Abstract
Introduction
Bombesin (BN) is an amphibian peptide that binds to the gastrin-releasing peptide receptor (GRPR). It has been demonstrated that BN analogues can be radiolabeled for potential diagnosis and treatment of GRPR-expressing malignancies. Previous studies have conjugated various chelators to the eight C-terminal amino acids of BN (BN(7-14)) for radiolabeling with 64Cu. Recently, (1,4,7-triazacyclononane-1,4,7-triacetic acid) (NOTA) has been evaluated as the five coordinate 64Cu complex with results indicating GRPR-specific tumor uptake. This study aimed to conjugate S-2-(4-isothiocyanatobenzyl)-NOTA (p-SCN-Bn-NOTA) to BN(7-14) such that it could form a six coordinate complex with 64Cu and evaluate the resulting peptide.
Methods
p-SCN-NOTA was conjugated to 8-aminooctanoic acid (Aoc)-BN(7-14) in solution to yield NOTA-Bn-SCN-Aoc-BN(7-14). The unlabeled peptide was evaluated in a cell binding assay using PC-3 prostate cancer cells and 125I-Tyr4-BN to determine the IC50 value. The peptide was radiolabeled with 64Cu and evaluated for internalization into PC-3 cells and for tumor uptake in mice bearing PC-3 xenografts using biodistribution and microPET imaging studies.
Results
The binding assay demonstrated that NOTA-Bn-SCN-Aoc-BN(7-14) bound with high affinity to GRPR with an IC50 of 1.4 nM. The radiolabeled peptide demonstrated time-dependent internalization into PC-3 cells. In vivo, the peptide demonstrated tumor-specific uptake and imaging that was comparable to that of previously reported 64Cu-labeled BN analogues.
Conclusions
These studies demonstrate that 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) binds to GRPR expressing cells and that it can be used for imaging of GRPR-expressing prostate cancer.
Keywords: Bombesin, NOTA, Prostate cancer, Cu-64
Introduction
The gastrin-releasing peptide receptor (GRPR) is a G-protein coupled receptor that is overexpressed on a number of solid tumors, including prostate, breast, and small cell lung cancer [1,2]. Consequently, ligands to GRPR have been of considerable interest in potential imaging and therapeutic applications. Of these ligands, bombesin (BN), an amphibian homologue of the mammalian GRP that binds the receptor with high affinity [3], has been extensively studied with the goal of developing agents capable of targeting GRPR-overexpressing malignancies [4-11]. In this regard, our laboratory has focused on the radiolabeling of BN analogues with the positron-emitting radionuclide, 64Cu [12-15].
Most of the previous work with 64Cu-radiolabeling of BN analogues have been performed with the macrocyclic chelator 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid (DOTA) [13,16], but in vivo dissociation of 64Cu and transchelation to other proteins have challenged the efforts by resulting in high uptake in normal tissues (i.e., liver and kidney) and low tumor to normal tissue ratios [17]. More recently, 1,4,7-triazacyclononane-1,4,7-triacetic acid (NOTA) has been conjugated to BN(7-14), permitting comparison to DOTA conjugated BN(7-14) [18,19]. These studies directly conjugated NOTA to Aoc-BN(7-14) via one of the carboxylate arms of NOTA (to form NO2A-Aoc-BN(7-14)), resulting in a five coordinate copper complex. In these studies, the NOTA analogues have reduced uptake in normal tissues compared to the corresponding DOTA analogues resulting in improved tumor to normal tissue ratios.
The focus of this study was to determine if these tumor to normal tissue ratios could be improved even further by conjugating a chemically-related, six coordinate chelator, p-SCN-Bn-NOTA to BN(7-14) for complexing 64Cu. The BN analogue, NOTA-Bn-SCN-Aoc-BN(7-14), evaluated in this study is shown in Figure 1. Our data demonstrate this analogue’s binding to GRPR-positive PC-3 human prostate cancer cells and internalization into these cells after radiolabeling with 64Cu. In addition, the tumor-specific localization and normal tissue accumulation of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) were determined with in vivo biodistribution studies and in microPET imaging studies using mice bearing heterotopic PC-3 tumors.
Figure 1.
Chemical structure of NOTA-Bn-SCN-Aoc-BN(7-14).
