Abstract
A rare case of bilateral scleromalacia perforans, bilateral peripheral corneal thinning (contact lens cornea) and unilateral orbital inflammatory disease in a 50 year old female patient with an indolent form Wegener's granulomatosis(WG) involving lungs and sinuses is reported. The patient survived for 12 years after the initial diagnosis of systemic disease. There was perforation of left globe following trauma and no perforation of the right globe till the last follow up of the patient.
Keywords: Wegener's granulomatosis, scleromalacia perforans, peripheral thinning of cornea, proptosis
INTRODUCTION
Wegener's granulomatosis (WG) is a systemic disease of unknown aetiology characterized by granulomatous inflammation of upper and lower respiratory tract, necrotizing vasculitis and nephritis. The disease exists in two forms; an indolent form (limited, local-regional, with absence of renal involvement) and fulminate form (active, generalized). Ocular involvement can occur in both forms of the disease, with a reported incidence ranging from 28% to 60% of cases and as high as 87% at some time during the patient's life. It may be present at the time of diagnosis or infact may be the presenting feature in 8% to 16% of patients[1]-[8]. The most common ocular lesions observed in WG patients are orbital inflammatory disease, necrotizing scleritis and peripheral ulcerative keratitis. Orbital involvement is manifested as proptosis and is due to primary granulomatous inflammation or contiguous spread of the disease from adjacent paranasal sinuses. Peripheral ulcerative keratitis is a destructive inflammation of the corneal periphery associated with an epithelial defect producing ulceration and peripheral corneal thinning. It is commonly accompanied by scleritis of the necrotizing type giving rise to red painful eye and blurring of vision. Occasionally, non ulcerative type of peripheral keratitis may manifest as peripheral stromal thinning characterized by gradual resorption of peripheral stroma leaving the epithelium intact. End stage of this may result in a contact lens cornea appearance. This is seen in more commonly in rheumatoid arthritis than in WG. Scleromalacia perforans is a type of anterior necrotizing scleritis without inflammation resulting in progressive scleral thinning[9]. Pubmed seach revealed only one case of bilateral scleromalacia perforans[10], and three cases of peripheral corneal thinning[11],[12] in WG patients. We describe a rare case of bilateral scleromalacia perforans, bilateral peripheral corneal thinning and unilateral orbital inflammatory disease in a patient with an indolent form WG involving lungs and sinuses.
CASE REPORT
A 50 year old Chinese lady was first diagnosed to have WG in August 1992 when she presented with cough, hemoptysis, fever and weight loss. She had nasal obstruction, foul smelling nasal discharge, rhinitis, bilateral maxillary sinusitis. There was sclera thinning and peripheral corneal thinning in the upper nasal quadrant in the left eye. Visual acuity was normal in the left eye. Chest X-ray showed multiple irregular opacities in both lungs. Biopsy from a lung nodule and nasal mucosa showed chronic inflammation with granuloma and a positive antineutrophilic cytoplasmic antibody (ANCA), confirming the diagnosis of WG. Renal function tests and renal biopsy were normal. She was treated with oral cyclophosphamide and prednisolone. All the symptoms resolved and general condition improved. She developed steroid induced diabetes and hypertension in September 1993, and she was treated with oral hypoglycemic and anti hypertensive agents. Cyclophosphamide and prednisolone were tapered slowly and stopped in June 1999.
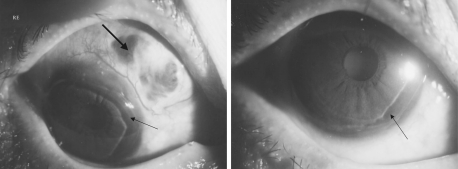
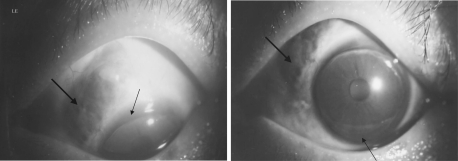
She presented to eye clinic on 28th December 2001 with discomfort, gritty sensation and mild pain in both eyes of one month duration. Right eye: Visual acuity was 6/12, not improving with pinhole. There was mild congestion of conjunctiva in upper nasal quadrant. Sclera thinning in upper nasal quadrant with visible uveal tissue and no signs of inflammation was noted. There was peripheral corneal thinning ( of corneal thickness) in upper and lower temporal quadrants (Figure 1). Anterior chamber, iris and pupil were normal. Posterior subscapsular cataract was present. Applanation tension (intraocular pressure) was 18mmHg. Ocular movements were normal.
Figure 1. Right eye showing scleral thinning in upper nasal quadrant with visible uveal tissue (thick arrow) and peripheral corneal thinning in upper and lower nasal quadrants (thin arrow).
Left eye: visual acuity was 6/12, not improving with pinhole. There was mild circumcorneal congestion of the conjunctiva. Scleral thinning with visble uveal tissue and no signs of inflammation was noted in upper nasal quadrant. There was non vascularized peripheral corneal thinning all round the cornea with overhanging edges giving the appearance of contact lens cornea (Figure 2). Anterior chamber, iris and pupil were normal. Posterior subcapsular cataract was present. Applanation tension (intraocular pressure) was 16mmHg. Fundus examination, after dilating the pupils with 10g/L Tropicamide eye drops, did not show any abnormality in both eyes.
