Abstract
A 22-year-old patient suffering from both-side extreme hyperopia with amblyopia was corrected with an Artisan iris-fixated intraocular lens (IOL) implantation followed to clear lens extraction (CLE) with posterior chamber (PC)-IOL implantation. The preoperative refraction values were +17.75DS -1.50DC × 168° for the right eye and +17.25DS -0.75DC × 8° for the left eye. The uncorrected visual acuity (UCVA) was 20/200 bilaterally and the spectacle-corrected visual acuity (BSCVA) was 20/50 bilaterally. One year after Artisan iris-fixated IOL implantation, bilateral BSCVA was 20/50 with a refraction of +1.25DS -0.75DC × 13° for the right eye and +1.50DS -1.00DC × 55° for the left eye. The outcomes of an Artisan iris-fixated IOL implantation followed to CLE with PC-IOL implantation were encouraging for the correction of extreme hyperopia. Long term follow-up examinations were necessary for further determination of the efficacy and safety of this combinational procedure.
Keywords: hyperopia, clear lens extraction, iris-fixated intraocular lens
INTRODUCTION
The correction of extreme hyperopia remains to be a great challenge for refractive surgeries. The selective surgical techniques include phakic intraocular lens (pIOL) implantation or clear lens extraction (CLE) with posterior chamber-intraocular lens (PC-IOL) implantation, which are relatively effective for the treatment of high hyperopia[1], [2]. However, optimal results have not yet been achieved in the case of extreme hyperopia because of the critical range of anterior chamber for pIOL or the limitation of available power for PC-IOL. The combination of different surgical procedures could potentially provide an approach for the correction of extreme hyperopia.
We presented here a case of bilateral extreme hyperopia treated by Artisan iris-fixated IOL implantation after CLE combined with PC-IOL implantation.
CASE REPORT
A 22-year-old man was suffering from both-side extreme hyperopia with amblyopia. He received two-stage procedure treatment. Clear lens was extracted and a PC-IOL with the diopter of +34.0D (Rayner 570C, Rayner Intraocular Lenses LTD., Hove, England) was implanted in the capsular bag for the both eyes one after the other. After 3 months, an Artisan iris-fixated IOL (Artisan Aphakia IOL 205001Y, Ophtec B.V., Groningen, The Netherlands) was implanted with the power of +17.5D for the right eye and +14.5D for the left eye. The power of Artisan IOL was calculated with van der Heijde formula, which uses the mean corneal curvature (K), the adjusted anterior chamber depth (ACD), and the patient's spherical equivalent (SE) at a vertex distance of 12.0mm3. After 3 months of Artisan IOL implantation, posterior capsule opacity (PCO) occurred and Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser capsulotomy was performed in the both eyes.
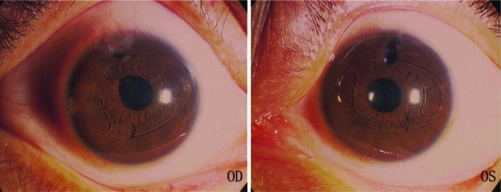
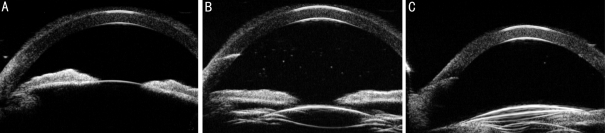
The pre- and post-operative examinations included slit-lamp microscopy, dilated fundus examination, cycloplegic and manifest refraction, uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BSCVA) (Snellen visual chart), central corneal thickness (CCT) and White-to-White (WTW) (Orbscan II, Orbtek Inc., Bausch & Lomb, Rochester, NY), intraocular pressure (IOP) (Goldmann applanation tonometry, Haag-streit, Bern, Switzerland), endothelial cell density (ECD) (Konan Specular Microscope SP-9000, Konan Medical Inc., Tokyo, Japan), ACD (ultrasound biomicroscopy, SUOER UBM scan SW-3200, Tianjin Suowei Inc., Tianjin, China), and axial length (AXL) (A-ultrasound scanning, Cinescan A/B scan, Quantel Medical Inc., France). The clinical evaluation was shown in Table 1. The photography of anterior segment after 1 year of CLE with PC-IOL implantation, Artisan iris-fixated IOL implantation and Nd:YAG laser capsulotomy was shown in Figure 1. The ultrasound biomicroscopy of anterior segment after different refractive surgeries was shown in Figure 2.
