Abstract
Problem
The Brazilian population lacks equitable access to specialized health care and diagnostic tests, especially in remote municipalities, where health professionals often feel isolated and staff turnover is high. Telehealth has the potential to improve patients’ access to specialized health care, but little is known about it in terms of cost-effectiveness, access to services or user satisfaction.
Approach
In 2005, the State Government of Minas Gerais, Brazil, funded the establishment of the Telehealth Network, intended to connect university hospitals with the state’s remote municipal health departments; support professionals in providing tele-assistance; and perform tele-electrocardiography and teleconsultations. The network uses low-cost equipment and has employed various strategies to overcome the barriers to telehealth use.
Local setting
The Telehealth Network connects specialists in state university hospitals with primary health-care professionals in 608 municipalities of the large state of Minas Gerais, many of them in remote areas.
Relevant changes
From June 2006 to October 2011, 782 773 electrocardiograms and 30 883 teleconsultations were performed through the network, and 6000 health professionals were trained in its use. Most of these professionals (97%) were satisfied with the system, which was cost-effective, economically viable and averted 81% of potential case referrals to distant centres.
Lessons learnt
To succeed, a telehealth service must be part of a collaborative network, meet the real needs of local health professionals, use simple technology and have at least some face-to-face components. If applied to health problems for which care is in high demand, this type of service can be economically viable and can help to improve patient access to specialized health care.
Résumé
Problème
La population brésilienne manque d'un accès équitable aux soins de santé spécialisés et aux tests de diagnostic, surtout dans les communes reculées, où les professionnels de santé se sentent souvent isolés et où la rotation du personnel est élevée. La télésanté peut améliorer l'accès des patients aux soins de santé spécialisés, mais on sait peu de choses de son rapport coût-efficacité, de l'accès aux services ou de la satisfaction des utilisateurs.
Approche
En 2005, le gouvernement de l'État de Minas Gerais, au Brésil, a financé la création d'un réseau de télésanté, visant à relier les hôpitaux universitaires aux services de santé municipaux reculés de l'État, à soutenir les professionnels dans la téléassistance et à effectuer des télé-électrocardiographies et téléconsultations. Le réseau utilise un équipement à faible coût et a recouru à diverses stratégies pour surmonter les obstacles relatifs à l'utilisation de la télésanté.
Environnement local
Le réseau de télésanté relie les spécialistes des hôpitaux universitaires de l'État aux professionnels des services de santé primaires de 608 communes du grand État de Minas Gerais, beaucoup d'entre eux se trouvant dans des zones reculées.
Changements significatifs
De juin 2006 à octobre 2011, 782 773 électrocardiogrammes et 30 883 téléconsultations ont été effectués par l'intermédiaire du réseau, et 6 000 professionnels de santé ont été formés à son utilisation. La plupart de ces professionnels (97%) se sont montrés satisfaits du système qui offrait un bon rapport coût-efficacité, était économiquement viable et évitait 81% des renvois potentiels de cas vers des centres éloignés.
Leçons tirées
Pour être un succès, un service de télésanté doit faire partie d'un réseau collaboratif, satisfaire les besoins réels des professionnels de santé locaux, utiliser une technologie simple et disposer d'au moins quelques éléments en face à face. En cas d'application à des problèmes sanitaires pour lesquels la demande de soins est élevée, ce type de service peut être économiquement viable et aider à améliorer l'accès des patients aux soins de santé spécialisés.
Resumen
Situación
La falta de igualdad en el acceso de la población brasileña a la asistencia sanitaria especializada y a las pruebas diagnósticas, en especial, en municipios remotos, en los que los profesionales sanitarios suelen sentirse aislados y la rotación de personal es alta. La telesalud tiene el potencial de mejorar el acceso de los pacientes a la asistencia sanitaria especializada, pero se dispone de poca información en cuanto a la eficacia en relación a los costes, al acceso a los servicios o a la satisfacción del usuario.
Enfoque
En el año 2005, el gobierno del estado de Minas Gerais, Brasil, financió el establecimiento de la Red de telesalud con la intención de conectar los hospitales universitarios con los departamentos sanitarios de municipios remotos del estado, así como para ayudar a los profesionales a que pudieran proporcionar asistencia y realizar electrocardiografías y consultas a distancia. La red utiliza equipos de bajo coste y ha empleado varias estrategias para superar las barreras del uso de la telesalud.
Marco regional
La red de telesalud conecta a los especialistas de los hospitales universitarios estatales con los profesionales de asistencia sanitaria primaria en 608 municipios del extenso estado de Minas Gerais, muchos de ellos en áreas remotas.
Cambios importantes
Desde junio de 2006 hasta octubre de 2011, se realizaron 782 773 electrocardiogramas y 30.883 consultas a distancia a través de la red y se formó a 6.000 profesionales sanitarios en su uso. La mayor parte de estos profesionales (97%) estaban satisfechos con el sistema, que ofrece una buena eficacia en relación a los costes, es económicamente viable y evitó el 81% de las referencias de casos potenciales a centros distantes.
