Abstract
Background
We have previously performed a genome-wide linkage study in Scandinavian Type 1 diabetes (T1D) families. In the Swedish families, we detected suggestive linkage (LOD≤2.2) to the chromosome 5p13-q13 region. The aim of our study was to investigate the linked region in search for possible T1D susceptibility genes.
Methodology/Principal Findings
Microsatellites were genotyped in the Scandinavian families to fine-map the previously linked region. Further, SNPs were genotyped in Swedish and Danish families as well as Swedish sporadic cases. In the Swedish families we detected genome-wide significant linkage to the 5-hydroxytryptamine receptor 1A (HTR1A) gene (LOD 3.98, p<9.8×10−6). Markers tagging two separate genes; the ring finger protein 180 (RNF180) and HTR1A showed association to T1D in the Swedish and Danish families (p<0.002, p<0.001 respectively). The association was not confirmed in sporadic cases. Conditional analysis indicates that the primary association was to HTR1A. Quantitative PCR show that transcripts of both HTR1A and RNF180 are present in human islets of Langerhans. Moreover, immunohistochemical analysis confirmed the presence of the 5-HTR1A protein in isolated human islets of Langerhans as well as in sections of human pancreas.
Conclusions
We have identified and confirmed the association of both HTR1A and RFN180, two genes in high linkage disequilibrium (LD) to T1D in two separate family materials. As both HTR1A and RFN180 were expressed at the mRNA level and HTR1A as protein in human islets of Langerhans, we suggest that HTR1A may affect T1D susceptibility by modulating the initial autoimmune attack or either islet regeneration, insulin release, or both.
Introduction
The incidence of Type 1 diabetes (T1D) is rapidly increasing around the world [1] and Sweden has one of the highest incidence rates of T1D [2]. T1D is an autoimmune disease which is characterised by gradual destruction of insulin producing beta-cells located in the pancreas.
The detailed aetiology of T1D is still unknown, yet it is understood that both environmental and genetic factors contribute to disease susceptibility. Studies have identified more than 40 susceptibility loci for T1D [3]. The Major Histocompatibility Complex (MHC) on chromosome 6 is known to be the key T1D susceptibility region accounting for more than 50% of the total genetic risk. Other T1D susceptibility genes include the insulin gene (chromosome 11p5), the CTLA-4 gene (chromosome 2q33), IL2RA (chromosome 10p15), IFIH1 (chromosome 2q24) and the PTPN22 gene (chromosome 1p13) [3]. However, the identified T1D susceptibility genes and gene regions do not explain all of the genetic risk. This could be due to gene-gene and gene-environment interactions, epigenetic effects but also due to so far unidentified susceptibility genes.
We have in a previous genome-wide linkage study detected suggestive linkage (LOD<2.2) to the chromosome 5p13-q13 region in a Scandinavian T1D family material [4]. In the present study we narrowed the region of linkage and identified associated markers in the 5-hydroxytryptamine (serotonin) receptor 1A (HTR1A) and the ring finger protein 180 (RNF180) genes. We then confirmed this association in independent materials. Further we have detected HTR1A and RNF180 expression in human pancreatic islets of Langerhans.
Methods
Ethics Statement
The ethics committees at Karolinska Insitutet, Umeå University, Copenhagen University and Oslo University have approved blood sampling for the purpose of genetic analyses for the current study. Oral or written consent was obtained from the patients, controls or their guardians.
Further, the ethics committee at Lund University has approved the sampling of pancreases of organ donors who have approved the use of their organs for medical research according to the organ donor register.
Patients and Controls
Scandinavian families
The Swedish families consist of 184 multiplex and 9 simplex Swedish families, including a total of 200 affected T1D sib-pairs. The Danish family material consist of 147 multiplex and 5 simplex families with 175 affected sib-pairs, while the Norwegian material consists of 77 multiplex and 2 simplex families with 89 affected sib-pairs [4] (Table 1).
Table 1. T1D data materials.
| Category | Swedish | Danish | Norwegian |
| Sib pairs: | |||
| Affected | 200 | 175 | 89 |
| Unaffected | 53 | 135 | 23 |
| Discordant | 277 | 287 | 123 |
| Multiplex families | 184 | 147 | 77 |
| Simplex | 9 | 5 | 2 |
| Age at onset median(range) | 14 (0–53) | 13 (0–71) | 12 (1–52) |
| DISS2 | BDD | MS | |
| Cases | 778 | 2300 | – |
| Controls | 836 | – | 527 |
| T1D at onset (%) | 76.2 | 95 | – |
| Age/age onset median | 25 | 10 | |
| (range) | (15–34) | (0–19) | (18–70) |
Only healthy controls were used from the Epidemiological Investigations in Multiple Sclerosis (EIMS) study.
Diabetes Incidence Study in Sweden 2 (DISS2)
The Diabetes Incidence Study in Sweden consists of 778 patients with diabetes and 836 matched controls identified through the diabetes incidence study register. The incident DISS2 patients were between 15 and 34 years. At follow-up visits 528 patients were classified with T1D [5]. The remaining 250 patients were classified as type 2 diabetes patients, secondary diabetes or unclassified diabetes patients and were therefore excluded from our study.
Better Diabetes Diagnosis Study (BDD)
The BDD cohort consists of 2742 newly diagnosed diabetes patients. All patients were less than 18 years of age at the time of diagnosis. Patients were recruited between May 2005 and September 2009 from 40 pediatric clinics in Sweden [6]. At follow up, 95% of the patients were classified as T1D while the remaining 5% were classified with type 2, MODY, secondary, “other” or “unknown” type of diabetes. All patients of non-European descent were excluded from the cohort. In the current study we have included 2300 T1D patients from the BDD cohort.
Multiple Sclerosis (MS) controls
We have included 527 healthy controls between the ages of 18–70 years from an ongoing population based case control study of multiple sclerosis (MS) called EIMS (Epidemiological Investigations in Multiple Sclerosis) in our analysis. Controls were matched for age, gender and residential area to incident MS cases throughout Sweden [7].
