Abstract
AIM
To assess and compare the flap morphology using anterior segment optical coherence tomography (AS-OCT) in laser in situ keratomileusis (LASIK) with Femto LDV femtosecond lasers versus Hansatome mechanical Microkeratome.
METHODS
AS-OCT (Visante) was used to compare 1 month postoperatively the morphology of the flaps created with Femto LDV femtosecond lasers or Hansatome Microkeratome. The intended flap thickness was 110µm and 160µm respectively. The thickness of twenty-five points across each flap, which were 0mm, 1.5mm, 2.5mm, and 3.5mm to the corneal vertex on the horizontal, vertical, 45° and 135° meridian respectively, was evaluated.
RESULTS
One month postoperative, the central flap thickness in the Femto LDV group was 107.43±4.70µm, while 125.90±17.50µm in the Hansatome group. The difference between the actual and the expected flap thickness was 5.61±3.84µm and 31.52±12.27µm, respectively. The Hansatome group had presented a statistically significant result (P<0.001). Flap morphology showed a more regular planar shape in the Femto LDV group and a meniscus shape in the Hansatome group.
CONCLUSION
AS-OCT is a direct and fast procedure to assess the flap morphology. The morphology by AS-OCT showed that the flaps created with Femto LDV femtosecond laser were more accurate and regular than the flaps created with Hansatome microkeratome.
Keywords: AS-OCT, laser in situ keratomileusis, flap, femtosecond laser
INTRODUCTION
Currently, laser in situ keratomileusis (LASIK) is the most commonly performed corneal refractive surgery[1]. The most critical step in successful LASIK surgery is the creation of the corneal flap. We have used mechanical microkeratomes to form the flap over the past 20 years. Despite considerable progress has been made with the mechanical microkeratomes, complications such as incomplete flaps, free flaps, buttonholes, and irregular flaps continue to plague refractive surgeons[2]-[4]. With the progressive understanding of corneal morphology, the pursuit of more safer and predictable flaps has led to a bladeless method of flap preparation[5]-[7].
Recently, several new femtosecond laser systems were introduced. These include the IntraLase femtosecond laser (IntraLase Corp.), the Femto LDV (Zeimer Group), and the VisuMax (Carl Zeiss Meditec)[8]. Since the introduction of the IntraLase femtosecond laser for ophthalmic applications, there are several studies have compared this laser with mechanical microkeratomes[9]-[12]. However, little has been published, on the different outcomes between Femto LDV femtosecond laser and microkeratomes. Therefore, the study we present was designed to evaluate the performance of this newer system.
The classical method of measuring corneal flap thickness involved subtracting the residual stromal thickness, determined using ultrasound pachymetry during surgery, from the preoperative corneal thickness[13]. However, that method was not precise enough, and a more direct method of measuring corneal flap thickness became necessary. One direct method is anterior segment optical coherence tomography[14],[15] (AS-OCT, Visante, Carl Zeiss Meditec), which measures flap thickness using real-time images and can be used to measure flap thickness after LASIK. In this study, we used this method to evaluate the flap morphology created by Femto LDV femtosecond laser and mechanical microkeratome, Hansatome (Bausch & Lomb), assessing the accuracy and regularity of the corneal flaps.
We also compared the refractive outcomes at one month postoperative. Perhaps these clinical outcomes would be the most convincing evidence to confirm whether the Femto LDV femtosecond laser have advantages over the microkeratome in the flap-making procedure.
PATIENTS AND METHODS
Patients
This nonrandomized clinical trial involved 50 eyes of 25 patients who were identified as good candidates for LASIK by examinations. All procedures was reviewed and approved by the Ethics Committee of Zhongshan Ophthalmic Center of Sun Yat-sen University. Informed consent was obtained from the subjects after the procedures were explained to them.
The Femto LDV group comprised 24 eyes of 12 patients, and the Hansatome group comprised 26 eyes of 13 patients. All patients had exhibited a stable preoperative corneal topography without evidence of keratoconus, corneal thickness that allowed a minimum residual untreated posterior corneal thickness of 250µm, documented stable refraction for at least 1 year, and best spectacle-corrected visual acuity (BSCVA) of at least 20/20.
