Minimally invasive parathyroidectomy with a lateral approach was found to be an acceptable option in select patients with sporadic primary hyperparathyroidism and previous endocrine neck surgery.
Keywords: Neck therapy, Endocrine, Parathyroidectomy, Minimally invasive, Hyperparathyroidism
Abstract
Objective:
Previous endocrine neck surgery (PENS) in patients with sporadic primary hyperparathyroidism (PHP) is considered a contraindication for minimally invasive parathyroidectomy (MIP). The purpose of our study was to determine the effectiveness of MIP in such patients.
Methods:
From January 2004 to December 2009, 270 patients with PHP were treated in our department; 30 had had PENS in the past. Eighteen were selected to have MIP, while the other 12 had traditional neck explorations. Selection criteria for MIP were unilateral single- or double-gland disease localized preoperatively with at least 2 concordant imaging techniques and patient informed consent. Imaging studies included high-resolution neck ultrasound and sestamibi scan in most patients, and CT scan, selective venous sampling, and MRI in 7 patients. Unilateral explorations via a lateral approach with the patients under local (UALA in 13 patients), general (MIP in 4 patients), or local followed by general anesthesia (1 patient) were performed.
Results:
Sixteen of the 17 patients became normocalcemic after the operation. There was no conversion to traditional exploration. A single adenoma was found in 16 patients and hyperplasia in one. One patient underwent a successful parathyroidectomy 8 months later via mesothoracoscopy, because the parathyroid gland was localized correctly but was beyond access via neck. There were no postoperative complications. Mean duration of the procedure and length of stay were similar to MIP in patients without PENS. Mean follow-up of 33 months (range, 4 to 70) did not reveal any recurrence.
Conclusion:
These results illustrate that MIP is a valuable option in select patients with sporadic PHP and PENS. Localization with 2 or more concordant imaging techniques could avoid intraoperative sestamibi or qPTH testing with low morbidity (0%), high biochemical cure rate (100% in this series), rapid recovery, and finally substantially lower the cost of the procedure.
INTRODUCTION
Minimally invasive parathyroidectomy (MIP) has been accepted as the procedure of choice for the majority of patients with primary hyperparathyroidism (PHP) and single-gland disease and seems to have replaced the gold standard of bilateral neck exploration. The successful results of such minimally invasive procedures are reported to be over 96% in the literature.1,2 Previous endocrine neck surgery (PENS), especially total thyroidectomy, in patients with sporadic PHP was considered by many as a contraindication for MIP. However, in the last decade, a few experienced surgeons have been able to perform minimally invasive parathyroidectomies in patients with PENS achieving very highly successful results. The purpose of our study was first to determine the feasibility of MIP in patients with previous endocrine neck surgery in our department and second to establish the success rates.
PATIENTS AND METHODS
From January 2004 to December 2009, 270 patients with PHP were treated in our department. After the detailed history, 30 of the 270 patients (11.1%) had a previous endocrine neck surgery (most cases were classical total thyroidectomies). Minimally invasive parathyroidectomy was performed only when there was unilateral single- or double-gland disease, and the adenoma(s) was preoperatively localized with 2 concordant imaging techniques, one of which was Sestamibi scanning. Whenever those criteria were not met, patients were scheduled for a bilateral neck exploration. Eighteen of the 30 patients (60%) fulfilled the selection criteria. The remaining 12 patients failed to fulfill either one or both of the selection criteria and underwent a bilateral neck exploration. For the first group, the sex ratio (M/F) was 1/16, and the mean age was 64.8 years (range, 35 to 83).
All patients had preoperative localization with 99mTc- labelled sestamibi imaging and high-resolution ultrasonography of the neck. CT scan, selective venous sampling, and MRI were performed in 7 patients. The previous endocrine neck operations in the 17 patients of the first group were 16 total and subtotal thyroidectomies for benign disease and in 1 case the patient underwent a 2-stage planned UALA (unilateral approach under local anesthesia) parathyroidectomy for parathyroid hyperplasia. All of the patients with PENS had a preoperative voice laryngoscopy to exclude unsuspected damage to the recurrent laryngeal nerves.
Thirteen of 17 patients underwent UALA and 4 underwent MIP while under general anesthesia. When the patient did not feel comfortable during the procedure, the anesthesiologist used light sedation with small doses of intravenous propofol (9 cases). In the event of persistent patient discomfort, despite the sedation, the procedure was converted to MIP with the patient under general anesthesia (1 patient).
