Abstract
AIM
To report maternal and fetal adverse outcomes, in spite of appropriate treatment and regular follow up, in diabetic pregnant women with proliferative diabetic retinopathy.
METHODS
Case series of four young pregnant diabetics aged between 20 and 25 years with type I diabetes mellitus and proliferative diabetic retrinopathy.
RESULTS
The maternal adverse outcomes were abortion in one patient, pre-eclampsia and preterm delivery in one patient, and renal failure requiring dialysis in one patient. The fetal adverse outcomes were neonatal death in one case and premature baby in another case.
CONCLUSION
These cases highlight the fact that diabetic pregnant women should be closely followed up by the obstetricians and physicians when they have proliferative retinopathy. The proliferative diabetic retinopathy should be considered as a part of the assessment when counseling a diabetic woman in antenatal check up and also in the follow up visits during pregnancy.
Keywords: pregnancy, type I diabetes mellitus, proliferative diabetic retinopathy, vitreous haemorrhage
INTRODUCTION
Proliferative diabetic retinopathy is a sight threatening condition and also a poor prognostic factor in pregnancy. Termination of pregnancy due to proliferative retinopathy is no longer the trend of management with the advancements in the ophthalmologic, medical and obstetrical fields. Any complication of diabetes mellitus in pregnancy is a significant morbidity and may have a psychosocial impact on mother and newborn. Maternal complications include preterm labour, infectious morbidities, hydramnios, hypertensive disorders (pre-eclampsia, eclampsia) and worsening of retinopathy. Fetal and neonatal complications include still birth, congenital malformations, altered fetal growth, metabolic abnormalities, polycythemia, hyperbilirubinemia, cardiomyopathy and respiratory distress syndrome[1].
A study by Klein et al on the outcome of pregnancy found that of maternal age, duration of diabetes, glycosylated hemoglobin, proteinuria, cigarette smoking status and severity of diabetic retinopathy, only the last variable significantly predicted an adverse outcome[2]. Therefore the severity of retinopathy should be considered as a part of the assessment when counseling a diabetic woman when she becomes pregnant. We describe four type I diabetic women with proliferative diabetic retinopathy who had adverse maternal and fetal outcomes.
CASE SERIES
In the course of a study of all diabetic pregnant women (with preexisting diabetes mellitus before pregnancy) who attended the eye clinic from Jun. 2006 till Jun. 2008, four patients with proliferative diabetic retinopathy were identified in the first trimester and followed up until 4 weeks after delivery. Visual acuity on the Snellen chart and fundus examination (with dilated pupils) with slitlamp biomicroscope using 90 D lens were performed in each ophthalmic visit of these patients. Laser panretinal photocoagulation was performed when indicated. The patients' systolic and diastolic blood pressure, glycosylated haemoglobin (HbA1c) level, proteinuria and any significant obstetric findings were noted. The delivery notes and the fetal outcomes were reviewed.
Case 1
A 21-year-old primigravida was first seen in the eye clinic on Jan. 2008 at 10 weeks of her unplanned pregnancy. She was diagnosed to have type 1 diabetes mellitus one year prior to pregnancy but was not compliant to treatment. Her presenting visual acuity was hand movement in the right eye and 6/36 in the left eye. Poor visual acuity was attributed to diffuse vitreous haemorrhage in the right eye and active proliferative diabetic retinopathy in the left eye. Her diabetic control was poor prior to conception as evidenced by high HbA1c (10.2%) at antenatal booking. Blood pressure was normal and there was no nephropathy. She underwent one session of immediate panretinal photocoagulation in both eyes at presentation. However, the following week she had a missed abortion and was admitted in the hospital for dilatation and curettage. Post abortion laser treatments were continued for few more sessions and her visual acuity improved to 6/18 in both eyes. The vitreous haemorrhage in the right eye absorbed slowly over time, and vision improved to 6/12 in both eyes. She was counseled for her next pregnancy by the obstetrician.
Case 2
A 20-year-old lady with known type 1 diabetes mellitus for 8 years was seen in the eye clinic on Mar. 2008 at 12 weeks of gestation. She had an abortion earlier and this was her second pregnancy. Two years ago, she had received laser treatment (panretinal photocoagulation) in her right eye for proliferative diabetic retinopathy and had undergone pars plana virectomy for vitreous haemorrhage clearance in her left eye. The proliferative diabetic retinopathy was stable after that in both eyes. At presentation, her best corrected visual acuity was 6/9 in the right eye and 6/24 in the left eye. Ophthalmic examination showed stable proliferative diabetic retinopathy with adequate laser scars in both eyes. Her HbA1c was 7.9%, blood pressure was within normal limit and there was no proteinuria. For the next 8 weeks of follow-up, her diabetic retinopathy remained quiescent and the glycemic control was satisfactory. Unfortunately at 20 weeks of gestation, she started to have microalbuminuria with progressive deterioration of kidney function leading to generalized body oedema. She remained normotensive. The kidney-ureter-bladder ultrasound was normal. At 32 weeks of gestation, the Doppler ultrasound examination showed a high resistance in the umbilical artery of the fetus, indicating that the fetus was compromised. An emergency caesarean section was performed immediately and a preterm baby with a birth weight of 1.755kg was delivered. Despite good intensive care, the baby passed away at day nine of life due to respiratory distress syndrome.
