Abstract
There has been growing evidence of a link between chronic respiratory disease, asthma in particular, and mental disorders among youth. The mechanism for this link remains unknown. Several studies have empirically addressed the question of this pathway, and accumulating results may shed new light on the nature of this association. The goal of the current paper is to provide an integrative summary of the literature to date and to present a new interdisciplinary hypothesis for one possible mechanism explaining the link between asthma and anxiety/depression among youth. This hypothesis posits that comorbid anxiety/depression and nicotine dependence among adults, may be one pathway leading to the comorbidity of asthma and anxiety/depression among youth. We propose this mechanism operates via exposure to environmental tobacco smoke and/or prenatal tobacco use, which confers an increased risk for asthma, and parental anxiety/depression which confers increased risk of anxiety/depression among offspring via familial transmission. We predict that further testing of this hypothesis will help to reveal the largely neglected problem of nicotine dependence especially among women—and the far-reaching impact of this addiction on the health of children.
1.0. Introduction
Anxiety disorders, depression, and asthma are the most common and arguably among the most pressing public health problems among youth in the United States and worldwide. The etiologies of anxiety disorders, depression, and asthma are not known and there are no known cures. Improved insight into their etiologies, including potentially shared etiologies, would ultimately help to significantly reduce impairment and disability over the lifespan of millions of people.
1.1. The problem of asthma among youth
Asthma is a pulmonary inflammatory condition, which most often begins in childhood. The clinical phenomena associated with asthma include paroxysmal wheezing, shortness of breath, and cough that accompanies airway hyperreactivity. Cumulative prevalence of asthma range from 14% in inner city U.S. children 17 or younger (Weiland et al., 2004), 25.9% in British school children aged 12-14 (Anderson et al., 2005), and 9.5% and 10.4% among Italian youth, aged 6-7 and 13-14, respectively (Galassi et al., 2006). Unlike other childhood-onset chronic illnesses (e.g., Type I diabetes mellitus), evidence suggests many cases of childhood asthma could be largely prevented and the course vastly improved. Documented risk factors for childhood-onset asthma include family history of asthma, having allergies, cockroach allergen, exposure to prenatal smoking and exposure to environmental tobacco smoke (Becklake & Ernst, 1997; Sporik et al., 1991).
1.2. The problem of anxiety disorders among youth
Anxiety disorders are the most common mental disorders among youth and adults in the community. Prevalence data on anxiety disorders in the community suggest prevalence rates ranging from 5-13% of youth under 17 (e.g., Costello et al., 1996; Garland et al., 2001). One-year and lifetime prevalence of anxiety disorders has been estimated to be approximately 18.1% and 28.8% among adults, respectively (e.g., Kessler et al., 2005). Onset of anxiety disorders is most common during childhood and early adolescence. Anxiety disorders often persist for decades, and early-onset of anxiety disorder is a strong predictor of subsequent onset of affective and substance use disorders (e.g., Reiger et al., 1998) and of persistent and chronic anxiety disorders across the lifespan (Kendall et al., 2004). Previous data also suggest that childhood anxiety disorders are associated with social and school-related impairment, suicidal ideation, and suicide attempt (Gould et al., 1998; Straus et al., 1987). Epidemiologic studies have found risk factors for anxiety disorders, yet etiologic determinants have not been conclusively identified.
1.3. The problem of depression among youth
Large-scale population research has indicated that, at any given time, 10-15% of children and adolescents in the United States suffer from depression or a similar serious mental disorder that affects mood, energy, interest, sleep, and overall functioning (Smucker et al., 1986; US DHHS, 1999). The symptoms of depression are persistent, can interfere with one’s ability to function on a daily basis, and may be chronic. Epidemiologic and clinical research have documented that the age of first onset of major depression is commonly during adolescence, and prepubertal onsets, though less frequent, do occur (Lewinsohn et al., 1994).
1.4. The asthma epidemic in children
Available data from various population samples within the US and other countries suggest that childhood asthma has increased up to six fold in some areas from 1950 to the present time (e.g., Kabesh & Von Mutius, 2002; Wood, 2002), though the reason for the rise in childhood asthma remains unknown. Previous studies also suggest that the prevalence of asthma varies widely by geographic and demographic characteristics.
Population-level genetic changes cannot explain the recent asthma epidemic, as a population’s gene pool takes a much longer period of time to exhibit such changes. Currently, the Hygiene Hypothesis is the main theory that purports to explain this phenomenon, positing that increasingly sanitized conditions in Westernized countries have resulted in changes to individuals’ immune systems, which have increased the risk of allergies and thereby led to the rise of asthma in industrialized (i.e., more sanitized) countries as compared to third-world countries (Stratchan, 1989). Thus, under the Hygiene Hypothesis, asthma is characterized as a disease of the affluent. Skepticism about the usefulness of this hypothesis is increasing though, as it fails to explain some of the recent trends in asthma. Most importantly, the Hygiene Hypothesis is unable to explain the epidemiology of childhood asthma in Westernized countries where rates are substantially higher in inner-city, lower socioeconomic segments of the population compared to suburban, rural, and more affluent segments of the population (e.g., Akinbami et al. 2005; Beckett et al. 1996). A goal of the current study is to propose one alternative hypothesis to partially explain the epidemic of childhood asthma.