2. Materials and methods
2.1. Synthesis of Bombesin Analogue
The chelator, p-SCN-Bn-NOTA, was purchased from Macrocyclics (Dallas, TX) and the Fmoc-8-aminooctanoic acid (Aoc) was purchased from Advanced ChemTech (Louisville, KY). Amino acids were purchased from Novabiochem (Gibbstown, NJ). Aoc-BN(7-14) was synthesized on solid support using automated standard Fmoc chemistry at room temperature. Starting with the methionine-loaded Rink Amide resin (30 μmol), subsequent amino acids and Aoc were coupled to the resin by using the appropriate Fmoc-protected amino acids (90 μmol) and coupling reagents HBTU (90 μmol), HOBT (90 μmol), and DIEA (180 μmol). Aoc was coupled by the same method. Cleavage of the peptide from the resin and concomitant removal of all protecting groups was achieved with 94% TFA, 1% TIS, 2.5% EDT, and 2.5% water. The p-SCN-BN-NOTA (17.9 μmol) was conjugated to Aoc-BN(7-14) (6.0 μmol) in sodium bicarbonate solution (1.4 M, 62 μL) and DMF (1.5 mL) at room temperature for 15 hours. The resulting product was purified by preparative HPLC suing a Grace Vydac C-18 column (250 × 21.2 mm). The desired compound (2.8 mg, 30%) was obtained by linear gradient elution consisting of solvents A (0.1% TFA in water) and B (0.1% TFA in acetonitrile) from 90% to 40% A over 18 min at 10 mL/min. The elution was monitored by UV absorbance at 214 and 254 nm with the resulting NOTA-Bn-SCN-Aoc-BN(7-14) being > 95% pure by HPLC. The peptide characterized by analytical HPLC and the identity was confirmed by electrospray mass spectrometry (ES+MS): NOTA-Bn-SCN-Aoc-BN(7-14) calcd (M+1) m/z 1531.5; found 1533 (M+1),767 (M+2).
2.2. Competitive Binding Assay
The IC50 values of NOTA-Bn-SCN-Aoc-BN(7-14) were determined using a competitive binding assay with 125I-Tyr4-BN (PerkinElmer, Waltham, MA). PC-3 human prostate adenocarcinoma cells were obtained from the American Type Tissue Culture Center (Manassas, VA) and maintained in 45% RPMI 1640, 45% Ham’s F-12, and 10% heat inactivated fetal bovine serum (FBS). The media components were obtained from Invitrogen (Carlsbad, CA) and the FBS was obtained from Sigma Chemical Company (St. Louis, MO). The cells were seeded in 6-well plates (5 × 105 cells/well) and incubated at 37°C overnight. The media was then replaced with 1 mL of DMEM + 1% FBS containing increasing concentrations of NOTA-Bn-SCN-Aoc-BN(7-14) in triplicate such that the final concentration ranged from 5 pM to 0.5 μM. 125I-Tyr4-BN (0.05 nM final concentration) was then added to each well and the plates were incubated at 4°C for 2 hours. The cells were then rinsed twice with ice cold PBS and harvested. The cells were placed on a Packard II gamma counter (Perkin-Elmer, Boston, MA) to determine the cell-associated radioactivity. After correction for decay, the data were plotted using GraphPad Prism 4 Software (San Diego, CA) using the sigmoidal dose response equation, with cpm of radioactivity bound vs. log of the concentration of NOTA-Bn-SCN-Aoc-BN(7-14) for the determination of the IC50 values.
2.3. Radiolabeling of Bombesin Analogue
Copper-64 (64Cu; t1/2 = 12.7 h; β+ = 0.656 MeV, 17.8%) was produced on a biomedical cyclotron at Washington University in St. Louis [20]. The bombesin analogue was radiolabeled with 64Cu by diluting 64CuCl2 with at least a 10-fold excess of 0.1 M NH4OAc (pH = 5.5) and then ~37 MBq were added to a mixture of ~10 μg of NOTA-Bn-SCN-Aoc-BN(7-14) and 0.05 μg of L-ascorbic acid in a total volume of ~100 μL. The reaction mixtures were then incubated at room temperature for 45 minutes. The radiochemical purity of the peptide was determined by radio-TLC. One μL of the reaction mixtures was applied to Whatman MKC18F reversed-phase TLC plates (Whatman Inc., Florham Park, NJ) and developed with 10% ammonium acetate:methanol (30:70) as the mobile phase. The TLC plates were scanned on a BioScan Imaging Scanner (Washington, D.C.), and the radiolabeled peptides were used immediately without purification for in vitro and in vivo assays.
2.4. Internalization of Bombesin Analogue
PC-3 cells (5 × 105) were plated in 6-well plates and incubated overnight at 37°C. The cells were then washed twice with Hank’s Balanced Salts Solution (HBSS) followed by addition of 1 mL of DMEM containing 30 mM HEPES, 2 mM l-glutamine, 1 mM sodium pyruvate, and 1% BSA. Tyr4-BN (10 μg, Sigma Chemical Co.) was added to three of the six wells per plate to act as a blocking agent followed immediately by the addition of 64Cu- NOTA-Bn-SCN-Aoc-BN(7-14) (18.5 kBq) such that the final concentration of radiolabeled peptide was 1 nM. The plates were then incubated at 37°C for various times (15, 30 60, 120, and 240 min) at which point they were removed from the incubator and washed twice with HBSS. The cells were then washed twice with 500 μL of 20 mM sodium acetate in HBSS, pH 4.0, to remove surface bound radioactivity and these washes were discarded. The cells were then harvested using 1% SDS in 10 mM sodium borate and placed on the gamma counter to determine the amount of internalized radioactivity. The counts per minute (cpm) internalized were converted to fmol based on the specific activity of the peptides and normalized to the protein in each well as determined using the Pierce BCA Protein Kit (Rockford, IL). The data are presented as the specific amount (fmol in non-blocked wells minus fmol in blocked wells) of radiolabeled peptide internalized per mg of protein versus time.
