Abstract
Background
There is a long history of coronary heart disease (CHD) diagnosis and treatment in Chinese medicine (CM), but a formalized description of CM knowledge is still unavailable. This study aims to analyze a set of CM clinical data, which is important and urgent.
Methods
Relative associated density (RAD) was used to analyze the one-way links between the symptoms or syndromes or both. RAD results were further used in symptom selection.
Results
Analysis of a dataset of clinical CHD diagnosis revealed some significant relationships, not only between syndromes but also between symptoms and syndromes. Using RAD to select symptoms based on different classifiers improved the accuracy of syndrome prediction. Compared with other traditional symptom selection methods, RAD provided a higher interpretability of the CM data.
Conclusion
The RAD method is effective for CM clinical data analysis, particular for analysis of relationships between symptoms in diagnosis and generation of compact and comprehensible symptom feature subsets.
Background
Western medicine classifies coronary heart disease (CHD) as a kind of myocardial dysfunction and organic lesion, occasionally accompanied by coronary artery stenosis and vertebrobasilar insufficiency [1]. In contrast, Chinese medicine (CM) classifies CHD as a type of chest paralysis and heart pain, for which effective diagnosis and treatment are available [2].
CM treatment is based primarily on syndrome differentiation and physiology and pathology of Zang-fu organs and meridians. In CM, a symptom represents an observable indicator of abnormality, while a syndrome is the disease state manifested by symptoms. The connections between symptoms and syndromes in CM are not clearly defined. Therefore, it is necessary to delineate different relationships between symptoms and syndromes and explain the diagnosis results in comprehensible terms [3].
Machine learning builds empirical models on data for analysis and forecasting, which has recently been used for CM data analysis. Huang and Gao [4] reviewed several classifiers of data mining in CM. Li and Huang [5] used fuzzy neural network for analysis of CM ingredients. Wang et al. [6] used a decision tree method to generate prediction models for CM hepatitis data and liver cirrhosis data. Zhang et al. [7] combined factor and cluster analysis in the classification of CM syndromes related to post-hepatitic cirrhosis. Zhang et al. [8] used latent tree models to aid CM diagnosis. Knowledge discovery in database (KDD) [9], rough set [10], and expert system [11], have also been applied to CM.
Most CM machine learning works does not consider the medical meaning and links among features. However, CM data contain a large quantity of symptoms or syndromes which have specific medical meaning. Therefore, seeking the links between features including symptoms and syndromes in CM data analysis is also important.
Conventional methods usually use only one numerical value to describe the relationship of two symptoms. In this study, we use a pair of characteristic values to describe a relative link between the symptoms as a relative associated density (RAD). By analysing the characteristic value pairs, we searched significant one-way links between symptoms and confirmed the links according to CM theory [12,13]. The RAD method was also used to find one-way links among multiple syndromes in the clinical data.
Among a large number of symptoms in CM diagnosis data sets for a certain disease, some symptoms may be redundant. Therefore, selecting major or relevant symptoms is crucial to the performance of machine learning. Wang et al. [14] used support vector machine (SVM) to generalize symptom weights in CHD predictions. Liu et al. [15] used symptom frequency analysis to enhance modelling results in learning. Zhou et al. [16] developed a clinical reference information model (RIM) and a physical data model to manage various entities and relationships in CM clinical data. Principal component analysis (PCA) [17], partial least squares (PLS) [18], maximum relevance and minimum redundancy (MRMR) [19] have been used to perform symptom selection to improve prediction accuracy.
The results from conventional primary symptom selection or reduction methods are difficult to be interpreted in CM. For instance, PCA reduces symptom dimensionality at the expense of loss of medical meaning [20]. Although MRMR can predict fairly using only a few major symptoms [21], the results are often inconsistent with basic CM theory [12,13]. This study aims to use RAD to perform symptom selection, and evaluate whether the results can be better explained by CM theory [12,13].
Methods
Data set of CHD in CM
A total of 555 clinical cases were collected from the cardiology departments of Longhua Hospital, Shuguang Hospital, Shanghai Renji Hospital, and Shanghai Hospital of CM form March 2007 to May 2008 to compile the CHD data set used in this study. It could be obtained from the address http://levis.tongji.edu.cn/gzli/publication.htm[15].
Out of the 555 cases, 265 patients (47.7%) were male, age (mean ± standard deviation): 65.15 ± 13.17 and 290 patients (52.3%) are female, age: 65.24 ± 13.82. The symptoms collected from inquiry diagnosis include 125 symptoms in eight dimensions (cold or warm, sweating, head, body, chest and abdomen, urine and stool, appetite, sleeping, mood, and gynecology). The differentiation diagnosis includes 15 syndromes, as described in Liu et al. [15].
For unification of the results, specific types and feeling information of some symptoms were combined and some symptoms unique to females were deleted. The variables analyzed in this study include 63 symptoms and 10 syndromes. The 63 included symptoms were listed in Table 1. The 10 included syndromes were (I) heart-qi deficiency syndrome; (II) heart-yang deficiency syndrome; (III) heart-yin deficiency syndrome; (IV) heart-blood deficiency syndrome; (V) turbid phlegm syndrome; (VI) blood stasis syndrome; (VII) qi stagnation syndrome; (VIII) heart-fire hyperactivity syndrome; (IX) heart-kidney yang deficiency syndrome; (X) cardiopulmonary-qi deficiency syndrome.
Table 1.
