Abstract
Endogenous aspergillus endophthalmitis(EAE) after kidney transplant is a rare but important clinical problem due to potentially devastating consequences. Early diagnosis of EAE, timely removal of affected vitreous by vitrectomy, proper anti-fungal treatment, all contributed to the successful control of the disease. Therapeutic success of EAE in post-transplant patients depends largely on prompt diagnosis. Definite diagnosis of EAE is based on positive culture results of vitreous specimen, while fundoscopy and B scan ultrasound may aid early diagnosis. In terms of anti-fungal medicine, amphotericin B has long been the first choice, but its systemic applicaiton has severe adverse reactions, especially for patients with impaired renal function. Herein, we report the treatment modality of EAE after kidney transplant with vitrectomy, systemic administration of micafungin plus voriconazole, topical application of fluconazol and amphotercin B.
Keywords: aspergillus, endophthalmitis, kidney transplan-tation, amphotercin B, micafungin
INTRODUCTION
Endogenous aspergillus endophthalmitis(EAE) is a rare complication in kidney transplantation patients. Relatively speaking, the prognosis of aspergillus endophthalmitis is poor due to extensive retinal necrosis and choroidal damage[1]. The outcome of aspergillus endophthalmitis (AE) in renal transplant patients was poor with 70%-100% mortality[2]. In an electronic Medline review, we found only four papers on AE in renal transplant patients between 1975 and August 2011[2]-[4]. Since EAE has potentially devastating outcomes and limited therapeutic options, it makes great sense to study its diagnosis and treatment.
TYPICAL CASE
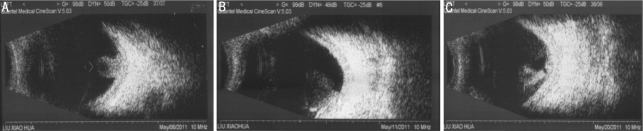
A 38-year-old female underwent left kidney transplant because of chronic renal failure (uremia) and received intense immuno-suppressionn with oral methylprednisolone, tacrolimus, mizoribine. Forty-eight days after transplant, she presented with left eye redness and blurred vision. Ocular examination revealed visual acuity of 0.5(6/12) in the left eye (1.2(6/5) in the right). On slit lamp examination, there was mixed hyperemia in the conjunctiva, with keratic precipitates (KP) on the cornea, Tyndall (+) and opaque vitreous. Applanation intraocular pressure was 17mmHg. Fundus examination revealed a pale optic disc and a ball-shaped object in the vitreous adjacent to retina. Examination of right eye showed normal findings. She was diagnosed as panuveitis in the left eye and given topical corticosteroids and pranopulin. Additionally, two days later, massive pigmented particles in vitreous were noted. Fundus examination showed white punctate infiltrates at posterior pole. The patient was given Prednisone (60mg) in the morning. Considering the development of the disease and neutrophilia (0.931), provisional diagnosis was changed to endogenous fungal endophthalmitis and she was treated with voriconazole (0.2g iv, and gutt, bid), oral fluconazol(150mg, qid), topical fluconazol, clotrimazole and pranopulin. We used serial B scan ultrasound to monitor the condition, which revealed worsening of the vitreous reaction (Figure 1A, B and C).
Figure 1. Bscan ultrasonogram.
A:(on the day of first eye check-up) pre-retinal echogenic mass with high reflectivity in vitreous cavity; B:(53 days post transplant) worsening vitreous reaction; C: (before vitrectomy) intensive punctate vitreous opacities, with notable enlargement of the mass
Sixty-two(62) days after transplant, the condition became worse, conservative therapy had no obvious effect, necessitating vitrectomy. Preoperatively, visual acuity decreased to light perception (LP). On slit-lamp examination, there were more KP (++), Tyndall (+++), fibrinous exudates in anterior chamber, slight opacity of posterior lens capsule and yellowish-white mass inside vitreous cavity. She underwent left lensectomy, pars plana vitrectomy, laser endophotocoagulation, air-fluid exchange and silicone oil injection. Intra-operatively, it was noted that greyish-white cotton-wool opacity formed in vitreous cavity, beaded hyphae grew around optic disc, macular area was greyish-yellow and edematous, massive greyish-white lesion formed in the inferior retina, with superficial retinal detachment in the lower periphery. After removing the lesion, we could see greyish-white cheese-like necrosis focal of inferior retina and choroid, surrounding which were scattered greyish-white satellite lesions.