2.5. Biodistribution Studies
All animal studies were performed under the Guidelines for the Care and Use of Research Animals through the Washington University Animal Studies Committee. PC-3 cells in PBS (200 μL; 1 × 107 cells) were injected subcutaneously into 3-4 week old female SCID mice (Taconic, Hudson, NY). The tumors were allowed to grow for 23 days (tumor weight ~250 mg) and the mice (n = 5 per group) were injected intravenously (i.v.) with 0.5 MBq (100 ng) of 64Cu- NOTA-Bn-SCN-Aoc-BN(7-14). The mice were sacrificed 1, 4, or 24 hours later and the blood, liver, spleen, kidney, muscle, bone, pancreas, and tumor harvested, weighed, and counted in the gamma counter. An additional group of mice were injected with the radiolabeled bombesin analogues pre-mixed with 100 μg of Tyr4-BN to serve as a blocking agent and sacrificed at 1 hour. The percent injected dose per gram of tissue (% ID/g) was determined by decay correction of the 64Cu-labeled bombesin analogues for each sample normalized to a standard of known weight, which was representative of the injected dose.
2.6. MicroPET/CT Imaging Studies
PC-3 cells were implanted in SCID mice as described above. The mice (n = 4) were injected i.v. with 2.8 MBq (750 ng) of 64Cu- NOTA-Bn-SCN-Aoc-BN(7-14) with or without 150 μg of Tyr4-BN. At 1, 4, and 24 hours after injection, the mice were anesthetized with 1-2% isoflurane, positioned supine, and imaged on microPET FOCUS 220 or Inveon PET small animal scanners (Siemens Medical Solutions). The PET acquisition times were 10 min for the 1 and 4 hour time points and 20 min for the 24 hour time point. CT images were obtained using a MicroCAT II System (ImTek, Inc., Knoxville, TN). The images were reconstructed with an Ordered-Subset Estimation Maximization (OSEM) algorithm which included corrections for scatter and attenuation. Regions of interest were drawn to encompass the entire tumor to determine the maximum activity concentration (nCi/cc) in the tumor. To calculate the standardized uptake values (SUVs), the nCi/cc was divided by the nCi injected (decay corrected to the scan start time) and multiplied by the mouse weight.
2.7. Statistical Analysis
All data are presented as the mean ± SEM. The Student’s two-tailed t-test was used to determine statistical significance at the 95% confidence level, with p ≤ 0.05 being considered significantly different.
3. Results
3.1. Competitive Binding Assay
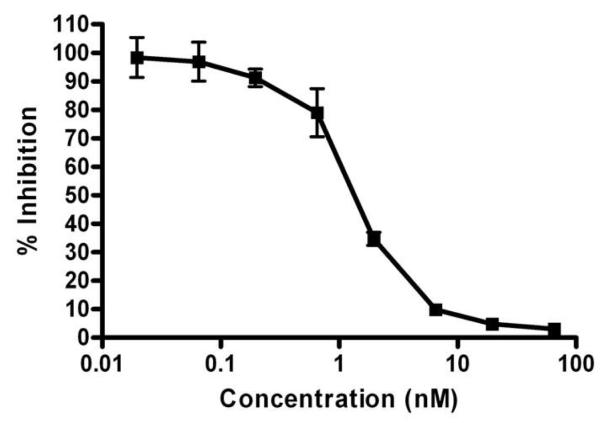
A representative competitive binding curve of NOTA-Bn-SCN-Aoc-BN(7-14) is shown in Figure 2. The binding of 125I-Tyr4-BN to PC-3 cells was inhibited by various concentrations of NOTA-Bn-SCN-Aoc-BN(7-14). The IC50 value for NOTA-Bn-SCN-Aoc-BN(7-14) was 1.4 ± 0.6 nM.
Figure 2.
Inhibition of 125I-Tyr4-BN binding to PC-3 cells with various concentrations of NOTA-Bn-SCN-Aoc-BN(7-14). Increasing concentrations of NOTA-Bn-SCN-Aoc-BN(7-14) were added to triplicate wells followed by 125I-Tyr4-BN (0.05 nM final concentration). After incubation for 2 hours at 4°C, the cells were then rinsed, harvested, and placed on a gamma counter to determine the cell-associated radioactivity. The data are expressed as the mean counts per minute (cpm) of radioactivity in 3 experiments ± SEM versus the log of the concentration (in nM) of the BN analogues.
