Abstract
Purpose
To evaluate what psychological and behavioral factors predict who is likely to seek SNP-based genetic test for multiple common health conditions where feedback can be used to motivate primary prevention.
Methods
Adults aged 25 to 40, who were enrolled in a large managed care organization were surveyed. Those eligible could log on to a secure study Web site to review information about the risks and benefits of a SNP-based genetic test and request free testing. Two primary outcomes are addressed: Accessing the Web (yes, no) and deciding to be tested (completed a blood draw at the clinic)
Results
Those considering genetic susceptibility testing did hold genetically deterministic beliefs (0.42 on scale of 0-behavior to 1-genetic), but believed genetic information to be valuable and were confident they could understand such information. Individuals who believed it important to learn about genetics (OR=1.28), were confident they could understand genetics (OR=1.26), and reported the most health habits to change (OR=1.39) were most likely to get tested.
Conclusions
Physician-patient interactions could benefit if physicians develop “net friendly” strategies to capitalize on patients’ interest in online genetics information and leverage the interaction as a teachable moment to encourage family health history assessment and improved health behaviors.
Keywords: personalized genomics, risk assessment, internet, psychosocial predictors
INTRODUCTION
Emboldened by the completion of the sequence of the human genome, many scientists envision a future in which personalized genomic risk information will be provided to individuals to motivate risk-reducing behaviors, and improve primary intervention and treatment. 1, 2 One suggested approach is to conduct whole genome scans of healthy individuals and return personalized risk profiles that identify propensities to multiple health conditions. Ideally, this information would enable individuals to take precautions prior to their experiencing negative health outcomes.
Indeed, the first generation of SNP-based testing is now being marketed directly to consumers. 3 The resulting genomic profiles are based on simultaneously testing for multiple polymorphisms at multiple loci. At prices ranging from $399 to $2500 (with optional added service costs), these tests are still not affordable to most Americans. However, rapid advancements in analysis technologies and decreasing cost means that these tests will likely become affordable in the coming decade.
The lack of proven clinical utility of these tests raises concern among the scientific and medical communities who consider these tests to represent “premature translation.” 4-6 Critics argue that these genetic variants contribute relatively little to risk for common health conditions and that the general public, naïve to the complex and multi-factorial nature of these diseases, could misinterpret results. Moreover, concerns also have been raised that the speed at which genomic knowledge has been uncovered has left little time for health professionals to acquire the skills needed to accurately interpret such test results. 7 Thus, patients presenting with personalized genomic profiles in hand may be met by puzzled primary care physicians and prompt unwarranted referrals to health services.
Currently, little is known about the psychological and behavioral factors that characterize patients who seek genetic susceptibility testing for common preventable health conditions (e.g., heart disease, adult onset diabetes, or common cancers). What little is known comes predominantly from studies of rare hereditary cancer syndromes and Alzheimer’s disease. 8, 9 Individuals seeking genetic testing for these conditions have been relatively homogeneous with respect to socioeconomic status and race (well-educated, white). Moreover, these individuals largely have been recruited from families identified to be at high risk for these syndromes where mutation carriers have up to 80% increased lifetime risk. Thus, not surprisingly, these individuals typically report perceiving themselves to be at high risk for these conditions, and to feel concerned that they may be at genetic risk.8, 10, 11 These results may not generalize to the context of genetic testing for common health conditions in healthy individuals where gene variants act together with environmental and behavioral risk factors to increase risk, and genes alone confer relatively modest increases in risk, usually on the order of 20-30%. 12
The rapid pace of genetic discovery has been complemented with increased distribution of health information via the Internet. Internet access to health information arguably can empower the public as health consumers because it enables user-controlled interactions with information and other customization capabilities, is available virtually free of charge, and covers a breadth of topics. 13 Indeed, in the case of genomic testing, the Internet could provide a platform for a balanced presentation of information whereby individuals can consider, at their own pace and in privacy, whether or not to undergo such testing, all key to informed decision-making. 14 However, concerns too have been raised that over-reliance on the Internet may create a “digital divide” due to unequal Internet access and distrust in the security of information shared online. 15 Data available thus far on health information seekers who use the Internet shows consistently that women, whites, and the highly educated are overrepresented. 15
Concerns also have been raised that Internet health information seeking “triangulates” the patient-physician encounter in ways that can be challenging for both parties. 16 Several editorials have raised practical questions about how physicians might handle patients who present them with genome scans, suggesting that these new technologies may distract from important and valid clinical assessments.17 Yet, little is known about the psychological and behavioral factors that characterize Internet information seekers generally or those seeking genetic information online. Consideration of these factors could help health systems and health care providers prepare for patient demand and as such, inform early steps towards clinical integration of counseling and service delivery that might be prompted by such testing.