Table 1. The clinical data before and after clear lens extraction with posterior chamber-intraocular lens implantation and Artisan iris-fixated intraocular lens implantation.
| Time | Eye | UCVA | BSCVA | Refraction (D) | ACD (mm) | IOP (mmHg) | ECD (/mm2) | CCT (µm) | WTW (mm) | AXL (mm) | Slit-lamp Microscopy |
| Before CLE+PC-IOL | OD | 20/200 | 20/50 | +17.75DS-1.50DC×168° | 2.66 | 14.0 | 2624 | 554 | 11.7 | 16.16 | Shallow anterior chamber |
| OS | 20/200 | 20/50 | +17.25DS-0.75DC×8° | 2.55 | 15.0 | 2921 | 550 | 11.7 | 16.20 | Shallow anterior chamber | |
| 1 month after CLE+PC-IOL before iris-fixated IOL implantation | OD | 20/200 | 20/50 | +12.50DS -0.75DC×166° | 4.01 | 16.7 | 2564 | 575 | Iris depigmentation | ||
| OS | 20/100 | 20/50 | +11.00DS -0.50DC×10° | 3.98 | 18.0 | 2785 | 562 | ||||
| 1 week after CLE+PC-IOL and iris-fixated IOL implantation | OD | 20/100 | 20/50 | +1.25DS -1.50DC×9° | 2.87 | 15.0 | 2415 | 561 | Oval pupilIris depigmentation | ||
| OS | 20/70 | 20/50 | +1.00DS | 2.91 | 14.3 | 2770 | 555 | ||||
| 1 month after CLE+PC-IOL and iris-fixated IOL implantation | OD | 20/70 | 20/50 | +1.50DS -1.00DC×10° | 2.80 | 13.5 | 2561 | 562 | Oval pupilIris depigmentation | ||
| OS | 20/70 | 20/50 | +1.25DS -0.75DC×45° | 2.85 | 15.0 | 2720 | 558 | ||||
| 3 months after CLE+PC-IOL and iris-fixated IOL implantation before Nd:YAG capsulotomy | OD | 20/200 | 20/100 | +1.25DS -1.00DC×5° | 2.88 | 14.7 | 2487 | 549 | Oval pupilIris depigmentation PCO | ||
| OS | 20/100 | 20/70 | +1.50DS -1.50DC×50° | 2.96 | 16.3 | 2692 | 552 | PCO | |||
| 3¼ months after CLE + PC-IOL, iris-fixated IOL implantation, and 1 week after Nd:YAG capsulotomy | OD | 20/70 | 20/50 | +1.50DS -0.50DC×15° | 2.84 | 15.5 | 2358 | 565 | Oval pupilIris depigmentation | ||
| OS | 20/70 | 20/50 | +1.50DS -1.00DC×60° | 2.90 | 13.0 | 2690 | 558 | ||||
| 12 months after CLE + PC-IOL, iris-fixated IOL implantation, and 9 months after Nd:YAG capsulotomy | OD | 20/70 | 20/50 | +1.25DS -0.75DC×13° | 2.83 | 15.7 | 2392 | 560 | 11.7 | 16.17 | Oval pupilIris depigmentation |
| OS | 20/70 | 20/50 | +1.50DS -1.00DC×55° | 2.87 | 12.7 | 2723 | 564 | 11.7 | 16.20 |
UCVA: uncorrected visual acuity; BSCVA: best-spectacle corrected visual acuity; ACD: anterior chamber depth; IOP: intraocular pressure; ECD: endothelial cell density; CCT: central corneal thickness; WTW: white-to-white; AXL: axial length; CLE: clear lens extraction; PC-IOL: posterior chamber-intraocular lens
Figure 1. The photography of anterior segment of extreme hyperopia 1 year after CLE combined with PC-IOL implantation, Artisan iris-fixated IOL implantation and Nd:YAG laser capsulotomy.
OD: the photography of anterior segment of the right eye; OS: the photography of anterior segment of the left eye
Figure 2. The ultrasound biomicroscopy of anterior chamber of extreme hyperopia after different refractive surgeries.
A: before CLE combined with PC-IOL implantation; B: after CLE combined with PC-IOL implantation and before Aritsan iris-fixated IOL implantation; C: after CLE combined with PC-IOL implantation, Artisan iris-fixated pIOL implantation and Nd:YAG laser capsulotomy
DISCUSSION
Despite recent remarkable advances in refractive surgery, it is still difficult to correct high hyperopia, especially extreme hyperopia. Corneal refractive procedures, including laser in situ keratomileusis (LASIK), photorefractive keratectomy (PRK), and conductive keratoplasty (CK), are relatively safe and effective for the treatment of low and moderate hyperopia[4],[5], but not for high hyperopia. Intraocular refractive surgeries including pIOL implantation and CLE with PC-IOL implantation can provide effective, predictable and stable visual rehabilitation for high but not yet for extreme hyperopia.