3.2. Radiolabeling and Internalization
The bombesin analogue was radiolabeled with 64Cu at room temperature in > 95% radiochemical purity and at a specific activity of 12.4 GBq/μmol for internalization, biodistribution, and imaging studies. Figure 3 shows the internalization of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14). Curve fitting showed that the maximum internalization was 896 ± 119 fmol/mg for 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14). The initial velocity of internalization was 8.9 fmol/mg/min for 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) as determined by linear regression of the data from 0 to 60 min.
Figure 3.
Internalization of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) into PC-3 cells. Cells were incubated with the 64Cu-labeled analogues for various times with or without Tyr4-BN as an inhibitor. After acid washing the cells to remove cell surface radioactivity, the cells were lysed, collected, and the amount of internalized radioactivity was counted. The data are shown as the mean of 3 experiments ± SEM, with each experiment being performed in triplicate.
3.3. Biodistribution Studies
Figure 4 shows the % ID/g for 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) in various tissues at 1, 4, 24 hours, and 1 hour with block. The blood concentration of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) was 0.44% ID/g at 1 hour, and 0.06 and 0.05 at 4 and 24 hours, respectively. Specific uptake of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) was noted at one hour in the pancreas at a concentration of 19.7% ID/g and in the tumor (2.8% ID/g) when compared to the animals blocked with Tyr4-BN (p < 0.05). Concentrations of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) revealed non-specific uptake in other tissues, including liver (3.41% ID/g), spleen (0.62% ID/g), kidney (1.62% ID/g), muscle (0.54% ID/g), and bone (0.54% ID/g), when compared to blocked animals at one hour.
Figure 4.
Biodistribution of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) in mice bearing PC-3 xenografts. PC-3 cells tumors were generated in SCID mice, and the animals (n = 5 per group) were injected with 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14). The mice were sacrificed 1, 4, and 24 hours later, and the blood, liver, spleen, kidney, muscle, bone, pancreas, and tumor were harvested, weighed, and counted in the gamma counter. An additional group of mice were injected with the radiolabeled bombesin analogues pre-mixed with Tyr4-BN as a blocking agent. The percent injected dose per gram of tissue (% ID/g) was determined by decay correction of each sample normalized to weight. The data for each group represent the mean ± SEM.
The tumor/blood, tumor/liver, tumor/kidney, and tumor/muscle ratios are shown in Table 1. The tumor/blood ratio one hour after injection was found to be 6.2, while the tumor/kidney and tumor/liver ratios were 1.7 and 0.8, respectively. Examination of the kinetics of tumor uptake for 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) reveal that between 1 and 4 hours the concentration fell from 2.8 to 1.0% ID/g. At 24 hours, the concentration had fallen to 0.19% ID/g, which was indistinguishable from other tissues. Clearance from the pancreas was very rapid with only 2% of the activity achieved at 1 hour still detectable at 24 hours.
Table 1.
| Tumor:Organ | 1h | 4h | 24h |
|---|---|---|---|
| Tumor:Blood | 6.218 | 18.029 | 3.609 |
| Tumor:Kidney | 1.707 | 1.935 | 0.728 |
| Tumor:Liver | 0.809 | 2.489 | 0.685 |
| Tumor:Muscle | 5.102 | 23.754 | 7.022 |
3.4. MicroPET/CT Imaging Studies
Small animal PET/CT images of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) at 1, 4, and 24 hours are shown in Figure 5. Transaxial and coronal views of two mice (one receiving blocking agent and the other not receiving blocking agent) from the fused PET/CT for mice bearing PC-3 xenografts are shown in this figure. The mice on the left in each panel received 150 μg of Tyr4-BN as a blocking agent and the mice on the right did not. Tumor uptake is observed in the mice that did not receive the blocking agent at 1 and 4 h, while mice that received the blocking agent showed less uptake in tumors at these timepoints. Clearance of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) from the tumor was so rapid, that radioactive retention was not observed in non-blocked tumors at 24 h. Figure 6 shows the SUV analysis from the PET/CT studies. This shows that the tumor uptake was selective with 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) at 1 and 4 h, while retention was not observed at 24 h. The tumor uptake of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) was significantly reduced (p < 0.05) at 1 and 4 h in the presence of the blocking agent.
Figure 5.