Methods
The Femto LDV system delivers nanojoule pulse energy to the eye and uses megahertz repetition rates. The femtosecond laser, using photodisruption to create a corneal cut within the corneal tissue, was programmed to flap thickness of 110µm and flap diameter of 8.5mm. For the microkeratome group, the flap was created by Hansatome with an intended flap thickness of 160µm and flap diameter of 8.5mm. All flaps had a superior hinge. The corneal ablations were performed with the Technolas 217 laser system (Bausch & Lomb) and all eyes were targeted at the refraction of plano.
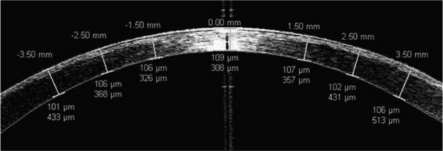
The AS-OCT images of cornea were taken by the same experienced examiner 1 month after surgery. The measurement was repeated 3 times per patient to increase the accuracy with this method. The thickness of twenty-five points across each flap, which were 0mm, 1.5mm, 2.5mm, and 3.5mm to the corneal vertex on the horizontal, vertical, 45° and 135° meridian respectively, was evaluated. The corneal vertex is defined as 0, the negative on the left and positive on the right (Figure 1).
Figure 1. The image of the Femto LDV femtosecond laser flap shows a planar shape and regular morphology in horizontal meridian.
The other examinations were performed at 1 month after LASIK, including manifest refraction, uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), slit-lamp examination and so no.
Statistical Analysis
Statistical analysis was performed with SPSS software (version 17.0, SPSS, Inc.). The results were analyzed with t-test or ANOVA. A P value of 0.05 was taken as the threshold of statistical significance.
RESULTS
Table 1 showed all parameters are not statistically different between the 2 groups preoperatively.
Table 1. Preoperative characteristics in the Femto LDV femtosecond laser group and Hansatome microkeratome group.
| Variable | Femto LDV Group (n=12, 24 eyes) | Hansatome Group (n=13, 26 eyes) |
| Age (y) | 26.27±5.34 | 26.93±4.78 |
| Spherical error (range, D) | -5.98±2.47 (-2.50 to -9.50) | -5.34±1.73 (-2.50 to -8.75) |
| Cylindrical error (range, D) | -0.86±0.75 (0 to -2.50) | -0.67±0.55 (0 to- 1.75) |
| Spherical equivalent (range, D) | -6.28±1.98 (-4.25 to -10.0) | -5.91±1.46(-3.25 to -9.25) |
There was no flap complication in either group. The AS-OCT provided images of complete flap cross section with precise architecture and reduced movement artifacts and distortion[16].
Flap Accuracy
One month postoperative, the central flap thickness in the Femto LDV group was 107.43±4.70µm, while 125.90±17.50µm in the Hansatome group. The mean difference between the actual and the expected flap thickness was 5.61±3.84µm and 31.52±12.27µm, respectively. There was no significant difference in the Femto LDV group, while the Hansatome group presented a statistically significant result (P<0.001). The central thickness of femtosecond laser flap was significantly more accurate than the microkeratome flap (P<0.01).
Flap Regularity
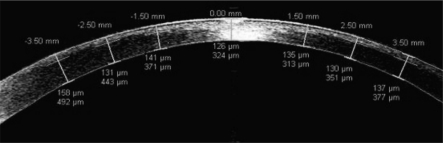
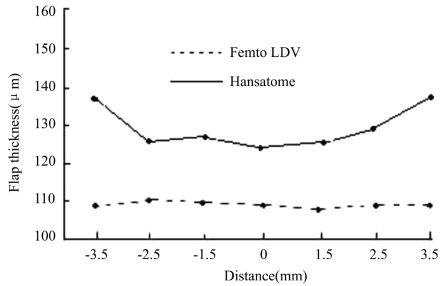
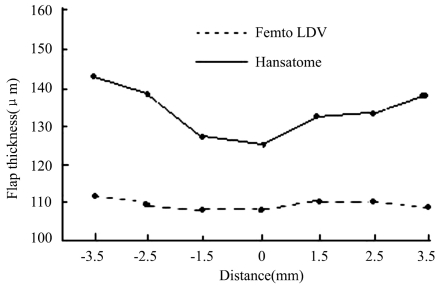
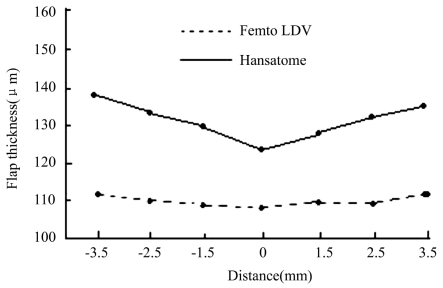
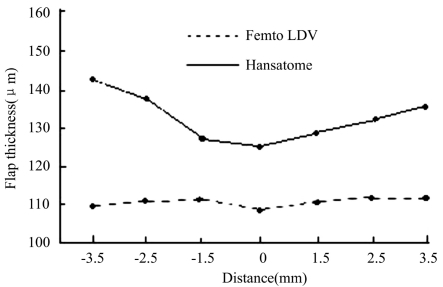
The morphology of the flap showed by the AS-OCT was different between the Femto LDV and Hansatome. The Femto LDV flap had a more regular planar shape (Figure 1). The thickness at the 25 measurement points was scattered around the value of 110.0 mm. The maximum difference between the actual and the expected flap thickness at 25 different measurement points was only 13.0µm. The Hansatome flap was showed with a meniscus shape (Figure 2), which was thin in the center and gradually increased toward the periphery. The thickness at the 25 measurement points have changed significantly (P<0.001). There was no significant asymmetry between the temporal and nasal thickness or the inferior and superior thickness measurements in either group (P>0.05).
