Abstract
Background
Short-term results after proximal interphalangeal joint (PIPJ) arthroplasty with pyrolytic carbon (pyrocarbon) implant have shown that this implant suffers from high rates of complications; however patient satisfaction is high. The aim of this study is to evaluate the effectiveness of the pyrocarbon implant for use in PIPJ at a minimum 2 years follow-up.
Methods
Thirteen consecutive candidates who underwent 21 PIPJ arthroplasty with pyrocarbon implant were evaluated prospectively. Functional measurements and the Michigan Hand Outcomes Questionnaire (MHQ) were administered preoperatively and at 12-months, and intermediate-term (>2 years) postoperatively. Preoperative and intermediate-term mean data for all functional measures and MHQ scores were compared.
Results
A total of 13 patients were treated in this study with a mean follow-up of 44 months. Grip strength, key pinch strength, and active arc of motion demonstrated no statistical difference between pre-operative and intermediate-term assessment. All domains of the MHQ showed improved large effect size at intermediate-term follow-up, especially Pain and Satisfaction. There were 10 complications in 9 joints (42.9% complication rate). Patients without complications had better functional outcomes, however there were no statistical differences in MHQ scores between patients with and without complications except for Pain (p=0.04).
Conclusions
PIPJ arthroplasty with pyrocarbon implant seems to be an effective way of reducing pain without sacrificing active arc of motion. Despite a high rate of complications, patients generally were satisfied, especially with pain relief. Additionally, complications do not affect patients’ satisfaction even if hand function was affected. Further decision-making analysis to compare arthroplasty and fusion for each finger may help surgeons to select the appropriate operative procedures.
Levels of Evidence
Therapeutic IV
Keywords: Arthroplasty, Outcome, Proximal interphalangeal joint, Pyrocarbon, Pyrolytic carbon, Surface replacement arthroplasty
INTRODUCTION
Proximal interphalangeal joint (PIPJ) arthritis is a disabling condition that affects 27 million Americans,1 who live with pain, weakness, and deformity. For severe PIPJ arthritis there are 3 treatment options: (1) conservative treatments (medications, reducing activity levels, physical therapy, and/or splinting), (2) fusion, and (3) arthroplasty. However, the selection criterion among these options is controversial. Generally, when pain can no longer be managed by conservative treatments and weakness affects daily activities, surgical intervention is recommended to reduce pain and maintain hand function. The choice between fusion and implant arthroplasty of the PIPJ most often depends on the digit involved. Implant arthroplasty is preferred for the ulnar 2 digits, the ring and small fingers, because these joints are important in power grip. Thus, preservation of joint mobility is necessary. On the other hand, for the painful PIPJ arthritis of the index and long fingers, fusion is usually acceptable; these digits require stability for fine pinch, meaning that preservation of joint mobility is not as important. With the advancement in implant technology, however, patients are more often requesting arthroplasty on the index and long finger, as well.
The ideal resolution for PIPJ arthritis produces a painless and freely movable joint, and the development of implant technology strives toward this goal. The silicone implant has been used since the early 1960s for PIPJ arthroplasty and has contributed to the progress of small joint arthroplasty. However, the silicone implant is not designed anatomically (constrained hinge-type design) and has problems with long-term durability. In addition, implant-related complications, such as implant fracture and dislocation, inflammatory synovitis, joint deformity, heterotopic bone formation, erosive reaction to implant debris, and loss of motion, are quite common and have been reported to be as high as 19%.2–10
Thus, it was apparent that a new type of implant was required, one with biomechanical advantages and fewer complications. Surface replacement arthroplasty was developed as newer prosthetic device for the PIPJ that closely resembles the anatomic configuration of the phalangeal head and the articular base of the middle phalanx (non-constrained design). Surface replacement arthroplasty of the PIPJ has been traditionally performed using a cobalt-chromium proximal component and an ultra-high molecular weight polyethylene (UHMWPE) distal component11-13 and, more recently, using pyrolytic carbon (pyrocarbon) components.
Pyrocarbon implants are the latest technology in this field and have been reported as an ideal joint replacement material because of their excellent wear characteristics and biological compatibility with joint tissues.14–16 Additionally, pyrocarbon implants are unlinked, minimally constrained, and are designed to resemble the anatomic surfaces of PIPJ (a bi-condylar structure), which facilitates flexion-extension motion. Their use requires minimal bone resection, which preserves the collateral ligaments for joint stabilization unlike silicone implants. There is hope that the pyrocarbon implant’s biomechanical advantages over the silicone implant would translate into increased longevity, with fewer long-term complications.
Unfortunately, recent reports presenting the short-term results of PIPJ arthroplasty with pyrocarbon implant have shown that the pyrocarbon implant suffers from similar short-term complications to those of the silicone implant.17–20 Interestingly, nearly all studies have described high patient satisfaction despite these complications.17, 19–21 Our previous study has shown similar encouraging results, primarily in pain relief and patient satisfaction, but also demonstrated complications related to implant dislocations at the time of 12-month follow-up.17 Because short-term outcomes studies have not shown definitely that this new technology was a reliable option for PIPJ arthroplasty, long-term outcomes studies are required. But such studies of the pyrocarbon implant for the PIPJ have not been reported unreported, and even intermediate-term outcomes studies are limited thus far.8, 22 The aim of this study is to evaluate the effectiveness of the pyrocarbon implant in a prospective cohort of patients who underwent PIPJ arthroplasty with follow-up period of at least 24 months.