A 2-cm to 2.5-cm transverse incision was made in a skin crease directly over the localized parathyroid gland along the front border of the sternocleidomastoid muscle. The strap muscles were divided by sharp dissection with the scissors until the neurovascular cervical bundle was encountered. The lateral margin of the remnant of the thyroid gland was recognized when it was present, and the plane of dissection continued with a medial direction without any hemorrhage until the parathyroid adenoma(s) was identified. It is important to note that in most cases the dissection and removal of the glands was surprisingly easy without any hemorrhaging. A silicon negative pressure drain was placed only in cases of difficult dissection. No gamma probe, qPTH assays (IOPTHA), or frozen-section analysis was performed.
All patients were considered for discharge on the first postoperative day after the morning measurement of blood calcium levels. Calcium and vitamin D3 tablets were given on discharge in cases in which there was a high drop of blood calcium levels. In addition in these cases, patients returned for a second measurement on the third postoperative day. The duration of the operation, the length of stay, the conversions and complication rates were recorded prospectively. All patients were seen in the outpatient clinic on the fifth postoperative day to remove the steri-strip bands and undergo assessment for complications. Further follow-up was at 4 months to 12 months. No statistical analysis was performed.
RESULTS
Over a period of 6 years, 270 patients underwent treatment for primary HPT, and 30 of these had previous neck endocrine surgery. Only 17 of the 30 patients with PENS fulfilled the criteria for MIP. In 12 of the 17 patients selected, the Sestamibi scanning was concordant with the neck ultrasound, and no further imaging was performed. In 7 patients, the 2 methods that were mentioned were nonconcordant and further imaging was performed including computed tomography or magnetic resonance imaging of the neck (3 cases) and selective venous sampling (4 cases).
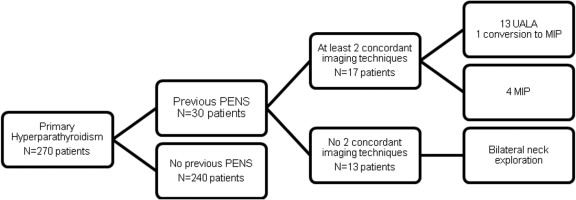
The type of anesthesia, local vs general, depended on the patient's individual preferences. Of a total of 17 patients, 13 had UALA and 4 had MIP while under general anesthesia. In only one case was the operation started as UALA but converted to MIP, because of the patient's anxiety and discomfort (Figure 1).
Figure 1.
Flow chart of the selection process for patients with MIP.
A single parathyroid adenoma was identified in 16 patients, and there was a single case of parathyroid hyperplasia. The location of the excised adenomas was right inferiorly in 7 cases, left inferiorly in 5 cases, right superiorly in 2 cases, at the right upper mediastinum in 1 case, and into the left lobe of the thymus in 1 case. The patient with a histology report of parathyroid hyperplasia was the same patient who was diagnosed preoperatively with hyperplasia, and we decided to perform a 2-stage UALA for the first time. In one of the patients in the UALA group, although the parathyroid adenoma was successfully localized preoperatively with 2 imaging techniques, it was impossible to access it via the neck due to the patient's hunchback and relatively deep localization into the superior mediastinum. Subsequently, the patient had a mesothoracoscopy 8 months later, and the parathyroid adenoma was successfully removed.
The mean operating time was 38 minutes (range, 25 to 45), and it was comparable to the group of patients with MIP without PENS. No surgical complications (nerve damage, hemorrhage, trauma infection) or hypoparathyroidism occurred. The mean hospital stay was approximately 20 hours (range, 19 to 23). The patients were discharged on the first postoperative day after the morning measurement of blood calcium levels. All patients became normocalcemic after the operation; 9 of them required vitamin D3 and calcium supplementation for 5 days to 10 days. No incidents of postoperative hypocalcemia requiring re-admission were recorded. The mean follow-up was 33 months (range 4 to 70), and all of the patients completed follow-up. Thus far, no complications and no cases of recurrent HPT have been reported. The patients, whose minimum follow-up was 4 months, are now more than 10 months out from the operation still with no evidence of complications or recurrence.