Case 3
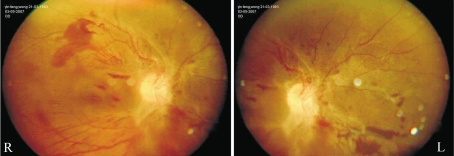
A 25-year-old primigravida attended eye clinic on Feb. 2008 at 9 weeks of gestation. She had pregestational type 1 diabetes mellitus for 12 years associated with hypertension and cerebrovascular accident with left hemiparesis one year prior to pregnancy. She was under regular follow up in the eye clinic for proliferative diabetic retinopathy in both eyes. Laser panretinal photocoagulation was carried out in both eyes one year back. At presentation, her best corrected visual acuity in the right eye was 6/6 and in the left eye was counting finger. Fundus examination of both eyes showed presence of fibrous tissue tractions in the temporal quadrants of both eyes (Figure 1) with diffuse vitreous haemorrhage in the left eye. Laser scars were seen faintly in both eyes, but not sufficient.
Figure 1. Fundus photographs of severe proliferative diabetic retinopathy showing fibrous tissue tractions in the temporal quadrants of both eyes.
She was topped up with panretinal photocoagulation in both eyes and the eyes responded well. At the same time, the blood pressure reading was noted to be borderline high (140/90mmHg); HbA1c level was 8.7%; and there was trace of microalbuminuria. Her anti-hypertensive agent (nifedipine) was increased to a higher dosage and subcutaneous low-molecular weight heparin was added in view of her previous cerebrovascular event. At 28 weeks of gestation, the vitreous haemorrhage had resolved in the left eye and the visual acuity improved to 6/12. Her glycemic control was maintained in the range of 4.0-7.0mmol/Lwith short acting insulin before meals and intermediate acting insulin at bedtime. By 29 weeks of gestation, there was progressive increase in proteinuria despite good blood pressure control and she also required a higher dose of both short acting and intermediate acting insulin in order to maintain the desired glycemic level. There was no evidence of fetal compromise yet at that time. At 34 weeks of gestation, the patient began having raised blood pressure readings of systolic up to 170mmHg and diastolic up to 130mmHg. She also developed features of impending eclampsia and acute pulmonary oedema that required an emergency caesarean section to be performed. She delivered a healthy baby with the birth weight of 2.012kg. Post delivery, she recovered well. The vision remained same at 6/6 in the right eye and 6/12 in the left eye
Case 4
A 24-year-old woman with type 1 diabetes for 10 years was under regular follow up in the eye clinic for proliferative diabetic retinopathy. She was receiving laser photocoagulation treatments in both eyes when she got pregnant. Previously, in the pre-gestation period, she had been advised to undergo pars plana vitrectomy with endolaser treatment in the left eye to control the severe proliferative changes, but the patient deferred. When the patient was reviewed at 8 weeks of gestation in the eye clinic on Mar. 2008, her best corrected visual acuity was 6/6 in the right eye and 6/24 in the left eye. Fundus examination revealed florid proliferative diabetic retinopathy with inferior vitreous haemorrhage in the right eye and tractional retinal detachment with vitreous haemorrhage in the left eye. She was found to have +++ proteinuria, but renal function tests were normal. Her blood pressure was high, so she was started on oral methyldopa. Her HbA1c was 7.3%. As the pregnancy progressed, she was given few sessions of panretinal photocoagulation in both eyes, with no favorable response. The vitreous haemorrhage persisted in both eyes. She continued to receive the laser treatment throughout the pregnancy. Despite strict insulin therapy, the proteinuria progressively worsened and she developed acute renal failure at 27 weeks of gestation, requiring haemodialysis every alternate day. Hypertension was controlled medically. At 28 weeks of gestation, the Doppler ultrasound examination showed fetal compromise and she underwent emergency caesarean section. A premature baby with the birth weight of 900g was delivered. The baby was ventilated for 2 months and fortunately baby survived. Post delivery, the patient however continued to have renal failure and needed continuous ambulatory peritoneal dialysis. Her diabetic retinopathy progressed in the left eye with a drop in visual acuity to 6/60. She subsequently underwent pars plana vitrectomy with endolaser treatment in the left eye. However, her left eye did not improve and continued to progress to neovascular glaucoma, with final visual acuity of perception to light. The visual acuity in right eye remained at 6/12.