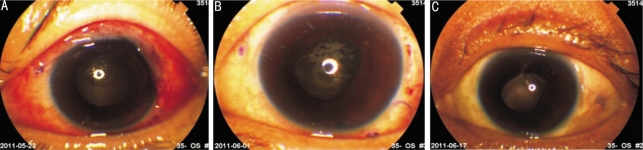
Microscopic examination and culture of vitreous fluid extracted during the surgery showed presence of aspergillus . The final diagnosis was endogenous fungal (aspergillus) endophthalmitis. Patient was then given micafungin(50mg, iv, and gutt, qd for 2days 100mg/d, iv, and gutt, qd for 3 weeks), topical fluconazol, clotrimazole, amphotercin B and diclofenac sodium (each drug 4 times per day). 1-2 days postoperatively with the above treatment, KP, Tyndall and vitreous haemorrhage showed signs of reduction. On 3rd postoperative day, fibrinous exudates were noted in the anterior chamber (Figure 2A) and covered the entire pupil region on the 7th day. From 12th day onwards, the exudates were noted to be gradually absorbing (Figure 2B) and basically disappeared on the 19th day. Pupil became irregular and fixed with posterior synechia of the iris (Figure 2C).
Figure 2. Anterior segment-post vitrectomy.
A: 3rd day, exudative membrane in the pupil region;B: 12th day, fibrinous exudates like a fishing net, with slight absorption in superior pupil region;C: 19th day, irregular pupil with posterior synechiae
RESULTS
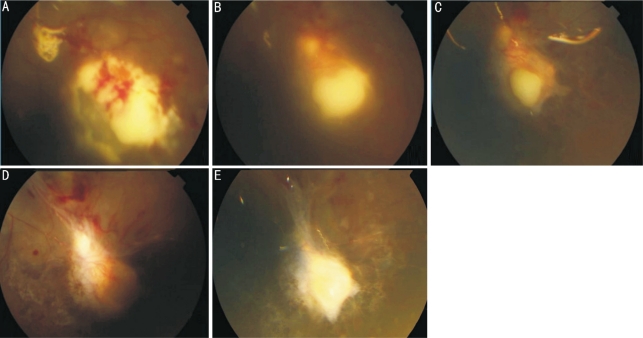
Patient was discharged on 21st postoperative day, best-corrected visual acuity (BCVA) of left eye was 0.02(6/300), anterior segment and fundus were in a stable condition, and the percentage of neutrophil cells(NEU%) was 0.725. Topical application of antifungals were continued (qid each), systemic administration was changed to oral voriconazole(100mg bid). On 28th day postoperatively, further consultation revealed BCVA of 0.05 (6/120). Anterior segment was quiet, without obvious inflammation. Through the follow-up of 3-odd months by now, fundus photographs (Figure 3) suggested that the fungal infection of left eye was basically under control. Close monitoring was still essential and patient was asked to pay visit to our clinic on a regular basis.
Figure 3. Fundus appearance-post vitrectomy.
A: 3rd day, the remaining lesion of inferior retina enlarged a little, multiple bleedings were seen across the retina, but satellite lesions were stable; B: 12th day, the yellowish-white lesion became localized; C: 19th day, the lesion with distinct borders became smaller, satellite lesions showed gradual recession; D: 28th day, the greyish-white lesion in inferior retina resolved and was not raised any more. Infratemporal retina showed strand of scarring with fibrosis from vascular arcades to focal zone. Greyish-yellow macular edema and scattered hemorrhagic foci were still present; E: 103th day, hemorrhagic foci resolved and a scar with well-demarcated borders remained
DISCUSSION
Renal transplant patients are vulnerable to various infections, but endogenous aspergillus endophthalmitis (EAE) is a rare complication[5]. Subsequent steroid therapy after misdiagnosis of uveitis further facilitates the development of infection by impairing defense mechanisms. Since EAE is often misdiagnosed and indicative of underlying systemic infections, first priority should be given to early diagnosis to ensure better clinical outcome.