Genetic Fine-mapping of Chromosome 5
Microsatellite genotyping
Fine mapping of chromosome 5 was performed by typing microsatellites in the Scandinavian families. A total of 40 microsatellite markers were selected from NCBI (http://www.ncbi.nlm.nih.gov/), GDB (http://gdbwww.gdb.org/), and Marshfield (http://research.marshfieldclinic.org/genetics/). PCR conditions and quality controls were as described [4].
SNP genotyping
For genotyping of Single Nucleotide Polymorphisms (SNPs) a total of 67 SNPs were selected with an average spacing of 10–30 kb and a minor allele frequency above 0.3. A lower rare allele frequency was only accepted for SNPs within genes. Fifteen SNPs were chosen in possible functional candidate T1D susceptibility genes in the 5p13-q13 region (Table S1). All SNPs were genotyped either using Pyrosequencing (Pyrosequence Inc., Sweden) [8] or the TaqMan method (Applied Biosystems Inc., Sweden) as described [9].
All SNPs in the MS controls were genotyped using the Human660-Quad chip as described [10].
DNA sequencing
Due to the lack of identified SNPs in HTR1A, sequencing of the gene and its flanking regions was performed using the ABI Prism 3730 Genetic Analyser method (Applied Biosystems Inc., Sweden). DNA from six T1D patients (four patients carrying a HTR1A T1D risk haplotype and two carrying a non-risk haplotype) and five controls (two controls with the T1D risk haplotype and three without) were sequenced. Haplotypes were defined through previously typed SNPs using the GeneHunter program. The 11 756 bp long DNA sequence was divided into approx. 1 000 bp segments. Primer sequences are available on request. Primers were obtained from DNA Technology A/S (Risskov, Denmark). Sequencing was performed in ABI the Prism 3730 Genetic Analyser and the results were analysed in the SeqScape software, v. 2.5 (Applied Biosystems Inc., Sweden).
Statistical Analysis
All microsatellite markers were mapped to the chromosome 5p13-q13 region using CRIMAP [11]. Mendelian consistencies, excess of homozygosity (Hardy-Weinberg equilibrium) and allele frequencies for the analysed SNPs and microsatellites in the families were estimated using the zGenStat program (H. Zazzi, unpublished). Linkage was assessed by non-parametric linkage methods (ALLEGRO [12]). Single- and multi-point linkage analyses were performed using the exponential model with equal weighing. Combined analysis of linkage and association as well as identifying SNPs responsible for linkage was performed in the Linkage and Association Modeling in Pedigrees (LAMP) software program [13]. The LD structure and tagging of SNPs were analyzed in Haploview [14]. LD blocks were identified using all three block definitions with similar results. Hardy-Weinberg equilibrium was tested among controls only. Single SNP and haplotype association as well as conditional association analysis were assessed using the Unphased computer program (version 3.0.6) [15]. Study cohort was used as a confounder in the combined association analyses.
Imputation
Imputation of the rs6295, rs356570 and rs6880454 SNPs among the MS controls was performed using the MaCH v. 1.0.16 analysis program with default settings [16]. Previous SNP genotyping results from the MS Genome wide association (GWAS) study were used. Quality controls of typed SNPs included checking for call-rates (per sample and per SNP), heterozygosity, recent shared ancestry, non-European ancestry, MAF and deviation from Hardy-Weinberg equilibrium [10].
Human Islet Donor Material
Human islets were obtained from the Nordic Network for Clinical Transplantation, Uppsala and distributed by the Human tissue laboratory at Lund University Diabetes Center, Malmö, Sweden.
Quantitative-PCR of HTR1A and RNF180 mRNA from Human Islets of Langerhans
mRNA was prepared from human islets of Langerhans from a total of 10 healthy age and gender matched donors using mRNA Easy Plus mini kit, (Qiagen, Hilden, Germany). cDNA was obtained by reverse transcription (Maxima ™ First Strand cDNA Synthesis Kit, Fermentas, Thermo Scientific, Sweden). The mRNA levels were quantified using a Probe/Rox Real-Time PCR (Maxima™ Probe/ROX qPCR Master Mix (2X), Fermentas, Thermo Scientific, Sweden) with an ABI PRISM 7900 (Applied Biosystems, Inc., Sweden), and assays-on-demand were employed for HTR1A (Hs 00265014) and RNF180 (Hs 00400379) (Applied Biosystems Inc., Sweden). Each sample was run in duplicate, and the transcript quantity was normalized to the mRNA level of cyclophilin A (Hs 01565700, PPIA), polymerase 2 (Hs 00172187, POL2A) and hypoxanthine guanine phosphoribosyl transferase (Hs 01003267, HPRT) (Applied Biosystems).
Tissue Preparation and Immunohistochemistry
For histochemical analyses human islets and biopsies from human pancreas were fixed overnight in Stefanini’s solution (2% paraformaldehyde and 0.2% picric acid in 0.1 M phosphate buffered saline, pH 7.2), rinsed thoroughly in Tyrode solution containing 10% sucrose and frozen on dry ice. Sections (10 µm) were cut and thaw-mounted on slides. Antibodies were diluted in phosphate buffered saline (pH 7.2) containing 0.25% bovine serum albumin and 0.25% Triton X-100. Sections were incubated with primary antibodies (goat anti- 5HTR1A; code sc-1459; dilution 1∶100 (Santa Cruz Biotech. Inc., CA USA), guinea pig anti-proinsulin; code 9003; dilution 1∶2560; EuroDiagnostica, Malmö, Sweden), and rabbit anti-glucagon; code 7811; dilution 1∶5000 (EuroDiagnostica) overnight at 4°C in moisturizing chambers. The specificity of immunostaining was tested using primary antisera pre-absorbed with homologous antigen (100 µg of peptide per ml antiserum at working dilution). Immunofluorescence was examined in an epi-fluorescence microscope (Olympus, B×60). By changing filters the location of the different secondary antibodies in double staining was determined. Images were captured with a digital camera (Nikon DS-2Mv).
Computational Analysis
The web based software RAVEN (www.cisreg.ca/cgi-bin/RAVEN/a) was used for detecting potential transcription factor binding sites.
Results
Fine-mapping of Chromosome 5p13-q13 and HTR1A Sequencing
The region on chromosome 5 (5p13-q13) which previously showed suggestive linkage [4] was narrowed down by genotyping additional microsatellites and SNPs located in the area, in separate cohorts.
