Dir Sir,
I am doctor Guo-Yuan Yang, from the Department of Ophthalmology of West China Hospital of Sichuan University in Chengdu, Sichuan Province, China. I write to present a case report of posterior lentiglobus with cataract.
Posterior lentiglobus is a rare abnormality in the shape of the crystalline lens, characterized by a progressive spheroidal protuberance affecting the posterior lens surface. It could cause lens opacity gradually. But the weakness of the posterior capsule wall makes the surgery challenging, especially for those who has large area of capsule bulging. So we reported a case, in which the area of capsule bulging was about 6 mm in diameter, successfully treated by the technique of posterior continuous curvilinear capsulorhexis(PCCC). Transmission electron microscopy examinations (TEM) of the posterior capsule also were conducted.
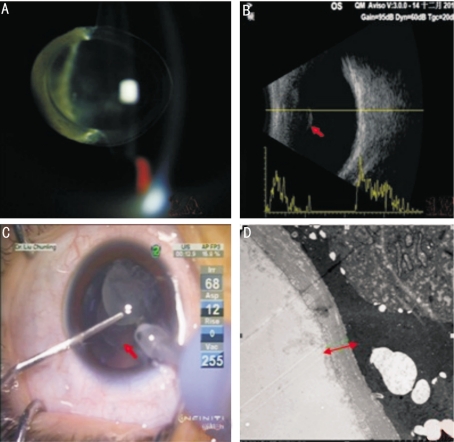
A 5-year-old boy was referred to our department for evaluation of his squint and decreased visual acuity (VA) in the left eye. The parents noticed his decreased vision since 6 months after birth and secondary exotropia around the age of 3 years. The boy was normal full-term delivery, breast feeding. His mother had no history of radiation exposure in her pregnant period. There was no family history of cataract or any other systemic illness. On examination, his visual acuity was 20/20 in the right eye and only light perception in the left eye. Hirschberg test revealed an exotropia of 15°. Slit-lamp examination showed hemispherical protrusion of the posterior lens surface with a totally opacity in the central region of the lens in the left eye (Figure 1A). The posterior capsule was opaque, too. Dilated fundoscopy of the left eye was not accessible because of the totally opacity of the lens. Intraocular pressure (IOP) was 11.8mmHg and 14.9mmHg respectively in the right and left eye. As the little boy was too young, A-scan ultrasonography was impossible under surface anesthesia. B-scan examination showed the protrusion of the posterior lens in the left eye (Figure 1B). Some ophthalmic biological parameters were obtained by B-scan and IOL master (Carl Zeiss V.5.4, Germany). Keratometry value was 42.35 D and 43.32 D in the right eye, and 40.37 D and 42.99 D in the left. Axial length of the right eye was 22.38 mm and in the left eye it was 22.10mm. Lens thickness was 4.1mm in the right and 4.77mm in the left. Extraction cataract extracapsularis(ECCE),intraocular lens (IOL) implantation and anterior vitrectomy were performed under general anesthesia. With a clear corneal incision, the anterior chamber was filled with viscoelastics (Alcon, USA). An anterior continuous curvilinear capsulorhexis(ACCC) was made. The hemispherical protrusion of the posterior capsule was separated by blunt dissection technique. The intracapsular material aspiration was performed. A posterior continuous curvilinear capsulorhexis(PCCC) 6 mm in diameter and anterior vitrectomy were performed, followed by in-the-bag implantation of a +23.00D ADAPT--AO IOL (BAUSCH&LOMB, USA). That's because the axial lenth of aphakic eye grows faster than normal following infantile IOL surgery, so for 5-year-old child ,at least +2D refraction should be given rather than that towards 0D postoperatively. At the time of lens aspiration, the bulging posterior capsule confirmed the diagnosis of lentiglobus(Figure 1C). The area of capsule bulging was about 6 mm in diameter. Simultaneously, capsular flutter was noted. The capsulorhexis fragment was fixed in 3% buffered glutaraldehyde and embedded with Epon812. Then ultrathin sections stained with uranyl acetate and lead citrate were examined under electron microscope at 80 kV(Hitachi TEM system, Japan). But no typical thinned basal lamina with basement membrane disruption and unusual nodular structure was found. The thickness of the thinnest part in posterior capsule is about 1.83um in diameter (Figure 1D). Synthesis training for form vision deprivation amblyopia was prescribed postoperatively. Six months later, the visual acuity was improved to 20/100 in the left eye. No complications were observed.
Figure 1. The clinical manifestation and auxiliary examination results of the patient.
A: The posterior lentiglobus photograph of the left eye. The slit beam on the posterior lens surface is more curved than usual; B: B-scan examination showed the protrusion of the posterior lens in the left eye(arrow); C: Intraoperative photograph of the left eye. The bulging posterior capsule is showed (arrow); D: Transmission electron microscopy of the posterior lens capsule. The thinnest diameter is approximately 1.83 um (arrow).
