Abstract
AIM
To evaluate the clinical presentations of traumatic optic neuropathy and to assess the visual outcome of three groups of patients managed differently (conservative, intravenous corticosteroids only and combination of intravenous and oral corticosteroids) at an academic tertiary care referral centre.
METHODS
A retrospective study was conducted involving 24 consecutive patients (27 eyes) with traumatic optic neuropathy attending Hospital Universiti Sains Malaysia from January 2007 till December 2009.
RESULTS
Twenty-four patients (27 eyes) were included. All cases involved were males. Mean age was 33 years old. Motor vehicle accident was the major cause (83.3%). Both eyes were equally involved. Most of the eyes had poor vision on presentation (HM-NPL, 81.5%) with associated periorbital haematoma (22 eyes) and subconjunctival haemorrhage (20 eyes). Majority of patients (19 patients, 79.2%) presented with more than one bony fracture of skull or orbit and 5 patients (20.8%) had no fractures. None of the patients had evidence of optic nerve compression on CT scans or MRI done. Eleven patients (45.8%) had been treated with intravenous and oral corticosteroids. The other 7 patients (29.2%) were treated conservatively and the third group (6 patients, 25.0%) was on intravenous corticosteroids only. Eleven of 12 eyes (91.7%) treated with intravenous and oral corticosteroids had shown 1 line improvement of visual acuity. Those eyes treated conservatively (77.8%) had shown 1 line improvement of visual acuity. As for patients treated with intravenous corticosteroids only, four patients remained NPL, one patient had mild visual improvement and the other one's vision remained the same. The visual improvement in patients treated with conservative management was not significant (P=0.386). Patients treated with intravenous corticosteroids alone have shown no visual improvement statistically(P<0.05). Patients treated with intravenous followed by oral corticosteroids had significant visual improvement (P<0.05). There was no statistically significant difference in visual outcome between patients treated with corticosteroids and patients treated conservatively (P=0.368). No patient underwent surgical decompression of the optic nerve. In this series, the follow up ranges from 6 months to 3 years.
CONCLUSION
Most of the traumatic optic neuropathy patients presented with periorbital haematoma, subconjunctival haemorrhage and orbital wall fractures. Patients treated with intravenous followed by oral corticosteroids have better visual outcome compared to conservative management.
Keywords: traumatic optic neuropathy, orbital fractures, corticosteroids
INTRODUCTION
Optic neuropathy is a potential blinding complication of head or orbital trauma. The most common form of traumatic optic neuropathy is indirect damage to the optic nerve and has been reported following 0.5% to 5% of all closed head trauma[1],[2]. It is defined as traumatic visual loss which occurs without external or initial ophthalmoscopic evidence of injury to the eye or its nerve. Indirect injuries are caused by concussive forces that are transmitted to the optic nerve as a result of orbitofacial or cranial trauma[3],[4]. This impact may generate a shock wave which can lead to optic nerve avulsion or posterior indirect traumatic optic neuropathy[5],[6]. On the other hand, direct traumatic optic neuropathy results from direct trauma to the optic nerve from sharp objects, missiles and bony fragments[7]. The clinical presentations vary. The degree of the visual loss does not always correlate with the severity of trauma. The presence or severity of fractures of the orbit neither directly predicts the severity of visual loss nor determines prognosis[8]. The optimal treatment of traumatic optic neuropathy remains controversial. There has been no conclusive evidence for standardized treatment protocol due to lacking of large randomised control trials of management as a result of low incidence of this condition[9]. Observation, corticosteroids treatment and decompression of the optic nerve have been advocated and significant recovery of vision has been found in those treated with corticosteroids, optic nerve decompression, or both as compared to observation alone[10].
MATERIALS AND METHODS
Subjects
A retrospective study was conducted involving 24 consecutive patients (27 eyes) with traumatic optic neuropathy attending Hospital Universiti Sains Malaysia (academic tertiary care referral centre) between January 2007 till December 2009. The patients' particulars were obtained using optic neuropathy database and the medical records were reviewed. The data of 24 patients (27 eyes) were analyzed. All the cases were male. The ages ranged from 5 to 77 years old with mean age of 33 years old. The age group involved was predominantly 11-30 years old group (58.3%). The major causes of trauma were motor vehicle accident (83.3%), followed by blunt trauma (12.5%) and fall (4.2%). Most of the patients were healthy (70.8%) and few of them had diabetes mellitus, hypertension and ischemic heart disease.