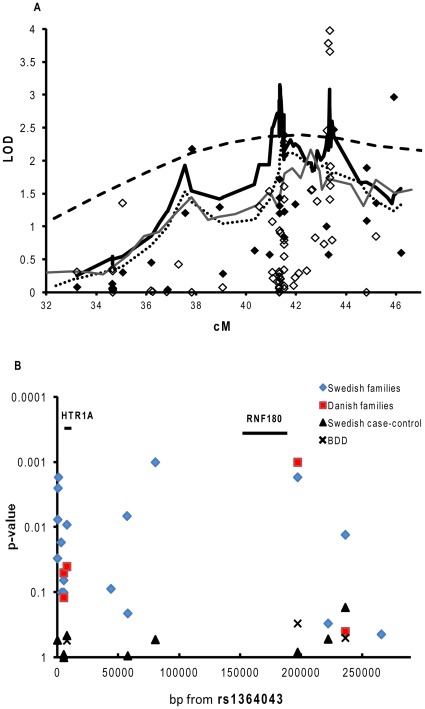
We first typed an additional 36 microsatellites in the Scandinavian families. A region of 20.6 cM between the microsatellites D5S407 and D5S428 showed strongest support for linkage (LOD 2.16, p<0.0008). In the single point analysis, using the exponential equal weighting model, D5S2048 reached a LOD of 2.97 (p<0.0002). The added evidence for linkage to this region provided by the Danish and Norwegian families was modest (LOD 0.68 p<0.04 and LOD 0.22 p<0.16). We therefore decided to perform further analysis in the Swedish families by typing four additional microsatellites. D5S2000 showed strongest linkage in a multipoint analyses (LOD 2.70, approx 41.5 cM, Figure 1a).
Figure 1. a–b. Linkage and association analysis in Scandinavian families and case-control cohort.
Linkage analysis of T1D on chromsome 5 in Swedish, -Danish and -Norwegian multiplex families (a). The dashed line represents multipoint linkage from the original scan in the Swedish, Danish and Norwegian families [4]. The thin dark grey line represents the “fine mapping” including 36 microsatellites in all Scandinavian families. A region between D5S407 and D5S428 (at approx 41.5 cM in figure) showed a linkage of LOD 2.16. The dotted line represents the Swedish families using all 40 microsattelites (multipoint). Here, D5S2000 showed strongest linkage (LOD 2.70). The black diamonds represent the “fine mapping” single point analysis in the Swedish families. In the singlepoint analysis for the Swedish families, D5S2048 showed strong linkage (LOD 2.97). The black thick line represents linkage in Swedish families to T1D on chromosome using an extra 4 microsattelites and 61 SNPs, reveiling three linked peaks where the most strongly linked region was the 5p13-q13 (at approx 43 cM on figure) region (LOD 2.7 for rs6295). In the singlepoint analysis using all 61 SNPs and 4 extra microsattelites (white diamonds) rs878567 and rs6295 showed genome-wide significant linkage (LOD 3.9 and LOD 3.65 respectively). Linkage was calculated using the Exponential Equal Weighting model in the Allegro program.SNP association for the Swedish sporadic cases and controls and Swedish and Danish multiplex families (b) was calculated from rs1158292 (63 001 317 bp) to rs6880454 (63 5028 02 bp). Swedish families (diamonds). Danish families (squares), DISS2 (triangles) and BDD (crosses). Association analysis was carried out in the Unphased program. For the BDD cohort, association was calculated using controls included in the Swedish (MS) EIMS study.
We next chose to genotype 61 evenly distributed SNPs across the 50 695 kb–63 532 kb region which was the region showing strongest evidence of linkage. Genotyping results revealed three linked regions (Figure 1a). The region showing strongest linkage (5p13-q13) contained the HTR1A gene. Two SNPs; rs878567 and rs6295, which are located on either side of HTR1A, displayed genome wide significant linkage of LOD 3.98, p<9.8×10−6 and LOD 3.66, p<2×10−5 (Figure 1a). Also, rs749099 located downstream of HTR1A showed significant linkage (LOD 3.78, p<1.5×10−5).
In the Swedish families, significant association was observed for the rs6295 SNP (p<0.01) which is located in very close proximity to HTR1A (1019 bp upstream of HTR1A). Also, several other SNPs in the HTR1A region showed association to T1D (Table 2 and Figure 1b), suggesting that HTR1A is a T1D susceptibility gene. Additionally, it was seen that rs356570, 190 kb upstream of HTR1A is associated to T1D (p<0.002).
Table 2. Association to the chromosome 5p13 region in Swedish multiplex/simplex families.
| Marker name | Location bp | Minor Allele | Minor allele frequency | Call rate % | p-value |
| rs1158292 | 63 001 317 | A | 0.38 | 93 | 0.2 |
| rs1364043 | 63 266 735 | G | 0.22 | 89 | 0.03 |
| rs970453 | 63 266 983 | C | 0.46 | 87 | 0.008 |
| rs72767932 | 63 267 175 | G | 0.14 | 88 | 0.003 |
| rs1423691 | 63 267 546 | C | 0.48 | 84 | 0.002 |
| rs749099 | 63 269 720 | T | 0.45 | 94 | 0.02 |
| rs749098 | 63 270 176 | G | 0.20 | 85 | 0.1 |
| rs878567 | 63 271 875 | C | 0.50 | 91 | 0.06 |
| rs6449693 | 63 271 902 | A | 0.50 | 95 | 0.1 |
| rs6295 | 63 274 449 | G | 0.49 | 90 | 0.01 |
| rs1364041 | 63 324 375 | G | 0.12 | 97 | 0.2 |
| rs382098 | 63 310 581 | C | 0.48 | 89 | 0.08 |
| rs749100 | 63 323 746 | C | 0.41 | 95 | 0.007 |
| rs356562 | 63 346 993 | A | 0.4 | 95 | 0.001 |
| rs356570 | 63 463 673 | G | 0.37 | 89 | 0.002 |
| rs12697015 | 63 4886 95 | C | 0.15 | 98 | 0.3 |
| rs6880454 | 63 502 802 | T | 0.08 | 95 | 0.01 |
| rs11949052 | 63 532 300 | A | 0.14 | 98 | 0.4 |
SNP location (bp) was obtained from “HapMap Data Rel 19/phasell Oct 05, on NCBI B34 assembly, dbSNP b124” in HapMap.