In 2006, the Multiplex Initiative, a pre-clinical, multi-center, prospective observational study, was launched. Our primary aim (and the focus of this report) is to evaluate with a population-based sample of healthy adults (i.e., a sampling frame with a known denominator) what factors predicted interest in and uptake of a multiplex genetic susceptibility test (MGST) for eight common health conditions. Our intent was to educate a representative sample of individuals about genetic testing while assessing their social, psychological and behavioral characteristics. This enabled us to compare the characteristics of the sizable group who chose not to be tested to those who requested testing.
We obtained data describing our population-based sampling strategy in which hard-to-reach subgroups, specifically African Americans, men and those with low education were oversampled (Hensley-Alford et al, unpublished). African Americans and men were least likely to complete the baseline survey, and log onto the Web site, and African Americans were least likely to opt for genetic testing. In this report, we explore a broad array of factors previously identified as predictors of health information seeking, 18 to address four questions of importance to understanding the implications of MGST being offered directly to consumers: (1) Were Multiplex Information Seekers inclined to hold genetically deterministic explanations for common preventable health conditions?; (2) Were Multiplex Information Seekers inclined to be “risk perceivers”, that is, report high objective and subjective risk for the health conditions? (3) Were Multiplex Information Seekers inclined to be “skilled information consumers”, that is, report greater competence with the health care system and genetics?; or (4) Were Multiplex Information Seekers inclined to be “health information monitors” that is, especially interested in health information?
MATERIALS AND METHODS
Study Sample
The sampling frame for the Multiplex Initiative was drawn from a pool of 350,000 commercially insured members of a large Midwestern health maintenance organization. Sampling strategies are described in more detail elsewhere (Hensley-Alford et al, unpublished). Briefly, the sample included members identified in the health plans’ enrollment files to be aged 25-40, enrolled continuously for at least two years, assigned to a primary care physician, and self-identified as either being black or white. Diagnosis codes were used to exclude members who had been previously diagnosed with diabetes mellitus, atherosclerotic cardiovascular disease, osteoporosis, or cancer. A random sample of members who matched the selection criteria was drawn, oversampling for: males, African Americans, and individuals living in areas where greater than 10% of residents had low levels education as determined by U.S. census data. An advance letter that included a $2 bill was mailed to all individuals explaining the survey and providing a toll-free number to call to decline participation.
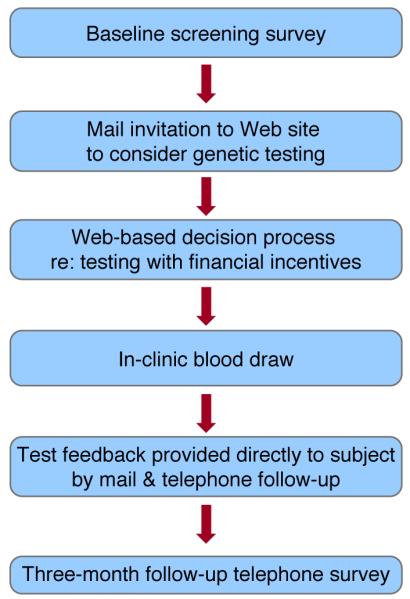
Study Procedures
The flow chart of study procedures is depicted in Figure 1. Recruitment occurred from February 2007 to May 2008. Those who completed the baseline screening survey and deemed eligible were sent a brochure describing the Multiplex study, information to access a secure study Web site (http://www.multiplex.gov) and a $20 bill. Individuals who did not have access to the internet could request hard copies of information pages and could request testing by telephone. At the study Web site, participants could review five information modules about the MGST. The final module offered participants the free test, an offer they could accept or decline. Compensation (gift cards to a national retail chain) was provided for completing online surveys that followed each module. Those requesting testing were asked to schedule a clinic visit for a blood drawn. The Web site described that participants who were tested would receive: (1) a report explaining the meaning of their results in the mail about six months after blood collection; (2) a telephone call from a research educator to discuss the results; and (3) a follow-up telephone survey three months after receiving their test results. Genetic consultations were available at the participant’s request. All procedures were approved by the Institutional Review Boards of the National Human Genome Research Institute and the Henry Ford Health System.
