This is a rare case of a bronchogenic cyst found below the diaphragm within the lesser sac successfully resected by laparoscopic means.
Keywords: Bronchogenic cyst, Endoscopic ultrasound, Laparoscopy
Abstract
Bronchogenic cysts rarely develop in the abdomen they typically reside in the mediastinum. We present a unique case of a bronchogenic cyst within the lesser sac. Endoscopic ultrasound proved to be a critical diagnostic tool, and the patient underwent a laparoscopic resection of the lesion.
INTRODUCTION
Bronchogenic cysts are congenital anomalies of the tracheobronchial tree that are normally found within the mediastinum. They rarely develop inferior to the diaphragm, in either a retroperitoneal or intraperitoneal location. We report a case of an intraperitoneal paraesophageal bronchogenic cyst within the lesser sac. This cyst was diagnosed by endoscopic ultrasound and aspiration, and it was successfully treated with laparoscopic resection.
CASE REPORT
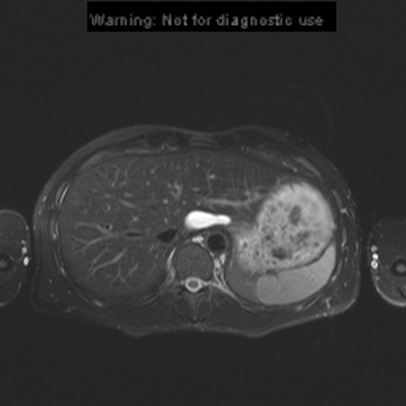
A 33-year-old man presented with a 9-month history of intermittent epigastric and right upper quadrant pain and burning, and a pressure sensation like “a ball” within the abdomen. His past medical history was significant for recurrent spontaneous pneumothoraces, requiring pleurodesis and resulting in chronic chest wall pain and narcotic requirements. Clinical examination did not reveal any palpable masses but was significant for mild to moderate tenderness of the deep epigastrium. Laboratory values, including liver chemistries, were normal. Ultrasonography suggested a 4.3cm x 1.7cm echogenic lesion in the caudate lobe of the liver, consistent with either a hemorrhagic cyst or thrombosed vascular structure. Magnetic resonance imaging (MRI) demonstrated a 4.5cm x 1.7cm ovoid, well-circumscribed lesion abutting the caudate lobe of the liver and the proximal stomach near the gastroesophageal junction (Figure 1). There was no air fluid level to suggest communication with the gastrointestinal tract.
Figure 1.
MRI showing bronchogenic cyst at gastroesophageal junction (Axial T2 GRASE (gradient and spin echo) with fat suppression.
Endoscopic ultrasound (EUS) revealed a large cystic structure without internal nodules or masses adjacent to the liver and proximal stomach in the lesser sac. The aspirate was a thick, turbid, mucus-like material. Its cytology included squamous cells, ciliated glandular cells, and clusters of foam cells, all consistent with a bronchogenic cyst.
The abdomen was explored with a 30-degree laparoscope. Upon evaluation of the lesser sac, we discovered a 6cm x 3cm thick-walled cyst superior to the celiac axis. Its fibrous and areolar attachments were divided with a Harmonic scalpel and electrocautery, and the oblong cyst was removed intact and in its entirety. The cyst was not contiguous with the adjacent viscera, including the gut, nor was there any adjacent pathology. The patient was discharged home a few hours later, and his preoperative abdominal symptoms resolved, although he continues to experience chronic chest wall pain. Histology of the cyst revealed respiratory epithelium with a chronic lymphocytic infiltrate lining a smooth muscle wall, consistent with a bronchogenic cyst.