Minor allele frequencies and p-values for the Swedish multiple/simplex families were obtained from Unphased v. 3.0.6. Hardy-Weinberg (H–W) values were calculated amongst controls.
When the LAMP software was used to confirm our observed linkage for rs6295, suggestive linkage of LOD 2.4 (p<0.01) was observed for the rs6295 SNP. Further, when test for association was performed for rs6295 a LOD of 3.1 and p<1.6×10−4 was observed, suggesting that this SNP is responsible for the observed linkage.
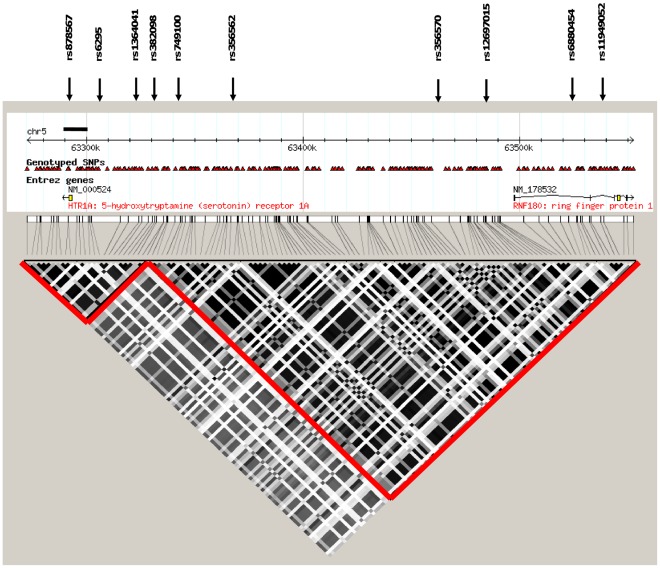
No SNPs in the coding sequence of HTR1A were found in Ensemble or dbSNP. Therefore, in the search for possible unidentified SNPs, sequencing of the HTR1A gene and promoter was carried out. In an 11 756 bp long region around HTR1A, we sequenced 9 low risk haplotypes and 10 high risk haplotypes identified by haplotype association in the Swedish famililes. Through the sequencing, six previously identified and genotyped SNPs (rs1364043, rs1423691, rs749099, rs878567, rs6449693 and rs6295) were confirmed. Further, three SNPs which had not been published in a public data base at the time of the study, were identified (rs1364043, rs970453 and rs749098) and genotyped in the Swedish families. Using the Haploview program for LD block identification, it was seen that all of these SNPs are located within the same LD block (Figure 2). No SNPs in the coding sequence of the HTR1A gene were identified.
Figure 2. LD plot for HTR1A and RNF180.
LD-block of the HTR1A and RNF180 regions was obtained from Haploview using HapMap data. The linkage disequilbrium measure shown is r2 and the block definition is solid spine defined by Gabriel et al., [35]. HTR1A and RNF180 are situated in two separate blocks (r2 = 0.91 between the two blocks). When LD for the two associated SNPs (rs356570 and rs6880454) is calculated we observe a D́ value of 1 while r2 is 0.021. The SNPs in bold were typed to verify the involvement of RNF180 to T1D susceptibility. Rs12697015 tags three other SNPs located in the RNF180 downstream region. rs6880454 tags 17 additional SNPs on either side of RNF180. rs11949052 only tags for itself. Standard settings were used for tagging anlysis in Haplowiev. The bold lines indicate the HTR1A sequenced area.
Using the Haploview program and genotypes in the 63 280 kb to 63 560 kb region from individuals with European ancestry from the HapMap project, we saw that rs356570 tags for 71 SNPs located further upstream of HTR1A. A number of these SNPs are located within or around the RNF180 gene, suggesting that this gene could be involved in T1D susceptibility as well. It was also seen that the region between HTR1A and RNF180 has very high LD (Figure 2).
To test the involvement of RNF180 in the susceptibility to T1D, another three SNPs in or around RNF180 were genotyped in the Swedish family material (Figure 1b). Genotyping analysis revealed significant association between T1D and rs6880454 (p<0.01 Table 2).
Confirmation in Independent Cases and Controls
For confirmation of association, we genotypes markers in, Danish families and two collections of sporadic Swedish T1D cases; DISS2 and BDD material (Table 3).
Table 3. Association to the chromosome 5p13 region in Danish multiplex/simplex families, BDD cohort and the Swedish case-control material.
| Marker name | Danish families | Swedish-Danish families | Swedish case-control | BDD cohort | MS controls | Pooling of data | |||||||
| Patients | Controls | Patients | Controls | ||||||||||
| n = 778 | n = 836 | n = 2700 | n = 527 | ||||||||||
| Minor allele frequency | Call rate % | p-value | p-value | Genotypefrequency% AA/AB/BB | Genotypefrequency% AA/AB/BB | Call rate% | p-value | Genotypefrequency% AA/AB/BB | Call rate% | Genotypefrequency% AA/AB/BB | p-value | p-value | |
| rs1364043 | 59.5/35.3/5.1 | 61.4/33.6/4.9 | 93 | 0.5 | |||||||||
| rs878567 | 0.50 | 95 | 0.05 | 0.015 | 25.6/49.9/24.5 | 24.4/51.8/23.8 | 89 | 0.9 | |||||
| rs6449693 | 0.50 | 93 | 0.06 | 0.04 | 25.6/50.2/24.1 | 25.9/49.6/24.4 | 81 | 0.9 | |||||
| rs6295 | 0.50 | 92 | 0.04 | 0.003 | 27.5/50.9/21.6 | 26.6/49.6/23.8 | 89 | 0.4 | 27.2/50.0/22.9 | 95 | 26.6/50.1/23.4 | 0.4 | 0.01 |
| rs1364041 | 77.7/20.6/1.7 | 78.2/19.7/2.0 | 83 | 0.8 | |||||||||
| rs356562 | 37.5/49.3/13.3 | 37.3/47.2/15.5 | 94 | 0.5 | |||||||||
| rs356570 | 0.38 | 95 | 0.001 | 8.5×10−5 | 38.8/48.6/12.6 | 39.5/46.5/14.0 | 94 | 0.8 | 40.8/45.3/13.9 | 97 | 41.5/44.4/14.1 | 0.6 | 0.003 |
| rs12697015 | 73.1/25.3/1.6 | 71.9/26.0/2.2 | 93 | 0.5 | |||||||||
| rs6880454 | 0.07 | 91 | 0.5 | 0.02 | 82.8/15.5/1.7 | 83.5/15.1/1.4 | 70 | 0.2 | 82.3/16.8/1.1 | 95 | 83.1/16.1/0.8 | 0.5 | 0.05 |
Allele frequencies and p-values for the Danish multiplex-simplex families and p-values for the Swedish cases-control and BDD studies were obtained from Unphased v. 3.0.6. P-values for the BDD cohort were obtained using controls from the Swedish MS case-control study.