Axial (top panels) and coronal (bottom panels) view of maximum-intensity projections of microPET images with co-registered CT of mice bearing PC-3 xenografts in the rear flank at 1 h, 4 h, and 24 h. The mice were injected i.v. with 2.8 MBq (750 ng) of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14), anesthetized with 1-2% isoflurane, and imaged for 10 min at the 1 and 4 h time points and 20 min at the 24 h time point. The mice on the left of each frame were injected with 150 μg of Tyr4-BN as blocking agent. The “T” denotes the position of the tumors and the “B” indicates the bladder position.
Figure 6.
Standardized uptake values (SUVs) for the tumor uptake of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) over time as determined by microPET imaging. After mice were imaged, CT and PET data was coregistered and regions of interest were drawn to encompass the entire tumor. SUV was calculated and data shown. The hatched column represents the 64Cu-labeled analogue that was co-injected with blocking agent. The imaging data represent the mean ± SEM of 4 mice per group.
4. Discussion
Initial studies with 64Cu chelators included 64Cu-DOTA and 64Cu-TETA, but their disappointing kinetic stability led to the development of other chelators. In this regard, crossbridged and sarcophogine based chelators have been developed that are more effective in containing copper in vivo [17,21-22]. In addition, NOTA is a chelator that can form a six coordinate complex with copper [23], has a high stability constant (log K = 21.6) that is similar to TETA (log K = 21.7) and DOTA (log K = 22.3) [24], but is more stable than either TETA or DOTA at physiologic pH (7.4) or below [25]. In vivo studies on the effective stability and accumulation of the 64Cu-NO2A-Aoc-BN(7-14) conjugate in GRPR-expressing, PC-3 xenografted tumors in SCID mice have been promising [19]. However, these studies directly conjugated NOTA to Aoc-BN(7-14) via one of the carboxylate arms of NOTA, leaving five coordination sites available for copper complexation. The purpose of this study was to evaluate BN(7-14) radiolabeled with 64Cu using a C-functionalized NOTA analogue with all three carboxylate arms available for complexation.
In the present study, NOTA-Bn-SCN-Aoc-BN(7-14) bound with high affinity to GRPR with an IC50 of 1.4 nM. The affinity of this ligand for GRPR is similar or slightly better than that previously reported NO2A, NOTA, SarAr, and DOTA analogues [13,18-19,26]. Radiolabeling of the analogues with 64Cu was perfromed at room temperature with excellent efficiency, which is similar to other NOTA, DOTA, or SarAr analogues, but more mild than the 70°C required for CB-TE2A [18,26-28]. The initial internalization rate of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) over the first hour of incubation with the peptide was 8.9 fmol/mg/min which is between 2- and 3-times faster than that found with SarAr analogues [26]. In addition, the maximum internalization was determined to be 896 fmol/mg, which is comparable to that which has been described for other BN-chelator conjugates [18,26-27]. While not formally shown in this study, the ability of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) to internalize suggests that it is functioning as an agonist of GRPR. While it has generally been assumed that internalizing radiolabeled BN agonists are preferred to non-internalizing antagonists due to residualization of the radioactivity in tumor cells, recent publications using BN antagonists and other radiolabeled peptide antagonists have suggested otherwise [9,29-30].
The PC-3 tumor uptake of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) in biodistribution studies was 2.76% ID/g at 1 hour, which is similar to the 3.59% ID/g that has been reported with 64Cu-NO2A-Aoc-BN(7-14) [18-19]. It is lower, however, than the 4.72 and 6.05% ID/g reported when the aminohexanoic acid (Ahx) or para-aminobenzoic acid (AMBA) linkers were used between NOTA and BN(7-14) [19]. Interestingly, only 7% of the radioactivity remained in the tumor at 24 h when compared to 1 h, which is dramatically less than the 28% retention observed for the 64Cu-NO2A-Aoc-BN(7-14) [19]. Uptake in normal tissues at 1 h was similar between 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) and 64Cu-NO2A-Aoc-BN(7-14), while clearance from these tissues was more rapid with 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) having 2-10 times less radioactivity in most normal tissues at 4 and 24 h when compared to 64Cu-NO2A-Aoc-BN(7-14).
The tumor to normal tissue ratios for 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) were similar to the ratios observed for 64Cu-NO2A-Aoc-BN(7-14) at 1 and 4 h, but less at 24 h due to the rapid tumor clearance [19]. 64Cu-NO2A-AMBA-BN(7-14) had higher tumor to normal tissue ratios than all of these analogues at all time points [19], demonstrating the importance of the linking group on tumor and normal tissue uptake. It is not clear why the radioactive clearance from the tumor and normal tissues is more rapid for 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) than for 64Cu-NO2A-Aoc-BN(7-14) leading to lower tumor to normal tissue ratios. Based on the initial crystal structure showing NOTA as forming a six coordinate complex with copper [23], the high stability of the complex at pH 7.4 or lower [25], and the in vitro kinetic studies showing the stability of a 67Cu-NOTA derivative with all six coordination sites available for complexation [31], we hypothesized that a six coordinate 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) analogue would have greater in vivo stability than the five coordinate 64Cu-NO2A-Aoc-BN(7-14). Our results indicate that this may be true; however, the increased stability may have also allowed rapid clearance of the radioactive metabolites from the tumor, leading to lower tumor to normal tissue ratios. It is also possible that our hypothesis is incorrect and the in vivo stability between the six and five coordinate complexes are similar based on another report showing the crystal structure of a five coordinate copper complex for NOTA [32]. It should also be noted that we have not explicitly shown that we are forming the six coordinate complex in 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) although there are six coordination sites available. Therefore, the biodistribution differences between 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) and 64Cu-NO2A-Aoc-BN(7-14) may be a function of metabolite clearance based on charge and lipophilicity differences. It is unlikely that the complex is less stable as normal tissue uptake is low. Metabolism studies will be performed to determine the reason for the difference between these two analogues.