1.5. Association between asthma and mental health problems among youth
Evidence to date suggesting an association between asthma and mental disorders among youth has come mainly from four sources. First, data from clinical samples show higher levels of behavioral problems, as well as depression and anxiety symptoms, in pediatric asthma patients with moderate-to-severe asthma compared to controls and pediatric patients with other medical illnesses (e.g., Feldman et al., 2006; Fritz et al., 1987; Wamboldt, et al., 1998). Similarly, data from pediatric patients in psychiatric treatment settings show higher than expected levels of asthma among youth with anxiety disorders (e.g., Koltek et al. 1998; McQuaid et al., 2001). A second line of evidence comes from epidemiologic data which have shown an association between asthma and anxiety disorders among youth in community samples (e.g., Goodwin et al., 2003; Ortega et al., 2002). Specifically, several studies have found higher rates of anxiety disorders (e.g., separation anxiety disorder, overanxious disorder, phobia, panic) among youth with asthma in community samples compared to those with diabetes and other chronic illnesses (e.g, Ortega et al., 2002) and compared with those without asthma (e.g., Craske et al., 2001; Goodwin et al., 2004a). Findings on the link between respiratory disease and depression among youth in the community have been mixed, with some showing a link (Ortega et al., 2004), while others do not (Vila et al., 2000). Third, there is evidence of a familial association between panic disorder and respiratory disease, with data showing higher than expected rates of panic disorder among relatives of patients with severe respiratory disease (van Beek et al., 2005), as well as evidence of a relationship between severity of psychiatric problems in family members and severity of asthma in pediatric patients (Gorman et al., 2001). Results from a three-generation study show parental depression is associated with increased risk of respiratory disease in offspring (Goodwin et al, 2007a). Fourth, a number of studies have shown longitudinal associations between asthma and panic attacks among adults over several year time-intervals (Goodwin et al., 2004a; Hasler et al., 2005).
1.6. Respiratory function and anxiety
In a parallel line of research, there is mounting evidence of a link between respiratory abnormalities and anxiety disorders in youth and adults. Specifically, laboratory studies have provided evidence that youth with anxiety disorders have higher sensitivity to CO2 inhalation, compared with youth without mental disorders (e.g., Pine et al., 2000; Pine et al., 2005). In comparison to adults without mental disorders, similar studies have also shown in adults that specific anxiety disorders (e.g., panic disorder) are associated with increased sensitivity to CO2 and that this sensitivity is specific to anxiety since depression is not associated with heightened CO2 sensitivity (e.g., Gorman et al., 2001; Martinez et al., 2001). These results cumulatively support the hypothesis that there may be a shared vulnerability to respiratory abnormalities associated with anxiety disorders and respiratory disease.
2.0. Mechanism of the association between asthma and mental disorders in children
Despite consistent results suggesting a link between respiratory conditions and mental disorders in youth, the mechanism of the association between asthma and mental disorders remains unclear. There are three main possible explanations this link.
2.1. Childhood mental health problems cause the onset of asthma
Longitudinal evidence to date, which may provide clues as to the likelihood of whether or not there is a causal relationship between asthma and mental disorders has not falsified this possible pathway, though the majority of evidence does not support a causal link. For instance, one recent study found that behavioral abnormalities in the first years of life were associated with the subsequent onset of asthma (Calam et al., 2005), yet another longitudinal study of youth found no link between respiratory symptoms at age 5 and risk of mental health problems at age 14 (Alati et al., 2005). Therefore, it is not necessarily the case that this is a causal link—and a biological mechanism through which a causal link would exist is not clear.
2.2. Asthma causes the onset of mental health problems
One study found a link between early respiratory symptoms and increased risk of any mental disorder among adolescents (Goodwin et al., 2004b), though asthma was not measured in this study and data on respiratory symptoms were obtained via self-report. Another longitudinal study examining the relationship between asthma in adolescence and the risk of anxiety disorders in young adulthood found that respiratory problems at age 15 were associated with increased risk of anxiety disorders at age 18-21 (Craske et al., 2001). Among adults, two studies have found longitudinal links between asthma and mental health problems. One illustrated a link between asthma and the onset of panic attacks one year later (Goodwin & Eaton, 2003), while a second longitudinal study found that asthma was associated with panic disorder (Hasler et al., 2005). These studies are temporally consistent with a potential mechanism whereby asthma could cause anxiety/depression, though these studies did not adjust for key potentially confounding/mediating factors, and it is not clear what the specific causal biological mechanisms would be in this pathway.
2.3. Common risk factors and the comorbidity of asthma and mental disorders
To the best of our knowledge, only one study to date has examined the possible mechanism of the observed link between asthma and mental health problems in youth; this study found that this link was not causal, but was explained by confounding/mediating risk factors for both asthma and mental health problems (Goodwin et al., 2004b). Yet, the study was not able to identify what those risk factors were because a limited number of risk factors were included in the analysis and a limited number of psychosocial and psychological factors were measured in the survey.
3.0. Hypothesis
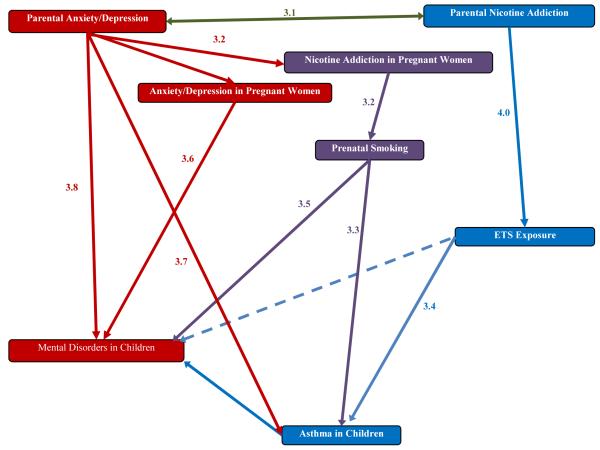
In this paper, we present a new theory explaining one possible mechanism for the observed association between asthma and mental disorders among youth (See Figure 3). Specifically, we hypothesize that the comorbidity of asthma and mental disorders is due to common exposure factors of parental mental disorders and addiction, yet the pathway through which each of these risk factors affects the outcomes differs. We propose that increased risk of asthma among offspring of parents with nicotine dependence is due to increased exposure to prenatal and postnatal tobacco smoke, while the increased risk of mental disorders in offspring of parents with mental disorders and offspring is via familial/genetic pathway, which has also already been documented in the literature. As such, comorbidity of mental disorders and addictive behaviors in parents is one possible mechanism that may explain the comorbidity of asthma and mental disorders in youth.