Figure 1.
Multiplex Test
The selection process for the markers included in the MGST is described in detail elsewhere (Wade et al., in press). Briefly, working groups including scientists from a broad range of disciplines engaged in deliberations to arrive at selection criteria and to apply these criteria to the evidence base for genetic variants associated with prevalent health conditions. Gene variants that met criteria identified by the working groups were subjected to an independent peer review by an expert panel whose recommendations were used to develop a final list of gene variants.
The outcome of this process was the development of the MGST that included 15 genetic polymorphisms associated with increased risk for eight common health conditions (type 2 diabetes, lung, colon, and skin cancers; coronary heart disease, hypercholesterolemia, hypertension, and osteoporosis; Table 1). The eight selected health conditions are adult-onset and “preventable” – meaning that there are widely accepted evidence-based prevention recommendations for these conditions. 19
Table 1.
Health conditions and genetic variants included in the Multiplex Genetic Susceptibility Test (MGST)
| Health Conditions | Gene Symbol |
Variant | |
|---|---|---|---|
| Cancer: | Melanoma | MC1R | RHC |
| Lung | MPO | −463G->A | |
| Colorectal | MTHFR | 677C->T | |
| Heart Disease: | Hypertension | AGT | M235T |
| Ischemic heart disease | APOB | Xba1 | |
| Coronary heart disease |
CETP | Taq1B | |
| HDL levels | LIPC | −514C->T | |
| Heart disease | NOS3 COL1A1 | E298D | |
| Osteoporosis: | Fracture | COL1A1 | Sp1 |
| Fracture | ESR1 | Xba1 | |
| Fracture | IL6 CAPN10 | −174G->C | |
| Type 2 Diabetes: | Type 2 diabetes | CAPN10 | SNP43 |
| Type 2 diabetes | KCNJ11 | E23K | |
| Type 2 diabetes | PPARG | P12A | |
| Type 2 diabetes | TCF7L2 | rs12255372 | |
Measures
The baseline questionnaire and the Web-based assessment of test decision (accessed on average about 6 weeks after completing the baseline survey) provide the prospective data for this report.
Dependent Variables
Information seeking was indicated by two variables: accessing the Web site (yes, no) and getting tested as indicated by completing a blood draw at the clinic (yes, no).
Independent Variables
Demographic characteristics included gender extracted from the HFHS enrollment database, self-identified race and education as reported on the baseline telephone survey. Beliefs about genetics as a cause of disease was based on a comparison of the individual’s beliefs about the extent to which each of the eight health conditions were genetic, that is, “passed from one generation to the nex” (1-not at all to 7-completely) versus the extent to which the health conditions were brought on by “health habits such as diet, exercise, and smoking” (1-not at all to 7-completely). A summary score across all health conditions was computed ranging from 0 to 1, where 0 represented a general tendency to attribute health conditions to genetics alone and 1 represented attributing health conditions to behavior alone. The extent to which it was perceived to be important to learn more about genetics was assessed on a scale from 1-not at all important to 7-very important.
Objective and subjective personal risk was characterized by seven variables: reported family history of six common health conditions (cancer, heart disease, osteoporosis, adult onset diabetes, high blood pressure, and high cholesterol; range 0 to 6). Self-reported height and weight was used to calculate Body Mass Index (BMI). Current smoking status was based on reporting ever having smoked and having smoked in the last 7 days. Number of health habits to change was assessed with an open-ended question in which the individual indicated specific health behaviors that they wanted to change (range 0-6). Perceived health status was indicated by self rating health as excellent, good, fair or poor. Perceived risk (i.e., perceived lifetime likelihood of each of the eight health conditions; 1-not at all likely to 7-completely likely), perceived severity of the condition (1-not at all serious to 7-very serious) and related worry (1-not at all worried to 7-very worried) were assessed individually for each of the eight health conditions. An average score was calculated across the eight health conditions for perceived risk, severity, and worry.