Figure 2. The image of the Hansatome microkeratome flap shows a meniscus shape in horizontal meridian.
Figure 3 to Figure 6 provided the mean thickness of the 25 measurement points in different meridians as previously described. We could determine the different morphology of the flap created by Femto LDV femtosecond laser or Hansatome microkeratome.
Figure 3. Mean measurements of the Femto LDV and Hansatome in the horizontal meridian.
Figure 6. Mean measurements of the Femto LDV and Hansatome in the 135° meridian.
Figure 4. Mean measurements of the Femto LDV and Hansatome in the vertical meridian.
Figure 5. Mean measurements of the Femto LDV and Hansatome in the 45° meridian.
Refractive Outcomes
At one month postoperatively, 91.7% of Femto LDV eyes had a UCVA of ≥ 20/20, as compared to 88.5% of Hansatome eyes (P>0.05). There was no loss of BCVA in either group. Accuracy within ±0.50 D of plano was 87.5% for Femto LDV eyes and 84.6% for Hansatome eyes. Table 2 showed the refractive outcomes between the 2 groups postoperatively. There was no statistically significant difference between all these parameters.
Table 2. Postoperative refractive outcomes in the Femto LDV Femtosecond laser group and Hansatome microkeratome group.
| Variable | Femto LDV Group (n=12, 24 eyes) | Hansatome Group (n=13, 26 eyes) |
| UCVA ≥ 20/20 | 91.7% | 88.5% |
| Spherical error (range, D) | -0.02±0.09 (-0.5 to 0.5) | -0.08±0.12 (-0.75 to 0.25) |
| Cylindrical error (range, D) | -0.03±0.11 (0 to -0.5) | -0.05±0.13 (0 to- 0.75) |
| Spherical equivalent (range, D) | -0.05±0.26D (-0.75 to 0.5) | -0.13±0.23 (-0.75 to 0.25) |
DISCUSSION
Previously, the accuracy of flap creation were evaluated exclusively by the central flap thickness[17]. However, the architecture of the entire flap would be the proper way to estimate the morphology. AS-OCT is a direct and fast procedure that has been shown to be useful in the analysis of postoperative flap thickness. AS-OCT has the advantage of showing a cross-section of the cornea so that the flap can be seen and measured directly after surgery. Although the boundaries between the corneal flap and stroma become ambiguous, especially in the central portion of the cornea, the repeatability analysis in the previous study had showed that AS-OCT flap thickness measurement was reliable for the entire extension of the flap[18]. In order to improve the accuracy of this method, the images were taken by the same experienced examiner and the measurement was repeated 3 times per patient. Kim et al[18] also found that measuring corneal flap thickness using AS-OCT became difficult after 1 month, consequently, we used this system to evaluate the precision and morphology of the flap at one month after LASIK.