The 63 symptoms in the data set
| No. | Symptom |
|---|---|
| 1 | Chills |
| 2 | Cold limbs |
| 3 | Dampness-heat |
| 4 | Feverish palms and soles |
| 5 | Spontaneous sweating |
| 6 | Night sweat |
| 7 | Palpitation |
| 8 | Chest distress |
| 9 | Chest pain |
| 10 | Short breath/dyspnea/suffocation |
| 11 | Edema |
| 12 | Hypodynamia |
| 13 | Dysphoria |
| 14 | Paroxysmal night dyspnea |
| 16 | Amnesia |
| 16 | Dizziness |
| 17 | Tinnitus |
| 18 | Mouth and tongue sore |
| 19 | Cough |
| 20 | Cough with sputum |
| 21 | Hiccup |
| 22 | Acid regurgitation |
| 23 | Gastric stuffiness |
| 24 | Gastralgia |
| 25 | Epigastric upset |
| 26 | Nausea and vomiting |
| 27 | Heavy breathing |
| 28 | Lateral thorax distending pain |
| 29 | Abdomen distending pain |
| 30 | Soreness and weakness of waist and knees |
| 31 | Numbness of hands and feet |
| 32 | Body soreness |
| 33 | Thirsty and dry pharynx |
| 34 | Absence of thirst and no desire for water drink |
| 35 | Intake of fluid failing resolve thirst |
| 36 | Like cold drink |
| 37 | Like hot drink |
| 38 | Poor appetite and less amount of food |
| 39 | Always hungry |
| 40 | Hunger without desire to eat |
| 41 | Bitter taste |
| 42 | Mucosity in mouth |
| 43 | Tastelessness in mouth |
| 44 | Loose stool |
| 45 | Water like stool |
| 46 | Diarrhea with undigested food |
| 47 | Diarrhea in the morning |
| 48 | Stool sometimes sloppy and sometimes bound |
| 49 | Constipation |
| 50 | Dry stool like sheep feces |
| 51 | Non-smooth defecation or tenesmus |
| 52 | Clear urine in large amounts |
| 53 | Dark urine |
| 54 | Frequent micturition |
| 55 | Deficient urine |
| 56 | Stranguria |
| 57 | Urinating burning heat |
| 58 | Dribble of urine |
| 59 | The frequent and increased urination at night |
| 60 | Aggravating gloom |
| 61 | Sleepiness |
| 62 | Impetuosity and susceptibility to rage |
| 63 | Easily frightened and scared |
The RAD method
Probability and statistics
In the medical diagnosis of CHD, frequency of symptom occurrence may be different. For instance, the chest tightness symptom and the dizziness symptom are frequent symptoms, while the sleepiness symptom and the diarrhea with undigested food symptom are rare symptoms. In the data analysis, the first step is to distinguish between the frequent and the rare symptoms.
In probability of symptoms, Pfi stands for the appearance probability of the ith symptom across all cases, which is defined as
| (1) |
where Fim = 1 if the ith symptom appears in the mth case, or else Fim = 0. N denotes the number of the cases.
Similarly, Pli stands for the appearance probability of the ith syndrome across all cases, which is defined as
| (2) |
where the ith syndrome appears in the mth sample, Lim = 1, or else Lim = 0.
Building the symptom-symptom interaction network
Equations (1) and (2) calculate the appearance probability of all symptoms and syndromes. But these values cannot reveal their potential connections. Symptom-symptom interaction (SSI) network in the same manner as used for human social networks was used to find the connections [21,22].
When two different symptoms occur simultaneously in the same case, sign Gim = 1 indicating that symptom Fi and symptom Fj appear at the same time in the mth case, or else Gijm = 0. FiFj stands for the number of simultaneous occurrences of Fi and Fj. Then for N cases,
| (3) |
which contains two types of information: the frequency of features and the relevancy of two features.
Relative associated density
Equation (3) is largely concerned with the frequency of symptoms. In other words, frequent relationships between symptoms are obvious, while less frequent relationships are hard to be detected. The difference is even more than 300 folds. Therefore, this study used RAD, which uses conditional probability to measure the relationships of symptoms and syndromes.
The term C(Fi, Fj) represents the RAD values of symptom Fi associated with Fj and use C(Fj, Fi) represents the RAD values of symptom Fi associated with Fj. According,
| (4a) |
| (4b) |
Symptom selection with RAD
In the mth case, if symptom Fi appears with syndrome Lj, Hijm = 1; otherwise, Hijm = 0. Then for all N cases,
| (5) |
RAD estimates the influence of the appearance probability on the interaction between a symptom and a syndrome. Equation (6) calculates the RAD value between symptoms and syndromes,
| (6) |
This kind of association could be recognized as the contribution of one symptom to the syndrome.
Each syndrome was considered a single label; thus we selected corresponding symptoms regardless of their RAD values. For each single label prediction, the symptoms with low RAD values were removed one by one, and the predictions were calculated with SVM and KNN. The symptoms that lead to the highest prediction were recorded as the result of symptom selection.
MRMR symptom selection was used for a comparison [19]. The idea of MRMR is to search the optimal subset by maximizing relevance while minimizing redundancy based on mutual information. To maintain consistency with the RAD method, we used SVM [23] and KNN [24] for classification.
To evaluate the prediction results, we calculated the true positive rate (TPR), and true negative rate (TNR) criteria: TPR = TP/(TP + FN), TNR = TN/(FP + TN), where TP is the number of true positives, TN is that of true negatives, FP is that of false positives, and FN is that of false negatives. The G-means criterion was used to describe the equilibrium of the positive and negative classes of the prediction results, where G-means = (TPR * TNR)1/2.
Results and discussion
RAD performed better than MRMR in feature selection for machine learning to discover CM relationships among the symptoms, syndromes, and even between the symptoms and syndromes in a CHD data set. RAD analysis found one-way connections among symptoms and the syndromes that are consistent with CM theory. RAD not only improves prediction accuracy but also enhanced interpretability.