The application of CLE with PC-IOL implantation for extreme hyperopia was limited by the available power of PC-IOL. In this case, the predicted PC-IOL powers calculated by Haigis and Hoffer Q formulae which were relatively accurate in the eyes with short AXL, were both +57.0D bilaterally. Unfortunately, PC-IOL of +34.0D, which is the highest power available in the market, otherwise unavoidable large spherical error will accompany with the higher power, was implanted for the both eyes.
Piggyback PC-IOLs implantation can provide a larger power range when lacking the optional power of a single PC-IOL[6]. However, there were several reports showing the occurrence of interlenticular opacification after piggyback acrylic PC-IOLs implantation[7],[8], which could not be treated with Nd:YAG laser, the most common and effective method to treat PCO. It has also been reported that piggyback PC-IOLs implantation was associated with papillary-blocking glaucoma and pigmentary dispersion syndrome. These problems typically occur as a consequence of fibrosis of the zonular lens complex, which decreases the space in the sulcus and iris capture due to the haptics in the ciliary sulcus[9],[10].
Another technique, pIOL implantation, has been developed to correct moderate and high hyperopia. In general, pIOLs can be classified into anterior chamber iris-fixated pIOL, posterior chamber pIOL and anterior chamber angle-supported pIOL[11]. The Verisyse/Artisan iris-fixated IOL is one kind of pIOLs for the treatment of myopia, hyperopia and astigmatism in both aphakic and phakic eyes. Compared with other kinds of pIOLs, iris-fixated pIOL is considered to reduce the risks of cataract formation in posterior chamber pIOL implantation and injury of anterior chamber angle and endothelium in anterior chamber angle-supported pIOL implantation[12]. Usually, the application of pIOL is limited by the critical range of ACD, especially for moderate and higher hyperopia which is always accompanied with shallow anterior chamber. In order to avoid corneal decompensation, the recommended minimal pre-operative ACD for implantation of an Artisan IOL is 2.8mm for the type 203 (design for phakia) and 3.3mm for the type 205 (design for aphakia).
In this case report, the initial ACD was 2.66mm for the right eye and 2.55mm for the left eye before CLE, which was not adequate to implant any kinds of pIOL. In addition, no individual refractive surgery could fully correct extreme hyperopia. Therefore, a combination of refractive surgeries including CLE with PC-IOL implantation and Artisan iris-fixated/piggyback IOL implantation was developed. We designed a two-stage procedure to evaluate the ACD after CLE, though it may add the risks of infection, hemorrhage and so on. After CLE with PC-IOL implantation, as expected, ACD was increased to 4.01 and 3.78mm for the right and left eye, respectively, which provided an adequate space for an Artisan iris-fixated IOL implantation. Since the power range of the type 203 (+2.0D ∼ +12.0D) was not optional for this case, the only choice of Artisan IOL is the type 205 (+2.0D ∼ +30.0D). After 1 year of Artisan iris-fixated IOL implantation, the ACD was stable with a measurement bias of approximately 1%.
In the past, corneal decompensation was a severe complication for pIOLs with ECD loss[13]. Since the introduction of Artisan iris-fixated pIOL, a clinical trial of United States FDA has shown the safety of ECD with an average endothelial cell loss of 4.8% ± 7.8% over 3 years after surgery[14]. Most studies exhibited an initial endothelial cell loss in the first year, and the loss did not decrease significantly up to 5 years after implantation[15]. In our one-year follow-up after implantation, ECD decrease of 8.8% for the right eye and 6.8% for the left eye was shown. Long-term following up is necessary for safety determination.
Within one-year following up, mild oval pupil and iris depigmentation were observed in the right eye. Unexpected complication, e.g., severe endothelial cells loss, pigment dispersion syndrome, IOL decentration, pupillary blocking glaucoma, intra-lenticular opacification, or chronic iritis, were not observed in the both eyes post-operatively.
We conclude from the one-year follow-up observation that in hyperopic patients, usual procedure is to put a piggy back lens because of shallow ACD in one stage procedure, but if the plan is two stages we have a chance to evaluate the ACD after clear or cataractous lens removal. If it had depth enough, we can put an iris fixated lens. With implanting an iris fixated lens over the in-the-bag-lens, risk of interlenticular opacification of piggyback would be cleared. Long-term following up is necessary to further determine the efficacy and safety of this combinational procedure.