Figure 3.
3.1. Association between anxiety/depression and nicotine addiction
There is abundant evidence to date showing high rates of smoking among adults with anxiety/depression. Several population-based studies have shown cross-sectional associations between mental disorders and increased rates of cigarette use and nicotine dependence among adults (e.g., Grant et al., 2004a; Grant, et al., 2004b). Evidence from longitudinal studies has also suggested that depression and anxiety disorders are associated with increased risk of the initiation of cigarette smoking and nicotine dependence (e.g., Breslau et al., 2004; Goodwin & Hamilton 2002), as well as the reverse (Isensee et al., 2003). Finally, clinical research has shown that mental disorders are associated with higher levels of withdrawal symptoms during attempts to quit smoking and that smokers with a mental disorder also exhibit lower quit rates compared with smokers without mental disorders (e.g., Covey, 1999; Glassman et al., 1990). In sum, evidence to date suggests that cigarette smoking and nicotine dependence are common among a majority of adults with anxiety/depressive disorders and that having anxiety/depressive disorders appears to significantly hinder both efforts to stop smoking and effectiveness of treatment for nicotine dependence.
3.2. Association between anxiety/depression and nicotine addiction among pregnant women
A growing number of studies have documented a relationship between anxiety/depression and higher levels of cigarette use and nicotine dependence among pregnant women. Specifically, a recent population-based study (Goodwin et al., 2007a), showed that 21.7% of pregnant women in the United States reported using cigarettes during their pregnancy. Comparison of the prevalence of mental disorders among pregnant women who did and those who did not use cigarettes showed that pregnant women who used cigarettes were significantly more likely to have any Axis I mental disorder (OR = 1.64, 95% CI: 1.03–2.62) and any personality disorder (OR = 1.98, 95% CI: 1.1–3.48). In sum, while it is commonly thought that smoking during pregnancy is rare, evidence suggests that it is quite common among women in various segments of the population especially, it appears, among women with anxiety/depressive disorders.
3.3. Association between prenatal smoking and asthma in children
Prenatal smoking is known to be associated with a wide range of ill effects on health of the infant, such as low birth weight, low rate of fetal growth, asthma, upper respiratory infections preterm delivery, and sudden infant death syndrome (SIDS) (e.g., Kramer, 1987). Several studies have shown consistent associations between exposure to prenatal smoking and increased risk of asthma onset in infants and young children (e.g., US DHHS, 2006). In effect, exposure to prenatal smoking is one of few documented risk factors for the onset of asthma in infancy and childhood.
3.4. Association between exposure to Environmental Tobacco Smoke and risk of asthma in children
Environmental tobacco smoke (ETS) is a known risk factor for childhood asthma onset, as well as for numerous other health conditions in infants and children including SIDS, early respiratory infections, otitis media, and other health problems (e.g., Becklake & Ernst, 1997; US CDC, 1996). One third of children under the age of seven are exposed to ETS in the home daily (Shushter et al., 2002). Evidence consistently suggests that ETS is both a risk factor for asthma onset and trigger for asthma exacerbation and attacks among youth. Parental ETS in the home is thought to be the most common source of exposure to ETS for youth (e.g., Cook & Strachan, 1997), and its effect appears to be dose dependent as symptom prevalence in asthmatic children has been shown to increase with the number of parents that smoke (Cook & Strachan, 1997). In particular, an association has been shown to exist between prenatal exposure to ETS and an increased risk of childhood asthma and wheezing (OR = 1.87, 95% CI: 1.25-2.81) (Ehrlich et al., 1996). Prenatal ETS exposure has been shown to work independently of postnatal ETS exposure, as prenatal exposure appears to be a specific risk factor for asthma, whereas postnatal exposure is associated with a range of other respiratory symptoms (Pattenden et al., 2006). Self report and urine continine levels indicate that maternal smoking is closely linked with asthma and asthma severity in children, while the association between paternal smoking and childhood asthma is harder to detect, presumably due to proximity (DiFranza et al., 2004). Regardless, studies suggest that 26% of children who report ETS as a trigger for asthma symptoms or attacks have at least one parent who smokes (DiFranza et al., 2004; Gergen et al., 1988; Nardini, et al., 2001).
3.5. Association between exposure to prenatal smoking and mental disorders in children
Numerous studies have documented a link between prenatal smoking and mental disorders in children. Prenatal smoking has been associated with ADHD, conduct disorder, and depression among children in several studies (e.g., Fergusson et al., 1998; Indredavik et al., 2007). The relationship between adolescent psychopathology and number of cigarettes smoked prenatally per day appears to be linear, with an increased number of cigarettes per day being associated with an increased rate of DSM-IV symptom criteria in adolescents, though some of this relationship may be due to confounding and selection factors (Fergusson et al., 1998). In sum, there appears to be a link between prenatal smoking and mental disorders in children.