DISCUSSION
Bronchogenic cysts are rare congenital anomalies of the ventral foregut that arise from abnormal budding of the tracheobronchial tree during the fifth week of fetal development.1,2 They are typically found in the mediastinum in presternal, pulmonary, or pericardial areas,3–5 but there have been infrequent reports of bronchogenic cysts being discovered inferior to the diaphragm. The most common site of these abdominal cysts is in the retroperitoneum, and they are often thought to be adrenal masses.6–8
The location of a bronchogenic cyst inferior to the diaphragm is attributable to the fact that, until the sixth week of development, the pleuroperitoneal membrane and embryonic diaphragm have not yet fused. Consequently, abnormal tracheobronchial buds can be isolated by the growing diaphragm and migrate into the abdomen.5 Bronchogenic cysts are composed of smooth muscle, cartilage, and glands lined with ciliated columnar epithelium.6,9 This is in contrast to esophageal duplication cysts that have 2 smooth muscle layers, as does the esophagus.9,10
A literature review yielded over 40 reported cases of intraabdominal bronchogenic cysts, of which 13 were truly intraperitoneal.11,12 Most intraperitoneal bronchogenic cysts are associated with the stomach, diaphragm, pancreas, or gallbladder.5,7,12–14 There are only 2 other reports of adults with intraperitoneal paraesophageal bronchogenic cysts, both of which were immediately adjacent to the gastroesophageal junction, and apparently not within the lesser sac.15,16 Only one other intraperitoneal paraesophageal bronchogenic cyst has been reported within the lesser sac, and that was in a 10-year-old boy.17
Intraabdominal bronchogenic cysts are often asymptomatic and discovered incidentally.6,18 When symptoms are present, as in our case, they may be nonspecific, such as intermittent discomfort or epigastric pressure. The symptoms may be due to cyst expansion and compression of adjacent viscera, rupture, or secondary infection.6,17,19,20 When imaging reveals an upper-abdominal cyst, the differential diagnosis is a function of the cyst's location and the patient's age. A differential diagnosis for adults includes cystic lesions of the liver, pancreas, or spleen; gastrointestinal stromal tumor (GIST); teratoma; dermoid cyst; lipoma; adrenal tumor; paraganglioma; pheochromocytoma; lymphangioma; mesothelioma; hemangioma; lymphoma; dermoid cyst; gastrointestinal (eg, esophageal) duplication cyst; bronchogenic cyst; leiomyoma; neurofibromas; hematoma; abscess; or cystic degeneration of a neoplasm.6,17,18,20 Pediatric patients could have many of the same diagnoses, but the diagnoses in children are likely to be dermoid cysts, teratomas, adrenal tumors, duplication cysts, bronchogenic, or other cysts originating from foregut and urogenital malformations, or neuroblastoma/ganglioneuroblastoma.17,18
Computed tomography (CT) and MRI are frequently used in the assessment of an abdominal mass. However, these modalities have limitations with bronchogenic cysts.6 With CT, bronchogenic cysts may appear to be hyperdense, due to the thick proteinaceous fluid contents, suggesting a calcified solid mass.20 An MRI scan may reveal a cystic pattern, when long T1 and T2 signals are present.6,20,21 However, it may be difficult to determine the origin of the lesion and whether it is adherent to or intrinsic to an intraabdominal organ such as the liver or pancreas.21
Endoscopic ultrasound (EUS) has enhanced the assessment of pancreatobiliary diseases and gastrointestinal malignancies, and it also permits aspiration for cytology.22,23 Endoscopic fine needle aspiration secured a diagnosis of a bronchogenic cyst in our case. Furthermore, the absence of 2 muscle layers offered us assurance that the patient did not have an esophageal duplication cyst that might have required a more elaborate, and perhaps open, operation. To the best of our knowledge, EUS has been reported in the diagnosis of a bronchogenic cyst just once before our case, and that was done without aspiration. This diagnostic option is available to both adults and children, although general anesthesia may be necessary for younger patients.24
The treatment of bronchogenic cysts is surgical resection. Removal of the cyst will most likely alleviate symptoms and avoid complications, such as infection, rupture, or compression of adjacent viscera, as well as the rare but dangerous possibility of malignant transformation.25–28 Moreover, once the cyst is removed, a definitive diagnosis is established.