PATIENTS AND METHODS
Between November of 2004 and May 2009, 13 consecutive patients underwent 21 PIPJ arthroplasties with pyrocarbon implant (Ascension Orthopedics, Austin, Texas) and were analyzed prospectively. The primary indication for this procedure was intractable pain in the PIPJ unresponsive to conservative treatments. Inclusion criteria were the following: age of 18 years or older, the ability to read and write in English, the cognitive ability to complete the outcomes assessment. Every patient who presented during the study period met the inclusion criteria and was successfully recruited. Written informed consent was obtained from each patient. Patients were evaluated 3 month, 6 months and 12 months following surgery. During May 2011 through July 2011 all patients who had surgery prior to May 2009 were invited back to the hand clinic to undergo an intermediate-term follow-up evaluation. Patients were compensated $20 for their time. This study was approved by the University of Michigan Medical School Institutional Review Board.
Functional Assessment
Grip strength, key pinch strength, and active arc of motion (AAM), were assessed preoperatively, 12-months postoperatively, and at follow-up of at least 2 years. Grip and pinch strength were measured by a researcher with a Jamar dynamometer (Sammons Preston Rolyan, Bolingbrook, Ill.) and a pinch gauge (B&L Engineering, Tustin, Calif.), respectively. AAM was measured by an independent certified hand therapist.
Patient-Rated Assessment
The Michigan Hand Outcomes Questionnaire (MHQ) was also administered preoperatively, 12-months postoperatively, and at final follow-up. The MHQ is a self-administered instrument that measures 6 health-status domains that are important to patients with hand disorders: overall hand function, activities of daily living, pain, work performance, aesthetics, and patient satisfaction. The responsiveness, reliability, and validity of the MHQ have been proven for a variety of common hand conditions.23–29 Patient demographic data were also collected.
Complications
The preoperative and postoperative radiographs (at 3 months, 6 months, 12 months postoperatively, and final follow-up) were evaluated for signs of osseointegration and loosening. Osseointegration was assessed by measuring the width of resorption zones around the implant. Each PIPJ pyrocarbon implant has a radiopaque core coated with 0.5 mm of radiolucent carbon, so periprosthetic lucency is expected.30 Only implants that exhibited irregular periprosthetic lucency of >0.5 mm at the time of the final follow-up were considered loose by radiographic criterion. The grading system for the migration of small bone implants created by Sweets et al.22 was used (Grade 0, a well-aligned implant; Grade 1, macroscopically evident migration; Grade 2, severe migration with the stem opposing the cortex; and Grade 3, breach of the cortex by the stem). Grades 2 and 3 were defined as implant migrations in this study.
Statistical Analysis
Means and standard deviations were assessed for functional outcomes preoperatively, 12-months postoperative and final follow-up time points. Grip strength and key pinch strength were calculated as the percentage of the contralateral hand. Based on the standard method of correcting for hand dominance, the resulting percentage was adjusted for a 10% increase in strength of the dominant hand.31 Preoperative means and intermediate-term postoperative means for all functional outcome measures were compared using the Wilcoxon signed rank test because normality of these samples could not be established. Mean arc of motion was summarized by the total number of joints involved, whereas grip strength and key pinch scores were summarized by total number of patients involved.
MHQ score and subscale means and standard deviations were assessed at preoperative, 12-month and final time points. Standardized effect size was used to determine the magnitude of change between preoperative and final postoperative scores; an effect size of 0.2 was defined as a small effect, 0.5 as medium effect and 0.8 as large effect based on Cohen’s criteria.32 We also compared intermediate-term functional outcomes and MHQ scores between patients with complications and patients without complication using the Mann-Whitney U test, the non-parametric version of the 2-sample independent t-test. All statistical analysis was performed using SAS 9.2 (SAS Institute, Inc., Cary N.C.) software.
RESULTS
A total of 13 patients, 11 women and 2 men, were treated in this study. Nine patients had a single unilateral procedure, and 4 patients had multiple procedures, including 3 bilateral cases. Each procedure was performed separately because of the technical difficulty associated with this procedure and the possibility of dislocation. The majority of patients had a diagnosis of osteoarthritis (77%). One pyrocarbon implant replaced an existing silicone implant. One procedure was performed after an unsuccessful microvascular toe joint transfer. The mean follow-up period was 44 months with a range of 24–76 months. The demographic information is listed in Table 1.
Table 1.
Patient Demographic Data
| Value | |
|---|---|
| Joints | 21 |
| Patients | 13 |
| Gender (female/male) | 11 / 2 |
| Age (yrs) | |
| Overall | |
| Mean (range) | 57 (48–72) |
| Female | |
| Mean (range) | 56 (50–61) |
| Male | |
| Mean (range) | 60 (48–72) |
| Long-term follow-up (months) | |
| Mean (Range) | 44 (24–76) |
| Laterality of procedure* | |
| Right/Left | 11 / 10 |
| Digit involved | |
| Index | 5 |
| Long | 10 |
| Ring | 5 |
| Small | 1 |
| Diagnosis | |
| Osteoarthritis | 10 |
| Post-traumatic arthritis | 1 |
| Psoriatic arthritis | 1 |
| Septic arthritis | 1 |
Three patients had bilateral procedures
Functional Outcomes
Table 2 shows the functional outcomes data. Functional data were available for 13 patients preoperatively, 6 patients at 12-months and 13 patients at final follow-up. There was no significant change in grip strength over the follow-up period. Key pinch strength improved at 12-months but the intermediate-term outcome was slightly worse; however, the difference between preoperative and intermediate-term assessments was not significant. AAM data were available for 19 joints preoperatively, 8 joints at 12-month and 21 joints at final follow-up. At intermediate-term follow-up, AAM improved but the difference was not statistically significant. All t test results were confirmed with Wilcoxon signed rank sum tests.
Table 2.