Flap preparation, which is the most critical step in LASIK, can be performed with a femtosecond laser or a mechanical microkeratome. Previous studies have reported the standard deviation of flap thickness with microkeratomes in the range of ±20 to ±40µm[19],[20]. The aim of more predictable and accurate flaps led to the development of a bladeless method of flap creation with the femtosecond laser. Guy et al[21] have founded that the standard deviation of flaps to be ±29µm with the Hansatome microkeratome (Bausch & Lomb) and ±14.5µm with the IntraLase femtosecond laser. Femto LDV femtosecond laser is a relatively newer system, and the nature of cutting processes is different from IntraLase[22]. In this study, we sought to evaluate whether there was difference between Femto LDV and Hansatome in flap creation using AS-OCT.
The accuracy of the central flap thickness is a key safety consideration for LASIK. In this study, the intended flap thickness was 110µm with Femto LDV and 160um with Hansatome. A recent study has reported the Femto LDV achieved a mean central flap thickness of 130±9µm with an intended flap (thickness) of 130µm in vitro porcine[23]. Similar to other clinical research, we found a slightly thinner than intended central flap thickness(107.43±4.70µm) with Femto LDV[24],[25]. On the other hand, in our study of Hansatome, the mean central flap thicknesses using the 160µm head was 125.90±17.50µm, which presented a large thinner actual flap thickness than would be predicted by the manufacturer. Previous studies also showed that actual flap thickness was thinner than predicted[26],[27]. The lack of precision in central flap thickness would be an important drawback of this instrument, because it would be difficult for the surgeon to evaluate the amount of residual corneal thickness exactly, which was prepared for laser ablation, especially for correction of high myopia.
Although the central flap thickness is very important, the impact of peripheral flap should not be ignored. The AS-OCT images showed that the general morphology of the Femto LDV flaps in all meridians across section were planar and symmetrical in all eyes. The mean flap thickness changed slightly from the central vertex toward the periphery. The thickness at the 25 measurement points was scattered around the setting value of 110.0µm. In contrast, the flap shape is typically thinner in the center and thicker in the periphery with Hansatome. Figure 2 showed this meniscus shape which might increase the incidence of buttonhole perforation. We speculated that the more planar flap morphology would increase the safety of flap formation and, might improve the ablation outcomes.
The Femto LDV femtosecond laser may have advantages over the Hansatome in the flap-making procedure. Theoretically, a better flap architecture would contribute to a superior clinical result, because the precision of the flap was increased, the stability of the flap was improved, the epithelial injury was decreased and so on[21],[28]. However, the clinical relevance of femtosecond laser remains controversial[25],[29]-[31]. In our study, the Femto LDV failed to have significant superiority over Hansatome in refractive outcomes such as UCVA, spherical errors and cylindrical errors (Table 2). The potential reasons might be a limited follow-up time and a small sample. Furthermore, though the microkeratome provided a meniscus-shaped flap, there was no significant asymmetry between the temporal and nasal or the inferior and superior thickness measurements. In addition, our surgeons are good at using microkeratome for many years. A larger controlled prospective trial may be warranted to confirm this finding. Moreover, additional clinical parameters are needed, such as corneal aberration, contrast sensitivity value, corneal sensation and so on.
In summary, the AS-OCT flap morphology measurement is reliable for the entire extension of the flap. Although the similar refractive outcomes with these two systems are present, the Femto LDV femtosecond laser provides precise flaps with predictable thickness and a relatively uniform morphology. We believe that the superior flap accuracy and regularity using femtosecond laser would be a key factor to improve the safety and predictability of LASIK in future. Although postoperative AC-OCT provides a relatively accurate measurement of the corneal flap, in-operative ultrasound corneal pachymetry is still indispensable to LASIC surgery, because it indicates real-time index of flap thickness.