Diagnosis
The diagnosis of EAE is mainly based on common risk factors, clinical manifestations and culture of specimens. Most fungal infections are observed among patients with immune deficiency, such as transplant recipients (major risk factors include intensive immunosuppression and long-term corticosteroid treatment)[6]. Fungal infection usually occurs 3 weeks after the surgery. Clinically, the infection begins as choroidoretinitis in the posterior part of the eye. Whereas, anterior segment is deceptively quiet although an iridocyclitis may occur[2]. Early presentations of our patient include blurred vision, redness, mixed hyperemia, Tyndall (+), and vitreous opacity, which are similar to previous reports. Early fundoscopy and vitreous biopsy may play an important role in diagnosing EAE. Positive culture for aspergillus from vitreous specimen is the most trustworthy, but fungal identification and drug sensitive test will take another week after positive culture. Unlike Candida endophthalmitis, aspergillosis clinically presents with extensive areas of deep retinitis/choroiditis, and vitreous biopsy may not yield positive results[15]. Furthermore, since vitreous biopsy is traumatogenic, we used serial B scan ultrasound to monitor the condition. Disorders of neutrophil function also play a role, since the first line of immunological defense is macrophages and fungi are mainly eliminated by neutrophils[1]. In our patient, neutrophil count on days prior to surgery was 0.903, 0.888, and 0.865 respectively.
Antifungal Treatment
Because of the high correlation between the stage of EFE and final visual acuity, it is very important that treatment be begun as soon as possible[7]. Currently there are no ideal antifungals. The lack of antifungal drugs with high blood-ocular permeability results in an extremely poor visual prognosis. Amphotericin B has long been the standard treatment for proven EAE, but its adverse effects, including renal damage, hematotoxicity, kaliopenia, make it unsuitable for transplant recipients. Besides, the rising of resistance and possibility of focal retina necrosis even with amphotericin B of low doses have prompted the need for new alternatives[8]. Echinocandins, namely caspofungin (CAS), anidulafungin and micafungin (MFG) are new members of the armamentarium of antifungal agents. Micafungin is a new echinocandin and a first line agent for aspergillosis showing no hepatorenal damage[9]. It has excellent efficacy against Aspergillus by inhibiting fungal cell wall beta-glucan synthesis. Micafungin has been reported to inhibit growth of tissue forms of A. fumigatus, and phagocytes plus micafungin together have an additive effect[10]. Considering its pharmacological properties, dose adjustment isn't required for renal impairment when using MFG. In the only RCT comparing CAS and MFG, MFG in doses of 100mg and 150mg were compared with CAS in patients with invasive fungal infection; success rate was comparable with no significant difference in mortality, relapse or adverse effects[11]. Denning et al[9] administered at least one dose of micafungin to 225 patients who met diagnostic criteria for invasive aspergillosis (IA). As both primary and salvage therapy, micafungin proved efficacious and safe in high-risk patients with IA. It's demonstrated that micafungin, either alone or in combination, is a viable option in the treatment of invasive aspergillosis. Azoles are usually used for prophylaxis and maintenance. Numerous case reports demonstrate successful use of systemic voriconazole to treat fungal endophthalmitis. Unlike amphotericin B which requires intravenous administration, voriconazole is available in oral and i.v. forms[6]. It has 96% oral bioavailability in patients with normal gastrointestinal absorption[12]. There're sparse clinical data for the efficacy of combination antifungal therapy, but in-vitro studies and animal models prove that combination therapy may have additive activity against fungi[1]. So the antifungal regimen for our patient is voriconazole(IV GTT), fluconazol (PO) preoperatively, micafungin (IV GTT) postoperatively and oral voriconazole after discharge.
Surgical Interventions
If ocular involvement progresses despite systemic treatment, ophthalmic surgery is recommended. Vitrectomy plus intravitreal injection of antimicrobial drug is the treatment of choice for any type of endophthalmitis[13]. Vitrectomy performed under no contraindications is generally used to remove vitreous abscess, recuperate the transparency of refracting media and deride nidus of infection. Vitrectomy confers significant improvements in vision and should be performed early in severe cases. Previous reports also suggest that a vitrectomy sample is more likely to yield positive culture results than vitreous tap[14].