Functional Outcome, Mean ± 95%CI
|
p Value |
||||
|---|---|---|---|---|
| Preoperatively | 12 months | Intermediate-term* | Wilcoxon Signed Rank Test† |
|
| Grip strength (kg) | 11.0±9.9 | 12.9±12.0 | 12.4±13.5 | 0.692 |
| Grip strength (%) of contralateral | 71.4±52.3 | 57.2±36.7 | 77.4±38.7 | 0.301 |
| Key pinch (kg) | 6.3±2.9 | 8.4±3.0 | 4.8±4.2 | 0.182 |
| Key pinch (%) of contralateral | 91.3±16.0 | 82.7±41.0 | 95.7±17.6 | 0.129 |
| Active arc of motion (°) | 43°±16° | 39°±19° | 51°±24° | 0.341 |
Intermediate-term: ≥ 24 months after operation (mean follow-up=44 months)
The p value was calculated using the Wilcoxon signed rank sum test for non-parametric paired samples comparing preoperative mean and intermediate-term means (significance at p < 0.05). Because normality could not be established, we applied the Wilcoxon signed rank sum test to confirm the t test result
Patient-Rated Outcomes
MHQ data were available for 13 patients preoperatively, for 6 patients at 12-months and 13 at final follow-up. All domains of the MHQ improved greatly at 12-months postoperatively and stayed high at intermediate-term follow-up. All domains showed large effect size (>0.8) at intermediate-term follow-up, with the exception of Work (effect size: 0.2) and Aesthetics (effect size: 0.5) domain. (Table 3) This result indicates pyrocarbon implant arthroplasty improves many aspects of patients’ hand function, especially Pain (effect size: 1.7), and this leads to high satisfaction with the outcomes (effect size: 1.8). Over the intermediate-term period, some domains slightly decreased compared to 12-months postoperatively, however patient-rated satisfaction continued to be high.
Table 3.
Michigan Hand Outcome Questionnaire Data*
| Domain | Preoperatively | 12 months | Intermediate-term | Effect Size† |
|---|---|---|---|---|
| Overall | 43 ± 12 | 63 ± 23 | 62 ± 19 | 1.2 |
| Function | 54 ± 17 | 65 ± 18 | 69 ± 14 | 1.0 |
| ADL | 53 ± 19 | 70 ± 25 | 70 ± 20 | 0.8 |
| Work | 53 ± 24 | 66 ± 25 | 58 ± 28 | 0.2 |
| Pain | 66 ± 14 | 33 ± 36 | 31 ± 25 | 1.7 |
| Aesthetics | 32 ± 18 | 58 ± 27 | 44 ± 29 | 0.5 |
| Satisfaction | 29 ± 13 | 51 ± 35 | 62 ± 22 | 1.8 |
ADL: activities of daily living
The Michigan Hand Outcomes Questionnaire domains are based on a scale of 0 to 100. For all domains except Pain, a higher score indicates better performance. For the Pain domain, a lower score indicates less pain.
The effect size is defined as (mean2 - mean1)/(SD of difference in means). An effect size of 0.2 is small, 0.5 is medium, and 0.8 is large.
Complications
Thirteen of 21 pyrocarbon implants (62%) demonstrated radiographic signs of loosening at the most recent follow-up point. There were a total of 10 complications in 9 joints, affecting 9 patients; 12 joints (4 patients) were free of complications (Table 4). The complication rate by joint was 43%. Seven implants experienced dislocation (33%), 2 implants had intermittent squeaking of the pyrocarbon joints (10%), and 1 case experienced a minor incision infection, treated with antibiotics. Interestingly, all implant-related complications (dislocation and squeaking) were identified in the index and long fingers, although our present series does had a high proportion of index and long fingers arthroplasties (71%). All cases of implant dislocation were managed conservatively by dorsal blocking splinting, because the patients did not complaint of pain and/or functional disability. Although we offered PIPJ fusion to patients with complications, no patient has opted to pursue this option at this time.
Table 4.
Complications
| Type of complication |
Sex | Primary diagnosis | Digit(s) involved (follow-up: Mos) |
Complication | Implant loosening (+/−) |
Treatment | Comments |
|---|---|---|---|---|---|---|---|
|
Major | |||||||
| F | Degenerative osteoarthritis |
Rt-long (36) | Dislocation | + | Conservative | ||
| F | Degenerative osteoarthritis |
Rt-index (68) Rt-long (76) |
Dislocation (Rt-index) |
+ (1 implant) |
Conservative | ||
| F | Degenerative osteoarthritis |
Lt-ring (39) Lt-long (46) Rt-index (50) Rt-ring (58) |
Dislocation (Lt-long) |
+ (2 implants) |
Conservative | After silicone implant (Lt-long) |
|
| M | Degenerative osteoarthritis |
Rt-long (55) | Dislocation | + | Conservative | ||
| F | Septic arthritis | Lt-long (36) | Dislocation | + | Conservative | ||
| F | Degenerative osteoarthritis |
Lt-long (24) | Dislocation | + | Conservative | ||
| F | Psoriatic arthritis | Lt-long (38) | Dislocation, Squeaking |
+ | Conservative | ||
|
Minor | |||||||
| F | Degenerative osteoarthritis |
Rt-index (35) Lt-long (62) Lt-ring (69) |
Squeaking (Rt-index) |
+ (1 implant) |
No treatment | ||
| F | Degenerative osteoarthritis |
Lt-ring (31) Rt-long (46) Rt-ring (50) |
Infection of incision (Lt-ring) |
− | Antibiotics | ||
|
Non- complications | |||||||
| M | Posttraumatic arthritis |
Lt-long (28) | N/A | + | N/A | After toe transfer | |
| F | Degenerative osteoarthritis |
Rt-small (35) | N/A | − | N/A | ||
| F | Degenerative osteoarthritis |
Lt-index (45) | N/A | + | N/A | ||
| F | Degenerative osteoarthritis |
Lt-index (24) | N/A | + | N/A | ||
F: female, M: male, Rt: right, Lt: left
Patients without complications (4 cases, listed in Table 4) had significantly better AAM compared to patients with complications (9 cases) (p=0.05) (Table 5). Patients without complication also had higher MHQ scores in every domain but the differences were not statistical significant except for Pain (p=0.04).