Posterior lentiglobus is an uncommon abnormality, characterized by a progressive spheroidal protuberance. Some papers refer to this anomaly as “lenticonus”. But we think the term lentiglobus is anatomically more accurate because the bulging is spherical and not conical. The prevalence is about 1 in 100 000 people[1]. The disease may be unilateral or bilateral. It can present as the only ocular anomaly or association with persistent fetal vasculature stalk[2], morning glory syndrome[3] and Alport syndrome[4]. Bilateral posterior lentiglobus may be inherited in an X-linked[5] or an autosomal dominant fashion[6]. Its etiology remains obscure and mysterious even today. It may involve subepithelial capsular hyperplasia, embryologic hyaloid artery traction, inherent weakness of the posterior capsule wall, and excessive strain during accommodation, resulting in posterior herniation of the lens. Kim et al[7] suggested that the mean age at presentation of posterior lenticonus was about 39.0+/-37.4 months. Travi et al[8] reported that conservative treatment of amblyopia in unilateral small posterior lens opacities and lenticonus initially can be successful. But Wilson and Trivedi[9] thought that a delayed diagnosis and surgical treatment of posterior lentiglobus may result in dense amblyopia from form vision deprivation, which may be resistant to occlusion therapy after surgery. A fragile, floppy capsule makes cataract surgery challenging. During the surgery, hydrodissection is contraindicated. Fluctuations in the IOP and turbulence of the fluid in the anterior chamber can threaten the capsular bag stability. Praveen et al[10] reported one case with intraoperative posterior capsule flutter in posterior lentiglobus. We also had the same experience intraoperatively. So a low flow rate and low bottle height is dedicated to avoid of uncontrolled peripheral extension of the posterior capsule defect. In our case, the opacification of the bulging posterior capsule was very severe. So removal of the bulging posterior capsule can also be helpful to the treatment of amblyopia postoperatively. But we think that even the bulging posterior capsule is not opaque, it is necessary to perform posterior capsulorhexis. Posterior capsule opacification (PCO) is rapid and virtually inevitable in such young patients with floppy, outstretched capsule. Primary capsulotomy and anterior vitrectomy can reduce the risk of PCO[11]. The technique of posterior curvilinear continuous capsulorrhexis (PCCC) can also be helpful in converting preexisting posterior capsule rupture to a desired size. Transmission electron microscopy of the posterior lens capsule revealed the thickness of the thinnest part is only 1.83 um. Murakami et al[12] reported one case in which the thinnest diameter was approximately 2.3 um. The thinner diameter in our case may have relation to greater intralenticular pressure due to large area of protuberance. But we did not find typical thinned basal lamina with basement membrane disruptions and unusual nodular structures, as has been described previously[12]-[13]. Maybe the thinning posterior lens capsule in the central part comes from the pressure of bulging lens and inherent weakness of the posterior capsule wall.
Footnotes
There is no conflict of interest.
REFERENCES
- 1.Cheng KP, Hiles DA, Biglan AW, Pettapiece MC. Management of posterior lenticonus. J Pediatr Ophthalmol Strabismus. 1991;28(3):143–149. doi: 10.3928/0191-3913-19910501-07. [DOI] [PubMed] [Google Scholar]
- 2.Abdel-Hafez G, Wilson ME, Trivedi RH. Progression of a unilateral posterior lentiglobus associated with a persistent fetal vasculature stalk. JAAPOS. 2010;14(1):81–82. doi: 10.1016/j.jaapos.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Xiao-Guang Cao, Xiao-Xin Li, Yong-Zhen Bao. Morning Glory Syndrome Associated with Posterior Lenticonus. Open Neurol J. 2009;3:45–47. doi: 10.2174/1874205X00903010045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Mahmood AM, Al-Swailem SA, Al-Khalaf A, Al-Binali GY. Progressive posterior lenticonus in a patient with alport syndrome. Middle East Afr J Ophthalmol. 2010;17(4):379–381. doi: 10.4103/0974-9233.71591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vivian AJ, Lloyd C, Russell-Eggitt I, Taylor D. Familial posterior lenticonus. Eye (Lond) 1995;9(Pt 1):119–123. doi: 10.1038/eye.1995.19. [DOI] [PubMed] [Google Scholar]
- 6.Schipper I, Senn P, Schmid M. Diagnosis and management of bilateral posterior lenticonus in 7 members of the same family. J Cataract Refract Surg. 2006;32(2):261–263. doi: 10.1016/j.jcrs.2005.07.046. [DOI] [PubMed] [Google Scholar]
- 7.Kim MJ, Kim JH, Yu YS. The Surgical Management of Posterior Lenticonus Associated with Pediatric Cataract. J Korean Ophthalmol Soc. 2007;48(5):649–654. [Google Scholar]
- 8.Travi GM, Schnall BM, Lehman SS, Kelly CJ, Hug D, Hirakata VN, et al. Visual outcome and success of amblyopia treatment in unilateral small posterior lens opacities and lenticonus initially treated nonsurgically. JAAPOS. 2005;9(5):449–454. doi: 10.1016/j.jaapos.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Wilson ME, Trivedi RH. Intraocular lens implantation in pediatric eyes with posterior lentigloubus. Trans Am Ophthalmol Soc. 2006;104:176–182. [PMC free article] [PubMed] [Google Scholar]
- 10.Praveen MR, Vasavada AR, Koul A, Ravat FA, Trivedi RH, Shah SK, et al. et al. Intraoperative posterior capsule flutter in posterior lentiglobus. JAAPOS. 2010;14(4):367–368. doi: 10.1016/j.jaapos.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Lloyd IC, Ashworth J, Biswas S, Abadi RV. Advances in the management of congenital and infantile cataract. Eye (Lond) 2007;21(10):1301–1309. doi: 10.1038/sj.eye.6702845. [DOI] [PubMed] [Google Scholar]
- 12.Murakami Y, Kusaka S, Hayashi N, Soqa K, Fujikado T. Wavefront analysis and ultrastructural findings in an eye with posterior lentiglobus. JAAPOS. 2010;14(6):530–531. doi: 10.1016/j.jaapos.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Junk AK, Stefani FH, Ludwig K. Bilateral anterior lenticonus: Scheimpflug imaging system documentation and ultrastructural confirmation of Alport syndrome in the lens capsule. Arch Ophthalmol. 2000;118(7):895–897. [PubMed] [Google Scholar]