Figure 2. Left eye showing scleral thinning in the upper nasal quadrant with visible uveal tissue(thick arrow) and peripheral corneal thinning in the upper and lower part of limbus(thin arrow).
Halitosis and saddle nose deformity were noted. A repeat ANCA was positive and she was restarted on oral prednisolone by the chest physician. Scleral thinning remained unchanged in both eyes. However, peripheral corneal thinning progressed slowly around the cornea (360 degrees) in the right eye over a period of one year, giving the appearance of contact lens cornea in both eyes.
Her vision in March 2003 was 6/36 in the right eye and 6/24 in the left eye. The reduced visual acuity was due to posterior subcapsular cataract in both eyes. She developed redness and proptosis of the left eye (8 mm protrusion) in July 2003. MRI showed infiltration of left maxillary, ethmoidal, frontal sinuses and left orbit (Figure 3).
Figure 3. MRI showing infiltration of left maxillary, ethmoidal, frontal sinuses and left orbit (arrow marks).
In August 2003, she presented to casualty department with severe pain and discharge after she accidentally knocked her left eye against a door, one day prior to the visit. Left eye was proptosed and lids were erythematous and swollen. She could not open her eyelids. On separating the lids with eye speculum, a large perforation involving the superior thinned limbal cornea with prolapse of vitreous and uveal tissue were noted. Vision in the left eye was only perception of light. She was admitted to eye ward and IV ciprofloxacin and gentamicin were started. Right eye findings were same as before with good vision. Computed tomography (CT) scan of the orbits showed proptosis of left eye with retrobulbar infiltration of granulomatous tissue and vitreous haemorrhage (Figure 4).
Figure 4. CT scan showing proptosis, retrobulbar infiltration (arrow) and vitreous haemorrhage (arrow) in the left eye.
She was advised evisceration in view of ruptured globe and poor vision for which patient agreed. Evisceration of left eye was done under general anaesthesia. Postoperatively, IV antibiotics were continued. The patient was discharged from the hospital after one week.
At last follow up in February 2004, her vision in right eye was 6/36 (with pin hole 6/24), peripheral thinning of cornea and sclera were same. Immature cataract was present. Left socket was clean and prosthesis was fitted. Her general condition remained stable. Later on, the patient defaulted follow up; on enquiry by telephone we came to know that the patient died in her house in July 2004.
DISCUSSION
The ophthalmic manifestations of WG described in the literature include non-specific conjunctivitis, tarso-conjunctival granulomatous inflammation with scarring, episcleritis, scleritis, granulomatous sclera-uveitis, peripheral ulcerative keratitis, uveitis, retinitis, retinal vasculitis, exudative retinal detachment, optic neuropathy, nasolacrimal duct obstruction, orbital inflammatory disease and ocular motor cranial neuropathy[1]-[8]. Ocular involvement may result from a variety of pathologies. These include focal vasculitis of small arterioles, veins and areteries, granulomatous inflammation, vascular thrombosis and haemorrhage, or as a consequence of chronic inflammation or ischemia or as a contiguous spread of the disease from the adjacent paranasal sinuses[3].
Scleritis of the necrotizing type is the most common ocular pathology seen in WG, occurring in more than half of patients with ocular WG[1],[13]. Scleritis in WG reflects the severity of the systemic involvement[1],[5]. Its pathological process is due to primary granulomatous vasculitis with consequent ischemia. This can potentially result in limbal ischemia and sclera necrosis with risk of perforation. Peripheral keratitis is usually associated with anterior scleritis, especially so with the necrotizing type[5].
Scleromalacia perforans is one of the types of anterior scleritis which occurs in autoimmune diseases. The presentation is usually of a black or gray area of scleral thinning surrounded by active inflammation. This patient had progressive scleral thinning without inflammation, (scleromalacia perforans) which is usually seen more often in rheumatoid arthritis[9]. Occurrence of scleromalacia perforans in WG is rare and only one such case has been reported in the literature[10].
Peripheral ulcerative keratitis develops after breakdown of the peripheral corneal epithelium and progresses centrally and circumferentially. It may appear similar to Mooren's ulcer except the sclera involvement. Peripheral corneal infiltration or thinning occurs in a patient with an underlying autoimmune disease like rheumatoid arthritis or WG. In patients with systemic vasculitis the corneal involvement has been attributed to occlusive vasculitis involving the intrascleral portions of the anterior ciliary or perilimbal vessels[14]. Circulating antibodies to both corneal conjunctival epithelium have been detected in serum from peripheral ulcerative keratitis patients[15]. There is immune complex deposition in peripheral cornea; diseased epithelium, keratocytes and recruited inflammatory cells may result in release of matrix metalloproteinases that degrade collagen and extracellular matrix resulting in thinning of cornea[9].
