surgical reconstruction[5]. Hammes[6] reported that using pulse-dye laser to remove the port wine nevus had caused motor impairment and supersensitive pain to the light of the pupil because of lacking the protection of the patients' eyes, which lasted for 12 months without relief. It was very important to wear the protective spectacles and keep a safety distance when using laser to operate around the orbital rim.
Nevertheless, reports about using radiofrequency in facial cosmetology generally focused on removing wrinkles with non-ablation technique to make the skin youthful[7]. Originally radiofrequency ablation technique was used for heart diseases to eradicate supraventricular arrhythmia[8], for renal tumors to ablate[9], and later for intervertebral disc protrusion[10], prostatic hypertrophy[11],[12] and tumors[13]-[17]. Now by the systematic research on radiofrequency ablation technique to eradicate the palpebral margin neoplasm, a series of effective treatment procedures have been established, which could precisely, separately and thoroughly eliminate the targets[2]. Radiofrequency ablation technique have many advantages, such as high precision, short operation time, no bleeding, less damage to other tissues, no eyelash loss or injured eyelash, rapid formation of postoperative protection layer, fast healing of wound surface, no visible scars, no pigmentation, disposable electrode, no cross infection, easier operation, no requirements of wearing protective spectacles for both the practitioner and the patient, no pain, and very slight inflammatory reaction after the surgery. It could meet different needs of the clinical work. In addition, not only can it help the patients regain their beauty, but also builds their self-confidence. Thus it is a very effective and valuable new therapeutic technique that should be recommended for application in the clinic.
REFERENCES
- 1.Zhao SY, Zhao GX. Surgery method and pathology analysis of palpebral margin pigmented nevus. Chin J Pract Ophthalmol. 2002;10:765–767. [Google Scholar]
- 2.Wang XL, He QH, Jiang TY, Suo W, Xiao HY. Successful eradication of palpebral margin neoplasms using XL-radiofrequency ablation skin apparatus. Int J Ophthalmol. 2008;8(11):2341–2343. [Google Scholar]
- 3.Wang XL, Suo W, Jiang TY, He QH, Xiao HY. Successful eradication of xanthelasma papebrarum using XL-radiofrequency ablation skin apparatus. Int J Ophthalmol. 2010;10(7):1383–1385. [Google Scholar]
- 4.Huang DP, Cai JH, Lu R, Huang YD. Ultrapulse CO2 laser used for the successful treatment of palpebral margin neoplasms. Chin J Pract Ophthalmol. 2007;25:660–663. [Google Scholar]
- 5.Korn BS, Kikkawa DO, Schanzlin DJ. Blepharoplasty in the post-laser in situ keratomileusis patient: preoperative considerations to avoid dry eye syndrome. Plast Reconstr Surg. 2007;119(7):2232–2239. doi: 10.1097/01.prs.0000260750.15059.17. [DOI] [PubMed] [Google Scholar]
- 6.Hammes S, Augustin A, Raulin C, Ockenfels HM, Fischer E. Pupil damage after periorbital laser treatment of a port-wine stain. Arch Dermatol. 2007;143(3):392–394. doi: 10.1001/archderm.143.3.392. [DOI] [PubMed] [Google Scholar]
- 7.Sadick NS, Alexiades-Armenakas M, Bitter P, Jr, Hruza G, Mulholland RS. Enhanced full-face skin rejuvenation using synchronous intense pulsed optical and conducted bipolar radiofrequency energy (ELOS): introducing selective radiophotothermolysis. J Drugs Dermatol. 2005;4(2):181–186. [PubMed] [Google Scholar]
- 8.Spector P, Reynolds MR, Calkins H, Sondhi M, Xu Y, Martin A, Williams CJ, Sledge I. Meta-analysis of ablation of atrial flutter and supraventricular tachycardia. Am J Cardiol. 2009;104(5):671–677. doi: 10.1016/j.amjcard.2009.04.040. [DOI] [PubMed] [Google Scholar]
- 9.Hui GC, Tuncali K, Tatli S, Morrison PR, Silverman SG. Comparison of percutaneous and surgical approaches to renal tumor ablation: metaanalysis of effectiveness and complication rates. J Vasc Interv Radiol. 2008;19(9):1311–1320. doi: 10.1016/j.jvir.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Chao SC, Lee HT, Kao TH, Yang MY, Tsuei YS, Shen CC, Tsou HK. Percutaneous pulsed radiofrequency in the treatment of cervical and lumbar radicular pain. Surg Neurol. 2008;70(1):59–65. doi: 10.1016/j.surneu.2007.05.046. [DOI] [PubMed] [Google Scholar]
- 11.Savoie PH, Lopez L, Simonin O, Loubat M, Bladou F, Serment G, Karsenty G. Two-years follow-up of radiofrequency thermotherapy for urination disorders due to benign prostatic hyperplasia. Prog Urol. 2009;19(7):501–506. doi: 10.1016/j.purol.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Le Gal S, Fouques Y, Mallick S, Taksin L, Le Toquin-Bernard S, Frachet O, Bensadoun H. Treatment of benign prostatic hyperplasia by radiofrequency (TUNA): a monocentric study of 28 cases treated in ambulatory surgery. Prog Urol. 2009;19(5):327–332. doi: 10.1016/j.purol.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Abbas G, Pennathur A, Landreneau RJ, Luketich JD. Radiofrequency and microwave ablation of lung tumors. J Surg Oncol. 2009;100(8):645–650. doi: 10.1002/jso.21334. [DOI] [PubMed] [Google Scholar]
- 14.Raman JD, Hall DW, Cadeddu JA. Renal ablative therapy: radiofrequency ablation and cryoablation. J Surg Oncol. 2009;100(8):639–644. doi: 10.1002/jso.21194. [DOI] [PubMed] [Google Scholar]
- 15.Maithel SK, Fong Y. Hepatic ablation for neuroendocrine tumor metastases. J Surg Oncol. 2009;100(8):635–638. doi: 10.1002/jso.21196. [DOI] [PubMed] [Google Scholar]
- 16.Van Vilsteren FG, Bergman JJ. Endoscopic therapy using radiofrequency ablation for esophageal dysplasia and carcinoma in Barrett's esophagus. Gastrointest Endosc Clin N Am. 2010;20(1):55–74. doi: 10.1016/j.giec.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Volkmer D, Sichlau M, Rapp TB. The use of radiofrequency ablation in the treatment of musculoskeletal tumors. J Am Acad Orthop Surg. 2009;17(12):737–743. doi: 10.5435/00124635-200912000-00002. [DOI] [PubMed] [Google Scholar]