Common and rare symptoms
We used equation (1) to determine the symptom frequency in the data set. The first 20 frequent symptoms were identified as listed in Table 2. Table 3 lists the first 10 rare symptoms in the data set.
Table 2.
The most frequent symptoms and their appearance probability
| Order | Symptom | Appearance probability |
|---|---|---|
| 1 | Chest distress | 78.6% |
| 2 | Short breath/dyspnea/suffocation | 69.7% |
| 3 | Hypodynamia | 65.4% |
| 4 | Palpitation | 64.5% |
| 5 | Soreness and weakness of waist and knees | 50.8% |
| 6 | Chest pain | 48.6% |
| 7 | Thirsty and dry pharynx | 48.6% |
| 8 | Dizziness | 48.5% |
| 9 | Aggravating gloom | 43.4% |
| 10 | Dysphoria | 40.4% |
| 11 | Spontaneous sweating | 39.1% |
| 12 | Numbness of hands and feet | 37.1% |
| 13 | Night sweat | 36.2% |
| 14 | Tinnitus | 35.1% |
| 15 | Chills | 35.0% |
| 16 | Cough | 32.6% |
| 17 | Impetuosity and susceptibility to rage | 32.3% |
| 18 | The frequent and increased urination at night | 29.5% |
| 19 | Like cold drink | 25.9% |
| 20 | Cough with sputum | 25.4% |
Table 3.
The 10 rarest appeared symptoms and their frequency
| Order | Symptom | Frequency |
|---|---|---|
| 1 | Urinating burning heat | 0.2% |
| 2 | Sleepiness | 0.7% |
| 3 | Diarrhea in the morning | 0.9% |
| 4 | Hunger without desire to eat | 1.1% |
| 5 | Non-smooth defecation or tenesmus | 1.3% |
| 6 | Water like stool | 1.4% |
| 7 | Diarrhea with undigested food | 1.4% |
| 8 | Stool sometimes sloppy and sometimes bound | 1.6% |
| 9 | Dribble of urine | 2% |
| 10 | Always hungry | 2.2% |
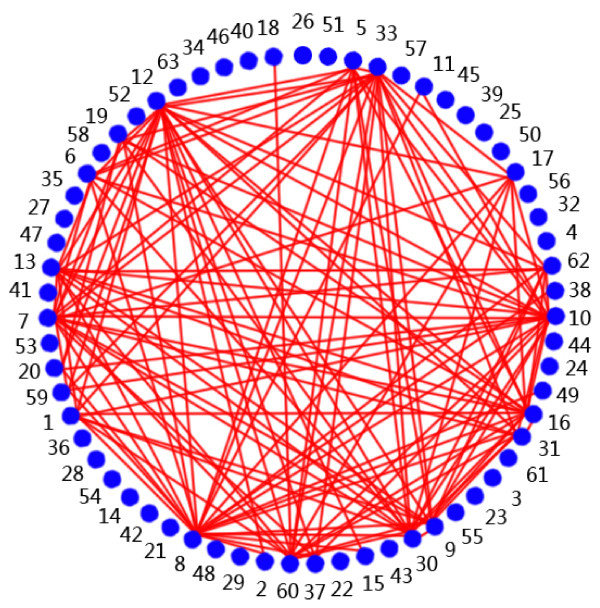
SSI was calculated by equation (3). Figure 1 shows a network constructed from the SSI results, i.e., the frequency and relationship among the symptoms. Table 4 lists the important symptoms shown in Figure 1.
Figure 1.
The network of SSI. The points denote the symptoms; solid lines connect the high SSI.
Table 4.
Symptoms with high SSI values shown in Figure 1
| Symptom | Symptom |
|---|---|
| Tinnitus | Soreness and weakness of waist and knees |
| Spontaneous sweating | Thirsty and dry pharynx |
| Impetuosity and susceptibility to rage | Chills |
| Palpitation | Aggravating gloom |
| Numbness of hands and feet | Night sweat |
| Chest pain | Cough |
| Hypodynamia | Like cold drink |
| Dizziness | Cough with sputum |
| Short breath/dyspnea/suffocation | The frequent and increased urination at night |
| Dysphoria | Chest distress |
CHD was identified as a kind of deficiency syndromes or excess syndromes. As shown in Tables 2 and 4, CHD was associated with kidney deficiency, diet disloyalty, mental disturbance, cold pathogen invasion, and other factors. CHD occurred in the heart but was related to the liver, the kidney, and the spleen. CHD was also bound with heart-qi deficiency, heart-yang deficiency, heart-blood deficiency, and heart-yin deficiency. The imbalance of liver, kidney, and spleen was often accompanied by turbid phlegm syndrome, qi stagnation syndrome, blood stasis syndrome. From the first 20 most frequent symptoms, the symptoms of chest distress, hard breath/dyspnoea/suffocation, palpitation, and chest pain were found to be the locating syndrome of syndrome patterns of the heart, in consistency with modern clinical practice of CHD in CM. Other symptoms among the top 20 were also basic factors in CM heart system diseases diagnosis [12,13].
Table 3 lists the top 10 rare symptoms and their probabilities. The symptoms of the heart syndrome patterns were hunger without desire to eat and water-like stool symptom. This result was also consistent with CM theory [12,13].
Analysis using the RAD method
RAD analysis of the SSI networks was used to determine the connections between symptoms, and identified major symptoms in CHD.
Equation (4) was used to determine the RAD values of SSI, as shown in Table 5.
Table 5.