Prognosis
The prognosis of EAE in kidney graft recipients is reported to be poor as the fungus has often already disseminated to other sites s and recovery of vision is unlikely due to extensive retinal damage[15]. Despite a low incidence, fungal infection in kidney transplant patients are associated with a high mortality, as a result of several factors including a low index of suspicion, lack of early diagnosis, limited antifungal prophylaxis and therapy, and toxicity of antifungal medications[5]. In our case, we tried to investigate for other organ involvement but no obvious finding was made. CT imaging of chest and MR imaging of brain for suspected pulmonary and cerebral aspergillosis respectively are included in the investigation of invasive aspergillosis. To ensure better prognosis, close observation and antifungal treatment should be continued even when patients make a good response to vitrectomy and antifungals. Most patients with chronic pulmonary aspergillosis require long-term maintenance therapy (i.e. months to years), and triazoles are the only oral agents available for this purpose[16]. Contemporarily, there is limited information about the therapy course of EAE. Durand et al[17] reported a case of successful treatment of post-cataract aspergillus endophthalmitis, where caspofungin was continued for 6 weeks and voriconazole for 6 months. In our case, oral voriconazole as maintenance for 3-6 months is recommended.
In conclusion, our case illustrates that immnocompromised patients with known risk factors, like transplant recipients presenting with nonspecific ocular symptoms, should be investigated for EAE. Fundoscopy and B scan ultrasound may aid early diagnosis. Due to small number of reported cases and diversity in treatment and outcomes, the optimal treatment of EAE hasn't been identified yet. A combination therapy of early vitrectomy, systemic and topical application of antifungal agents seems to be an adequate strategy. Novel antifungal agents with better CSF and ocular penetration and fewer side effects may be considered in the control of aspergillosis. Future studies should focus on prophylactic use of antifungal agents because established fungal infection is associated with high mortality. Apparently, there is an urgent need for more studies on inventing ideal antifungal agents and clarifying the effectiveness of new antifungals in the treatment of EAE.
REFERENCES
- 1.Aydin S, Ertugrul B, Gultekin B, Uyar G, Kir E. Treatment of two postoperative endophthalmitis cases due to Aspergillus flavus and Scopulariopsis spp. with local and systemic antifungal therapy. BMC Infect Dis. 2007;31(7):87. doi: 10.1186/1471-2334-7-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schelenz S, Goldsmith DJ. Aspergillus endophthalmitis: an unusual complication of disseminated infection in renal transplant patients. J Infect. 2003;47(4):336–343. doi: 10.1016/s0163-4453(03)00078-1. [DOI] [PubMed] [Google Scholar]
- 3.Weiss JN, Hutchins RK, Balogh K. Simultaneous aspergillus endophthalmitis and cytomegalovirus retinitis after kidney transplantation. Retina. 1988;8(3):193–198. doi: 10.1097/00006982-198808030-00009. [DOI] [PubMed] [Google Scholar]
- 4.Naidoff MA, Green WR. Endogenous Aspergillus endophthalmitis occurring after kidney transplant. Am J Ophthalmol. 1975;79(3):502–509. doi: 10.1016/0002-9394(75)90628-5. [DOI] [PubMed] [Google Scholar]
- 5.Alangaden GJ, Thyagarajan R, Gruber SA, Morawski K, Garnick J, El-Amm JM, West MS, Sillix DH, Chandrasekar PH, Haririan A. Infectious complications after kidney transplantation: current epidemiology and associated risk factors. Clin Transplant. 2006;20(4):401–409. doi: 10.1111/j.1399-0012.2006.00519.x. [DOI] [PubMed] [Google Scholar]