Our patient had peripheral corneal thinning without ulceration. The thinning of cornea was all round, giving the appearance of contact lens cornea' in both eyes. The thinning of peripheral cornea was so severe in the left eye that a blunt trauma caused a perforation of the globe which could not be salvaged.
This unusual case highlights how eye changes commonly seen in rheumatoid arthritis can also be present in a systemically debilitating disease such as WG. Before the orbital involvement, that accounts for the most common ocular finding in WG patients as reported in the literature, our patient developed atypical eye changes much earlier in the form of scleromalacia perforans and peripheral corneal thinning(without signs of inflammation) in both eyes. Presence of such atypical eye signs should be investigated for autoimmune diseases so that the systemic disease can be diagnosed early and treated effectively to improve the quality of life and save the life of the patient.
REFERENCES
- 1.Pakrou N, Selva D, Leibovitch I. Wegener's granulomatosis: Ophthlmic manifeatations and management. Semin Arthritis Rheum. 2006;35(5):284–292. doi: 10.1016/j.semarthrit.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Foster CS, Yang J. Wegner's granulomatosis. In: Albert DM, Jakobiec FA, editors. Principles and practice of ophthalmology. 2nd ed. Vol. 5. Vol. 2000. Philadelphia: WB saunders; pp. 4578–4588. In: [Google Scholar]
- 3.Harman LE, Margo CE. Wegner's granulomatosis. Surv Ophthalmol. 1998;42(5):458–480. doi: 10.1016/s0039-6257(97)00133-1. [DOI] [PubMed] [Google Scholar]
- 4.Sadiq SA, Jennings CR, Jones Ns, Downes RN. Wegener's granulomatosis: the ocular manifestations revisited. Orbit. 2000;19(4):253–261. doi: 10.1076/orbi.19.4.253.2654. [DOI] [PubMed] [Google Scholar]
- 5.Bullen CL, Leisegang TJ, McDonald TJ, DeRemee RA. Ocular complications of Wegener' granulomatosis. Ophthalmology. 1983;90(3):279–290. doi: 10.1016/s0161-6420(83)34574-7. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, Rottem M, Fauci AS. Wegener's granulomatosis: An analysis of 158 patients. Ann Intern Med. 1992;116(6):488–498. doi: 10.7326/0003-4819-116-6-488. [DOI] [PubMed] [Google Scholar]
- 7.Haynes BF, Fishman ML, Fauci AS, Wolff SM. The ocular manifestations of Wegener's granulomatosis: Fifteen years experience and review of the literature. Am J Med. 1977;63(1):131–141. doi: 10.1016/0002-9343(77)90125-5. [DOI] [PubMed] [Google Scholar]
- 8.Reinhold-Kellor E, Beuge N, Latza U, de Groot K, Rudert H, N lle B, Heller M, Gross WL. An interdisciplinary approach to the care of patients with Wegener's granulomatosis: long-term outcome in 155 patients. Arthritis Rheum. 2000;43(5):1021–1032. doi: 10.1002/1529-0131(200005)43:5<1021::AID-ANR10>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 9.Kanski JJ. 6th ed. Edinburogh: Butterworth Heinemann Elsevier; Clinical Ophthalmology- A systematic approach; p. 2007. [Google Scholar]
- 10.Bambery P, Gupta A, Sakhuja V, Kaur U, Gangwar DN, Jain IS, Deodhar SD. Ocular manifestations of Wegener's granulomatosis in north India. Sarcoidosis. 1988;5(2):132–135. [PubMed] [Google Scholar]
- 11.Biswas J, Babu K, Gopal L, Krishnakumar S, Suresh S, Ramakrishnan S. Ocular manifestations of Wegener's granulomatosis: Analysis of nine cases. Indian J Ophthalmol. 2003;51(3):217–223. [PubMed] [Google Scholar]
- 12.Miserocchi E, Waheed NK, Baltaztzis S, Foster CS. Chronic cicatrizing conjunctivitis in a patient with ocular cicatricial pemphigoid and fatal Wegener's granulomatosis. Am J Ophthalmol. 2001;132(6):923–924. doi: 10.1016/s0002-9394(01)01194-1. [DOI] [PubMed] [Google Scholar]
- 13.Harper SL, Letko E, Samson CM, Zafirakis P, Sangwan V, Nguyen Q, Uy H, Baltatzis S, Foster CS. Wegener's granulomatosis: the relationship between ocular and systemic disease. J Rheumatol. 2001;28(5):1025–1032. [PubMed] [Google Scholar]
- 14.Austin P, Green WR, Sallyer DC, Walsh FB, Kleinfelter HT. Peripheral corneal degeneration and occlusive vasculitis in Wegener's granulomatosis. Am J Ophthalmol. 1978;85(3):311–317. doi: 10.1016/s0002-9394(14)77721-9. [DOI] [PubMed] [Google Scholar]
- 15.John SL, Morgan K, Tullo AB, Holt PJ. Cornea autoimmunity in patients with peripheral ulcerative keratitis in association with rheumatoid arthritis and Wegener's granulomatosis. Eye. 1992;6(Pt6):630–636. doi: 10.1038/eye.1992.136. [DOI] [PubMed] [Google Scholar]