Genotype frequencies and p-values for the genotype test were obtained by using chi2 test.
In the Danish families, rs6295 showed modest association (p<0.04). However, a stronger association was observed between T1D and rs356570 (p<0.001). No individual SNP showed association to T1D (Table 3, Figure 1b) in the Swedish DISS2 or BDD materials. Pooling of all four materials revealed that both rs6295 and rs356570 were associated with T1D (p<0.01 and p<0.003 respectively). Further, rs6880454 showed suggestive association of p<0.05.
Two haplotypes in the HTR1A and RNF180 area in the Swedish and Danish families; a haplotype containing rs6295 (C) – rs356570 (A) – rs6880454 (G) showed positive association to T1D (p<0.002 and p<0.05 respectively) while haplotype rs878567 (T) – rs6449693 (G) – rs6295 (G) – rs356570 (G) showed protective association (p<0.03 and p<0.02, Table 4). No haplotype association was observed in the sporadic cases nor when all four materials were pooled.
Table 4. Haplotype association; Swedish – and Danish families.
| Family material | Haplotype | p-value |
| rs6295 -rs356570- | rs6880454 | |
| Swedish families | C-A-G | 0.0013 |
| Danish families | C-A-G | 0.048 |
| rs878567-rs6449693-rs6295- | rs356570 | |
| Swedish families | T-G-G-G | 0.025 |
| Danish families | T-G-G-G | 0.018 |
To see whether the two genes, HTR1A and RNF180 were associated independently of each other, a conditional analysis was performed. When the two family materials were pooled, the rs6295 marker which maps close to HTR1A was associated independently of markers in RNF180 (p<0.04). RNF180 showed no association independently of HTR1A.
For HTR1A an analysis in the RAVEN program revealed that the rs6295 SNP positioned next to the HTR1A gene is located in a binding site for two transcription factors; Irf-1 and NRF-2.
Quantitative-PCR of HTR1A and RNF180 mRNA from Human Islets of Langerhans
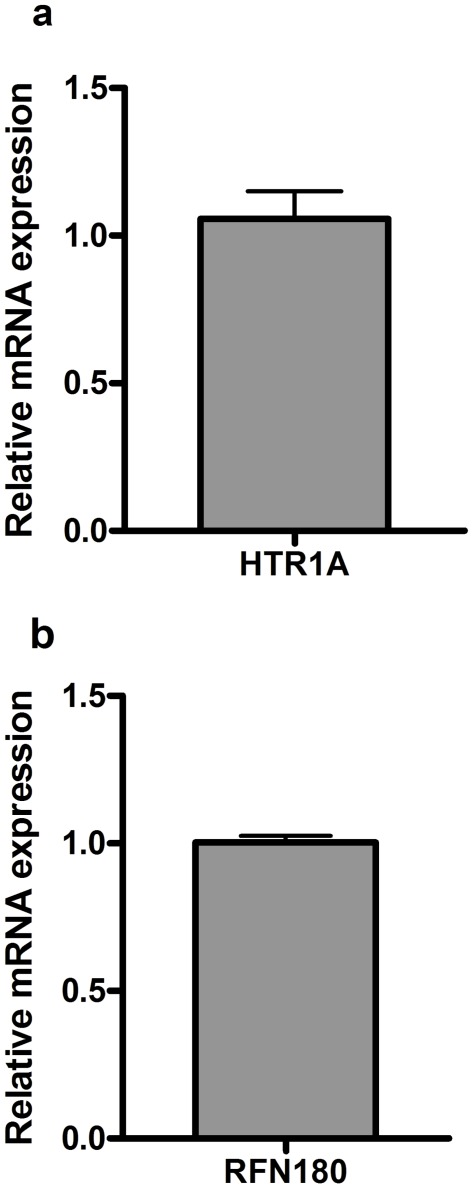
mRNA was isolated and converted to cDNA from a total of 10 healthy islet donors. Relative mRNA expression of HTR1A (n = 6) (Figure 3a) indicates expression of HTR1A in human islets of Langerhans. Relative expression of RFN180 (n = 4) was also detected in human islet donors (Figure 3b).
Figure 3. a-b. Q-PCR expression.
Q-PCR expression for HTR1A (a) and RNF180 (b) from mRNA isolated from a total of 10 human islet donors. Data is presented as means of expression relative to the housekeeping genes cyclophilin A (PPIA), polymerase 2 (POL2A) and hypoxanthine guanine phosphoribosyl transferase (HPRT) +/− SEM.
HTR1A Protein in Human Beta Cells and Alpha Cells
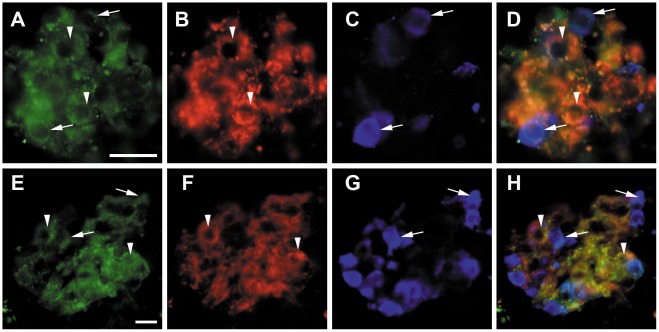
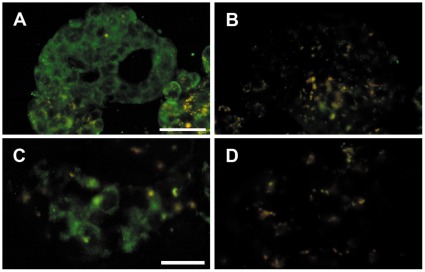
Staining of human beta and alpha-cells was performed to confirm results obtained from the q-PCR. Sections of human islets and human pancreatic specimens were triple immunostained for HTR1A, insulin and glucagon. This revealed that the HTR1A receptor is mainly expressed in beta-cells and alpha-cells (Figure 4). Importantly preabsorption with blocking peptide against HTR1A blocked all staining in both isolated human islets and in islets of human pancreatic sections (Figure 5).