Methods
All cases had complete eye examination including associated ocular injuries. The CT scans of brain and/or orbit were reviewed to evaluate the extent of injuries. The visual acuity was the main outcome measure of the study, which was measured by Snellen chart. The visual acuity was assessed at presentation, upon completing corticosteroids and on last follow-up. The associated ocular injuries were carefully evaluated. The treatment regimens were divided into 3 groups. This includes those who were treated conservatively, intravenous methylprednisolone 250mg qid for 3 days without commencement of oral prednisolone and a group which was started on intravenous methylprednisolone 250mg qid for 3 days followed by oral prednisolone 1mg/kg for 11 days.
RESULTS
Most of the eyes had poor vision on presentation (HM-NPL, 62.9%). Periorbital haematoma was present in all cases with skull and/or orbital fractures(Table 1, 2). The CT scans or MRI of brain and/or orbit revealed seven patients with intracranial bleeding. Majority of patients (19 patients, 79.2%) presented with more than one bony fracture of skull and/or orbit and 5 patients (20.8%) had no fractures. None of the patients had evidence of optic nerve compression on CT scan or MRI done. Majority of cases had generalized visual field defect on confrontation test, one patient with poor Glasgow Coma Scale and one paediatric case. All unilateral cases have reverse afferent pupillary defect positive except the three cases with bilateral involvement.
Table 1. Associated eye injuries in 24 patients.
| Types of injury | n |
| Periorbital hematoma | 22 |
| Subconjunctival hemorrhage | 20 |
| Scleral laceration | 1 |
| Exposure keratopathy | 1 |
| Corneal abrasion | 1 |
| Microhyphaema | 2 |
| Uveitis | 1 |
| Anterior lens subluxation | 1 |
| Commotio retinae (Berlin's edema) | 2 |
| Retroorbital hematoma | 1 |
| Carotid carvenous fistula | 1 |
| Other cranial nerve involvement | |
| 3rd cranial nerve | 1 |
| 4th cranial nerve | 2 |
| Total ophthalmoplegia | 1 |
Table 2. Orbital and skull fractures based on CT scan or MRI findings.
| Findings | n |
| Orbital wall fracture | 19 |
| Lateral orbital wall | 3 |
| Medial orbital wall | 5 |
| Superior orbital wall | 3 |
| Orbital floor | 2 |
| Zygomatic complex | 6 |
| Skull fracture | 10 |
| Basal skull | 2 |
| Frontal bone | 6 |
| Parietal bone | 1 |
| Occipital bone | 1 |
| No fracture | 5 |
There were 3 groups of patients which had been managed differently. Eleven patients (45.8%) had been treated with intravenous methylprednisolone 250mg qid for 3 days followed by oral prednisolone 1 mg/kg for 11 days. The second group (7 patients, 29.2%) was treated conservatively due to several reasons including severe head injury (4 patients), uncontrolled diabetes mellitus (2 patients) and young age (1 patient). The third group (6 patients, 25.0%) was on intravenous methylprednisolone 250mg qid for 3 days only. Oral prednisolone was not commenced due to no improvement in the visual acuity after intravenous corticosteroid. There was 77.8% of patients had visual acuity between 5/60 to NPL and 22.2% had 6/12 or better in patients managed conservatively. In the third group, 91.7% of patients had visual acuity between 5/60 to NPL and no patient had 6/12 or better vision.