Lecciones aprendidas
Para conseguir resultados, un servicio de telesalud debe formar parte de una red colaborativa, cubrir las necesidades reales de los profesionales sanitarios locales, utilizar tecnologías simples y tener al menos algunos componentes cara a cara. Si se aplica a los problemas sanitarios para los que existe una alta demanda de asistencia, este tipo de servicio puede ser económicamente viable y ayudar a mejorar el acceso del paciente a la asistencia sanitaria especializada.
ملخص
المشكلة
يفتقر السكان البرازيليون إلى الوصول بشكل متساو إلى الرعاية الصحية المتخصصة والاختبارات التشخيصية وخاصة في البلديات النائية، حيث يشعر الأخصائيون الصحيون في الغالب بالعزلة وترتفع معدلات دوران العاملين. وتتضمن الخدمات الصحية عن بعد إمكانية تحسين وصول المرضى إلى الرعاية الصحية المتخصصة، غير أنه لا يُعرف سوى القليل عنها فيما يتعلق بفعالية التكلفة أو الوصول إلى الخدمات أو رضى المستخدمين.
الأسلوب
في 2005، قامت حكومة ولاية ميناس جيرايس في البرازيل بتمويل تأسيس شبكة الخدمات الصحية عن بعد بهدف ربط المستشفيات الجامعية بإدارات الصحة البلدية النائية التابعة للولاية ودعم الأخصائيين في تقديم المساعدة عن بعد وإجراء تخطيط القلب الكهربائي والاستشارات عن بعد. وتستخدم الشبكة معدات منخفضة التكلفة وتوظف عددًا من الاستراتيجيات للتغلب على العوائق التي تحول دون استخدام الخدمات الصحية عن بعد.
المواقع المحلية
تربط شبكة الخدمات الصحية عن بعد الأخصائيين في المستشفيات الجامعية بأخصائيي الرعاية الصحية الأولية في 608 بلدية تتبع ولاية ميناس جيرايس الكبيرة، التي يقع العديد من بلدياتها في مناطق نائية.
التغيّرات ذات الصلة
من يونيو 2006 إلى أكتوبر 2011، تم إجراء 782773 مخطط قلب كهربائي و30883 استشارة عن بعد من خلال الشبكة وتم تدريب 6000 أخصائي صحي على استخدامها. وأعرب معظم هؤلاء الأخصائيين (97 %) عن رضاهم عن النظام الذي ثبتت فعالية تكلفته وملائمته من الناحية الاقتصادية، وتلافوا تحويل 81 % من الحالات المحتملة إلى المراكز البعيدة.
الدروس المستفادة
لكي تنجح الخدمة الصحية عن بعد، يتعين أن تكون جزءًا من شبكة تعاونية وأن تلبي الاحتياجات الفعلية للأخصائيين الصحيين المحليين، وأن تستخدم تكنولوجيا بسيطة وأن تشتمل على الأقل على بعض مكونات المقابلة وجهًا لوجه. ومن الممكن أن يكون هذا النوع من الخدمات - في حالة تطبيقه على المشكلات الصحية التي يزداد الطلب فيها على الرعاية - ملائمًا من الناحية الاقتصادية ومن الممكن أن يساعد في تحسين وصول المرضى إلى الرعاية الصحية المتخصصة.
摘要
问题
巴西人口缺乏公平获取专业医疗保健和诊断试验的条件,尤其是在偏远的城市,那里的卫生专业人员经常感到孤立,员工流失率很高。远程医疗有可能改善患者使用专业医疗保健服务的状况,但在成本效益、使用服务或用户满意度方面的情况却知之甚少。
方法
2005 年,巴西米纳斯吉拉斯州政府资助建立远程医疗网络,旨在将大学医院与本国的偏远城市卫生部门连接起来,支持专业人员提供远程协助并执行远程心电图描记和远程会诊。该网络采用低成本的设备并使用各种策略来克服远程医疗使用的障碍。
当地状况
远程医疗网络将州立大学医院的专家和在米纳斯吉拉斯大州的 608 个自治市(多是在偏远地区)的初级卫生保健专业人员连接起来。
相关变化
从 2006 年 6 月至 2011 年 10 月,通过网络执行了 782773 次心电图和 30883 次远程会诊,6000 名卫生专业人员接受有关其使用的培训。这些专业人士绝大多数(97%)都对该系统感到满意,该系统符合成本效益,经济上可行,并避免了 81% 潜在病例转介到遥远的中心。
经验教训
要取得成功,远程医疗服务就必须是协作网络的组成部分,满足当地卫生专业人员的实际需要,使用简单的技术,且至少有一些面对面的组件。如果应用于高需求医疗保健问题,这种类型的服务在经济上可行,有助于改善病人获得专业医疗保健服务的状况。
Резюме
Проблема
Население Бразилии испытывает недостаток гарантированного доступа к специализированному медицинскому обслуживанию и диагностическим тестам, особенно в удаленных муниципалитетах, где высока текучесть кадров, а медицинские работники чувствуют себя изолированными. Потенциалом для улучшения доступа пациентов к специализированному медицинскому обслуживанию обладает телемедицина, однако о ее экономической эффективности, доступности ее услуг и удовлетворенности ими пользователей известно немного.