CONCLUSION
Bronchogenic cysts rarely develop in the abdomen, but they should be entertained in the differential diagnosis of lesser sac cystic lesions. Endoscopic ultrasound with aspiration is a valuable diagnostic adjunct that can determine the nature, location, and histology of the cyst, and whether it may be amenable to laparoscopic resection. The majority of intraabdominal bronchogenic cysts reside in the retroperitoneum, and many of those can be resected with minimally invasive techniques similar to the treatment of those found within the peritoneal cavity. To our knowledge, this is the second reported case of a lesser sac bronchogenic cyst being laparoscopically resected, and the first such case described in adults.
Acknowledgments
Thank you to Dr. Ali Guermazi for help with images as well as with the French translation of a critical reference.
References:
- 1. Wright C. Congenital malformations of the lung. Current Diagnostic Pathology. 2006;12:191–201 [Google Scholar]
- 2. Berrocal T, Madrid C, Novo S, Gutiérrez J, Arjonilla A, Gómez-León N. Congenital anomolies of the tracheobronchial tree, lung, and mediastinum: embryology, radiology, and pathology. Radiographics. 2004. Jan-Feb;24(1)e17. [DOI] [PubMed] [Google Scholar]
- 3. Ozel SK, Kazez A, Koseoguliari AA, Akpolat N. Scapular bronchogenic cysts in children: case report and review of the literature. Pediatr Surg Int. 2005. October;21(10):843–845 [DOI] [PubMed] [Google Scholar]
- 4. Sarper A, Ayten A, Golbasi I, Demircan A, Isin E. Bronchogenic cyst. Tex Heart Inst J. 2003;30(2):105–108 [PMC free article] [PubMed] [Google Scholar]
- 5. Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408(1):93–98 [DOI] [PubMed] [Google Scholar]
- 6. Chung JM, Jung MJ, Lee W, Choi S. Retroperitoneal bronchogenic presenting as adrenal tumor in adult successfully treated with retroperitoneal laparoscopic surgery. Urology. 2009. February;73(2):442.e13–e15 [DOI] [PubMed] [Google Scholar]
- 7. Hedayati N, Cai DX, McHenry CR. Subdiaphragmatic bronchogenic cyst masquerading as an “adrenal incidentaloma.” J Gastrointest Surg. 2003. Sep-Oct;7(6):802–804 [DOI] [PubMed] [Google Scholar]
- 8. Yamamoto E, Nakayama H, Ozaki N, et al. Laparoscopically resected foregut cyst adjacent to the right adrenal gland. Diagn Ther Endosc. 1998;5(1):53–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harvell JD, Macho JR, Klein HZ. Isolated intra-abdominal esophageal cyst. Case report and review of the literature. Am J Surg Pathol. 1996. April;20(4):476–479 [DOI] [PubMed] [Google Scholar]
- 10. Nobuhara KK, Gorski YC, La Quaglia MP, Shamberger RC. Bronchogenic cysts and esophageal duplications: common origins and treatment. J Pediatr Surg. 1997. October;32(10):1408–1413 [DOI] [PubMed] [Google Scholar]
- 11. Liang MK, Yee HT, Song JW, Marks JL. Subdiaphragmatic bronchogenic cysts: a comprehensive review of the literature. Am Surg. 2005. December;71(12):1034–1041 [PubMed] [Google Scholar]
- 12. Kim KH, Kim JI, Ahn CH, et al. The first case of intraperitoneal bronchogenic cyst in Korea mimicking a gallbladder tumor. J Korean Med Sci. 2004. June;19(3):470–473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Amendola MA, Shirazi KK, Brooks J, Agha FP, Dutz W. Transdiaphragmatic bronchopulmonary foregut anomaly: “Dumbell” bronchogenic cyst. AJR Am J Roentgenol. 1982. June;138(6):1165–1167 [DOI] [PubMed] [Google Scholar]