Some RAD values of SSI
| Fi | |||||||
|---|---|---|---|---|---|---|---|
| Chills | Cold limbs |
Dampness -heat |
Spontaneous sweating | Palpitation | Chest distress |
Chest pain |
|
| Fj | |||||||
| Chills | 0.0% | 71.5% | 28.8% | 36.9% | 41.1% | 37.6% | 38.1% |
| Cold limbs | 45.4% | 0.0% | 22.0% | 21.7% | 25.7% | 22.9% | 23.3% |
| Dampness-heat | 8.8% | 10.6% | 0.0% | 15.7% | 11.7% | 11.0% | 10.4% |
| Spontaneous sweating | 41.2% | 38.2% | 57.6% | 0.0% | 41.9% | 42.4% | 41.5% |
| Palpitation | 75.8% | 74.8% | 71.2% | 69.1% | 0.0% | 68.6% | 61.5% |
| Chest distress | 84.5% | 81.3% | 81.4% | 85.3% | 83.5% | 0.0% | 80.7% |
| Chest pain | 53.1% | 51.2% | 47.5% | 51.6% | 46.4% | 50.0% | 0.0% |
Pij and Pji always appeared as a pair. Some symptoms were obviously one-way connections. For example, only 11.4% of occurrences of the hard breath symptom were accompanied by the hot flash symptom, while 74.6% of occurrences of the hot flash symptom appeared with the hard breath symptom. This was typical one-way connection between two symptoms.
Table 6 lists more connections between two symptoms. CM theory holds that chills occur with yang asthenia [12,13]. Yin asthenia occurs with hot flashes and night sweats [12,13]. The probabilities of chills appearing with hot flashes and night sweats is low, and their occurring probabilities are 0.087 and 0.061, separately.
Table 6.
One-way connections between symptoms
| Symptom | RAD (L to R) | Symptoms | RAD (R to L) |
|---|---|---|---|
| 28 Lateral thorax distending pain | 0.529 | 1 Chills | 0.046 |
| 56 Stranguria | 0.571 | 1 Chills | 0.041 |
| 47 Diarrhea in the morning | 0.600 | 3 Dampness-heat | 0.050 |
| 28 Lateral thorax distending pain | 0.529 | 5 Spontaneous sweating | 0.041 |
| 42 Mucosity in mouth | 0.764 | 5 Spontaneous sweating | 0.059 |
| 43 Tastelessness in mouth | 0.550 | 5 Spontaneous sweating | 0.050 |
| 52 Clear urine in large amounts | 0.625 | 5 Spontaneous sweating | 0.046 |
| 53 Dark urine | 0.571 | 5 Spontaneous sweating | 0.055 |
| 42 Mucosity in mouth | 0.529 | 6 Night sweat | 0.044 |
| 14 Paroxysmal night dyspnea | 0.933 | 7 Palpitation | 0.078 |
| 25 Epigastric upset | 0.826 | 7 Palpitation | 0.053 |
| 35 Intake of fluid failing resolve thirst | 0.700 | 7 Palpitation | 0.058 |
Table 6 also lists the RAD values of one-way connections between symptoms. For instance, the probability of chills accompanied by body coldness was 71.5%, while the probability of body coldness accompanied by chills was only 45.4%. These unequal results indicate that a patient suffering from chills would be more likely to have the body coldness symptom. By contrast, a patient suffering from body coldness would be less likely to have the chills symptom. Furthermore, the locating symptom of chest distress occurred with qualitative and locating symptoms, such as paroxysmal night dyspnoea or orthopnoea, tastelessness and tediousness, nausea and vomiting, epigastric upset, deficient urine, dark urine, feverish palms and soles, intake of fluid failing to resolve thirst, stool resembling sheep's droppings. When paroxysmal night dyspnoea or orthopnoea happened, chest distress symptoms rarely appeared at the same time. Therefore, the one-way connections between the symptoms calculated by RAD explained the clinical results in CM. For example, yang asthenia was the representation of chills, and when chills present, distending pain in the hypochondrium and urine astringent pain appeared at the same time. However, the latter two symptoms did not represent chills; thus, they would not be accompanied by the symptom of chills. For another example, spontaneous sweating was an expression of the qi asthenia symptom and possibly appeared with distending pain in the hypochondrium, a sticky slimy sensation in the mouth, dark urine, but not vice versa. From these two examples, we can see that the contribution of chills to yang asthenia was greater than that of spontaneous sweating to qi asthenia. In the meantime, we may infer that distending pain in the hypochondrium, a sticky slimy sensation in the mouth, and dark urine are not typical features of qi asthenia and yang asthenia. This association analysis of symptoms can show which symptoms are major features and identify possible relationships between symptoms and syndromes. This kind of analysis would provide an objective basis for standardization of dialectic diagnosis.
Relationships among the syndromes
Table 7 shows the frequencies of all 10 syndromes calculated using equation (2). Table 8 lists the RAD values of the syndrome.
Table 7.
Frequency values of 10 syndromes
| Order | Syndrome | Frequency |
|---|---|---|
| 1 | Blood stasis syndrome (VI) | 76.0% |
| 2 | Heart-qi deficiency syndrome (I) | 60.9% |
| 3 | Turbid phlegm syndrome (V) | 48.3% |
| 4 | Heart-yin deficiency syndrome (III) | 38.6% |
| 5 | Heart-yang deficiency syndrome (II) | 31.4% |
| 6 | Qi stagnation syndrome (VII) | 20.7% |
| 7 | Heart-kidney yang deficiency syndrome (IX) | 11.7% |
| 8 | Heart-fire hyperactivity syndrome (VIII) | 5.4% |
| 9 | Heart-blood deficiency syndrome (IV) | 2.9% |
| 10 | Cardiopulmonary-qi deficiency syndrome (X) | 2.5% |
Table 8.