In this study, the microPET/CT images obtained at 1, 4, and 24 hours after 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) injection in PC-3 tumor-bearing SCID mice are consistent with findings in the biodistribution study. These images clearly demonstrate specific tumor uptake of the 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) at 1 and 4 h when compared with animals also given blocking peptide. Similar to the biodistribution study, the images also show the rapid tumor clearance of the radioactivity as the tumor is not observed by 24 h. The uptake of peptide in non-tumor bearing tissues shows radioactivity in the abdomen corresponding to liver, pancreas, and kidneys which agrees with data gathered from the biodistribution study. The SUV analysis shows that tumor uptake of 64Cu-NOTA-Bn-SCN-Aoc-BN(7-14) was significantly decreased when co-injected with the blocking agent at 1 and 4 h. The SUV analysis also showed 44% and <1% retention of radioactivity in the tumor at 4 h and 24 h compared to 1 h, which is similar to the 36% and 7% observed in the biodistribution studies.
5. Conclusion
We have shown that the copper chelator, SCN-Bn-NOTA, can be coupled to BN(7-14) with retention of affinity to GRPR on PC-3 prostate cancer cells. The resulting conjugates were readily labeled with 64Cu and demonstrated rapid internalization into PC-3 cells. The conjugate has rapid tumor uptake and generally improved tumor/normal tissue ratios at early timepoints after injection. Nevertheless, this improvement does not persist at 24 hours, raising the possibility that either this six coordinate chelator or its metabolites are cleared from the tumor more readily than the previously reported five coordinate systems. That data gathered from this analogue, while encouraging for the potential detection or treatment of GRPR-expressing prostate cancers, could be optimized further.
Acknowledgements
This work was supported by the Department of Radiation Oncology, Washington University School of Medicine and NIH grants R01 CA136695. The authors gratefully acknowledge Margaret Morris, Nicole Fettig, Lori Strong, and Amanda Roth for performing the small animal imaging studies. Dr. Richard LaForest is thanked for his training in analysis of the imaging data.
Financial Support: Supported by the Department of Radiation Oncology, Washington University School of Medicine, NIH grant RO1 CA136695 and a DOE Integrated Radiochemistry Research Project of Excellence Grant (DE-SC00002032).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof ebefore it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Markwalder R, Reubi JC. Gastrin-releasing peptide receptors in the human prostate: Relation to neoplastic transformation. Cancer Res. 1999;59:1152–59. [PubMed] [Google Scholar]
- 2.Reubi JC, Wenger S, Schmuckli-Maurer J, Schaer JC, Gugger M. Bombesin receptor subtypes in human cancers: Detection with the universal radioligand 125I-[d-TYR6, β-ALA11, PHE13, NLE14] Bombesin(6-14) Clin Cancer Res. 2002;8:1139–46. [PubMed] [Google Scholar]
- 3.Anastasi A, Erspamer V, Bucci M. Isolation and structure of bombesin and alytesin, 2 analogous active peptides from the skin of the European amphibians Bombina and Alytes. Experientia. 1971;27:166–167. doi: 10.1007/BF02145873. [DOI] [PubMed] [Google Scholar]
- 4.Breeman WAP, de Jong M, Erion JL, Bugaj JE, Srinivasan A, Bernard BF, et al. Preclinical comparison of 111In-labeled DTPA- or DOTA-bombesin analogs for receptor-targeted scintigraphy and radionuclide therapy. J Nucl Med. 2002;43:1650–56. [PubMed] [Google Scholar]