Footnotes
Foundation item: Zhejiang Medical Scientific Research Foundation (No: 2009B075); Zhejiang Science and Technology Department Public Project, China (No: 2010C33085)
REFERENCES
- 1.Barisić A, Dekaris I, Gabrić N, Bohac M, Romac I, Mravicić I, Lazić R. Comparison of diffractive and refractive multifocal intraocular lenses in presbyopia treatment. Coll Antropol. 2008;32(Suppl 2):27–31. [PubMed] [Google Scholar]
- 2.Qasem Q, Kirwan C, O'Keefe M. 5-year prospective follow-up of Artisan phakic intraocular lenses for the correction of myopia, hyperopia and astigmatism. Ophthalmologica. 2010;224(5):283–290. doi: 10.1159/000299179. [DOI] [PubMed] [Google Scholar]
- 3.van der Heijde GL, Rouwen AJ. Optics of intraocular lenses and refractive keratoplasty. Curr Opin Ophthalmol. 1990;1(1):64–68. doi: 10.1097/00055735-199002000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Randleman JB, White AJ, Jr, Lynn MJ, Hu MH, Stulting RD. Incidence, outcomes, and risk factors for retreatment after wavefront- optimized ablations with PRK and LASIK. J Refract Surg. 2009;25(3):273–276. doi: 10.3928/1081597X-20090301-06. [DOI] [PubMed] [Google Scholar]
- 5.Ehrlich JS, Manche EE. Regression of effect over long-term follow-up of conductive keratoplasty to correct mild to moderate hyperopia. J Cataract Refract Surg. 2009;35(9):1591–1596. doi: 10.1016/j.jcrs.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 6.Habot-Wilner Z, Sachs D, Cahane M, Alhalel A, Desatnik H, Schwalb E, Barequet IS. Refractive results with secondary piggyback implantation to correct pseudophakic refractive errors. J Cataract Refract Surg. 2005;31(11):2101–2103. doi: 10.1016/j.jcrs.2005.05.023. [DOI] [PubMed] [Google Scholar]
- 7.Gayton JL, Apple DJ, Peng Q, Visessook N, Sanders V, Werner L, Pandey SK, Escobar-Gomez M, Hoddinott DS, Van Der Karr M. Interlenticular opacification: clinicopathological correlation of a complication of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg. 2000;26(3):330–336. doi: 10.1016/s0886-3350(99)00433-2. [DOI] [PubMed] [Google Scholar]
- 8.Werner L, Apple DJ, Pandey SK, Solomon KD, Snyder ME, Brint SF, Gayton JL, Shugar JK, Trivedi RH, Izak AM. Analysis of elements of interlenticular opacification. Am J Ophthalmol. 2002;133(3):320–326. doi: 10.1016/s0002-9394(01)01405-2. [DOI] [PubMed] [Google Scholar]
- 9.Kim SK, Lanciano RC, Jr, Sulewski ME. Pupillary block glaucoma associated with a secondary piggyback intraocular lens. J Cataract Refract Surg. 2007;33(10):1813–1814. doi: 10.1016/j.jcrs.2007.05.046. [DOI] [PubMed] [Google Scholar]
- 10.Chang WH, Werner L, Fry LL, Johnson JT, Kamae K, Mamalis N. Pigmentary dispersion syndrome with a secondary piggyback 3-piece hydrophobic acrylic lens. Case report with clinicopathological correlation. J Cataract Refract Surg. 2007;33(6):1106–1109. doi: 10.1016/j.jcrs.2007.01.044. [DOI] [PubMed] [Google Scholar]
- 11.Lovisolo CF, Reinstein DZ. Phakic intraocular lenses. Surv Ophthalmol. 2005;50(6):549–587. doi: 10.1016/j.survophthal.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Menezo JL, Peris-Martínez C, Cisneros AL, Martínez-Costa R. Phakic intraocular lenses to correct high myopia: adatomed, Staar, and Artisan. J Cataract Refract Surg. 2004;30(1):33–44. doi: 10.1016/j.jcrs.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 13.Mimouni F, Colin J, Koffi V, Bonnet P. Damage to the corneal endothelium from anterior chamber intraocular lenses in phakic myopic eyes. Refract Corneal Surg. 1991;7(4):277–281. [PubMed] [Google Scholar]
- 14.Stulting RD, John ME, Maloney RK, Assil KK, Arrowsmith PN, Thompson VM. U.S. Verisyse Study Group. Three-year results of Artisan/Verisyse phakic intraocular lens implantation. Results of the United States Food and Drug Administration clinical trial. Ophthalmology. 2008;115(3):464–472. doi: 10.1016/j.ophtha.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 15.Qasem Q, Kirwan C, O'Keefe M. 5-year prospective follow-up of Artisan phakic intraocular lenses for the correction of myopia, hyperopia and astigmatism. Ophthalmologica. 2010;224(5):283–290. doi: 10.1159/000299179. [DOI] [PubMed] [Google Scholar]