- 6.Chen HL, Chorng JL, Yu HH, Lih SW, Chun LW, Chen CT. Successful Treatment of Two Cases of Invasive Aspergillus Sinusitis with Voriconazole. Tzu Chi Med J. 2010;22(2):106–110. [Google Scholar]
- 7.Takebayashi H, Mizota A, Tanaka M. Relation between stage of endogenous fungal endophthalmitis and prognosis. Graefes Arch Clin Exp Ophthalmol. 2006;244(7):816–820. doi: 10.1007/s00417-005-0182-5. [DOI] [PubMed] [Google Scholar]
- 8.Aliyeva SE, Ullmann AJ, Kottler UB, Frising M, Schwenn O. Histological examination of an eye with endogenous Aspergillus endophthalmitis treated with oral voriconazole: a case report. Graefes Arch Clin Exp Ophthalmol. 2004;242(10):887–891. doi: 10.1007/s00417-004-0901-3. [DOI] [PubMed] [Google Scholar]
- 9.Denning DW, Marr KA, Lau WM, Facklam DP, Ratanatharathorn V, Becker C, Ullmann AJ, Seibel NL, Flynn PM, van Burik JA, Buell DN, Patterson TF. Micafungin (FK463), alone or in combination with other systemic antifungal agents, for the treatment of acute invasive aspergilloses. J Infection. 2006;53(5):337–349. doi: 10.1016/j.jinf.2006.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choi JH, Brummer E, Stevens DA. Combined action of micafungin, a new echinocandin, and human phagocytes for antifungal activity against Aspergillus fumigatus. Microb Infect. 2004;6(4):383–389. doi: 10.1016/j.micinf.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Pappas PG, Rotstein CMF, Betts RF, Nucci M, Talwar D, De Waele JJ, Vazquez JA, Dupont BF, Horn DL, Ostrosky-Zeichner L, Reboli AC, Suh B, Digumarti R, Wu CZ, Kovanda LL, Arnold LJ, Buell DN. Micafungin versus caspofungin for treatment of candidemia and other forms of invasive candidiasis. Clin Infect Dis. 2007;45(7):883–893. doi: 10.1086/520980. [DOI] [PubMed] [Google Scholar]
- 12.Breit SM, Hariprasad SM, Mieler WF, Shah GK, Mills MD, Grand MG. Management of endogenous fungal endophthalmitis with voriconazole and caspofungin. Am J Ophthalmol. 2005;139(1):135–140. doi: 10.1016/j.ajo.2004.08.077. [DOI] [PubMed] [Google Scholar]
- 13.Callegan MC, Gilmore MS, Gregory M, Ramadan RT, Wiskur BJ, Moyer AL, Hunt JJ, Novosad BD. Bacterial endophthalmitis: Therapeutic challenges and host pathogen interactions. Progr Ret Ey Res. 2007;26(2):189–203. doi: 10.1016/j.preteyeres.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weishaar PD, Flynn HW, Jr, Murray TG, Davis JL, Barr CC, Gross JG, Mein CE, McLean WC, Jr, Killian JH. Endogenous Aspergillus endophthalmitis: clinical features and treatment outcomes. Ophthalmology. 1998;105(1):57–65. doi: 10.1016/s0161-6420(98)71225-3. [DOI] [PubMed] [Google Scholar]
- 15.Rao NA, Hidayat AA. Endogenous mycotic endophthalmitis: variations in clinical and histopathological changes in candidiasis compared with aspergillosis. Am J Ophthalmol. 2001;132(2):244–251. doi: 10.1016/s0002-9394(01)00968-0. [DOI] [PubMed] [Google Scholar]
- 16.Jain LR, Denning DW. The efficacy and tolerability of voriconazole in the treatment of chronic cavitary pulmonary aspergillosis. J Infect. 2006;52(5):133–137. doi: 10.1016/j.jinf.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 17.Durand ML, Kim IK, D'Amico DJ, Loewenstein JI, Tobin EH, Kieval SJ, Martin SS, Azar DT, Miller FS, Lujan BJ, Miller JW. Successful treatment of Fusarium endophthalmitis with voriconazole and Aspergillus endophthalmitis with voriconazole plus caspofungin. Am J Ophthalmol. 2005;140(3):552–554. doi: 10.1016/j.ajo.2005.03.030. [DOI] [PubMed] [Google Scholar]