3.6. Association between exposure to environmental tobacco smoke and mental disorders in children
There is growing evidence that maternal prenatal anxiety/depression may be associated with impact on behavioral and emotional problems during childhood (Correia & Linhares, 2007; O’Connor et al., 2002a; O’Connor et al., 2002b; O’Connor et al., 2003), perhaps by altering the hypothalamic-pituitary-adrenal axis (Davis et al., 2007; O’Connor et al., 2005). A number of preclinical studies have also found consistent results (Henry et al., 1994; Thompson, 1957; Weinstock, 1997). Further research will be needed, it seems, in order to distinguish a specific prenatal/intrauterine mechanism for this pathway from a genetic or other familial transmission pathway.
3.7. Association between maternal/parental depression/anxiety disorders and the risk of asthma in children
Evidence to date suggests an association between parental mental health problems and increased risk of asthma onset in children (e.g., Goodwin et al., 2007b; Klinnert et al., 2001; Ortega et al., 2004), increased severity of asthma in youth (e.g., Ackakaya et al., 2003; Mrazek et al., 1987) and poorer asthma management (Frankel et al., 1998) including increased health service use and ER use (Bosley et al, 1966; Shalowitz et al., 2000). There is mounting evidence of a relationship between parental mental disorders and increased risk of asthma in children.
3.8. Association between maternal/parental/family history of anxiety/depression and risk of mental disorders in children
Numerous studies have shown linkages between parental psychopathology and increased risk of mental disorders in children (e.g., Black et al., 1992; Fyer et al., 1990; Weissman, 1993). For instance, one family study showed that when compared with children of parents without a psychiatric diagnosis, children whose parents suffered from an anxiety disorder were more than 7 times more likely to meet criteria for an anxiety disorder (Turner et al., 1987). Parental depression and substance use disorders are also shown to be associated with increased risk of anxiety disorders in children, as well as depression, and externalizing disorders. In sum, the familial risk of anxiety and depressive disorders to offspring has been fairly well documented.
4.0 Summary
To our knowledge, this hypothesis is the first to attempt to explain the mechanism of this observed link and this review indicates that there is available evidence supporting each step of the pathway. It also reflects a novel conceptualization of what is commonly considered in explaining the comorbidity of a mental and physical disorder. Using evidence from a range of previous studies in these areas, the weight of evidence in this paper seems to support the feasibility of this pathway.
Addictive disorders have historically been studied in terms of the health consequences to the individual, which clearly include both negative physical and mental health outcomes as well as economic. In particular with cigarette use/nicotine dependence, there is abundant evidence that addiction to cigarettes and/or nicotine in another form has deleterious health effects (US DHHS, 2004). That maternal nicotine addiction increases the risk of addictive disorders in offspring is also increasingly documented (Buka et al., 2003; Niaura et al., 2001). Yet, the possibility that nicotine addiction may negatively impact the physical health of offspring via an intermediary environmental mechanism (i.e., exposure to ETS) has not been studied in this context, nor within the field of addiction and/or mental health. There is abundant data documenting the biological pathway through which ETS affects children’s respiratory health in the pediatrics and respiratory literature (e.g., Becklake & Ernst, 1997; Burchfield et al., 1996; US CDC, 1997), as well as evidence of a link between maternal smoking and asthma in youth (Burchfield et al., 1996). What seems to have been missing in this literature is the potentially critical role of mental health and addiction in the perpetuation of this intergenerational problem. While it is known that ETS has detrimental effects on the health of children, household smoking rates remain high (US CDC, 1996) and the nicotine dependence in a parent is not widely regarded as a condition that may possibly endanger or increase the risk of chronic exposure to an array of dangerous chemicals to the child, especially early in life when often most time is spent indoors in the home. As such, it is increasingly clear that an integration of literatures from multiple disciplines, including psychiatry, addictions, medicine, epidemiology, and environmental health science, is needed in order to tell the complete story of what is happening in these complex chronic conditions where research to date in single disciplines have been unable to identify a cause.
4.1. Novel mechanism of transmission
Mother-to-child disease transmission is commonly thought to be within the sphere of infectious disease. What we have proposed here is that the psychiatric disease (i.e., nicotine dependence) in the mother is a risk factor for respiratory disease (i.e., childhood asthma) in the child via exposure to ETS, which is a direct result of the psychiatric disease. Within asthma research, ETS is considered an environmental risk factor. It is not generally examined from a psychiatric perspective, although it is the product of a mental disorder or addiction and appears as if not more difficult to treat as any other addiction (e.g., cocaine). As our theory suggests, parental nicotine dependence not only transmits increased risk of nicotine dependence to offspring, but also the risk of physical disease to the offspring through increased exposure and a known and well-documented environmental pathway.
It should be noted, as well, that there may potentially be numerous confounding factors associated with higher rates of both asthma and mental disorders among youth. It will be important to understand the possible confounding and/or mediating role of factors such as SES and geographic residence (e.g., urban vs. rural), as they may influence the exposure pathway. Although such factors may mediate or moderate the levels of exposure to the risk factors proposed here (e.g., small living quarters may increase level of exposure to ETS), it does not seem possible that they could replace this hypothesized pathway as these factors are not sufficient causes in themselves for the onset of asthma, based on available evidence to date.
4.2. Proposed Hypothesis and the Epidemic of Childhood Asthma
As noted earlier, the reason for the epidemic of childhood asthma is unknown, and the Hygiene Hypothesis (Strachan, 1989) has been increasingly questioned in recent years in terms of whether this theory can explain the modern epidemic given the geographic patterns and discrepancies which seem counter to this original hypothesis. We hypothesize that the ETS-mediation theory outlined in this paper provides one alternative, plausible hypothesis explaining the epidemic of asthma in children over the past several decades. In-depth discussion of the hypothesis in relation to the asthma epidemic is not possible here due to space constraints, but in brief, we have posited that the asthma epidemic in children may be due, in part, to a parallel increase in cigarette use – especially among women over the past several decades and, therefore, substantially increased early exposure to ETS, compared with earlier decades (see Goodwin et al., 2007a for more detailed write up).