Figure 4. Human isolated islets and human pancreas triple immunostained for HTR1A, insulin and glucagon.
Human isolated islets (A–D) and human pancreas (E–H) triple immunostained for HTR1A (A, E), insulin (B, F), and glucagon (C,G); merged in D and H. Arrow heads indicate beta cells with HTR1A immunoreactivity, arrows indicate alpha cells with HTR1A immunoreactivity. Scale bar = 20 um in A for upper panel, in E for lower panel.
Figure 5. Human isolated islets and human pancreas with HTR1A antibodies preabsorbed with blocking peptide against HTR1A.
Human isolated islets (A–B) and human pancreas (C–D). A and C immunostained for HTR1A. B and D the same islets as in A and C in consecutive sections immunstained with HTR1A antibodies preabsorbed with blocking peptide against HTR1A, demonstrating complete lack of immunoreaction. Scale bar = 50 um in A for upper panel, in 25 um in C for lower panel.
Discussion
We have in a previous genome-wide linkage study observed suggestive linkage of T1D to the 5p13-q13 region [4].
In previous reports several other autoimmune diseases such as Crohn’s disease [17], Autoimmune Thyroid disease (AITD) [18], Multiple Sclerosis (MS) [19], and Systemic lupus erythematosus (SLE) [20], have all been linked to the chromosome 5 region. Moreover, investigations indicate that IL7R which maps to the chromosome 5p13 region is associated to T1D as well as MS [21], [22].
The rs356570 SNP which is significantly associated to T1D in our Swedish and Danish families tags for several SNPs in the HTR1A and post RNF180 region. Also, two haplotypes showed protective and positive association respectively in our families. No single SNP or haplotype association was detected in the Swedish sporadic cohorts. An explanation for this could be that there may be heterogeneity between familial and sporadic cases due to an enrichment of rare susceptibility genes with strong effect in the family materials. In the Swedish sporadic materials common susceptibility genes with low risk are likely to be more common. Further, the difference in association may also be due to changes in the environment. The multiplex families were collected a long time ago and it may be that changes in susceptible environmental factors have resulted in a change of importance of T1D susceptibility genes as has been suggested by us previously [6].
HTR1A and RNF180 both show similar association to T1D in the multiplex families. However, in a conditional analysis, the HTR1A gene showed a slightly stronger association suggesting that HTR1A is the main T1D gene in this region. It should also be mentioned that since there is no LD between IL7R and the genes we have studied, our association cannot be due to IL7Ŕs association to T1D (r2<0.01 and D́<0.02 between rs6897932 in IL7R and rs356570 in HapMap data). Further, GWAS studies performed by the Type 1 Diabetes Genetic Consortium (T1DGC) [3] and Welcome Trust Case Control Consortium (WTCCC) [23] do not detect any association of our studied region in their materials. The genotyped markers in the WTCCC study included our typed markers rs878567, rs382098 and rs356562 but not our most associated marker rs356570 [23]. All typed markers are in strong LD with each other (r2<0.91). In the GWAS study performed by WTCCC, sporadic rather than familial cases were used. In our study we only detect significant association in family materials. The use of sporadic versus familial cases may explain the contradictory results in our and the WTCCC study. Additionally, no SNPs which show association in our study were genotyped in the T1DGC study. It would therefore be interesting to genotype our studied SNPs in the multiplex T1DGC families to test if the lack of confirming the association of HTR1A in sporadic cases is due to a true heterogeneity between sporadic and multiplex cases.
We observe association for the rs6295 SNP in the multiplex families. Bioinformatic analysis indicate that rs6295 is located in a binding site for at least two transcription factors; Irf-1 which plays a role in regulating apoptosis and tumor suppression and NRF-2 which regulates cellular oxidative stress. It is therefore of interest to test the effect of rs6295 on expression of HTR1A in order to understand whether or not it is involved in the destruction of pancreatic beta-cells.
There are seven different types of serotonin receptors [24]. It has recently been reported that the HTR2A receptor is associated with Rheumatoid Arthritis [25].
HTR1A is a relatively short intronless gene consisting of only 1 268 bp. The gene is known to encode for a G-protein coupled receptor specific for serotonin which mediates cellular signaling via the amine serotonin (5-HT) [26]. The HTR1A receptor is expressed in many tissues but is mainly known to mediate signal transduction in neurons in the central nervous system [27] where it is involved in various complex behaviors such as appetite, sleep and aggression. Changes in serotonin signaling are associated with depression and suicide [28]. Expression of HTR1A has also been reported throughout the enteric nervous system and in the endocrine pancreas [29].
In the present study, we show that the 5-HTR1A protein is present in human pancreatic beta and alpha-cells. In accordance, we also show that HTR1A mRNA is expressed in human pancreatic islets. This provides an important functional correlation to the genetic data.
The neurotransmitter serotonin has been shown to be produced in pancreatic islets of several different species [30] and in vitro studies of rodent islet studies show that serotonin inhibits insulin secretion [31]. Moreover, systemic activation of HTR1A with sumatriptan in humans has a clear inhibitory effect on insulin secretion [32]. Whether this is due to a regulation at a central level or via a direct effect on the beta-cells, or both, remains to be elucidated. Furthermore, during pancreas regeneration, the expression of HTR1A is decreased while the insulin release is increased [33]. From this, it may be speculated that different HTR1A genotypes affects insulin release and could thereby be involved in the development of T1D. HTR1A has also been reported to play a role in the immune system. It has been reported that activated T-cells express high amounts of HTR1A while resting T-cells have low HTR1A expression [34]. Further, HTR1A is known to down regulate adenylate cyclase which in turn regulates T-cell functions such as production of IL-2 and cytotoxic T-cell activity [34]. Hence polymorphisms in the HTR1A gene may also affect the T-cell activity and thereby influencing the risk of developing T1D.