RAD values of syndromes
| Li | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Lj | ||||||||||
| 1 | 0.00 | 0.01 | 0.81 | 0.69 | 0.62 | 0.64 | 0.59 | 0.60 | 0.03 | 0.71 |
| 2 | 0.01 | 0.00 | 0.08 | 0.06 | 0.33 | 0.30 | 0.27 | 0.10 | 0.97 | 0.00 |
| 3 | 0.51 | 0.10 | 0.00 | 0.13 | 0.44 | 0.38 | 0.31 | 0.60 | 0.09 | 0.43 |
| 4 | 0.03 | 0.01 | 0.01 | 0.00 | 0.03 | 0.02 | 0.02 | 0.03 | 0.00 | 0.00 |
| 5 | 0.49 | 0.50 | 0.55 | 0.44 | 0.00 | 0.55 | 0.50 | 0.43 | 0.46 | 0.79 |
| 6 | 0.80 | 0.73 | 0.75 | 0.63 | 0.87 | 0.00 | 0.84 | 0.53 | 0.63 | 0.86 |
| 7 | 0.20 | 0.18 | 0.17 | 0.13 | 0.22 | 0.23 | 0.00 | 0.33 | 0.11 | 0.14 |
| 8 | 0.05 | 0.02 | 0.08 | 0.06 | 0.05 | 0.04 | 0.09 | 0.00 | 0.02 | 0.07 |
| 9 | 0.01 | 0.36 | 0.03 | 0.00 | 0.11 | 0.10 | 0.06 | 0.03 | 0.00 | 0.00 |
| 10 | 0.03 | 0.00 | 0.03 | 0.00 | 0.04 | 0.03 | 0.02 | 0.03 | 0.00 | 0.00 |
High correlation of the syndromes
Relevant analysis of the relationships between syndromes found high correlations in heart-qi insufficiency, such as heart-yin deficiency, heart-blood deficiency, turbid phlegm, blood stasis, qi stagnation, heart-fire hyperactivity, and cardiopulmonary qi deficiency. For example, blood stasis was highly correlated with heart-qi insufficiency, heart-yang insufficiency, heart-yin deficiency, heart-blood deficiency, turbid phlegm, qi stagnation, heart-kidney yang deficiency, and cardiopulmonary qi deficiency. The one-way RAD values of these syndromes were 0.80, 0.73, 0.75, 0.63, 0.87, 0.84, 0.63, and 0.86, respectively.
The finding of high correlation of heart-qi insufficiency with heart-blood deficiency and heart-yin deficiency is consistent with CM theory that a long period of heart-qi insufficiency would result in yin blood, causing fluid and blood deficiency and then qi yin deficiency [25]. In consistency with this theory, qi yin deficiency syndrome was common. The correlations of heart-qi insufficiency with turbid phlegm, blood stasis, qi stagnation, heart-fire hyperactivity, and cardiopulmonary qi deficiency were high, and consistent with the feature of deficiency syndrome or excess syndrome of CHD [12,13]. According to CM theory [12,13], turbid phlegm, qi stagnation, and blood stasis are symptoms, while qi deficiency is the radical that causes heart vessel stagnation and then CHD. The high RAD values of turbid phlegm and cardiopulmonary qi deficiency would explain that cardiopulmonary qi deficiency causes retention of water and dampness, and then sputum and more turbid phlegm [12,13].
The high degree of correlation of blood stasis with heart-qi insufficiency, heart-yang insufficiency, heart-yin deficiency, heart-blood deficiency, turbid phlegm, qi stagnation, heart-kidney yang deficiency, and cardiopulmonary qi deficiency indicates that blood stasis appeared in these syndromes. According to CM theory [12,13], heart controlling the blood vessel, yang asthenia, and qi asthenia may cause degradation of driving blood ability, and then blood stasis. Heart-fire hyperactivity and heat scorching blood viscous may cause blood stasis [12,13]. Qi stagnation and poor blood flow may also cause blood stasis [12,13]. Blood stasis may be the basic pathogenesis of CHD [26].
One-way connection of the syndromes
Table 8 shows some syndrome pairs with obvious one-way connections. For example, the RAD value of heart-qi insufficiency to insufficiency of the heart blood was 0.69, but the reversed RAD value was only 0.03. The RAD value of heart-qi insufficiency to heart-fire hyperactivity was 0.60, while the reversed RAD was 0.05. Table 9 summarizes the one-way connections of the syndrome pairs.
Table 9.
One-way connections of the syndrome pairs
| Syndrome | RAD (L to R) | Syndrome | RAD (R to L) |
|---|---|---|---|
| Heart-blood deficiency syndrome | 0.687 | Heart-qi deficiency syndrome | 0.032 |
| Heart-fire hyperactivity syndrome | 0.600 | Heart-qi deficiency syndrome | 0.053 |
| Cardiopulmonary-qi deficiency syndrome | 0.714 | Heart-qi deficiency syndrome | 0.029 |
| Heart-fire hyperactivity syndrome | 0.600 | Heart-yin deficiency syndrome | 0.084 |
| Cardiopulmonary-qi deficiency syndrome | 0.785 | Turbid phlegm syndrome | 0.041 |
| Heart-blood deficiency syndrome | 0.625 | Blood stasis syndrome | 0.023 |
| Qi stagnation syndrome | 0.834 | Blood stasis syndrome | 0.227 |
| Heart-fire hyperactivity syndrome | 0.533 | Blood stasis syndrome | 0.037 |
| Heart-kidney yang deficiency syndrome | 0.630 | Blood stasis syndrome | 0.097 |
| Cardiopulmonary-qi deficiency syndrome | 0.857 | Blood stasis syndrome | 0.028 |
Taking heart-qi insufficiency and insufficiency of the heart blood as an example, CM theory [12,13] emphasizes the interdependence between qi and blood, and long-term qi insufficiencies will cause blood deficiency. However, insufficiency of the heart blood is not always accompanied by heart-qi insufficiency [12,13]. In elder patients, viscera function is weak, a pure sthenic syndrome is rare, and an asthenia with sthenia syndrome is more common. The RAD value of heart-qi insufficiency to heart-yin deficiency was 0.81, indicating that most CHD patients were qi asthenia together with yin asthenia. According to CM theory [12,13], heart-fire hyperactivity is not directly related to heart-qi insufficiency or insufficiency of heart-yin. High one-way connections were found for blood stasis to cardiopulmonary qi deficiency, insufficiency of the heart blood, heart-fire hyperactivity, qi stagnation, and heart-kidney yang deficiency. However, the RAD values of reversed connections were low, indicating that blood stasis was not the only reason for CHD.