4.3. Clinical and Public Health Implications
If evidence continues to support this link, there are substantial clinical and public health implications of this hypothesis. First, it seems clear that programs for smoking cessation in pregnant women would be more effective if a mental health component is included. In addition, while there is clearly a multitude of clinical and public health campaigns aimed at reducing childhood exposure to ETS in the home, programs aimed at promoting smoking cessation do not generally address either the issue of nicotine dependence or the possibility that comorbid depression/anxiety disorders are inhibiting quit efforts. Public health poster campaigns and the like are important in terms of educating people about the risks to their children, yet, the lack of success in reaching goal quit levels (e.g., Healthy People 2010), or in eliminating household smoking from homes with children (Ashley & Ferrence, 1998; Gergen et al., 1998), may be related to the fact that these addictions are not addressed or recognized as clinical disorders nor given the treatment required. Similar efforts should be made to extend treatment for nicotine dependence as have been made for the treatment of illicit substance dependence (Sees et al., 1990).
Future studies that can prospectively investigate the specific independent contributors of each of these factors in large, population-based multidisciplinary studies are needed so that the size,possible interaction, and impact of these various factors can be more fully understood. Further testing of this theoretical model will open up new opportunities for its application to other diseases, especially to the chronic diseases affecting youth in the United States, the majority of which appear to have behavioral components.
Figure 1.
Figure 2.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akinbami L, Rhodes J, Lara M. Racial and ethnic differences in asthma diagnosis among children who wheeze. Pediatrics. 2005;115:1254–1260. doi: 10.1542/peds.2004-0897. [DOI] [PubMed] [Google Scholar]
- Alati R, O’Callaghan M, Najman JM, Williams GM, Bor W, Lawlor DA. Asthma and internalizing behavior problems in adolescence: a longitudinal study. Psychosomatic Medicine. 2005;67:462–70. doi: 10.1097/01.psy.0000161524.37575.42. [DOI] [PubMed] [Google Scholar]
- Anderson HR, Ruggles R, Strachan DP, Austin JB, Burr M, Jeffs D, Standring P, Steriu A, Goulding R. Trends in prevalence of symptoms of asthma, hay fever, and eczema in 12-14 year olds in the British Isles, 1995-2002: a questionnaire survey. British Medical Journal. 2004;328:1052–3. doi: 10.1136/bmj.38057.583727.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashley MJ, Ferrence R. Reducing children’s exposure to environmental tobacco smoke in homes: issues and strategies. Tobacco Control. 1998;7:61–65. doi: 10.1136/tc.7.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett W, Belanger K, Gent JF, Holford TR, Leaderer BP. Asthma among Puerto Rican Hispanics: a multi-ethnic comparison study of risk factors. American Journal of Respiratory and Critical Care Medicine. 1996;154:894–899. doi: 10.1164/ajrccm.154.4.8887582. [DOI] [PubMed] [Google Scholar]
- Becklake MR, Ernst P. Asthma: Environmental Factors. Lancet. 1997;350:10–3. doi: 10.1016/s0140-6736(97)90030-1. [DOI] [PubMed] [Google Scholar]
- Black DB, Noyes R, Goldstein RB, Blum N. A family study of obsessive-compulsive disorder. Archives of General Psychiatry. 1992;49:362–368. doi: 10.1001/archpsyc.1992.01820050026004. [DOI] [PubMed] [Google Scholar]
- Bosley C, Corden Z, Cochrane G. Psychosocial factors and asthma. Respiratory Medicine. 1966;90:453–7. doi: 10.1016/s0954-6111(96)90170-5. [DOI] [PubMed] [Google Scholar]
- Breslau N, Novak SP, Kessler RC. Psychiatric disorders and stages of smoking. Biological Psychiatry. 2004;55:69–76. doi: 10.1016/s0006-3223(03)00317-2. [DOI] [PubMed] [Google Scholar]
- Buka SL, Shenassa ED, Niaura R. Elevated risk of tobacco dependence among offspring of mothers who smoked during pregnancy: a 30-year prospective study. American Journal of Psychiatry. 2003;160:1978–84. doi: 10.1176/appi.ajp.160.11.1978. [DOI] [PubMed] [Google Scholar]
- Burchfield CM, Higgins MW, Keller JB, Howatt WF, Butler WJ, Higgins ITT. Passive smoking in childhood: respiratory conditions and pulmonary function in Tecumseh, Michigan. The American Review of Respiratory Disease. 1986;133:966–973. doi: 10.1164/arrd.1986.133.6.966. [DOI] [PubMed] [Google Scholar]
- Calam R, Gregg L, Simpson A, Simpson B, Woodcock A, Custovic A. Behavior problems antecede the development of wheeze in childhood: a birth cohort study. American Journal of Respiratory and Critical Care Medicine. 2005;171:323–7. doi: 10.1164/rccm.200406-791OC. [DOI] [PubMed] [Google Scholar]
- Cook DG, Strachan DP. Health effects of passive smoking. 3. Parental smoking and prevalence of respiratory symptoms and asthma in school age children. Thorax. 1997;52:1081–1094. doi: 10.1136/thx.52.12.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correia LL, Linhares MB. Maternal anxiety in the pre- and postnatal period: a literature review. Revisita Latino-Americana de Enfermagem. 2007;15:677–83. doi: 10.1590/s0104-11692007000400024. 2007. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The great smoky mountains study of youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Covey LS. Tobacco cessation among patients with depression. Primary Care. 1999;26:691–706. doi: 10.1016/s0095-4543(05)70124-x. [DOI] [PubMed] [Google Scholar]