As mentioned earlier, two haplotypes containing rs356570 which maps upstream of both HTR1A and RNF180 were identified in this study. It is therefore possible that a polymorphism in this region effects the expression of both HTR1A and RNF180. Since we in this study observe that HTR1A might be involved in T1D susceptibility independently of RNF180, we suggest that expression studies of HTR1A should be carried out in order to fully understand its function in T1D development. Also, further SNP genotyping in large case-control studies and sequencing should be carried out to confirm the association and determine which SNP in and around HTR1A is the main T1D associated marker.
Supporting Information
Typed microsatellites in the original genome-scan [4] and fine mapping. Typed microsatellites in the original scan have been run on all Scandinavian families, Norwegian, Danish and Swedish. Fine mapping has been performed on the Swedish and Danish families. All SNPs have been genotyped in the Swedish families. SNPs marked with * have been typed in the Swedish case control material DISS2, Δ have been typed in the Danish families and # indicates SNPs typed in the BDD material.
(DOC)
Acknowledgments
We would like to acknowledge the Human Tissue Laboratory, Lund University Diabetes Center, Lund University, Clinical Research Center, Malmö, Sweden, and the Islet Isolation Unit at Uppsala University, Uppsala, Sweden, as well as the Nordic Network for Clinical Transplantation, for providing donor islet material. We would also like to thank the Members of the Diabetes Incidence Study in Sweden Study (DISS) Group: Hans Arnqvist, Department of Internal Medicine, University of Linköping, Linköping; Elisabeth Björck, Department of Medicine, University Hospital, Uppsala; Jan Eriksson, Department of Medicine, University of Umeå, Umeå; Lennarth Nyström, Department of Epidemiology and Public Health, University of Umeå, Umeå; Lars Olof Ohlson, Sahlgrenska Hospital, University of Göteborg, Göteborg; Bengt Scherstén, Department of Community Health Sciences, Dahlby, University of Lund, Lund; and Jan Östman, Centre for Metabolism and Endocrinology, Huddinge University Hospital, Stockholm.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The study has been funded by Swedish Research Council, Svenska Diabetes Fonden, Barndiabetes Fonden, Magnus Bergvalls Stiftelse, the Novo Nordisk Foundation, the Krapperup foundation, the Åke Wiberg foundation and the Swedish Society for Medicine (to MF). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Group DP. Incidence and trends of childhood Type 1 diabetes worldwide 1990–1999. Diabet Med. 2006;23:857–866. doi: 10.1111/j.1464-5491.2006.01925.x. [DOI] [PubMed] [Google Scholar]
- 2.Patterson CC DG, Gyurus E, Green A, Soltesz G EURODIAB Study Group. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–2020: a multicentre prospective registration study. Lancet. 2009;373:2027–2033. doi: 10.1016/S0140-6736(09)60568-7. [DOI] [PubMed] [Google Scholar]
- 3.Barrett JC, Clayton DG, Concannon P, Akolkar B, Cooper JD, et al. Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet. 2009;41:703–707. doi: 10.1038/ng.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nerup J, Pociot F. A genomewide scan for type 1-diabetes susceptibility in Scandinavian families: identification of new loci with evidence of interactions. Am J Hum Genet. 2001;69:1301–1313. doi: 10.1086/324341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jensen RA GL, Törn C, Landin-Olsson M, Karlsson FA, Palmer JP, et al. Multiple factors affect the loss of measurable C-peptide over 6 years in newly diagnosed 15- to 35-year-old diabetic subjects. J Diabetes Complications. 2007;21:205–213. doi: 10.1016/j.jdiacomp.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Carlsson A KI, Lindblad B, Engelson L, Nilsson A, Forsander G, et al. International Journal of Obesity; 2011. Association between HLA-DQ and BMI in newly diagnosed type 1 diabetes children in the Better Diabetes Diagnosis study in Sweden. pp. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hedstrom AK, Baarnhielm M, Olsson T, Alfredsson L. Tobacco smoking, but not Swedish snuff use, increases the risk of multiple sclerosis. Neurology. 2009;73:696–701. doi: 10.1212/WNL.0b013e3181b59c40. [DOI] [PubMed] [Google Scholar]
- 8.Holm P, Rydlander B, Luthman H, Kockum I. Interaction and association analysis of a type 1 diabetes susceptibility locus on chromosome 5q11-q13 and the 7q32 chromosomal region in Scandinavian families. Diabetes. 2004;53:1584–1591. doi: 10.2337/diabetes.53.6.1584. [DOI] [PubMed] [Google Scholar]
- 9.Ekelund E, Lieden A, Link J, Lee SP, D’Amato M, et al. Loss-of-function variants of the filaggrin gene are associated with atopic eczema and associated phenotypes in Swedish families. Acta Derm Venereol. 2008;88:15–19. doi: 10.2340/00015555-0383. [DOI] [PubMed] [Google Scholar]
- 10.Sawcer S, Hellenthal G, Pirinen M, Spencer CC, Patsopoulos NA, et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature. 2011;476:214–219. doi: 10.1038/nature10251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hauser ER, Boehnke M, Guo SW, Risch N. Affected-sib-pair interval mapping and exclusion for complex genetic traits: sampling considerations. Genet Epidemiol. 1996;13:117–137. doi: 10.1002/(SICI)1098-2272(1996)13:2<117::AID-GEPI1>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 12.Gudbjartsson DF JK, Frigge ML, Kong A, Gudbjartsson DF 1, K J, Frigge ML, Kong A. Allegro, a new computer program for multipoint linkage analysis. Nature Genetics. 2000;25:12–13. doi: 10.1038/75514. [DOI] [PubMed] [Google Scholar]