- 5.Hoffman TJ, Smith CJ. True radiotracers: Cu-64 targeting vectors based upon bombesin peptide. Nucl Med Biol. 2009;36:579–85. doi: 10.1016/j.nucmedbio.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Johnson CV, Shelton T, Smith CJ, Ma L, Perry MC, Volkert WA, et al. Evaluation of combined 177Lu-DOTA-8-AOC-BBN(7-14)NH2 GRP receptor-targeted radiotherapy and chemotherapy in PC-3 human prostate tumor cell xenografted SCID mice. Cancer Biother Radiopharm. 2006;21:155–66. doi: 10.1089/cbr.2006.21.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin KS, Luu A, Baidoo KE, Hashemzadeh-Gargari H, Chen MK, Brenneman K, et al. A new high affinity technetium-99m-bombesin analogue with low abdominal accumulation. Bioconjug Chem. 2005;16:43–50. doi: 10.1021/bc049820h. [DOI] [PubMed] [Google Scholar]
- 8.Maddalena ME, Fox J, Chen J, Feng W, Cagnolini A, Linder KE, et al. 177Lu-AMBA biodistribution, radiotherapeutic efficacy, imaging, and autoradiography in prostate cancer models with low GRP-R expression. J Nucl Med. 2009;50:2017–24. doi: 10.2967/jnumed.109.064444. [DOI] [PubMed] [Google Scholar]
- 9.Mansi R, Wang X, Forrer F, Kneifel S, Tamma ML, Waser B, et al. Evaluation of a 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-conjugated bombesin-based radioantagonist for the labeling with single-photon emission computed tomography, positron emission tomography, and therapeutic radionuclides. Clin Cancer Res. 2009;15:5240–49. doi: 10.1158/1078-0432.CCR-08-3145. [DOI] [PubMed] [Google Scholar]
- 10.Smith CJ, Volkert WA, Hoffman TJ. Radiolabeled peptide conjugates for targeting of the bombesin receptor superfamily subtypes. Nucl Med Biol. 2005;32:733–40. doi: 10.1016/j.nucmedbio.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Zhang H, Chen J, Waldherr C, Hinni K, Wasser B, Reubi JC, et al. Synthesis and evaluation of bombesin derivatives on the basis of pan-bombesin peptides labeled with indium-111, lutetium-177, and yttrium-90 for targeting bombesin receptor-expressing tumors. Cancer Res. 2004;64:6707–15. doi: 10.1158/0008-5472.CAN-03-3845. [DOI] [PubMed] [Google Scholar]
- 12.Parry JJ, Andrews R, Rogers BE. MicroPET imaging of breast cancer using radiolabeled bombesion analogs targeting the gastrin-releasing peptide receptor. Breast Cancer Res Treat. 2007;101:175–83. doi: 10.1007/s10549-006-9287-8. [DOI] [PubMed] [Google Scholar]
- 13.Parry JJ, Kelly TS, Andrews R, Rogers BE. In vitro and in vivo evaluation of 64Cu-labeled DOTA-linker-bombesin(7-14) analogues containing different amino acid linker moieties. Bioconjug Chem. 2007;18:1110–17. doi: 10.1021/bc0603788. [DOI] [PubMed] [Google Scholar]
- 14.Rogers BE, Bigott HM, McCarthy DW, Della Manna D, Kim J, Sharp TL, et al. MicroPET imaging of a gastrin-releasing peptide receptor-positive tumor in a mouse model of human prostate cancer using a 64Cu-labeled bombesin analog. Bioconjug Chem. 2003;14:756–63. doi: 10.1021/bc034018l. [DOI] [PubMed] [Google Scholar]
- 15.Rogers BE, Della Manna D, Safavy A. In vitro and in vivo evaluation of a 64Cu-labeled polyethylene glycol bombesin conjugate. Cancer Biother Radiopharm. 2004;19:25–34. doi: 10.1089/108497804773391649. [DOI] [PubMed] [Google Scholar]
- 16.Biddlecombe GB, Rogers BE, de Visser M, Parry JJ, de Jong M, Erion JL, et al. Molecular imaging of gastrin-releasing peptide receptor-positive tumors in mice using 64Cu- and 86Y-DOTA-(Pro1,Tyr4)-Bombesin(1-14) Bioconj Chem. 2007;18:724–30. doi: 10.1021/bc060281l. [DOI] [PubMed] [Google Scholar]
- 17.Boswell CA, Sun X, Niu W, Weisman GR, Wong EH, Rheingold AL, et al. Comparative in vivo stability of copper-64-labeled cross-bridged and conventional tetraazamacrocyclic complexes. J Med Chem. 2004;47:1465–74. doi: 10.1021/jm030383m. [DOI] [PubMed] [Google Scholar]