- Craske MG, Poulton R, Tsao JC, Plotkin D. Paths to panic disorder/agoraphobia: an exploratory analysis from age 3 to 21 in an unselected birth cohort. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:556–563. doi: 10.1097/00004583-200105000-00015. [DOI] [PubMed] [Google Scholar]
- Davis EP, Glynn LM, Schetter CD, Hobel C, Chicz-Demet A, Sandman CA. Prenatal exposure to maternal depression and cortisol influences infant temperament. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:737–46. doi: 10.1097/chi.0b013e318047b775. [DOI] [PubMed] [Google Scholar]
- DiFranza J, Aligne C, Weitzman M. Prenatal and postnatal environmental tobacco smoke exposure and children’s health. Pediatrics. 2004;113:1007–15. [PubMed] [Google Scholar]
- Ehrlich RI, Du Toit D, Jordaan E, Zwarenstein M, Potter P, Volmink JA, Weinberg E. Risk factors for childhood asthma and wheezing. Importance of maternal and household smoking. American Journal of Respiratory and Critical Care Medicine. 1996;154:681–8. doi: 10.1164/ajrccm.154.3.8810605. [DOI] [PubMed] [Google Scholar]
- Feldman JM, Ortega AN, McQuaid EL, Canino G. Comorbidity between asthma attacks and internalizing disorders among Puerto Rican Children at one-year follow-up. Psychosomatics. 2006;47:333–339. doi: 10.1176/appi.psy.47.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ, Horwood LJ. Maternal smoking during pregnancy and psychiatric adjustment in late adolescence. Archives of General Psychiatry. 1998;55:721–727. doi: 10.1001/archpsyc.55.8.721. [DOI] [PubMed] [Google Scholar]
- Frankel K, Wamboldt M. Chronic childhood illness and maternal mental health - why should we care? Journal of Asthma. 1998;35:621–30. doi: 10.3109/02770909809048964. [DOI] [PubMed] [Google Scholar]
- Fritz GK, Rubinstein S, Lewiston NJ. Psychological factors in fatal childhood asthma. American Journal of Orthopsychiatry. 1987;57:253–257. doi: 10.1111/j.1939-0025.1987.tb03535.x. [DOI] [PubMed] [Google Scholar]
- Fyer AJ, Mannuzza S, Gallops MS, Martin LY, Aaronson C, Gorman JM, Liebowitz MR, Klein DF. Familial transmission of simple phobias and fears: a preliminary report. Archives of General Psychiatry. 1990;47:252–256. doi: 10.1001/archpsyc.1990.01810150052009. [DOI] [PubMed] [Google Scholar]
- Galassi C, De Sario M, Biggeri A, Bisanti L, Chellini E, Ciccone G, Petronio MG, Piffer S, Sestini P, Rusconi F, Viegi G, Forastiere F. Changes in prevalence of asthma and allergies among children and adolescents in Italy, 1994-2002. Pediatrics. 2006;117:34–42. doi: 10.1542/peds.2004-2709. [DOI] [PubMed] [Google Scholar]
- Garland AF, Hough RL, McCabe KM, Yeh M, Wood P, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. Journal of American Academy of Child and Adolescent Psychiatry. 2001;40:409–18. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Gergen PJ, Fowler JA, Maurer KR, Davis WW, Overpeck MD. The burden of environmental tobacco smoke exposure on the respiratory health of children 2 months through 5 years of age in the United States: Third National Health and Nutrition Examination Survey, 1988 to 1994. Pediatrics. 1998;101:E8. doi: 10.1542/peds.101.2.e8. [DOI] [PubMed] [Google Scholar]
- Gergen PJ, Mullally D, Evans R. National survey of prevalence of asthma among children in the United States, 1976-1980. Pediatrics. 1988;81:1–7. [PubMed] [Google Scholar]
- Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, Johnson J. Smoking, smoking cessation, and major depression. The Journal of the American Medical Association. 1990;264:1546–9. [PubMed] [Google Scholar]
- Goodwin RD, Eaton WW. Asthma and the risk of panic attacks among adults in the community. Psychological Medicine. 2003;33:879–85. doi: 10.1017/s0033291703007633. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Fergusson DM, Horwood LJ. Asthma and depressive and anxiety disorders among young persons in the community. Psychological Medicine. 2004a;34:1465–1474. doi: 10.1017/s0033291704002739. [DOI] [PubMed] [Google Scholar]
- Goodwin R, Hamilton S. Cigarette smoking and panic: the role of neuroticism. American Journal of Psychiatry. 2002;159:1208–13. doi: 10.1176/appi.ajp.159.7.1208. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Jacobi F, Thefeld W. Mental disorders and asthma in the community. Archives of General Psychiatry. 2003;60:1125–1130. doi: 10.1001/archpsyc.60.11.1125. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Keyes K, Simuro N. Mental disorders and nicotine dependence among pregnant women in the United States. Obstetrics & Gynecology. 2007a;109:875–883. doi: 10.1097/01.AOG.0000255979.62280.e6. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Lewinsohn PM, Seeley JR. Respiratory symptoms and mental disorders among youth: results from a prospective, longitudinal study. Psychosomatic Medicine. 2004b;66:943–949. doi: 10.1097/01.psy.0000138123.70740.92. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Wickramaratne P, Nomura Y, Weissman MM. Familial depression and respiratory illness in children. Archives of Pediatric and Adolescent Medicine. 2007b;161:487–94. doi: 10.1001/archpedi.161.5.487. [DOI] [PubMed] [Google Scholar]