Self-rated competency in using the health care system and genetics included: general health confidence,20 that is, level of agreement (1-strongly disagree to 7-strongly agree) with three statements (e.g., “you are confident in your ability to understand most health-related information”, Cronbach’s alpha =0.71; and self-rated genetic competency21 based on a level of agreement (1-strongly disagree to 7-strongly agree) with six items (e.g., “you are confident in your ability to understand information about genetics”, Cronbach’s alpha=0.86).
General health information seeking and perceived norms was measured with four variables. Individuals self rated the frequency (4-daily, 3-weekly, 2-<weekly, 1-never) in the past 30 days of “having sought information about ways to stay healthy or feel better”. Access to the Internet was derived from combined responses to three questions: having ever gone online (yes, no), location of Internet usage (home, work, both) and having a personal email account (yes, no). Access ranged from level 1 (those who never went online) to level 4 (those who use the Internet at home with a personal email account). Norms regarding perceived importance of seeking health information (e.g., “the people who mean the most to you think you should learn more ways you can keep yourself healthy”) and norms regarding importance of staying healthy (e.g., “It’s important for you to take care of your health because of the people who mean the most to you”) were assessed. In each case, individuals rated their agreement (strongly disagree (1) to strongly agree (7)) with four statements (two for each domain).
Statistical Analyses
Means and proportions were computed to describe the distribution of independent variables. Bivariate associations of each of the independent variables with the two outcomes (logging on, getting tested) were tested for significance with chi-square and t-tests. Multivariate logistic regression models adjusting for race, education, and gender were tested that included all independent variables identified as significant in bivariate analyses at p<0.05 to predict each of the two outcome variables. Independent variables at p>0.20 were eliminated at each step using backward stepwise selection to arrive at a final model that “best” predicted each of the two outcome variables.
RESULTS
Recruitment
We attempted baseline surveys with 6,348 individuals; 1,292 declined to complete the survey, 2,614 were unreachable despite up to 10 repeated attempts, and 326 were deemed ineligible (e.g., reported having one of the health conditions). 1959 were eligible and completed the baseline survey. About a third of individuals who completed the survey were college graduates (37%) and white (37%); 46% were male, and 63% were married. Participants reported having a family health history on average for three (sd=1.5) of the MGST health conditions (See Table 2). The majority (82%) considered themselves to be in good health. A total of 612 individuals who completed the baseline survey visited the study’s Web site to consider testing; 528 registered a test decision. Of these, 266 provided written consent and had blood drawn for the MGST; 261 decided not to undergo testing.
Table 2.
Bivariate associations between psychosocial factors and information seeking outcomes
| Completed baseline survey |
Information seeking outcomes | ||||
|---|---|---|---|---|---|
| Logged on | Got tested | ||||
| N=1959 | No (n=1347) |
Yes (n=612) |
No (n=261) |
Yes (n=266) |
|
| Beliefs about genetics | |||||
| Mean perceived effects of genes and behavior on health conditions (0-entirely behavior – 1 entirely genetics) |