Table 5.
Intermediate-term Outcome Comparison- Patients with Complication and without Complication
| Function | With Complication |
Without Complication |
p Value£ |
|---|---|---|---|
| Grip strength, kg | 9.5 ± 13.9 | 17.0 ± 13.0 | 0.38 |
| Grip strength, % of contralateral | 60.5 ± 37.6 | 98.5 ± 32.2 | 0.11 |
| Key pinch, kg | 4.0 ± 3.7 | 6.1 ± 5.1 | 0.56 |
| Key pinch, % of contralateral | 102.8 ± 15.9 | 86.9 ± 17.3 | 0.39 |
| Jebsen-Taylor score | 28.0 ± 13.8 | 27.3 ± 5.9 | 0.94 |
| Active arc of motion | 43° ± 21° | 65° ± 24° | 0.05 |
| MHQ | With Complication |
Without Complication |
p Value£ |
|---|---|---|---|
| Overall | 57 ± 20 | 71 ± 15 | 0.42 |
| Function | 68 ± 14 | 72 ± 14 | 0.66 |
| ADL | 65 ± 23 | 76 ± 16 | 0.42 |
| Work | 51 ± 28 | 70 ± 26 | 0.24 |
| Pain | 41 ± 26 | 15 ± 14 | 0.04 |
| Aesthetics | 41 ± 25 | 48 ± 37 | 0.83 |
| Satisfaction | 60 ± 23 | 72 ± 18 | 0.27 |
Comparison of functional outcomes and MHQ score were assessed with Mann-Whitney U test.
CASE REPORTS
Case 1
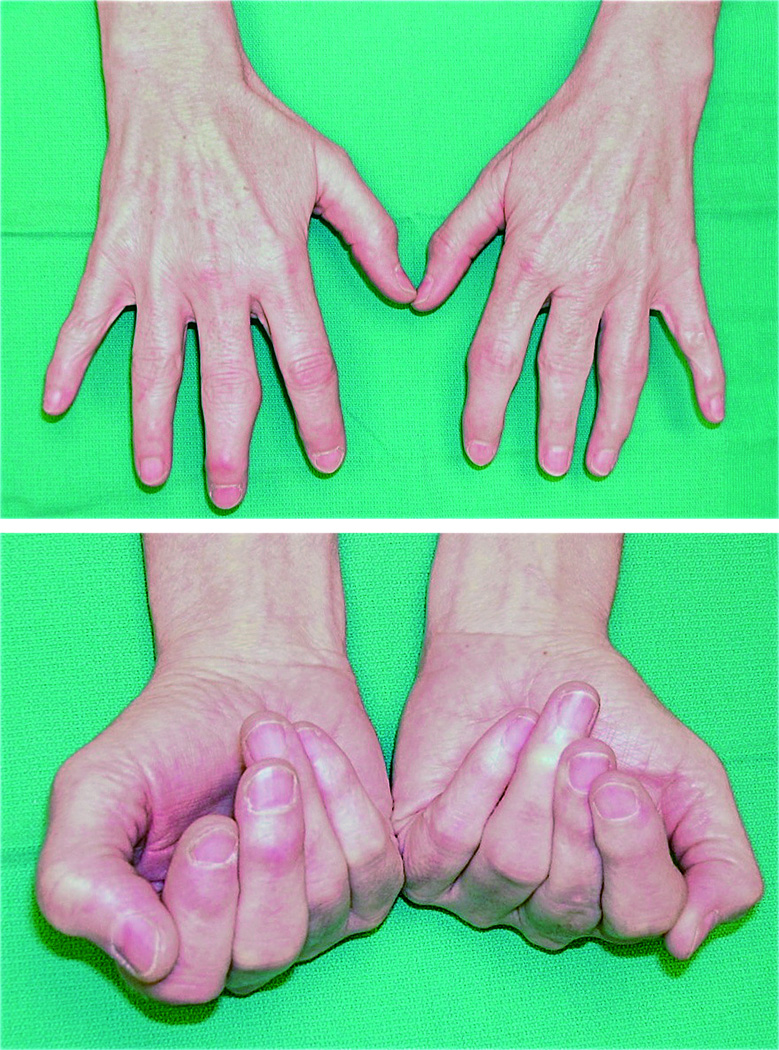
A 52-year-old right hand-dominant retired data entry clerk with a long-standing history of degenerative osteoarthritis affecting multiple joints of the hands (Figure 1a and 1b) previously underwent silicone implant arthroplasty of the left long finger PIPJ and distal interphalangeal joint (DIPJ) fusions of the right index, long, ring, and small fingers. She developed intractable pain in the right long PIPJ with osteoarthritis visible on X-ray (Figure 2), on which she chose to have pyrocarbon arthroplasty performed. Her recovery was unremarkable and she was pleased with the results, particularly pain relief. Three month after surgery, physical examination revealed mild hyperextension at the implanted joint, confirmed by X-ray (Figure 3). Three years after surgery, the implant was completely dislocated and the PIPJ was subluxed dorsally (Figure 4), however, the patient reported no problems in her daily activities and demonstrated good motion. The appearance of the hand 3 years postoperatively (Figure 5a and 5b) is almost similar to the preoperative one.