- Gorman JM, Kent J, Martinez J, Browne S, Coplan J, Papp LA. Physiological changes during carbon dioxide inhalation in patients with panic disorder, major depression, and premenstrual dysphoric disorder: evidence for a central fear mechanism. Archives of General Psychiatry. 2001;58:125–131. doi: 10.1001/archpsyc.58.2.125. [DOI] [PubMed] [Google Scholar]
- Gould MS, King R, Greenwald S, Fisher P, Schwab-Stone M, Kramer R, Flisher AJ, Goodman S, Canino G, Shaffer D. Psychopathology associated with suicidal ideation and attempts among children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:915–923. doi: 10.1097/00004583-199809000-00011. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004a;61:1107–15. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Grant B, Stinson F, Dawson D, Chou S, Dufour M, Compton W, Pickering R, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004b;61:807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hasler G, Gergen P, Kleinbaum V, Gamma A, Eich D, Rossler W, Angst J. Asthma and panic in young adults: A 20-year prospective community study. American Journal of Respiratory and Critical Care Medicine. 2005;171:1224–30. doi: 10.1164/rccm.200412-1669OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry C, Kabbaj M, Simon H, Le Moal M, Maccari S. Prenatal stress increases the hypothalamo-pituitary-adrenal axis response in young and adult rats. Journal of Neuroendocrinology. 1994;6:341–5. doi: 10.1111/j.1365-2826.1994.tb00591.x. [DOI] [PubMed] [Google Scholar]
- Indredavik MS, Brubakk AM, Romundstad P, Vik T. Prenatal smoking exposure and psychiatric symptoms in adolescence. Acta Paediatrica. 2007;96:377–82. doi: 10.1111/j.1651-2227.2006.00148.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isensee B, Wittchen HU, Stein MB, Höfler M, Lieb R. Smoking increases the risk of panic: findings from a prospective community study. Archives of General Psychiatry. 2003;60:692–700. doi: 10.1001/archpsyc.60.7.692. [DOI] [PubMed] [Google Scholar]
- Kabesh M, Von Mutius E, Silverman M. Childhood Asthma and Other Wheezing Disorders. 2nd ed Arnold; London, U.K.: 2002. Epidemiology and public health. [Google Scholar]
- Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: Outcomes in adolescence and impact on substance use and depression at 7.4 year follow up. Journal of Consulting and Clinical Psychology. 2004;72:276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Dembler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Klinnert M, Nelson H, Price M, Adinoff A, Leung D, Mrazek D. Onset and persistence of childhood asthma: Predictors from infancy. Pediatrics. 2001;108:E69. doi: 10.1542/peds.108.4.e69. [DOI] [PubMed] [Google Scholar]
- Koltek M, Wilkes TC, Atkinson M. The prevalence of posttraumatic stress disorder in an adolescent inpatient unit. Canadian Journal of Psychiatry. 1998;43:64–68. doi: 10.1177/070674379804300107. [DOI] [PubMed] [Google Scholar]
- Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bulletin of the World Health Organization. 1987;65:663–737. [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Clark GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duriation, and time to recurrence. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Martinez JM, Kent JM, Coplan JD, Browne ST, Papp LA, Sullivan GM, Kleber M, Perepletchikova F, Fyer AJ, Klein DF, Gorman JM. Respiratory variability in panic disorder. Depression and Anxiety. 2001;14:232–237. doi: 10.1002/da.1072. [DOI] [PubMed] [Google Scholar]
- McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. Journal of Developmental and Behavioral Pediatrics. 2001;22:430–439. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- Mrazek D, Miller B. The pediatric-patient with severe asthma and psychiatric-illness - diagnostic and therapeutic considerations. Seminars in Respiratory Medicine. 1987;8:347–52. [Google Scholar]
- Nardini S, Castellani P, Carrozzi L. Smoking cessation as a therapeutic and preventive intervention: a meeting report. Monaldi Archives for Chest Disease. 2001;56:540–4. [PubMed] [Google Scholar]
- Niaura R, Bock B, Lloyd EE, Brown R, Lipsitt LP, Buka S. Maternal transmission of nicotine dependence: psychiatric, neurocognitive and prenatal factors. American Journal of Addiction. 2001;10:16–29. doi: 10.1080/105504901750160420. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Ben-Shlomo Y, Heron J, Golding J, Adams D, Glover V. Prenatal anxiety predicts individual differences in cortisol in pre-adolescent children. Biological Psychiatry. 2005;58:211–7. doi: 10.1016/j.biopsych.2005.03.032. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Heron J, Glover V, Alspac Study Team Antenatal anxiety predicts child behavioral/emotional problems independently of postnatal depression. Journal of the American Academy of Child & Adolescent Psychiatry. 2002a;41:1470–7. doi: 10.1097/00004583-200212000-00019. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children’s behavioural/emotional problems at 4 years. Report from the Avon Longitudinal Study of Parents and Children. British Journal of Psychiatry. 2002b;180:502–8. doi: 10.1192/bjp.180.6.502. [DOI] [PubMed] [Google Scholar]
- O’Connor TG, Heron J, Golding J, Glover V, ALSPAC Study Team Maternal antenatal anxiety and behavioural/emotional problems in children: a test of a programming hypothesis. Journal of Child Psychology and Psychiatry. 2003;44:1025–36. doi: 10.1111/1469-7610.00187. [DOI] [PubMed] [Google Scholar]