- 18.Prasanphanich AF, Nanda PK, Rold TL, Ma L, Lewis MR, Garrison JC, et al. [64Cu-NOTA-8-Aoc-BBN(7-14)NH2] targeting vector for positron-emission tomography imaging of gastrin-releasing peptide receptor-expressing tissues. Proc Natl Acad Sci USA. 2007;104:12462–67. doi: 10.1073/pnas.0705347104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lane SR, Nanda P, Rold TL, Sieckman GL, Figueroa SD, et al. Optimization, biological evaluation and microPET imagin of copper-64-labeled bombesin agonists, [64Cu-NO2A-(X)-BBN(7-14)NH2], in a prostate tumor xenografted mouse model. Nuc Med Biol. 2010;37:751–61. doi: 10.1016/j.nucmedbio.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 20.McCarthy DW, Shefer RE, Klinkowstein RE, Bass LA, Margeneau WH, Cutler CS, et al. Efficient production of high specific activity 64Cu using a biomedical cyclotron. Nucl Med Biol. 1997;24:35–43. doi: 10.1016/s0969-8051(96)00157-6. [DOI] [PubMed] [Google Scholar]
- 21.Sun X, Wuest M, Weisman GR, Wong EH, Reed DP, Boswell CA, et al. Radiolabeling and in vivo behavior of copper-64-labeled crossbridged cyclam ligands. J Med Chem. 2002;45:469–77. doi: 10.1021/jm0103817. [DOI] [PubMed] [Google Scholar]
- 22.Bartolo NMD, Sargeson AM, Donlevy TM, Smith SV. Synthesis of a new cage ligand, SarAr, and its complexation with selected transition metal ions for potential use in radioimaging. J Chem Soc, Dalton Trans. 2001:2303–9. [Google Scholar]
- 23.Wieghardt K, Bossek U, Chaudhuri P, Herrmann W, Menke BC, Weiss J. 1,4,7-Triazacyclononane-N,N’,N”-triacetate (TCTA), a new hexadentate ligand for divalent and trivalent metal ions. Crystal structures of [CrIII(TCTA)], [FeIII(TCTA)], and Na[CuII(TCTA)] Inorg Chem. 1982;21:4308–14. [Google Scholar]
- 24.Anderegg G, Arnaud-Neu F, Delgado R, Felcman J, Popov K. Critical evaluation of stability constants of metal complexes of complexones for biomedical and environmental applications. Pure Appl Chem. 2005;77:1445–95. [Google Scholar]
- 25.Meares CF. Capturing copper for molecular imaging and therapy. In: Chen X, editor. Recent Advances of Bioconjugation Chemistry in Molecular Imaging. Research Signpost; Kerala, India: 2008. pp. 227–41. [Google Scholar]
- 26.Lears KA, Ferdani R, Liang K, Zheleznyak A, Andrews R, Sherman CD, et al. In vitro and in vivo evaluation of 64Cu-labeled SarAr-bombesin analogs in gastrin-releasing peptide receptor-expressing prostate cancer. J Nucl Med. 2011;52:470–77. doi: 10.2967/jnumed.110.082826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prasanphanich AF, Retzloff L, Lane SR, Nanda PK, Sieckman GL, Rold TL, et al. In vitro and in vivo analysis of [64Cu-NO2A-8-Aoc-BBN(7-14)NH2]: a site-directed radiopharmaceutical for positron-emission tomography imaging of T-47D human breast cancer tumors. Nucl Med Biol. 2009;36:171–81. doi: 10.1016/j.nucmedbio.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garrison JC, Rold TL, Sieckman GL, Figueroa SD, Volkert WA, Jurisson SS, et al. In vivo evaluation and small-animal PET/CT of a prostate cancer mouse model using 64Cu bombesin analogs: side-by-side comparison of the CB-TE2A and DOTA chelation systems. J Nucl Med. 2007;48:1327–37. doi: 10.2967/jnumed.107.039487. [DOI] [PubMed] [Google Scholar]
- 29.Cescato R, Maina T, Nock B, Nikolopoulou A, Charalambidis D, Piccand V, et al. Bombesin receptor antagonists may be preferable to agonists for tumor targeting. J Nucl Med. 2008;49:318–26. doi: 10.2967/jnumed.107.045054. [DOI] [PubMed] [Google Scholar]
- 30.Ginj M, Zhang H, Waser B, Cescato R, Wild D, Wang X, et al. Radiolabeled somatostatin receptor antagonists are preferable to agonists for in vivo peptide receptor targeting of tumors. Proc Natl Acad Sci USA. 2006;103:16436–41. doi: 10.1073/pnas.0607761103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kukis DL, Diril H, Greiner DP, DeNardo SJ, DeNardo GL, Salako QA, et al. A comparative study of copper-67 radiolabeling and kinetic stabilities of antibody-macrocycle chelate conjugates. Cancer (Suppl) 1994;73:779–86. doi: 10.1002/1097-0142(19940201)73:3+<779::aid-cncr2820731306>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 32.Van der Merwe MJ, Boeyens JCA, Hancock RD. Crystallographic and thermodynamic study of metal ion size selectivity in the ligand 1,4,7-triazacyclononane-N,N’,N”-triacetate. Inorg Chem. 1985;24:1208–13. [Google Scholar]