.42 (sd=.11) |
.42 (sd=.11) |
.42 (sd=.11) |
.41 (sd=.11) |
.42 (sd=.10) |
| Importance of learning about genes (scale 1-7) |
5.55 (sd=1.47) |
5.48 (sd=1.51) |
5.68** (sd=1.36) |
5.59 (sd=1.43) |
5.83* (sd=1.31) |
| Personal risk and related concern | |||||
| Mean conditions with family history (possible range: 0-6) |
3.12 (sd=1.5) |
3.07 (sd=1.51) |
3.22 (sd=1.49) |
3.10 (sd=1.55) |
3.36* (sd=1.48) |
| BMI > 30 | 35% | 36% | 33% | 36% | 30% |
| Current smoker | 28% | 29% | 28% | 28% | 30% |
| Perceive health to be excellent | 23% | 22% | 24% | 23% | 26% |
| Mean perceived risk for health conditions (scale 1-7) |
3.26 (sd=1.09) |
3.27 (sd=1.18) |
3.23 (sd=1.17) |
3.21 (sd=1.23) |
3.32 (sd=1.10) |
| Mean number of health habits to change (range 0-4) |
1.35 (sd=.88) |
1.34 (sd=.85) |
1.41 (sd=.85) |
1.28 (sd=.88) |
1.52** (sd=.89) |
| Mean perceived severity of health conditions (scale 1-7) |
6.11 (sd=.79) |
6.15 (sd=.79) |
6.02*** (sd=.80) |
6.13 (sd=.80) |
5.90** (sd=.78) |
| Mean worry about health conditions (scale 1-7) |
3.98 (sd=1.53) |
4.03 (sd=1.56) |
3.86* (sd=1.49) |
3.94 (sd=1.58) |
3.86 (sd=1.38) |
| Perceived competency in dealing with health system & genetics | |||||
| Confident to navigate health care system (scale 1-7) |
6.43 (sd=.73) |
6.40 (sd=.76) |
6.50** (sd=.65) |
6.48 (sd=.70) |
6.51 (sd=.62) |
| Confident can understand genetics (scale 1-7) |
5.69 (sd=1.06) |
5.67 (sd=1.06) |
5.75 (sd=1.05) |
5.66 (sd=1.13) |
5.84* (sd=.95) |
| General health information seeking and perceived norms | |||||
| Frequency of health information seeking (scale 1-4) |
2.30 (sd=.84) |
2.30 (sd=.84) |
2.30 (sd=.85) |
2.36 (sd=.87) |
2.28 (sd=.84) |
| Perceived norm: important to pursue ways to stay healthy (scale 1-7) |
4.61 (sd=1.86) |
4.69 (sd=1.85) |
4.44** (sd=1.88) |
4.51 (sd=1.90) |
4.30 (sd=1.90) |
| Perceived norm: important to stay healthy for others (scale 1-7) |
6.00 (sd=1.21) |
6.04 (sd=1.10) |
5.92* (sd=1.16) |
5.94 (sd=1.15) |
5.94 (sd=1.09) |
| Access to internet | 68% | 67% | 71%*** | 71% | 70% |
| Ever invited to participate in clinical research | 14% | 13% | 16%* | 13% | 20%* |
p<.05
p<.01
p<.001
Were Multiplex Information Seekers inclined to hold genetically deterministic explanations for common preventable health conditions?
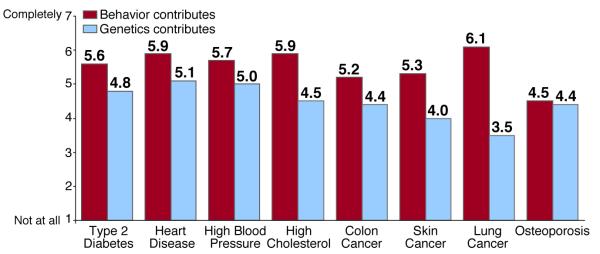
Figure 2 shows that at baseline participants generally rated behavior as a greater causal factor than genetics for seven of the eight health conditions on the MGST. Participants tended to believe that common health conditions could be attributed relatively equally to genes and behavior (X = 0.42, sd=0.11, 0 (behavior alone) to 1 (due to genes alone); Table 2); these attributions did not predict logging on or getting tested. Considering it to be important to learn about genetics predicted participants’ logging on, and getting tested (logging on: odds ratio, 1.21, 95% CI 1.12-1.31; getting tested: odds ratio 1.28, 95% CI 1.11-1.48; Tables 3 & 4).
Figure 2.
Table 3.
Final multivariate logistic regression model for psychological and behavioral predictors of logging on to consider multiplex genetic susceptibility testing after adjusting for race, education and gender
| Predictors | Odds ratio | 95% Confidence Interval |
|---|---|---|
| Worry about health conditions | 0.93 | 0.87 - 1.00 |
| Perceived severity of health conditions | 0.89 | 0.78 - 1.03 |
| Perceived importance to stay healthy for others |
0.92 | 0.84 - 1.00 |
| Confidence can understand genetics | 1.15 | 0.99 - 1.34 |
| Importance of learning about genetics | 1.21 | 1.12 - 1.31 |
| Access to the Internet | 1.26 | 1.11 - 1.44 |
Table 4.