Two-ways connections of the syndrome
In addition to the observations of one-way connections, two-way connections were also found. For example, the mutual RAD values of blood stasis and qi asthenia were 0.80 and 0.64, respectively, indicating that these two syndromes were highly correlated. CM theory [12,13] holds that qi asthenia and then poor blood flow would lead to blood stasis, in reverse. Long-term blood stasis may also cause qi asthenia. These two syndromes causally influence with each other.
Relationships between symptoms and syndromes
According to CM theory [12,13], a symptom is an expression of internal syndrome, and a syndrome is essential to symptom appearance. The RAD results (Table 10) calculated by equation (6) showed the one-way connections of symptoms to syndromes, whose connections could be viewed as the contributions of symptoms to syndromes.
Table 10.
Some RAD values between symptoms and syndromes
| Symptom | ||||||
|---|---|---|---|---|---|---|
| Syndrome | Chills |
Cold limbs |
Night sweat |
Palpitation |
Chest distress |
Chest pain |
| Heart-qi deficiency | 0.260 | 0.127 | 0.367 | 0.627 | 0.790 | 0.441 |
| Heart-yang deficiency | 0.592 | 0.437 | 0.310 | 0.684 | 0.782 | 0.546 |
| Heart-yin deficiency | 0.294 | 0.182 | 0.509 | 0.696 | 0.827 | 0.453 |
| Heart-blood deficiency | 0.250 | 0.250 | 0.250 | 0.625 | 0.750 | 0.250 |
| Turbid phlegm | 0.354 | 0.239 | 0.373 | 0.701 | 0.802 | 0.522 |
| Blood stasis | 0.348 | 0.216 | 0.344 | 0.652 | 0.787 | 0.512 |
| Qi stagnation | 0.374 | 0.235 | 0.400 | 0.670 | 0.739 | 0.522 |
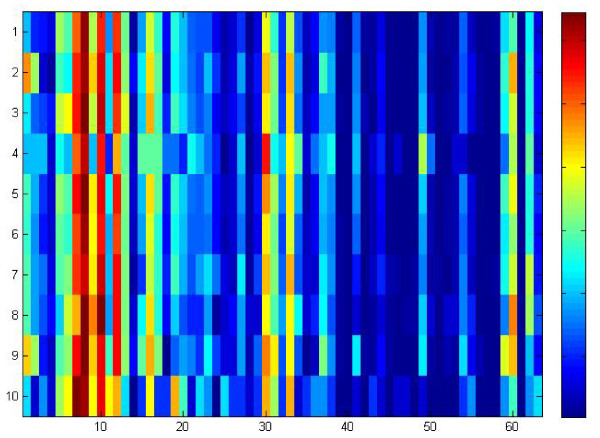
Figure 2 illustrates the data in Table 10, where the x-axis represents the 63 symptoms and the y-axis represents the 10 syndromes. Red rectangles represent high RAD values, and the blue ones represent low RAD values. From Figure 2, the correlations between symptoms and syndromes were determined. As shown in Figure 2, the symptoms of palpitation, chest distress, short breath, weakness, soreness, and weakness of waist and knees were related to most of the syndromes. At the same time, chills and some other symptoms showed strong connections to some syndromes, such as heart-kidney yang deficiency and yang asthenia. Table 11 lists the symptoms and syndromes with high and low RAD values. In Table 11, chills showed a low relation to most of the syndromes except for heart-yang insufficiency and heart-kidney yang deficiency, indicating that chills were closely related to the latter syndromes. CM theory [12,13] holds that weakness of yang and qi and lack of warmth may cause chills. The high RAD values of night sweats to insufficiency of heart-yin did confirm the CM theory that yang cannot be restricted by yin asthenia, and then deficiency fire will be an internal disturbance and cause night sweats [12,13]. Constipation and insufficiency of heart blood showed a strong connection. Inner Canon of Yellow Emperor points out that "people over 40 years old may lose half of the yin qi", and CM theory [12,13] holds that insufficiency of the heart blood causes body fluid deficiency, which in turn causes insufficient lubrication of the colon, leading to constipation. The strong connections between nocturnal frequent micturition and heart-kidney yang deficiency can be explained by the lack of yang in the heart and kidney which resulted in a decrease of the controlling and qi transformation functions, bladder retention failure, and then nocturnal frequent micturition.
Figure 2.
The RAD values of symptoms to syndromes.
Table 11.