Footnotes
Foundation item: Supported by National Natural Science Foundation of China (No. 81070754)
REFERENCES
- 1.Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, de Luise VP, Koch DD. Laser in situ keratomileusis for myopia and astigmatism: safety and ef cacy. A report by the American Academy of Ophthalmology. Ophthalmology. 2002;109:175–187. doi: 10.1016/s0161-6420(01)00966-6. [DOI] [PubMed] [Google Scholar]
- 2.Knorz MC. Flap and interface complications in LASIK. Curr Opin Ophthalmol. 2002;13(4):242–245. doi: 10.1097/00055735-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Lichter H, Stulting RD, Waring GO, 3rd, Russell GE, Carr J. Buttonholes during LASIK: etiology and outcome. J Refract Surg. 2007;23(5):472–476. doi: 10.3928/1081-597X-20070501-09. [DOI] [PubMed] [Google Scholar]
- 4.Ambròsio R, Jr, Wilson SE. Complications of laser in situ keratomileusis: etiology, prevention, and treatment. J Refract Surg. 2001;17:350–379. doi: 10.3928/1081-597X-20010501-09. [DOI] [PubMed] [Google Scholar]
- 5.Gatinel D, Chaabouni S, Adam PA, Munck J, Puech M, HoangXuan T. Corneal hysteresis, resistance factor, topography, and pachymetry after corneal lamellar flap. J Cataract Refract Surg. 2007;23:76–84. doi: 10.3928/1081-597X-20070101-12. [DOI] [PubMed] [Google Scholar]
- 6.Condon PI. Will keratectasia be a major complication for LASIK in the long term 2005 ESCRS Ridley Medal Lecture. J Cataract Refract Surg. 2006;32:2124–2132. doi: 10.1016/j.jcrs.2006.07.036. [DOI] [PubMed] [Google Scholar]
- 7.Guirao A. Theoretical elastic response of the cornea to refractive surgery: risk factors for keratectasia. J Cataract Refract Surg. 2005;21:176–185. doi: 10.3928/1081-597X-20050301-14. [DOI] [PubMed] [Google Scholar]
- 8.Salomao MQ, Wilson SE. Femtosecond laser in situ keratomileusis. J Cataract Refract Surg. 2010;36:1024–1032. doi: 10.1016/j.jcrs.2010.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sonigo B, Iordanidou V, Chong-Sit D, Auclin F, Ancel JM, Labbe A, Baudouin C. In vivo corneal confocal microscopy comparison of Intralase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2006;47(7):2803–2811. doi: 10.1167/iovs.05-1207. [DOI] [PubMed] [Google Scholar]
- 10.Lim T, Yang S, Kim M, Tchah H. Comparison of the IntraLase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Am J Ophthalmol. 2006;141:833–839. doi: 10.1016/j.ajo.2005.12.032. [DOI] [PubMed] [Google Scholar]
- 11.Sarayba MA, Ignacio TS, Binder PS, Tran DB. Comparative study of stromal bed quality by usingmechanical, IntraLase femtosecond laser 15-kHz and 30-kHz microkeratomes. Cornea. 2007;26:446–451. doi: 10.1097/ICO.0b013e318033e7cc. [DOI] [PubMed] [Google Scholar]
- 12.Sarayba MA, Ignacio TS, Tran DB, Binder PS. A 60 kHz IntraLase Femtosecond laser creates a smoother LASIK stromal bed surface compared to a Zyoptix XP mechanical microkeratome in human donor eyes. J Refract Surg. 2007;23:331–337. doi: 10.3928/1081-597X-20070401-04. [DOI] [PubMed] [Google Scholar]
- 13.Muallern MS, Yoo SH, Romano AC, Mallem MS, Yoo SH, Romano AC, Marangon FB, Schiffman JC, Cullbertson WW. Flap and stromal bed thickness in laser in situ kerotomileusis enhancement. J Cataract Refract Surg. 2004;30(11):2295–2302. doi: 10.1016/j.jcrs.2004.02.080. [DOI] [PubMed] [Google Scholar]
- 14.Nakagawa T, Maeda N, Higashiura R, Hori Y, Inoue T, Nishida K. Corneal topographic analysis in patients with keratoconus using 3-dimensional anterior segment optical coherence tomography. J Cataract Refract Surg. 2011;37(10):1871–1878. doi: 10.1016/j.jcrs.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 15.Chan JB, Yuen LH, Huang EH, Htoon HM, He M, Aung T, Tan DT, Mehta JS. Reproducibility of Cornea Measurements in Anterior Segment OCT Images of Normal Eyes and Eyes with Bullous Keratopathy Analyzed with the Zhongshan Assessment Program. Invest Ophthalmol Vis Sci. 2011;17;52(12):8884–8890. doi: 10.1167/iovs.10-6411. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Netto MV, Shekhar R, Krueger RR, Huang D. A longitudinal study of LASIKflap and stromal thicknesswith high-speed optical coherence tomography. Ophthalmology. 2007;114:1124–1132. doi: 10.1016/j.ophtha.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 17.Reinstein DZ, Srivannaboon S, Archer TJ, Silverman RH, Sutton H, Coleman DJ. Probabilitymodel of the inaccuracy of residual stromal thickness prediction to reduce the risk of ectasia after LASIK. Part II: quantifying population risk. J Refract Surg. 2006;22:861–870. doi: 10.3928/1081-597X-20061101-05. [DOI] [PubMed] [Google Scholar]