Figure 1.
a, b Case 1. Preoperative clinical pictures of a 52-year-old woman with a long history of osteoarthritis affecting multiple joints of the hands
(a) Extension view
(b) Flexion view
Figure 2.
Case 1. The osteoarthritic PIPJ in the right long finger with most severe symptoms will be replaced by a pyrocarbon implant
Figure 3.
Case 1. Radiograph of a right long proximal interphalangeal pyrocarbon joint (3 months after surgery)
Figure 4.
Case 1. Radiograph shows a dislocated right long proximal interphalangeal pyrocarbon joint (3 years after surgery)
Figure 5.
a, b Case 1. Extension (a) and flexion (b) views showing good motion of the right long PIPJ
Case 2
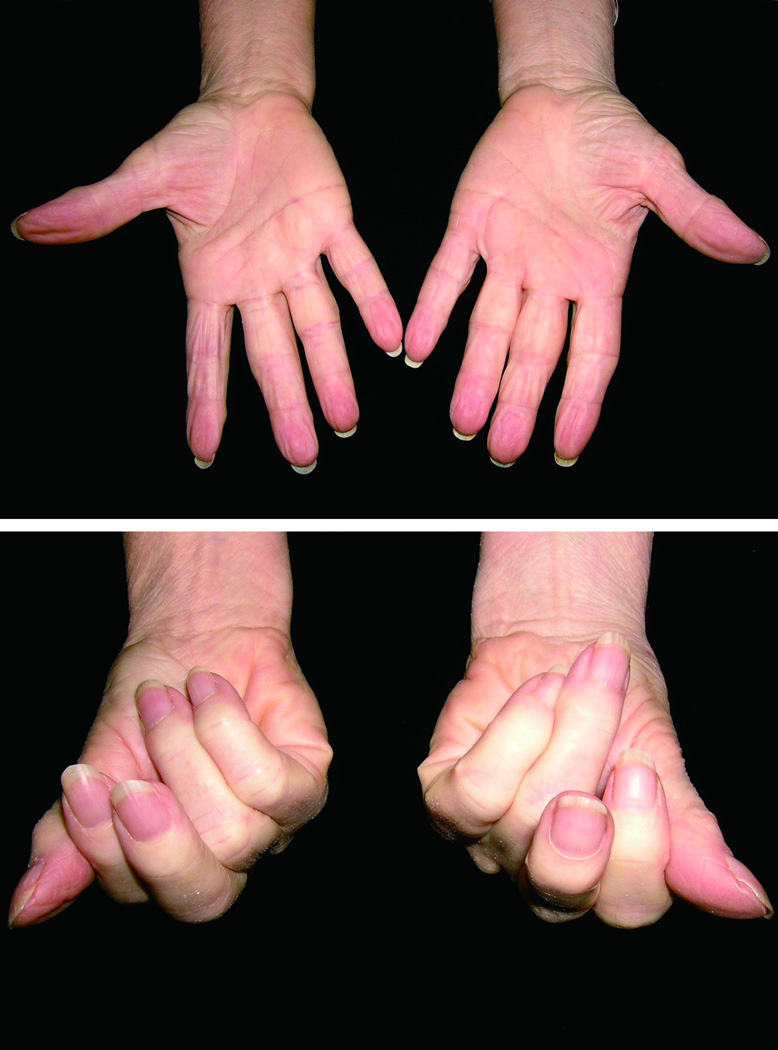
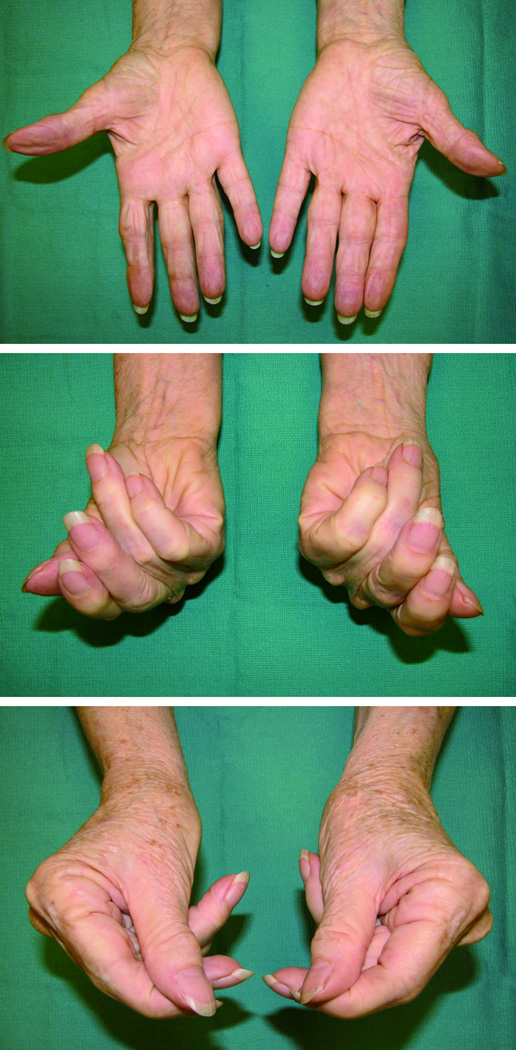
A 59-year-old, right hand–dominant female psychologist with history of diffuse degenerative osteoarthritis of the bilateral hands (Figure 6a and 6b), previously underwent silicone implant arthroplasty of the left long finger PIPJ. She had developed intractable pain and tenderness in her right index and long PIPJs. She underwent right index finger PIPJ arthroplasty with pyrocarbon implant (1st procedure), followed by right long finger PIPJ pyrocarbon arthroplasty 8 months later (2nd procedure). The patient was satisfied with pain relief immediately after these surgeries (Figure 7a and 7b). Ten months after the 1st procedure, the patient recognized a decreased range of motion as well as a clicking of her right index finger, although x-ray showed no evidence of the implant’s dislocation or loosening. Seventeen months after the 1st procedure, the pyrocarbon implant of the right index finger was dislocated (Figure 8a and 8b). Radiographic studies also showed the loosening of the implant. Although the range of motion of the index finger decreased, the index finger appears to be in appropriate position with no malrotation and is not causing the patient any pain (Figure 9a, 9b, and 9c). The patient was still able to perform activities of her daily living and did not desire fusion of this joint.