Symptoms with relative high and low RAD values to syndromes
| Symptom | Syndrome |
|---|---|
| Strong relation | |
| Chills | Heart-yang deficiency syndrome, Heart-kidney yang deficiency syndrome |
| Night sweat | Heart-yin deficiency syndrome, Cardiopulmonary-qi deficiency syndrome |
| Cough | Cardiopulmonary-qi deficiency syndrome |
| Soreness and weakness of waist and knees |
Heart-blood deficiency syndrome |
| Constipation | Heart-blood deficiency syndrome |
| The frequent and increased urination at night |
Heart-kidney yang deficiency syndrome |
| Edema | Cardiopulmonary-qi deficiency syndrome |
| Chest pain | Heart-blood deficiency syndrome |
| Weak relation | |
| The frequent and increased urination at night |
Heart-blood deficiency syndrome, Cardiopulmonary-qi deficiency syndrome |
| Edema | Heart-blood deficiency syndrome |
The weak connections (Table 11) of chest pain and insufficiency of the heart blood, nocturnal frequent micturition and insufficiency of the heart blood, and edema and insufficiency of the heart blood were also significant and consistent with CM theory [12,13].
Symptom selection with RAD
In this study, RAD was used for symptom selection, and then SVM [23] and K-nearest neighbours (KNN) [24] were used for the prediction.
Table 11 shows individual contributions of symptoms to the syndromes.
The predictions were not sound as the syndromes 4, 8, 9, and 10 in this data set showed serious imbalance; therefore, we omitted these results. For syndromes 1, 2, 3, 5, 6, and 7, (Table 12), the results were much better. Table 12 indicates that the prediction results with MRMR favoured either the positive class or the negative class. In the G-means results of the syndromes, these maximum values were obtained by the RAD method, indicating that RAD achieved a good balance between the positive class and the negative class. Although for some syndromes, the prediction results of RAD and MRMR were close when the TPR, TNR, and G-means values were all considered. In general, the results obtained by RAD were more reasonable.
Table 12.
Statistical Results of TPR, TNR and G-means by using SVM and KNN with RAD and MRMR or without symptom selection
| Syndrome | 1 | 2 | 3 | 5 | 6 | 7 | Average | |
|---|---|---|---|---|---|---|---|---|
| No Symptom Selection- SVM |
TPR | 0.708 | 0.463 | 0.729 | 0.472 | 0.799 | 0.906 | 0.680 |
| TNR | 0.411 | 0.770 | 0.535 | 0.602 | 0.516 | 0.667 | 0.583 | |
| G-m | 0.539 | 0.597 | 0.625 | 0.533 | 0.642 | 0.777 | 0.630 | |
| RAD-SVM | TPR | 0.723 | 0.518 | 0.786 | 0.588 | 0.796 | 0.771 | 0.713 |
| TNR | 0.429 | 0.781 | 0.547 | 0.536 | 0.592 | 0.865 | 0.609 | |
| G-m | 0.557 | 0.636 | 0.656 | 0.561 | 0.686 | 0.817 | 0.652 | |
| MRMR-SVM | TPR | 0.955 | 0.337 | 0.131 | 0.412 | 0.955 | 0.020 | 0.468 |
| TNR | 0.070 | 0.893 | 0.970 | 0.704 | 0.027 | 0.970 | 0.606 | |
| G-m | 0.259 | 0.549 | 0.356 | 0.539 | 0.161 | 0.141 | 0.334 | |
| No Symptom Selection- KNN |
TPR | 0.757 | 0.553 | 0.439 | 0.461 | 0.826 | 0.534 | 0.595 |
| TNR | 0.380 | 0.795 | 0.732 | 0.657 | 0.673 | 0.784 | 0.670 | |
| G-m | 0.536 | 0.663 | 0.567 | 0.550 | 0.746 | 0.647 | 0.631 | |
| RAD-KNN | TPR | 0.749 | 0.670 | 0.509 | 0.485 | 0.887 | 0.522 | 0.607 |
| TNR | 0.391 | 0.712 | 0.729 | 0.663 | 0.704 | 0.851 | 0.706 | |
| G-m | 0.541 | 0.691 | 0.601 | 0.567 | 0.790 | 0.667 | 0.643 | |
| MRMR-KNN | TPR | 1.000 | 0.401 | 0.170 | 0.354 | 0.942 | 0.161 | 0.505 |
| TNR | 0.146 | 0.901 | 0.981 | 0.783 | 0.018 | 0.897 | 0.621 | |
| G-m | 0.382 | 0.601 | 0.409 | 0.526 | 0.130 | 0.379 | 0.405 | |
Conclusions
The RAD method is effective for CM clinical data analysis, particular for analysis of relationships between symptoms in diagnosis and generation of compact and comprehensible symptom feature subsets.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GZL designed the study, supervised the data analysis, and organized discussion of the results. MYY designed the experiment and write the manuscript. SS dedicated in experiment results analysis and manuscript revision. YLW implemented the analysis method and performed the experiments. GPL participated into analysis implementation, data acquisition, and result discussion. All authors read and approved the final manuscript.
Contributor Information
Guo-Zheng Li, Email: gzli@tongji.edu.cn.
Sheng Sun, Email: sunsheng0201@126.com.
Mingyu You, Email: myyou@tongji.edu.cn.
Ya-Lei Wang, Email: liamwangcn@gmail.com.
Guo-Ping Liu, Email: tianshanghuo3838@163.com.
Acknowledgements
This work was supported by the National Natural Science Foundation of China under grant Nos. 30901897 and 61005006, as well as the Fundamental Research Funds for the Central Universities.