- 18.Kim JH, Lee D, Rhee K-I. Flap thickness reproducibility in laser in situ keratomileusis with a femtosecond laser: optical coherence tomography measurement. J Cataract Refract Surg. 2008;34:132–136. doi: 10.1016/j.jcrs.2007.08.036. [DOI] [PubMed] [Google Scholar]
- 19.Arbelaez MC. Nidek MK 2000 microkeratome clinical evaluation. J Refract Surg. 2002;18:S357–S360. doi: 10.3928/1081-597X-20020502-15. [DOI] [PubMed] [Google Scholar]
- 20.Shemesh G, Dotan G, Lipshitz I. Predictability of corneal flap thickness in laser in situ keratomileusis using three different microkeratomes. J Refract Surg. 2002;18:S347–S351. doi: 10.3928/1081-597X-20020502-13. [DOI] [PubMed] [Google Scholar]
- 21.Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(4):804–811. doi: 10.1016/j.jcrs.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 22.Lubatschowski H. Overview of commercially available femtosecond lasers in refractive surgery. J Refract Surg. 2008;24:S102–S107. doi: 10.3928/1081597X-20080101-18. [DOI] [PubMed] [Google Scholar]
- 23.Kermani Omid, MD, Oberheide Uwe., PhD Comparative micromorphologic in vitro porcine study of IntraLase and Femto LDV femtosecond lasers. J Cataract Refract Surg. 2008;34:1393–1399. doi: 10.1016/j.jcrs.2008.04.037. [DOI] [PubMed] [Google Scholar]
- 24.Pietilä J, Huhtala A, Jääskeläinen M, Jylli J, Mäkinen P, Uusitalo H. LASIK flap creation with the Ziemer femtosecond laser in 787 consecutive eyes. J Refract Surg. 2010;26(1):7–16. doi: 10.3928/1081597X-20101215-02. [DOI] [PubMed] [Google Scholar]
- 25.Vryghem JC, Devogelaere T, Stodulka P. Efficacy, safety, and flap dimensions of a new femtosecond laser for laser in situ keratomileusis. J Cataract Refract Surg. 2010;36(3):442–448. doi: 10.1016/j.jcrs.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 26.Maldonado MJ, Ruiz-Oblitas L, Munuera JM, Aliseda D, Garcia-Layana A, Moreno-Montanés J. Optical coherence tomography evaluation of the corneal cap and stromal bed features after laser in situ keratomileusis for high myopia and astigmatism. Ophthalmology. 2000;107(1):81–87. doi: 10.1016/s0161-6420(99)00022-6. [DOI] [PubMed] [Google Scholar]
- 27.Gailitis RP, Lagzdins M. Factors that affect corneal flapthickness with the Hansatome microkeratome. J Refract Surg. 2002;18:439–443. doi: 10.3928/1081-597X-20020701-04. [DOI] [PubMed] [Google Scholar]
- 28.Lim T, Yang S, Kim M, Tchah H. Comparison of the intraLase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Am J Ophthalmol. 2006;141(5):833–839. doi: 10.1016/j.ajo.2005.12.032. [DOI] [PubMed] [Google Scholar]
- 29.Patel SV, Maguire LJ, McLaren JW, Hodge DO, Bourne WM. Femtosecond laser versus mechanical microkeratome for LASIK; a randomized controlled study. Ophthalmology. 2007;114:1482–1490. doi: 10.1016/j.ophtha.2006.10.057. [DOI] [PubMed] [Google Scholar]
- 30.Murakami Y, Manche EE. Comparison of intraoperative subtraction pachymetry and postoperative anterior segment optical coherence tomography of laser in situ keratomileusis flaps. J Cataract Refract Surg. 2011;37(10):1879–1883. doi: 10.1016/j.jcrs.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 31.Hall RC, Mohamed FK, Htoon HM, Tan DT, Mehta JS. Laser in situ keratomileusis flap measurements: Comparison between observers and between spectral- domain and time-domain anterior segment optical coherence tomography. J Cataract Refract Surg. 2011;37(3):544–551. doi: 10.1016/j.jcrs.2010.10.037. [DOI] [PubMed] [Google Scholar]