- 14. Mcglynn TJ, Jr., Burnside JW, Gatenby RA. Symptomatic abdominal bronchogenic cyst mimicking acute ischemic heart disease. Heart Lung. 1981. Jan-Feb;10(1):109–111 [PubMed] [Google Scholar]
- 15. Bechade D, Zerbib F, Sauvet P, Boisseau C, Vialette G. Abdominal paraesophageal bronchogenic cyst. Gastroenterol Clin Biol. 1993;17(10):758–761 [PubMed] [Google Scholar]
- 16. Díaz Nieto R, Naranjo TA, Gómez Alvarez M, et al. Intraabdominal bronchogenic cyst. J Gastrointest Surg. 2010. April;14(4):756–758 [DOI] [PubMed] [Google Scholar]
- 17. Sauvat F, Fusaro F, Jaubert F, Galifer B, Revillon Y. Paraesophageal bronchogenic cyst: first case reports in pediatric. Pediatr Surg Int. 2006. October;22(10):849–851 [DOI] [PubMed] [Google Scholar]
- 18. Martín R, Sanz E, de Vicente E, et al. Differential diagnosis of asymptomatic retroperitoneal cystic lesion: a new case of retroperitoneal bronchogenic cyst. Eur Radiol. 2002. April;12(4):949–50 [DOI] [PubMed] [Google Scholar]
- 19. Miller RF, Graub M, Pashuck ET. Bronchogenic cysts; anomalies resulting from maldevelopment of the primitive foregut and midgut. Am J Roentgenol Radium Ther Nucl Med. 1953. November;70(5):771–785 [PubMed] [Google Scholar]
- 20. Murakami R, Machida M, Kobayashi Y, Ogura J, Ichikawa T, Kumazaki T. Retroperitoneal bronchogenic cyst: CT and MR Imaging. Abdom Imaging. 2000. Jul-Aug;25(4):444–447 [DOI] [PubMed] [Google Scholar]
- 21. Hisatomi E, Miyajima K, Yasumori K, et al. Retroperitoneal bronchogenic cyst: a rare case showing the characteristic Imaging feature of milk calcium. Abdom Imaging. 2003. Sep-Oct;28(5):716–720 [DOI] [PubMed] [Google Scholar]
- 22. Yamao K, Bhatia V, Mizuno N, Sawaki A, Shimizu Y, Irisawa A. Interventional endoscopic ultrasonography. J Gastroenterol Hepatol. 2009. April;24(4):509–519 [DOI] [PubMed] [Google Scholar]
- 23. Vilmann P, Jacobsen GK, Henriksen FW, Hancke S. Endoscopic ultrasonography with guided fine needle aspiration biopsy in pancreatic disease. Gastrintest Endosc. 1992. Mar-Apr;38(2):172–173 [DOI] [PubMed] [Google Scholar]
- 24. Attila T, Adler DG, Hilden K, Falgel DO. EUS in pediatric patients. Gastrointest Endosc. 2009. November;70(5):892–898 [DOI] [PubMed] [Google Scholar]
- 25. Jakopovic M, Slobodnjak Z, Krizanac S, Samarzija M. Large cell carcinoma arising in bronchogenic cyst. J Thorac Cardiovasc Surg. 2005. August;130(2):610–612 [DOI] [PubMed] [Google Scholar]
- 26. Servais E, Paul S, Port JL, Altorki NK, Lee PC. Carcinoid tumor nested within a bronchogenic cyst. J Thorac Cardiovasc Surg. 2008. July;136(1):227–228 [DOI] [PubMed] [Google Scholar]
- 27. Endo C, Imai T, Nakagawa H, Ebina A, Kaimori M. Bronchioloalveolar carcinoma arising in a bronchogenic cyst. Ann Thorac Surg. 2000. March;69(3):933–935 [DOI] [PubMed] [Google Scholar]
- 28. Sullivan SM, Okada S, Kudo M, Ebihara Y. A retroperitoneal bronchogenic cyst with malignant change. Pathol Int. 1999. April;49(4):338–341 [DOI] [PubMed] [Google Scholar]