DISCUSSION
Surgical treatment of PHP underwent a radical change in the last 12 years, and MIP has gained worldwide acceptance, replacing the gold standard of bilateral neck exploration in patients with a presumed solitary parathyroid adenoma, which concerns 80% of patients with PHP.1–4 Better localization techniques and knowledge of minimally invasive surgery have made MIP a safe and effective procedure with excellent cure rates in experienced hands (>96%), which are similar to traditional bilateral neck exploration.4,5
MIP is a general term including mini-incision focusing procedures performed with the patient under local or general anesthesia, video-assisted, and endoscopic parathyroidectomy with or without an intraoperative gamma probe or IOPTHA. A mini-incision focused approach is the current method of choice for the majority of members of the International Association of Endocrine Surgeons. This procedure is minimal not only due to a small incision, but also because it involves minimal tissue dissection, enables the operation to be performed using local anesthesia in an outpatient setting, lowers hospital stay and cost, lowers the incidence of hypocalcemia compared with standard bilateral exploration and provides better cosmesis and less postoperative pain. Its only major disadvantage includes the possible risk of missing multiglandular disease or a second adenoma.2,5,6
The success of MIP depends on the preoperatively accurate demonstration of the diseased parathyroid gland.7 The most used preoperative localization studies are the sestamibi and high-resolution ultrasonography of the neck with a high sensitivity and specificity of 80% and 90%. But when both of these procedures are in concordance with the diseased gland, the sensitivity reaches to 95% to 97%.5,8,9 In recent years, many centers have performed MIP with a 97% to 98% success rate without using any intraoperative adjuncts.3,5,9 Traditional use of perioperative or intraoperative gamma probe or IOPTHA to confirm the adequacy of resection have not raised the success rate for single-gland disease with concordant sestamibi and ultrasound, even in high-volume endocrine surgery centers.3,9–12 In our study, the CT and MRI scan have been successful in localizing the diseased parathyroid in only 2 cases, in both of which a giant parathyroid was found.
However if preoperative localization studies are not concordant, the use of other localization techniques and gamma probe or IOPTHA are recommended, because the prevalence of multiglandular disease approaches 17%. Similarly, the use of IOPTHA or the gamma probe is recommended for patients undergoing selective parathyroidectomy after a single localization study.3,12,13
PENS in patients with sporadic PHP has been considered a contraindication for MIP. Although in the last 12 years, PHP in a previously operated neck presents a significant challenge to experienced surgeons when performing MIP. So since 1998, Rotstein et al14 and Norman et al have performed successful MIP in the reoperative neck with gamma probe or IOPTHA with a success rate of 93% and 100%.15
We would like to distinguish the difference between the term PENS or reoperative neck in 2 groups. The first concerns patients with a previous parathyroid operation (thyroidectomy or other neck procedures) and the second concerns patients with a previous parathyroidectomy, which means that the second group is that with persistent or recurrent PHP. We agree that persistent or recurrent PHP is a special entity in which many preoperative localization methods and intraoperative gamma probe or IOPTHA might be necessary for acute localization of the gland(s). On the other hand for patients with previous nonparathyroid operations, MIP can be successfully performed, if 2 preoperative localization studies are concordant, because the incidence of single adenoma remains near 80%, the same with PHP in the nonoperated neck.
All patients in this study with MIP had a total or subtotal thyroidectomy, and the PHP appeared later, except in 1 patient with a 2-stage planned UALA for parathyroid hyperplasia. All patients had undergone 2 preoperative concordant localization methods. So after a 28-year experience in parathyroid surgery, we decided to perform UALA or MIP in these patients just like in the nonoperated group. All operations except mesothoracoscopy were performed by the author with a final success rate of 100%.
Barczynski3 emphasizes that
it should be stressed that MIP can be recommended only for surgeons with the appropriate experience in conventional parathyroid surgery (bilateral neck exploration). It is not the operation for ‘beginners,’ as there are many potential entrapments which can be encountered during this, easy at first sight, operation. Experience and sound clinical judgment cannot be replaced by any novel technological adjunct.
CONCLUSION
These results illustrate that MIP with a lateral approach is a valuable option in select patients with sporadic PHP and PENS, except recurrent and persistent PHP. Localization with 2 or more concordant imaging techniques could avoid intraoperative sestamibi or qPTH testing with low morbidity (0%), a high biochemical cure rate (100% in this series), rapid recovery, and finally by substantially lowering the cost of the procedure.