Figure 6.
a, b Case 2. Preoperative clinical pictures of a 59-year-old woman with a history of diffuse degenerative osteoarthritis of the bilateral hands
(a) Extension view
(b) Flexion view
Figure 7.
a, b Case 2. Radiograph showing stable and mobile right index PIPJ (immediately after surgery)
(a) Lateral view
(b) Anteroposterior view
Figure 8.
a, b Case 2. Radiograph shows a dislocated right index proximal interphalangeal pyrocarbon joint (17 months after surgery)
Figure 9.
a, b, c Case 2. The right index finger appears to be in appropriate position with no malrotation, although the range of motion of the finger decreased
(a) Extension view
(b) Flexion view
(c) Lateral pinch view
DISCUSSION
Although the data suggest that PIPJ pyrocarbon implants deliver excellent in vivo durability and biomechanics, there are no convincing data thus far to support the use of this prosthesis over the traditional silicone implant for the osteoarthritic PIPJ. Because the pyrocarbon implant is a relatively new technology, it has not been well investigated. There are currently 6 English language publications presenting short-term outcomes after pyrocarbon implant PIPJ arthroplasty.17–21, 33 (Table 6) Most outcomes studies of the short-term use of pyrocarbon implants for the PIPJ have shown high patient satisfaction, but nearly all studies have described some radiographic loosening of the implant and/or high rate of clinical complications. There are currently only 2 published reports evaluating intermediate-term outcomes after pyrocarbon PIPJ arthroplasty8, 22 (Table 6). Bravo et al.8 retrospectively studied a total of 50 implants in 35 patients with a minimum follow-up period of 27 months in 2007. In that study, decreased pain scores on a visual analog scale (VAS), improved grip and pinch, and subjective patient satisfaction (80%) were noted. The authors, however, showed that additional procedures were needed in 28% of joints, including 4 that were revised for instability (although dislocation was not specifically reported) and 4 that were revised for loosening of the implants. The authors also noted that 40% of the implants showed radiographic migration at the time of the final evaluation.
Table 6.
Published Reports on PIPJ Arthroplasty with Pyrocarbon Implants
| Report | Evaluation Group |
Follow- up (Month) |
Functional Outcomes |
Pain (No of Joints) |
Patients’ Satisfaction (No of Joints) |
Radiograph Findings (No of Joints) |
Complications (No of Joints) |
|---|---|---|---|---|---|---|---|
| Short-term study | |||||||
|
Tuttle et al 200619 |
18 joints 8 patients |
Mean 13 |
|
|
|
|
|
|
Herren et al 200620 |
17 joints 14 patients |
Mean 19 |
|
|
|
|
|
|
Nunley et al 200618 |
7 joints 5 patients |
Mean 17 |
|
|
|
|
|
|
Meier et al 200721 |
24 joints 20 patients |
Mean 15 | N/A |
|
|
|
|
|
Chung et al 200917 |
21 joints 14 patients |
> 12 |
|
|
|
N/A |
|
|
Wijk et al 201033 |
53 joints 43 patients |
Mean 23 |
|
|
|
N/A |
|
| Intermediate-term Study | |||||||
|
Bravo et al 20078 |
50 joints 35 patients |
Mean 37 >27 |
|
|
|
|
|
|
Sweets et al 201122 |
31 joints 17 patients |
Mean 55 >24 |
|
|
|
|
|
ROM: range of motion, VAS: visual analog scale, DASH: Disabilities of the Arm, Shoulder, and Hand, COPM: Canadian Model of Occupational Performance, JT test: Jebsen-Taylor test, MHQ: Michigan Hand Outcomes Questionnaire
In 2011, Sweets et al.22 presented minimum 2 year follow-up data of a total of 31 implants in 17 patients with an average follow-up of 55 months, which can be comparable to our data because of use of the MHQ. The average VAS score for pain was 3/10 and satisfaction averaged 3.4 points on a 5-point Likert scale; 12 of 17 patients stated that they would repeat the surgery. However, the arc of motion of the PIPJ decreased from 57° preoperatively to 31° (p < 0.05) postoperatively, when the involved hand was compared with the noninvolved hand at final follow-up all domains of the MHQ showed significant poorer scores, except Aesthetics. The authors also noted a high rate of complications, including joint contracture in 20 joints, subsidence and loosening in 15 joints, squeaking in 11 joints, dislocation in 5 joints, implant fracture in 1 joint, and a reoperation rate of 19%. Therefore, the authors concluded that pyrocarbon implant arthroplasty for PIPJ had a high complication rate, poor outcomes, and variable patient satisfaction, and they stopped performing this procedure.