Final multivariate logistic regression model for psychological and behavioral predictors of getting tested after adjusting for race and education
| Predictors | Odds ratio | 95% Confidence Interval |
|---|---|---|
| Perceived severity of health conditions |
0.73 | 0.57 - 0.95 |
| Confidence can understand genetics | 1.26 | 1.05 - 1.51 |
| Importance of learning about genetics | 1.28 | 1.11 - 1.48 |
| Number of health habits to change | 1.39 | 1.13 - 1.72 |
| Ever invited to participate in research | 1.40 | 0.86 - 2.30 |
Were Multiplex Information Seekers inclined to be “risk perceivers”, that is, report high objective and subjective risk for the health conditions?
The 1959 who completed the baseline survey considered the health conditions on the test to be quite severe (X=6.11 on a 7 point scale) and believed that they had at least one related risk factor in need of change. However, participants perceived themselves to be at relatively modest risk for the health conditions (X = 3.26 on a 7 point scale) and were not particularly worried about getting the health conditions (X = 3.98 on a 7 point scale). In multivariate analyses, none of the risk variables remained significant predictors of logging on (Table 3). However, perceiving the health conditions to be severe reduced the likelihood of getting tested (odds ratio=.73, 95% CI .57-.95). In contrast, perceiving one’s self to have more health habits to change increased the likelihood of getting tested (odds ratio = 1.39, 95% CI 1.13-1.72; Table 4).
Were Multiplex Information Seekers inclined to be “skilled information consumers”, that is, report greater competence with the health care system and genetics?
Participants reported high levels of confidence in their ability to navigate the health care system (X = 6.43 on a 7 point scale) and to understand genetics (X = 5.69 on a 7 point scale). Neither area of confidence was a predictor of logging on in multivariate analyses, but confidence to understand genetics was a significant predictor of getting tested (odds ratio=1.26, 95% CI 1.05-1.51; Table 4) whereas health system confidence was not. For each unit of increase in confidence to understand genetics, the likelihood of getting tested increased accordingly.
Were Multiplex Information Seekers inclined to be “health information monitors” that is, especially interested in health information?
Fully two-thirds of the participants had high levels of access to the Internet. Having more Internet access was a significant predictor of logging on in multivariate analyses (odds ratio=1.26, 95% CI 1.11-1.44), but was not associated with getting tested. General health information seeking also was not associated with either logging on or getting tested.
DISCUSSION
Only one-third of those offered state-of-the-science free genetic testing logged on to a study Web site to review information about the pros and cons of being tested. Of those who viewed the information pages on the Web site, half considered the pros and cons of free testing, and decided not to be tested. Our results suggest that when provided with balanced information, consumers recognize the limitations and utility of receiving personal genetic profiles; half decided against testing. However, up to half may regard such information to be useful even with its limitations.
We found no evidence that those who considered or sought testing were inclined to overestimate the contributions of genetics to common health conditions or to underestimate behavioral risk factors. On the contrary, those opting for testing held the same balanced view of the genetic contribution to disease as those who chose not to be tested. However, those who felt it to be most important to learn about genetics and felt confident in their ability to understand test results were clearly overrepresented among the genetic information seekers.
Frequent internet users and those who considered it to be most important to learn about genetics were most inclined to seek testing. Being active seekers of general health information was not an important predictor. Thus genetics may hold special allure and generate new groups of health information seekers. It is important to note that disparities in access and use of online health information mean that some subgroups remain underserved.15 Thus, those presenting to primary care providers will likely be the most Internet savvy and may well have sought a variety of other online health information.
Perceiving one’s self to have health habits in need of change was a positive predictor of getting tested. Fully a third of those participating in the study were obese or current cigarette smokers, suggesting that reporting health habits to change might be a surrogate indicator of desire to decrease risk. Individuals may see genetic susceptibility testing as a step in the direction of getting healthy. Indeed, previous studies of genetic testing for susceptibility to lung cancer that have targeted cigarette smokers have reported that those who sought testing were the most motivated to quit smoking. 22,23
Patients presenting to caregivers with personalized genome scans appreciate that both genes and environment influence common disease risk. While the current, but limited, evidence suggests that receiving genetic information by itself is ineffective in producing behavior change, 24 by being “net friendly” (i.e., avoiding a dismissive attitude towards genetic information) and providing positive reinforcement of patients’ demonstrated health consciousness, physicians might be able to effectively partner with patients for health promotion. 16 In particular, attempts to understand the reasons patients give for seeking genetic health information could enable physicians to make linkages between personalized genomic tests and clinically validated risk assessments like family history. Indeed others 25 have shown that when genetic testing is combined with family history information, patients may be more influenced by family history information than genetic results.