References:
- 1. Inabnet WB, Fulla Y, Richard B, Bonnichon P, Icard P, Chapuis Y. Unilateral neck exploration under local anesthesia: the approach of choice for asymptomatic primary hyperparathyroidism. Surgery. 126(6):1004–1009, 1999. December [DOI] [PubMed] [Google Scholar]
- 2. Chapuis Y. New directions in the surgical treatment of primary hyperparathyroidism. Bull Acad Natl Med. 2003;187(3):493–502 [PubMed] [Google Scholar]
- 3. Barczynski M. Minimally invasive parathyroidectomy without intraoperative parathyroid hormone monitoring: When and why? J Postgrad Med. 2009;55(4):239–240 [DOI] [PubMed] [Google Scholar]
- 4. Pang T, Stalberg P, Sidhu S, et al. Minimally invasive parathyroidectomy using the lateral focused mini-incision technique without intraoperative parathyroid hormone monitoring. Br J Surg. 94(3):315–319, 2007. March [DOI] [PubMed] [Google Scholar]
- 5. Haciyanli M, Genc H, Damburaci N, Oruk G, Tutuncuoglu P, Erdogan N. Minimally invasive focused parathyroidectomy without using intraoperative parathyroid hormone monitoring or gamma probe. J Postgrad Med. 2009;55(4):242–246 [DOI] [PubMed] [Google Scholar]
- 6. Thakur A, Sebag F, Slotema E, Ippolito G, Taúeb D, Henry JF. Significance of biochemical parameters in differentiating uniglandular from multiglandular disease and limiting use of intraorerative parathormone assay. World J Surg. 33(6):1219–1223, 2009. June [DOI] [PubMed] [Google Scholar]
- 7. Quiros R, Alioto J, Wilhelm S, Ali A, Prinz R. An algorithm to maximize use of minimally invasive parathyroidectomy. Arch Surg. 2004;139:501–507 [DOI] [PubMed] [Google Scholar]
- 8. Ghaheri BA, Koslin DB, Wood AH, Cohen JL. Preoperative ultrasound is worthwhile for reoperative parathyroid surgery. Laryngoscope. 114(12):2168–2171, 2004. December [DOI] [PubMed] [Google Scholar]
- 9. Henry JF. Reoperation for primary hyperparathyroidism: tips and tricks. Langenbecks Arch Surg. 2010;395:103–109 Epub 2009 Nov 19 [DOI] [PubMed] [Google Scholar]
- 10. Gawande AA, Monchik JM, Abbruzzese TA, Iannuccilli JD, Ibrahim SI, Moore FD., Jr Reassessment of parathyroid hormone monitoring during parathyroidectomy for primary hyperparathyroidism after 2 preoperative localization studies. Arch Surg. 141(4):381–384, 2006. April [DOI] [PubMed] [Google Scholar]
- 11. Stalberg P, Sidhu S, Sywak M, Robinson B, Wilkinson M, Delbridge L. Intraoperative parathyroid hormone measurement during minimally invasive parathyroidectomy: does it “value-add” to decision-making? J Am Coll Surg. 203(1):1–6, 2006. July [DOI] [PubMed] [Google Scholar]
- 12. Gil-Cardenas A, Gamino A, Reza A, Pantoja JP, Herrera MF. Is intraoperative parathyroid hormone assay mandatory for the success of targeted parathyroidectomy? J Am Coll Surg. 204(2):286–290, 2007. February [DOI] [PubMed] [Google Scholar]
- 13. Mihai R, Palazzo FF, Gleeson FV, Sadler GP. Minimally invasive parathyroidectomy without intraoperative parathyroid hormone monitoring in patients with primary hyperparathyroidism. Br J Surg. 94(1):42–47, 2007. January [DOI] [PubMed] [Google Scholar]
- 14. Rotstein L, Irish J, Gullane P, Keller MA, Sniderman K. Reoperative parathyroidectomy in the era of localization technology. Head Neck. 20(6):535–539, 1998. September [DOI] [PubMed] [Google Scholar]
- 15. Norman J, Denham D. Minimally invasive radioguided parathyroidectomy in the reoperative neck. Surgery. 124(6):1088–1092, 1998. December [DOI] [PubMed] [Google Scholar]