Our study also noted a higher incidence of complications (43%) compared to our short-term result, including dislocation in 7 joints. One reason for the high complication rate in our series may be the high proportion of index and long finger arthroplasties; all implant-related complications were observed in these 2 fingers. The index and long fingers require stability for fine pinch, and this functional characteristic may overload the implant and cause a high rate of implant-related complications, compared to ring and small fingers. Radiographic analysis demonstrated high frequency of implants loosening (57%). Compared to the silicone implant, the rate of the dislocation of pyrocarbon implant (33%) is almost the same as the rate of fracture (including suspected fractures) of the silicone implant (30%).10 Additionally, radiographic changes in both silicone and pyrocarbon implants are frequently seen. As to silicone PIPJ arthroplasty, Adamson et al.34 reported sclerosis around 43% of implants, and Ashworth et al.3 found sclerosis in 78% of cases and bony resorption in 12% of cases at long-term follow-up (mean ≥ 5.8 years). In pyrocarbon implants, radiographic signs of loosening and/or migration of the implant can be seen in 40–62% of the joints at intermediate-term follow-up (> 2 years).8, 22 The incidence rate of radiographic changes after pyrocarbon PIPJ arthroplasty may further increase with an additional follow-up time.
Despite these complications, patients are generally were satisfied. MHQ scores compared pre- and postoperatively in the involved hands, showed large effect size for Satisfaction. This result is most likely linked to large effect size in the Pain domain as well. The domains of Work and Aesthetics, showed lower effect size, which indicate that patients’ hands are still low functioning and their appearances are not ideal. Sweets et al reported that 12 of their 17 patients would undergo PIPJ pyrocarbon arthroplasty again, which points to high patient satisfaction. However, when the involved and noninvolved hands were compared, patients were significantly less satisfied with the involved hand.22
Based in part on these poor results and on the number and severity of complications, Sweets et al. opted to discontinue use of the pyrocarbon implant for PIPJ arthroplasty. We also found a high rate of complications, but high patient satisfaction and the repeated request for this type of implant prompted us to continue its use. In both short- and intermediate-term result studies, common findings are significant pain relief, high patient satisfaction, and high rates of complications. Additionally, radiographic findings reveal a higher rate of loosening with migration of the implants at intermediate-term follow-up compared to short-term results. The manufacturer initially stated that the pyrocarbon implant had the potential for bony ingrowth, but recent studies have confirmed that no bony ingrowth occurs between pyrocarbon and the surrounding bone. This indicates that the surrounding bone does not form a stable interface with these implants, and number of complications related to implant loosening may increase over the time. Biomaterial properties research aimed at achieving osteointegration may solve the loosening problem associated with pyrocarbon, given that the surface replacement concept for the current PIPJ implant design appears to be a sensible approach.
Arthroplasty of the PIPJ with a pyrocarbon implant seems to be an effective way of reducing pain without sacrificing AAM. Despite a high rate of complications, patients in our series were generally satisfied. At our center we attribute this to performing the procedure only on self-selecting patients who have suffered with painful hand arthritis for many years, sometimes decades. Patients are also well prepared for the lengthy recovery and possible complication.
Long-term outcomes studies in this field are still limited, and it is difficult to conclude whether pyrocarbon PIPJ arthroplasty is warranted over other PIPJ arthroplasties, or even PIPJ fusion. Long-term studies comparing the outcomes of index and long finger arthroplasties versus ring and small finger arthroplasties may be beneficial in light of the characteristic differences between these 2 groups. Further decision-making analysis to compare pyrocarbon implants and other implants, and PIPJ arthroplasty and fusion may help surgeons to select the appropriate operative procedure.
ACKNOWLEDGMENTS
This study was supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to K.C.C.). The authors thank Jeanne Riggs, C.H.T., for performing the hand therapy and measurements for patients in this study.
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (to Dr. Kevin C. Chung).
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure:
None of the authors has a financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Squitieri L, Chung KC. A systematic review of outcomes and complications of vascularized toe joint transfer, silicone arthroplasty, and PyroCarbon arthroplasty for posttraumatic joint reconstruction of the finger. Plast Reconstr Surg. 2008;121:1697–1707. doi: 10.1097/PRS.0b013e31816aa0b3. [DOI] [PubMed] [Google Scholar]
- 3.Ashworth CR, Hansraj KK, Todd AO, Dukhram KM, Ebramzadeh E, Boucree JB, Hansraj MS. Swanson proximal interphalangeal joint arthroplasty in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1997;342:34–37. [PubMed] [Google Scholar]
- 4.Foliart DE. Swanson silicone finger joint implants: a review of the literature regarding long-term complications. J Hand Surg Am. 1995;20:445–449. doi: 10.1016/S0363-5023(05)80104-2. [DOI] [PubMed] [Google Scholar]
- 5.Hage JJ, Yoe EP, Zevering JP, de Groot PJ. Proximal interphalangeal joint silicone arthroplasty for posttraumatic arthritis. J Hand Surg Am. 1999;24:73–77. doi: 10.1053/jhsu.1999.jhsu24a0073. [DOI] [PubMed] [Google Scholar]