To our knowledge, this is the first population-based (i.e., with a known denominator) study to prospectively evaluate the effects of offering MGST to a large and demographically heterogeneous population of healthy adults. Despite this considerable strength, there are some limitations. Given the large sample size, many of the relatively small associations between psychosocial factors and primary outcomes were statistically significant, but may not be clinically meaningful. To reduce the burden of research participation and increase the external validity of our findings, many of our psychosocial measures were extracted from larger validated scales in ways that may have diminished the rigor of the measures. Offering MGST at no charge to those with health insurance is not likely to represent how such testing ultimately will be disseminated. Thus, these findings in many ways represent a “best case” scenario. Evaluating different coverage scenarios, such as with and without co-pays has been shown previously to influence how patients use services26 and also could greatly influence which patients avail themselves of genetic testing.
In closing, physicians are increasingly seeing the Internet-informed health consumer. This information can unnecessarily triangulate interactions with patients if providers lack understanding of factors that motivate patients to seek such information. Genomic profiles present yet a new incarnation of this growing trend that like other health information might be leveraged to promote patient well-being if directed appropriately.
References
- 1.Go VL, Wong DA, Wang Y, Butrum RR, Norman HA, Wilkerson L. Diet and cancer prevention: evidence-based medicine to genomic medicine. J Nutr. Dec 2004;134(12 Suppl):3513S–3516S. doi: 10.1093/jn/134.12.3513S. [DOI] [PubMed] [Google Scholar]
- 2.Bell J. Predicting disease using genomics. Nature. 2004 May 27;429(6990):453–456. doi: 10.1038/nature02624. [DOI] [PubMed] [Google Scholar]
- 3.Katsanis SH, Javitt G, Hudson K. Public health. A case study of personalized medicine. Science. 2008 Apr 4;320(5872):53–54. doi: 10.1126/science.1156604. [DOI] [PubMed] [Google Scholar]
- 4.Hunter DJ, Khoury MJ, Drazen JM. Letting the genome out of the bottle--will we get our wish? N Engl J Med. 2008 Jan 10;358(2):105–107. doi: 10.1056/NEJMp0708162. [DOI] [PubMed] [Google Scholar]
- 5.Haga SB, Khoury MJ, Burke W. Genomic profiling to promote a healthy lifestyle: not ready for prime time. Nat Genet. 2003 Aug;34(4):347–350. doi: 10.1038/ng0803-347. [DOI] [PubMed] [Google Scholar]
- 6.Lunshof JE, Pirmohamed M, Gurwitz D. Personalized medicine: decades away? Pharmacogenomics. 2006 Mar;7(2):237–241. doi: 10.2217/14622416.7.2.237. [DOI] [PubMed] [Google Scholar]
- 7.Feero WG, Guttmacher AE, Collins FS. The genome gets personal--almost. JAMA. 2008 Mar 19;299(11):1351–1352. doi: 10.1001/jama.299.11.1351. [DOI] [PubMed] [Google Scholar]
- 8.Roberts JS, Cupples LA, Relkin NR, Whitehouse PJ, Green RC. Genetic risk assessment for adult children of people with Alzheimer’s disease: the Risk Evaluation and Education for Alzheimer’s Disease (REVEAL) study. J Geriatr Psychiatry Neurol. 2005 Dec;18(4):250–255. doi: 10.1177/0891988705281883. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005 Apr 13;293(14):1729–1736. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- 10.Henrikson NB, Harris JN, Bowen DJ. Predictors of self-referral into a cancer genetics registry. Cancer Epidemiol Biomarkers Prev. 2007 Jul;16(7):1387–1392. doi: 10.1158/1055-9965.EPI-06-0009. [DOI] [PubMed] [Google Scholar]
- 11.Lipkus IM, Iden D, Terrenoire J, Feaganes JR. Relationships among breast cancer concern, risk perceptions, and interest in genetic testing for breast cancer susceptibility among African-American women with and without a family history of breast cancer. Cancer Epidemiol Biomarkers Prev. 1999 Jun;8(6):533–539. [PubMed] [Google Scholar]