- Ortega AN, Huertas SE, Canino G, Ramirez R, Rubio-Stipec M. Childhood asthma, chronic illness, and psychiatric disorders. Journal of Nervous and Mental Disease. 2002;190:275–281. doi: 10.1097/00005053-200205000-00001. [DOI] [PubMed] [Google Scholar]
- Ortega A, McQuaid E, Canino G, Goodwin R, Fritz G. Comorbidity of asthma and anxiety and depression in Puerto Rican children. Psychosomatics. 2004;45:93–9. doi: 10.1176/appi.psy.45.2.93. [DOI] [PubMed] [Google Scholar]
- Pattenden S, Antova T, Neuberger M, Nikiforov B, De Sario M, Grize L, Heinrich J, Hruba F, Janssen N, Luttmann-Gibson H, Privalova L, Rudnai P, Splichalova A, Zlotkowska R, Fletcher T. Parental smoking and children’s respiratory health: independent effects of prenatal and postnatal exposure. Tobacco Control. 2006;15:294–301. doi: 10.1136/tc.2005.015065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS, Klein RG, Coplan JD, Papp LA, Hoven CW, Martinez J, Kovalenko P, Mandell DJ, Klein DF, Gorman JM. Differential carbon dioxide sensitivity in childhood anxiety disorders and nonill comparison group. Archives of General Psychiatry. 2000;57:960–967. doi: 10.1001/archpsyc.57.10.960. [DOI] [PubMed] [Google Scholar]
- Pine DS, Klein RG, Roberson-Nay R, Mannuzza S, Moulton JL, 3rd, Woldehawariat G, Guardino M. Response to 5% carbon dioxide in children and adolescents: relationship to panic disorder in parents and anxiety disorders in subjects. Archives of General Psychiatry. 2005;62:73–80. doi: 10.1001/archpsyc.62.1.73. [DOI] [PubMed] [Google Scholar]
- Reiger DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. British Journal of Psychiatry Supplement. 1998;34:24–8. [PubMed] [Google Scholar]
- Sees KL. Cigarette smoking, nicotine dependence, and treatment in addiction medicine. The Western Journal of Medicine. 1990;152:578–84. [PMC free article] [PubMed] [Google Scholar]
- Shalowitz M, Berry C, Quinn K, Wolf R. The relationship of life stressors and maternal depression to pediatric asthma morbidity in a subspecialty practice. Ambulatory Pediatrics. 2000;1:185–93. doi: 10.1367/1539-4409(2001)001<0185:trolsa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children’s Depression Inventory. Journal of Abnormal Child Psychology. 1986;14:25–39. doi: 10.1007/BF00917219. [DOI] [PubMed] [Google Scholar]
- Sporik R, Holgate ST, Cogswell JJ. Natural history of asthma in childhood: a birth cohort study. Archives of Disorders in Childhood. 1991;66:1050–1053. doi: 10.1136/adc.66.9.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson WR. Influence of Prenatal Maternal Anxiety on Emotionality in Young Rats. Science. 1957;125:698–699. doi: 10.1126/science.125.3250.698. [DOI] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Costello A. Psychopathology in the offspring of anxiety disorders patients. Journal of Consulting and Clinical Psychology. 1987;55:229–235. doi: 10.1037//0022-006x.55.2.229. [DOI] [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention (US CDC) State-Specific Prevalence of Cigarette Smoking Among Adults, and Children’s and Adolescent’s Exposure to Environmental Tobacco Smoke—United States 1996. Morbidity and Mortality Weekly Report. 1996;46:1038–1043. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (US DHHS) Mental Health: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 1999. [Google Scholar]
- U.S. Department of Health and Human Services (US DHHS) The health consequences of smoking: a report of the Surgeon General. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Washington, D.C.: 2004. [Google Scholar]
- U.S. Department of Health and Human Services (US DHHS) The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2006. [Google Scholar]
- Vila G, Nollet-Clemencon C, de Blic J, Mouren-Simeoni MC, Scheinmann P. Prevalence of DSM IV anxiety and affective disorders in a pediatric population of asthmatic children and adolescents. Journal of Affective Disorders. 2000;58:223–233. doi: 10.1016/s0165-0327(99)00110-x. [DOI] [PubMed] [Google Scholar]
- van Beek N, Schruers KR, Griez EJ. Prevalence of respiratory disorders in first-degree relatives of panic disorder patients. Journal of Affective Disorders. 2005;87:337–340. doi: 10.1016/j.jad.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Wamboldt MZ, Fritz G, Mansell A, McQuaid EL, Klein RB. Relationship of asthma severity and psychological problems in children. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:943–950. doi: 10.1097/00004583-199809000-00014. [DOI] [PubMed] [Google Scholar]
- Weiland SK, Bjorksten B, Brunekreef B, Cookson WO, von Mutius E, Strachan DP. Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): rationale and methods. The European Respiratory Journal. 2004;24:406–12. doi: 10.1183/09031936.04.00090303. [DOI] [PubMed] [Google Scholar]
- Weissman MM. Family genetic studies of panic disorder. Journal of Psychiatric Reseach. 1993;27:69–78. doi: 10.1016/0022-3956(93)90018-w. [DOI] [PubMed] [Google Scholar]
- Weinstock M. Does prenatal stress impair coping and regulation of hypothalamic-pituitary-adrenal axis? Neuroscience and Biobehavioral Reviews. 1997;21:1–10. doi: 10.1016/s0149-7634(96)00014-0. [DOI] [PubMed] [Google Scholar]
- Wood RA. Pediatric Asthma. Journal of the American Medical Association. 2002;288:745–747. [Google Scholar]