- 6.Pellegrini VD, Jr., Burton RI. Osteoarthritis of the proximal interphalangeal joint of the hand: arthroplasty or fusion? J Hand Surg Am. 1990;15:194–209. doi: 10.1016/0363-5023(90)90096-a. [DOI] [PubMed] [Google Scholar]
- 7.Beckenbaugh RD, Dobyns JH, Linscheid RL, Bryan RS. Review and analysis of silicone-rubber metacarpophalangeal implants. J Bone Joint Surg Am. 1976;58:483–487. [PubMed] [Google Scholar]
- 8.Bravo CJ, Rizzo M, Hormel KB, Beckenbaugh RD. Pyrolytic carbon proximal interphalangeal joint arthroplasty: results with minimum two-year follow-up evaluation. J Hand Surg Am. 2007;32:1–11. doi: 10.1016/j.jhsa.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Stanley JK, Evans RA. What are the long term follow-up results of silastic metacarpophalangeal and proximal interphalangeal joint replacements? Br J Rheumatol. 1992;31:839. doi: 10.1093/rheumatology/31.12.839. [DOI] [PubMed] [Google Scholar]
- 10.Takigawa S, Meletiou S, Sauerbier M, Cooney WP. Long-term assessment of Swanson implant arthroplasty in the proximal interphalangeal joint of the hand. J Hand Surg Am. 2004;29:785–795. doi: 10.1016/j.jhsa.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Linscheid RL, Murray PM, Vidal MA, Beckenbaugh RD. Development of a surface replacement arthroplasty for proximal interphalangeal joints. J Hand Surg Am. 1997;22:286–298. doi: 10.1016/S0363-5023(97)80165-7. [DOI] [PubMed] [Google Scholar]
- 12.Johnstone BR. Proximal interphalangeal joint surface replacement arthroplasty. Hand Surg. 2001;6:1–11. doi: 10.1142/s021881040100045x. [DOI] [PubMed] [Google Scholar]
- 13.Jennings CD, Livingstone DP. Surface replacement arthroplasty of the proximal interphalangeal joint using the PIP-SRA implant: results, complications, and revisions. J Hand Surg Am. 2008;33(1565):e1–e11. doi: 10.1016/j.jhsa.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 14.Cook SD, Beckenbaugh RD, Redondo J, Popich LS, Klawitter JJ, Linscheid RL. Long-term follow-up of pyrolytic carbon metacarpophalangeal implants. J Bone Joint Surg Am. 1999;81:635–648. doi: 10.2106/00004623-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Leuer LH, Gross JM, Johnson KM. Material properties, biocompatibility, and wear resistance of the Medtronic pyrolytic carbon. J Heart Valve Dis. 1996;5:S105–S109. [PubMed] [Google Scholar]
- 16.Ryder JK, Cao H. Structural integrity assessment of heart valve prostheses: a damage tolerance analysis of the CarboMedics Prosthetic Heart Valve. J Heart Valve Dis. 1996;5:S86–S96. [PubMed] [Google Scholar]
- 17.Chung KC, Ram AN, Shauver MJ. Outcomes of pyrolytic carbon arthroplasty for the proximal interphalangeal joint. Plast Reconstr Surg. 2009;123:1521–1532. doi: 10.1097/PRS.0b013e3181a2059b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nunley RM, Boyer MI, Goldfarb CA. Pyrolytic carbon arthroplasty for posttraumatic arthritis of the proximal interphalangeal joint. J Hand Surg Am. 2006;31:1468–1474. doi: 10.1016/j.jhsa.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 19.Tuttle HG, Stern PJ. Pyrolytic carbon proximal interphalangeal joint resurfacing arthroplasty. J Hand Surg Am. 2006;31:930–939. doi: 10.1016/j.jhsa.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 20.Herren DB, Schindele S, Goldhahn J, Simmen BR. Problematic bone fixation with pyrocarbon implants in proximal interphalangeal joint replacement: short-term results. J Hand Surg Br. 2006;31:643–651. doi: 10.1016/j.jhsb.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Meier R, Schulz M, Krimmer H, Stutz N, Lanz U. Proximal interphalangeal joint replacement with pyrolytic carbon prostheses. Oper Orthop Traumatol. 2007;19:1–15. doi: 10.1007/s00064-007-1192-8. [DOI] [PubMed] [Google Scholar]
- 22.Sweets TM, Stern PJ. Pyrolytic carbon resurfacing arthroplasty for osteoarthritis of the proximal interphalangeal joint of the finger. J Bone Joint Surg Am. 2011;93:1417–1425. doi: 10.2106/JBJS.J.00832. [DOI] [PubMed] [Google Scholar]
- 23.Waljee JF, Chung KC, Kim HM, et al. Validity and responsiveness of the Michigan Hand Questionnaire in patients with rheumatoid arthritis: a multicenter, international study. Arthritis Care Res. 2010;62:1569–1577. doi: 10.1002/acr.20274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horng YS, Lin MC, Feng CT, Huang CH, Wu HC, Wang JD. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder, and Hand questionnaire in patients with hand injury. J Hand Surg Am. 2010;35:430–436. doi: 10.1016/j.jhsa.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 25.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 26.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42:619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Kotsis SV, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder and Hand questionnaire in carpal tunnel surgery. J Hand Surg Am. 2005;30:81–86. doi: 10.1016/j.jhsa.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 28.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg Am. 2004;29:646–653. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg Am. 2007;32:84–90. doi: 10.1016/j.jhsa.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Clinical update. No 2. Vol 1. Austin, TX: Ascension Orthopedics; 2005. pp. 1–6. [Google Scholar]
- 31.Petersen P, Petrick M, Connor H, Conklin D. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989;43:444–447. doi: 10.5014/ajot.43.7.444. [DOI] [PubMed] [Google Scholar]
- 32.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 33.Wijk U, Wollmark M, Kopylov P, Tägil M. Outcomes of proximal interphalangeal joint pyrocarbon implants. J Hand Surg Am. 2010;35:38–43. doi: 10.1016/j.jhsa.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 34.Adamson GJ, Gellman H, Brumfield RH, Jr, Kuschner SH, Lawler JW. Flexible implant resection arthroplasty of the proximal interphalangeal joint in patients with systemic inflammatory arthritis. J Hand Surg Am. 1994;19:378–384. doi: 10.1016/0363-5023(94)90049-3. [DOI] [PubMed] [Google Scholar]