- 12.Lohmueller KE, Pearce CL, Pike M, Lander ES, Hirschhorn JN. Meta-analysis of genetic association studies supports a contribution of common variants to susceptibility to common disease. Nat Genet. 2003 Feb;33(2):177–182. doi: 10.1038/ng1071. [DOI] [PubMed] [Google Scholar]
- 13.Bernhardt JM, McClain J, Parrott RL. Online health communication about human genetics: perceptions and preferences of internet users. Cyberpsychol Behav. 2004 Dec;7(6):728–733. doi: 10.1089/cpb.2004.7.728. [DOI] [PubMed] [Google Scholar]
- 14.Green MJ, McInerney AM, Biesecker BB, Fost N. Education about genetic testing for breast cancer susceptibility: patient preferences for a computer program or genetic counselor. Am J Med Genet. 2001 Sep 15;103(1):24–31. doi: 10.1002/ajmg.1501. [DOI] [PubMed] [Google Scholar]
- 15.Lorence D, Park H. Group disparities and health information: a study of online access for the underserved. Health Informatics J. 2008 Mar;14(1):29–38. doi: 10.1177/1460458207086332. [DOI] [PubMed] [Google Scholar]
- 16.Wald HS, Dube CE, Anthony DC. Untangling the Web--the impact of Internet use on health care and the physician-patient relationship. Patient Educ Couns. 2007 Nov;68(3):218–224. doi: 10.1016/j.pec.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 17.McGuire AL, Burke W. An unwelcome side effect of direct-to-consumer personal genome testing: raiding the medical commons. JAMA. 2008 Dec 10;300(22):2669–2671. doi: 10.1001/jama.2008.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffin RJ, Dunwoody S, Neuwirth K. Proposed model of the relationship of risk information seeking and processing to the development of preventive behaviors. Environ Res. 1999 Feb;80(2 Pt 2):S230–S245. doi: 10.1006/enrs.1998.3940. [DOI] [PubMed] [Google Scholar]
- 19.Emmons K, Smedley B, Syme S. Institute of Medicine. Promoting Health: Intervention Strategies from Social and Behavioral Research. National Academy Press; Washington, DC: 2000. Behavioral and social science contributions to the health of adults in the United States. [Google Scholar]
- 20.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008 May;23(5):561–566. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parrott RL, Silk KJ, Condit C. Diversity in lay perceptions of the sources of human traits: genes, environments, and personal behaviors. Soc Sci Med. 2003 Mar;56(5):1099–1109. doi: 10.1016/s0277-9536(02)00106-5. [DOI] [PubMed] [Google Scholar]
- 22.McBride CM, Bepler G, Lipkus IM, et al. Incorporating genetic susceptibility feedback into a smoking cessation program for African-American smokers with low income. Cancer Epidemiol Biomarkers Prev. 2002 Jun;11(6):521–528. [PubMed] [Google Scholar]
- 23.O’Neill SC, White DB, Sanderson SC, et al. The feasibility of online genetic testing for lung cancer susceptibility: uptake of a web-based protocol and decision outcomes. Genet Med. 2008 Feb;10(2):121–130. doi: 10.1097/GIM.0b013e31815f8e06. [DOI] [PubMed] [Google Scholar]
- 24.Carlsten C, Burke W. Potential for genetics to promote public health: genetics research on smoking suggests caution about expectations. JAMA. 2006 Nov 22;296(20):2480–2482. doi: 10.1001/jama.296.20.2480. [DOI] [PubMed] [Google Scholar]
- 25.Tarini BA, Singer D, Clark SJ, Davis MM. Parents’ concern about their own and their children’s genetic disease risk: potential effects of family history vs genetic test results. Arch Pediatr Adolesc Med. 2008 Nov;162(11):1079–1083. doi: 10.1001/archpedi.162.11.1079. [DOI] [PubMed] [Google Scholar]
- 26.Curry SJ, Grothaus LC, McAfee T, Pabiniak C. Use and cost effectiveness of smoking-cessation services under four insurance plans in a health maintenance organization. N Engl J Med. 1998 Sep 3;339(10):673–679. doi: 10.1056/NEJM199809033391006. [DOI] [PubMed] [Google Scholar]