References
- Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom's General Practice Research Database. Arch Gen Psychiatry. 2007;64(2):242–249. doi: 10.1001/archpsyc.64.2.242. [DOI] [PubMed] [Google Scholar]
- Zhang S, Song YQ, Wang Y. Multicentric randomized double blinded clinical study of Yiqi Tongmai Oral Liquid against angina pectoris in patients with coronary heart disease (in Chinese) J Chin Integr Med. 2007;4:383–391. doi: 10.3736/jcim20070405. [DOI] [PubMed] [Google Scholar]
- Sheng F, Jiang J, Zheng X, Zhang XF. Introduction of clinical research methods for differential treatment and individual treatment of TCM China. J Tradit Chin Med Pharm. 2011;1:115–118. [Google Scholar]
- Huang T, Gao Y. Review on application of data mining technology in TCM pattern study. Acta Univ Tradit Med Sinensis Pharmacol Shanghai. 2010;1:85–87. [Google Scholar]
- Li YB, Huang XY. International Conference on Machine Learning and Cybernetics: 4-5 November 2002: Beijing. New York: IEEE; 2002. Traditional Chinese medicine recognition based on FNN; pp. 298–302. [Google Scholar]
- Wang Y, Ma LZ, Liao XW, Liu P. IEEE International Symposium on IT in Medicine and Education:12-14 December 2008; Xiamen. New York: IEEE; 2008. Decision tree method to extract syndrome differentiation rules of posthepatitic cirrhosis in traditional Chinese medicine; pp. 744–748. [Google Scholar]
- Zhang Q, Zhang WT, Wei JJ, Wang XB, Liu P. Combined use of factor analysis and cluster analysis in classification of traditional Chinese medical syndromes in patients with posthepatitic cirrhosis. J Chin Integr Med. 2005;3:14–18. doi: 10.3736/jcim20050105. [DOI] [PubMed] [Google Scholar]
- Zhang NL, Yuan SH, Chen T, Wang Y. Latent tree models and diagnosis in traditional Chinese medicine. Artific Intell Med. 2008;42:229–245. doi: 10.1016/j.artmed.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Feng Y, Wu ZH, Zhou XZ, Zhou ZM, Fan WY. Knowledge discovery in traditional Chinese medicine: state of the art and perspectives. Artific Intell Med. 2006;38:219–236. doi: 10.1016/j.artmed.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Qin ZG, Mao ZY, Deng ZZ. The application of rough set in the Chinese medicine rheumatic arthritis diagnosis. Chin J Biomed Engr. 2001;20:357–363. [Google Scholar]
- Wang XW, Qu HB, Liu P, Cheng YY. A self-learning expert system for diagnosis in traditional Chinese medicine. Expert Syst Appl. 2004;26:557–566. doi: 10.1016/j.eswa.2003.10.004. [DOI] [Google Scholar]
- Deng TT. Diagnostics of TCM. Shanghai: Shanghai Scientific and Technology Press; 1984. [Google Scholar]
- Wang YQ. Diagnostics of TCM. Beijing: Chinese Medicine Science and Technology Press; 2004. [Google Scholar]
- Wang J, He QY, Yao KW, Rong W, Xing YW, Yue Z. In: Fifth International Conference on Natural Computation:14-16 August 2009;Tianjian. Wang HY, Low KS, Wei KX, Sun JQ, editor. Los Alamitos: IEEE Computer Society; 2009. Support vector machine (SVM) and traditional Chinese medicine: syndrome factors based an SVM from coronary heart disease treated by prominent traditional Chinese medicine doctors; pp. 176–180. [Google Scholar]
- Liu GP, Li GZ, Wang YL, Wang YQ. Modelling of inquiry diagnosis for coronary heart disease in traditional Chinese medicine by using multi-label learning. BMC Complement Altern Med. 2010;10:4–37. doi: 10.1186/1472-6882-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X, Chen S, Liu B, Zhang R, Wang Y, Li P, Guo Y. Development of traditional Chinese medicine clinical data warehouse for medical knowledge discovery and decision support. Artif Intell Med. 2010;48:139–152. doi: 10.1016/j.artmed.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Jolliffe IT. Principal component analysis. New York: Springer-Verlag; 1986. [Google Scholar]
- Helland IS. PLS regression and statistical models. Scand J Stat. 1990;17:97–114. [Google Scholar]
- Peng HC, Long F, Ding C. Feature selection based on mutual information: criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans Pattern Analy Mach Intell. 2005;8:1226–1238. doi: 10.1109/TPAMI.2005.159. [DOI] [PubMed] [Google Scholar]
- Lu XM, Xiong ZL, Li JJ, Zheng SN, Huo TG, Li FM. Metabonomic study on 'Kidney-Yang Deficiency syndrome' and intervention effects of Rhizoma Drynariae extracts in rats using ultra performance liquid chromatography coupled with mass spectrometry. Talanta. 2011;15:700–708. doi: 10.1016/j.talanta.2010.09.026. [DOI] [PubMed] [Google Scholar]
- Hu XH, Wu D. Data mining and predictive modeling of biomolecular network from biomedical literature databases. IEEE/ACM Trans Comput BiolBioinform. 2007;4:251–263. doi: 10.1109/TCBB.2007.070211. [DOI] [PubMed] [Google Scholar]
- Kerstin D, Wolfgang N. How valuable is medical social media data? Content analysis of the medical web. Inform Sci. 2009;179:1870–1880. doi: 10.1016/j.ins.2009.01.025. [DOI] [Google Scholar]
- Burges JC. A tutorial on support vector machines for pattern recognition. Data Mining Knowl Discov. 1998;2:121–167. doi: 10.1023/A:1009715923555. [DOI] [Google Scholar]
- Cover TM, Hart PE. Nearest neighbor pattern classification. IEEE Transact Informat Theory. 1967;1:21–27. [Google Scholar]
- Yuan ZK, Huang XP, Fan FY. Analysis of the tounge micro-indexes of qi-blood Patterns of Heart Disorders. J Tradit Chin Med Univ Hunan. 2004.
- Bernardini S, Bertolini S, Pastore A, Cortese C, Motti C, Massoud R, Federici G. Homocysteine levels are highly predictive of CHD complications in subjects with familial hypercholesterolemia. Clin Chem Lab Med. 1999;255 [Google Scholar]