DISCUSSION
The above case series highlight how complicated a pregnancy can be in the presence of proliferative diabetic retinopathy. The spectrum of pregnancy outcomes that encountered in this series ranged from abortion to complicated pregnancy. In case 1, the pregnancy was unsuccessful due to poor glycemic control prior to pregnancy. In case 2, despite having persistent proteinuria, fortunately she did not progress to renal failure and had normal blood pressure readings throughout. However, her pregnancy was terminated at 32 weeks of gestation due to fetal compromise and eventually the baby passed away due to respiratory distress at day nine of life. In case 3, her pregnancy was complicated by hypertension, progressive proteinuria and uncontrolled diabetes requiring high dose of insulin therapy and finally she developed signs and symptoms of impending eclampsia. Fortunately the baby was not affected even though she had a preterm delivery. Case 4 had the worst outcome of all patients. She developed a permanent renal impairment requiring regular dialysis. Her baby was only 900gm and was nursed in the neonatal intensive care unit for prematurity. Even though the baby survived, there are possibilities of various morbidities associated with prematurity in the baby's later life.
Pregnancy is well known to affect the progression of diabetic retinopathy and can have adverse ocular outcome for the pregnant woman[3]. Poor glycemic controls at antenatal booking and rapid improvement in glycaemic control in early pregnancy have been shown to be risk factors for progression of retinopathy in pregnancy[4]. Laser photocoagulation remains the mainstay of treatment with reasonable outcomes.[5] Except in case 1, all other patients received laser photocoagulation and they did not show any worsening of diabetic retinopathy throughout the pregnancy. Progression of proliferative retinopathy may depend upon whether or not laser photocoagulation has been carried out before pregnancy. It has been noted that the risk of progression is decreased when laser treatment has been given prior to pregnancy[6]. Therefore, photocoagulation therapy is highly recommended if severe non proliferative or proliferative diabetic retinopathy is detected before the pregnancy. Proliferative diabetic retinopathy may not regress in the postpartum period as seen in case 4. In fact the retinopathy in this patient progressed in the post partum period, probably due to the delayed treatment as patient was not stable at that time. It is commonly believed that diabetic retinopathy regresses in the postpartum period[7].
However, a retrospective review of eight patients who developed sight-threatening diabetic retinopathy showed that the retinopathy did not regress in the postpartum period[8]. It has been reported that diabetic nephropathy is present in 5-10% of diabetic pregnancies[9]. Pregnancies complicated by nephropathy is associated with high complication rate such as renal failure during or after pregnancy, superimposed pre-eclampsia, intrauterine growth restriction, higher caesarean section rate and preterm deliveries. The complication of renal failure requiring frequent dialysis was seen in case 4 of our series.
In conclusion, good glycaemic control during pre-conceptual and pregnancy period have been shown to be associated with better maternal and fetal outcomes. Pre-pregnancy counseling is vital for diabetic women. The pregnancy should be planned in order to avoid the distressing outcomes. Our case series indicate the need of close follow-up during pregnancy and postpartum period in diabetic pregnant women with proliferative diabetic retinopathy.
REFERENCES
- 1.Reece EA, Homko CJ. Diabetes mellitus and pregnancy. In: Scott JR, Gibbs RS, Karlen BY, Haney AF, editors. Danforth's Obstetrics and Gynaecology. 9. Philadelphia: Lippincott Williams & Wlikins; 2003. pp. 247–256. In. [Google Scholar]
- 2.Klein BE, Klein R, Meuer SM, Moss SE, Dalton DD. Does the severity of diabetic retinopathy predict pregnancy outcome? J Diabet Complications. 1988;2(4):179–184. doi: 10.1016/s0891-6632(88)80005-9. [DOI] [PubMed] [Google Scholar]
- 3.Klein BE, Moss SE, Klein R. Effect of pregnancy progression of diabetic retinopathy. Diabetes Care. 1990;13(1):34–40. doi: 10.2337/diacare.13.1.34. [DOI] [PubMed] [Google Scholar]
- 4.Phelps RL, Sakol L, Metzger BE, Jampol LM, Frenkel N. Changes in diabetic retinopathy during pregnancy: correlations with regulation of hyperglycemia. Arch Ophthalmol. 1986;104(12):1806–1810. doi: 10.1001/archopht.1986.01050240080044. [DOI] [PubMed] [Google Scholar]
- 5.Price JH, Hadden DR, Archer DB, Harley JM. Diabetic retinopathy in pregnancy. Br J Obstet Gynaeco. 1984;91(1):11–17. doi: 10.1111/j.1471-0528.1984.tb05272.x. [DOI] [PubMed] [Google Scholar]
- 6.Best RM, Chakravarthy U. Diabetic retinopathy in pregnancy. Br J Ophthalmol. 1997;81(3):249–251. doi: 10.1136/bjo.81.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serup L. Influence of pregnancy on diabetic retinopathy. Acta Endocrinol Suppl (Copenh) 1986;277:122–124. doi: 10.1530/acta.0.111s0122. [DOI] [PubMed] [Google Scholar]
- 8.Chan WC, Lim LT, Quinn MJ, Knox FA, McCance D, Best RM. Management and outcome of sight-threatening diabetic retinopathy in Pregnancy. Eye. 2004;18(8):826–832. doi: 10.1038/sj.eye.6701340. [DOI] [PubMed] [Google Scholar]
- 9.Landon MB, Gabbe SG. Diabetes mellitus and pregnancy. Obstet Gyn Clin North Am. 1992;19(4):633–648. [PubMed] [Google Scholar]