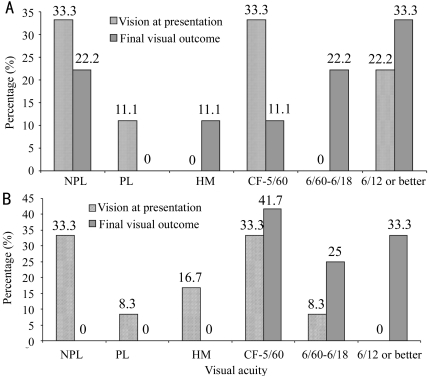
The follow-up ranges from 6 months to 3 years. Eleven of 12 eyes (91.7%) treated with intravenous methylprednisolone 250mg qid for 3 days followed by oral prednisolone 1mg/kg for 11 days had showed at least 1 line improvement of visual acuity (Figure 1). Those eyes treated conservatively (77.8%) had showed at least 1 line improvement of visual acuity (Figure 1). Four patients treated with intravenous corticosteroids only remained NPL, one patient had mild visual improvement from HM to CF only (16.7%) and the other one's vision remained the same.
Figure 1. Comparison of visual acuity based on management.
A: Conservative management; B: Intravenous methylprednisolone and oral prednisolone. CF: counting finger; HM: hand movement; PL: perception of light; NPL: non-perception of light
Patients treated with intravenous followed by oral corticosteroids had significant visual improvement(P<0.05).
The visual improvement in patients treated with conservative management was not significant (P=0.386). Therefore, patients treated with intravenous followed by oral corticosteroids have better visual outcome compared to patients under conservative management. No patients underwent any surgical intervention.
DISCUSSION
Traumatic optic neuropathy can cause optic nerve morbidity such as loss of vision, deficits in visual field, colour perception and an afferent pupillary defect. The diagnostic features of traumatic optic neuropathy are visual loss that occurs in the presence of a relative afferent pupillary defect without evidence of injury to the optic nerve or eye. The commonest site of indirect optic nerve injury is the optic canal[11]. Chou et al[12] had proposed that the damage of optic nerve at microscopic level, including contusion necrosis, nerve fibre tears and nerve infarction secondary to closed space edema, hemorrhage,thrombosis, vasospasm, impingement by bone spicules, and shearing of dural vessels in the optic canal. In an experimental study of primates, significant descending degeneration of the retinal ganglion did not occur until about 3 weeks after optic nerve transection, with maximum loss at 6-8 weeks following the injury[13]-[16].
All our patients with traumatic optic neuropathy were young male, mostly at age 11 to 30 (58.3%) years old which is consistent with other studies[17]-[19]. Motor vehicle accidents (83.3%) were the main cause of traumatic optic neuropathy in our study, while blunt trauma had the second highest incidence rate (12.5%) and followed by fall (4.2%). Similar findings were showed in Sadeghi-Tari study[3],[8],[9]. The involvement of right and left eyes were almost similar. We followed up the patients between 6 months to 3 years and all the patients reached the final vision at 6 months' duration of follow-up as similar in other studies[20],[21].
In the present study, the morbidity associated with traumatic optic neuropathy was decreased visual acuity and relative afferent pupillary defect, which was elicited by swinging flashlight test. The ocular manifestations most commonly associated with optic nerve injury were periorbital hematoma and subconjunctival hemorrhage, with no immediate changes in the optic nerve. The ocular manifestations that were observed in our study are consistent with other studies[17],[18]. Most of the eyes with traumatic optic neuropathy were associated with periorbital hematoma and orbital walls and/or skull fractures. All patients with NPL had periorbital hematoma with subconjunctival hemorrhage and 84.6% of NPL eyes were associated with orbital walls and skull fractures. These signs may indicate the increased morbidity to the optic nerve and strong relation to traumatic optic neuropathy in cases without evidence of optic nerve impingement or compression.