- 13.Li M, Boehnke M, Abecasis GR. Joint modeling of linkage and association: identifying SNPs responsible for a linkage signal. Am J Hum Genet. 2005;76:934–949. doi: 10.1086/430277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–265. doi: 10.1093/bioinformatics/bth457. [DOI] [PubMed] [Google Scholar]
- 15.Dudbridge F. Likelihood-based association analysis for nuclear families and unrelated subjects with missing genotype data. Hum Hered. 2008;66:87–98. doi: 10.1159/000119108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li MA, Abecasis GR. Mach 1.0: rapid haplotype reconstruction and missing genotype inference [abstract 2290/C]. Am J Hum Genet. 2006;S79:416. [Google Scholar]
- 17.Ma Y OJea. A genome-wide search identifies potential new susceptibility loci for Crohńs disease. Inflamm Bowel Diseases. 1999;5:271–278. doi: 10.1097/00054725-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Namjou B KJ, Kilpatrick J, Kaufman KM, Nath SK, Scofield RH, et al. Linkage at 5q14.3–15 in multiplex systemic lupus erythematosus pedigrees stratified by autoimmune thyroid disease. Arthritis Rheum. 2005;52:3646–3650. doi: 10.1002/art.21413. [DOI] [PubMed] [Google Scholar]
- 19.Oturai A, Larsen F, Ryder LP, Madsen HO, Hillert J, et al. Linkage and association analysis of susceptibility regions on chromosomes 5 and 6 in 106 Scandinavian sibling pair families with multiple sclerosis. Ann Neurol. 1999;46:612–616. [PubMed] [Google Scholar]
- 20.Namjou B, Nath SK, Kilpatrick J, Kelly JA, Reid J, et al. Stratification of pedigrees multiplex for systemic lupus erythematosus and for self-reported rheumatoid arthritis detects a systemic lupus erythematosus susceptibility gene (SLER1) at 5p15.3. Arthritis Rheum. 2002;46:2937–2945. doi: 10.1002/art.10588. [DOI] [PubMed] [Google Scholar]
- 21.Todd JA, Walker NM, Cooper JD, Smyth DJ, Downes K, et al. Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007;39:857–864. doi: 10.1038/ng2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lundmark F, Duvefelt K, Iacobaeus E, Kockum I, Wallstrom E, et al. Variation in interleukin 7 receptor alpha chain (IL7R) influences risk of multiple sclerosis. Nat Genet. 2007;39:1108–1113. doi: 10.1038/ng2106. [DOI] [PubMed] [Google Scholar]
- 23.Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447:661–678. doi: 10.1038/nature05911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoyer D, Hannon JP, Martin GR. Molecular, pharmacological and functional diversity of 5-HT receptors. Pharmacol Biochem Behav. 2002;71:533–554. doi: 10.1016/s0091-3057(01)00746-8. [DOI] [PubMed] [Google Scholar]
- 25.Kling A, Seddighzadeh M, Arlestig L, Alfredsson L, Rantapaa-Dahlqvist S, et al. Genetic variations in the serotonin 5-HT2A receptor gene (HTR2A) are associated with rheumatoid arthritis. Ann Rheum Dis. 2008;67:1111–1115. doi: 10.1136/ard.2007.074948. [DOI] [PubMed] [Google Scholar]
- 26.Barnes NM, Sharp T. A review of central 5-HT receptors and their function. Neuropharmacology. 1999;38:1083–1152. doi: 10.1016/s0028-3908(99)00010-6. [DOI] [PubMed] [Google Scholar]
- 27.Lesurtel M, Soll C, Graf R, Clavien PA. Role of serotonin in the hepato-gastroIntestinal tract: an old molecule for new perspectives. Cell Mol Life Sci. 2008;65:940–952. doi: 10.1007/s00018-007-7377-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stockmeier CA, Shapiro LA, Dilley GE, Kolli TN, Friedman L, et al. Increase in Serotonin-1A Autoreceptors in the Midbrain of Suicide Victims with Major Depression–Postmortem Evidence for Decreased Serotonin Activity. The Journal of Neuroscience. 1998;18:7394–7401. doi: 10.1523/JNEUROSCI.18-18-07394.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirchgessner AL, Liu MT, Raymond JR, Gershon MD. Identification of cells that express 5-hydroxytryptamine1A receptors in the nervous systems of the bowel and pancreas. J Comp Neurol. 1996;364:439–455. doi: 10.1002/(SICI)1096-9861(19960115)364:3<439::AID-CNE5>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 30.Sundler F, Hakanson R, Loren I, Lundquist I. Amine storage and function in peptide hormone-producing cells. Invest Cell Pathol. 1980;3:87–103. [PubMed] [Google Scholar]
- 31.Zawalich WS, Tesz GJ, Zawalich KC. Effects of prior 5-hydroxytryptamine exposure on rat islet insulin secretory and phospholipase C responses. Endocrine. 2004;23:11–16. doi: 10.1385/ENDO:23:1:11. [DOI] [PubMed] [Google Scholar]
- 32.Coulie B, Tack J, Bouillon R, Peeters T, Janssens J. 5-Hydroxytryptamine-1 receptor activation inhibits endocrine pancreatic secretion in humans. Am J Physiol. 1998;274:E317–320. doi: 10.1152/ajpendo.1998.274.2.E317. [DOI] [PubMed] [Google Scholar]
- 33.Mohanan VV KR, Paulose CS. Hypothalamic 5-HT functional regulation through 5-HT1A and 5-HT2C receptors during pancreatic regeneration. Life Sci. 2006;78:1603–1609. doi: 10.1016/j.lfs.2005.07.027. [DOI] [PubMed] [Google Scholar]
- 34.Aune TM, McGrath KM, Sarr T, Bombara MP, Kelley KA. Expression of 5HT1a receptors on activated human T cells. Regulation of cyclic AMP levels and T cell proliferation by 5-hydroxytryptamine. J Immunol. 1993;151:1175–1183. [PubMed] [Google Scholar]
- 35.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, et al. The structure of haplotype blocks in the human genome. Science. 2002;296:2225–2229. doi: 10.1126/science.1069424. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Typed microsatellites in the original genome-scan [4] and fine mapping. Typed microsatellites in the original scan have been run on all Scandinavian families, Norwegian, Danish and Swedish. Fine mapping has been performed on the Swedish and Danish families. All SNPs have been genotyped in the Swedish families. SNPs marked with * have been typed in the Swedish case control material DISS2, Δ have been typed in the Danish families and # indicates SNPs typed in the BDD material.
(DOC)