The treatment of traumatic optic neuropathy includes keeping patients under observation, administering corticosteroid therapy, or performing optic nerve decompression with or without steroid therapy[22]. In our study, no surgical optic canal decompression was performed because none of our patients reported having any optic canal fracture or optic nerve impingement in radiological investigation. There is no available optimal management protocol, as most of the published data are either retrospective or presented in case reports[18]. The International Optic Nerve Trauma Study, which was undertaken to formulate an optimal management protocol, failed because of the limited number of eligible patients. The majority of published data do not clearly define the criteria of visual improvement; some studies defined improvement as an increase in 1 to 3 lines in visual acuity[11],[20]. Methylprednisolone therapy was advocated as the initial treatment of choice because of its neuroprotective mechanism[23]. The exact mechanism of corticosteroids in reducing optic nerve injury is still unclear. Steroids may have the neuroprotective effects of decreasing the intraneural or extraneural edema and relieving compression of the nerve fibres. By reducing vasospasm steroids may also limit contusion necrosis of the nerve and block neuronal death in the setting of trauma is through inhibition of free radicals[9].
The International Optic Nerve Trauma Study reported visual acuity improvement in 52% of patients treated with high dose steroids and 37% of patients treated with mega dose steroids in Sadeghi-Tari study[9] after three months' follow-up. Eleven of 12 eyes (91.7%) treated with intravenous methylprednisolone and oral prednisolone had improved at least 1 line of visual acuity, compared to the eyes (77.8%) that were managed conservatively. The visual improvement in patients treated with conservative management was not significant (P=0.386). Those patients treated with intravenous corticosteroids alone showed no visual improvement statistically (P<0.05). However, all eyes only treated with intravenous methylprednisolone did not show vision improvement after 3 days of steroid; therefore the oral steroids were discontinued. In this group, 66.7% of eyes remained NPL after 6 months of follow-up. It indicates that continuation of oral steroids was only beneficial to those eyes with immediate visual improvement after intravenous methylprednisolone.
There are a few limitations in our study. Firstly, this is a retrospective study that leads to the inability to randomly assign patients to each treatment option to ensure a meaningful comparison. Secondly, there is a lack of eligible patients in each group and the number of patients in each group is not similar. Furthermore, no surgical intervention or optic decompression treatment was included because none of them have optic nerve impingement or compression.
In conclusion, most of the traumatic optic neuropathy patients were presented with periorbital hematoma, subconjunctival hemorrhage and orbital wall fractures. Patients treated with intravenous followed by oral corticosteroids have better visual outcome compared to those under conservative management. The continuation of oral corticosteroid is only beneficial to those eyes with immediate visual improvement after intravenous corticosteroid.
REFERENCES
- 1.Carta A, Ferrigno L, Salvo M, Bianchi-Marzoli S, Boschi A, Carta F. Visual prognosis after indirect traumatic optic neuropathy. J Neurol Neurosurg Psychiatry. 2003;74:246–248. doi: 10.1136/jnnp.74.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kovacic M, Gracner T, Gracner B. Indirect Traumatic Optic Neuropathy-Two Case Reports. Coll Antropol. 2001;25:57–61. [PubMed] [Google Scholar]
- 3.Glaser JS. Traumatic optic neuropathy. In: Glaser L, Glaser JS, editors. Neuro-ophthalmology. 3rd ed. Lippincott Williams and Wilkins; 1999. pp. 186–188. [Google Scholar]
- 4.Beretska JS, Rizzo JF. Controversy in the management of traumatic optic neuropathy. Int Ophthalmol Clin. 1994;34:87–96. doi: 10.1097/00004397-199403430-00010. [DOI] [PubMed] [Google Scholar]
- 5.Liu GT, Volpe NJ, Galetta SL. Philadelphia: WB Saunders; 2001. Neuro-ophthalmology: Diagnosis and Management; pp. 170–172. [Google Scholar]
- 6.Kline LB, Morawetz RB, Swaid NS. Indirect injury of the optic nerve. Neurosurgery. 1984;14:756–764. doi: 10.1227/00006123-198406000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Nazir SA, Westfall CT, Chacko JG, Philips PH, Stack BC., Jr Visual recovery after direct traumatic optic neuropathy. Am J Otolaryngol. 2010;31:193–194. doi: 10.1016/j.amjoto.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Cockerham Kimberly Peele. Ophthalmic Care of the Combat Casualty. 2003. Traumatic optic neuropathy; pp. 395–403. [Google Scholar]
- 9.Sadeghi-Tari A, Lashay AR, Tabassi A. Visual outcome of traumatic optic neuropathy in patients treated with intravenous megadose of steroids. Acta Medica Iranica. 2005;43(2):110–114. [Google Scholar]
- 10.Li KK, Teknos TN, Lai A, Lauretano AM, Joseph MP. Traumatic optic neuropathy: result in 45 consecutive surgically treated patients. Otolaryngol Head Neck Surg. 1999;120(1):5–11. doi: 10.1016/S0194-5998(99)70362-1. [DOI] [PubMed] [Google Scholar]
- 11.Steinsapir KD, Goldberg RA. Traumatic optic neuropathy. Surv Ophthalmol. 1994;38:487–518. doi: 10.1016/0039-6257(94)90145-7. [DOI] [PubMed] [Google Scholar]
- 12.Chou PI, Sadun AA, Chen YC, Su WY, Lin SZ, Lee CC. Clinical experiences in the management of traumatic optic neuropathy. Neuro-ophthalmology. 1996;16:325–336. [Google Scholar]
- 13.Quigley HA, Davis EB, Anderson DR. Descending optic nerve degeneration in primates. Invest Ophthalmol Visual Sci. 1977;16:841–849. [PubMed] [Google Scholar]
- 14.Lundstrum M, Frisen L. Evolution of descending optic atrophy: a case report. Acta Ophthalmol. 1975;53:738–746. doi: 10.1111/j.1755-3768.1975.tb01189.x. [DOI] [PubMed] [Google Scholar]
- 15.Medeiros FA, Moura FC, Vessani RM, Susanna R., Jr Axonal loss after traumatic optic neuropathy documented by optical coherence tomography. Am J Ophthalmol. 2003;135:406–408. doi: 10.1016/s0002-9394(02)02049-4. [DOI] [PubMed] [Google Scholar]
- 16.Miyahara T, Kurimoto Y, Kurokawa T, Kuroda T, Yoshimura N. Alterations in retinal nerve fiber layer thickness following indirect traumatic optic neuropathy detected by nerve fibre analyser, GDx-N. Am J Ophthalmol. 2003;136:361–364. doi: 10.1016/s0002-9394(03)00199-5. [DOI] [PubMed] [Google Scholar]
- 17.Rajinganth MG, Gupta AK, Gupta A, Bapuraj JR. Traumatic optic neuropathy: visual outcome following combined therapy protocol. Arch Otolaryngol Head Neck Surg. 2003;129:1203–1206. doi: 10.1001/archotol.129.11.1203. [DOI] [PubMed] [Google Scholar]
- 18.Steinsapir KD. Treatment of traumatic optic neuropathy with high-dose corticosteroid. J Neuroophthalmol. 2006;26:65–67. doi: 10.1097/01.wno.0000204646.94991.68. [DOI] [PubMed] [Google Scholar]
- 19.Entezari M, Rajavi Z, Sedighi N, Daftarian N, Sanagoo M. High-dose intravenous methylprednisolone in recent traumatic optic neuropathy; a randomized double-masked placebo-controlled clinical trial. Graefes Arch Clin Exp Ophthalmol. 2007;245:1267–1271. doi: 10.1007/s00417-006-0441-0. [DOI] [PubMed] [Google Scholar]
- 20.Levin LA, Beck RW, Joseph MP, Seiff S, Kraker R. The treatment of traumatic optic neuropathy: the International Optic Nerve Trauma Study. Ophthalmology. 1999;106:1268–1277. doi: 10.1016/s0161-6420(99)00707-1. [DOI] [PubMed] [Google Scholar]
- 21.Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, Eisenberg HM, Flamm E, Leo-Summers L, Maroon J. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury: Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990;322:1405–1411. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- 22.Luxenberger W, Stammberger H, Jebeles JA, Walch C. Endoscopic optic nerve decompression: the Graz experience. Laryngoscope. 1998;108:873–882. doi: 10.1097/00005537-199806000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Hall ED. The neuroprotective pharmacology of methylprednisolone. J Neurosurg. 1992;76:13–22. doi: 10.3171/jns.1992.76.1.0013. [DOI] [PubMed] [Google Scholar]