Подход
В 2005 г. правительство штата Минас-Жерайс, Бразилия, профинансировало создание Телемедицинской сети, предназначенной для организации обмена информацией между университетскими клиниками и удаленными государственными муниципальными отделами здравоохранения, оказания поддержки специалистам в предоставлении дистанционной помощи, а также для выполнения дистанционной электрокардиографии и проведения телеконсультаций. Сеть использует доступное оборудование и в ней были применены различные стратегии для преодоления барьеров в использовании телемедицины.
Местные условия
Телемедицинская сеть позволяет обмениваться информацией специалистам университетских клиник страны с работниками первичной медицинской помощи в 608 городах крупного штата Минас-Жерайс, многие из которых находятся в отдаленных районах.
Осуществленные перемены
С июня 2006 г. по октябрь 2011 г. С помощью сети было выполнено 782773 электрокардиограммы и проведено 30883 телеконсультации, 6000 медицинских работников прошли обучение по использованию сети. Большинство этих работников (97%) остались довольны системой, которая показала себя рентабельной, экономически жизнеспособной и предотвратила направление пациентов в удаленные медицинские центры в 81% требующих этого случаев.
Выводы
Чтобы успешно выполнять свои функции, телемедицинская служба должна быть частью объединенной сети, удовлетворять реальные потребности медицинских работников на местах, использовать простые технологии и иметь хотя бы несколько компонентов для личного общения. Применительно к заболеваниям, для которых широко востребована медицинская помощь, подобная служба может быть экономически жизнеспособной и способна помочь в улучшении доступа пациента к специализированному медицинскому обслуживанию.
Introduction
Brazil is a vast country of marked cultural, economic, geographic and infrastructural contrasts. It is composed of 27 federative units: 26 states and one federal district that contains the capital, Brasilia. Although the Brazilian Constitution guarantees universal and equitable access to high-quality health care, these contrasts make such access difficult to provide. Primary care is central to Brazil’s public health system, which aims to provide comprehensive health care, specialized services and hospital care, as well as health promotion and disease prevention activities.1 Minas Gerais, a large state, has 19 million inhabitants unevenly distributed among 853 municipalities and is characterized by inequities in health care.2
Problem
Residents of small and remote municipalities have difficulty accessing specialized care because health resources are concentrated in the largest cities. Health professionals in remote areas tend to be young and inexperienced and are often isolated and in need of further training. The resulting high turnover rates in the primary care workforce compromise service quality. This, plus the small amount invested in linking primary care with other levels of care and the failure to provide good access to diagnostic tests, prevents the Brazilian primary health-care model from fully meeting its objectives.1
Telehealth, or the use of information technologies in the health professions to provide care, impart education or conduct research, has the potential to reduce existing health-care inequities by supporting primary care professionals in remote areas.2–4 Telehealth offers an effective means of improving communication between primary care practitioners and specialists in reference centres, facilitating access to diagnostic tests and enhancing health care quality in under-served communities.2,5 However, little information is available with respect to cost-effectiveness, access to services, process of care and user satisfaction in connection with telehealth.5
Approach
Programme development
In 2005, the State Government of Minas Gerais, Brazil, funded the establishment of the Telehealth Network, designed to connect the teaching hospitals of five public universities with municipal health departments.6 The health department of the state initially implemented the programme as a research project in 82 municipalities with fewer than 10 500 inhabitants. Because cardiovascular diseases are the leading cause of death in Minas Gerais and remote areas have a serious shortage of cardiologists, the state health department decided to focus the project on telecardiology [Minas Telecardio Project],6 specifically on tele-electrocardiography (i.e. the use of the internet to send electrocardiograms [EKGs] from remote areas to university hospitals for interpretation). The project proved feasible and financially sound6–8 and satisfaction among physicians working in remote locations increased markedly.9,10
After 2007, the Telehealth Network of Minas Gerais began providing teleconsultations also. In other words, primary-care professionals began using the network’s web site to address questions to university staff in areas such as medicine, nursing, dentistry, physiotherapy, nutrition, pharmacy, psychology and audiology. Primary-care professionals can thus perform their clinical activities with the support of a network of specialists on duty in the universities. The specialist who first answers the teleconsultation can seek the help of a subspecialist if s/he considers it necessary. This service is viewed as an ongoing educational tool, since every teleconsultation represents a learning experience. The network was progressively expanded and had reached 608 municipalities by August 2010.
The Telehealth Network relies on low-cost technical equipment easily accessible to poor villages: computers, printers, digital electrocardiographs, digital cameras (e.g. for photographing skin lesions), webcams and low-band-width internet. All teleconsultations take place among health-care professionals, since Brazil’s Board of Physicians [Conselho Federal de Medicina] does not authorize teleconsultations between physicians and patients.
A methodology for implementing and maintaining the network was developed. Staff visited all cities in the network and regional meetings with municipal health-care practitioners were held periodically in the municipalities or university hospitals to discuss the benefits of telehealth, the barriers to its implementation (e.g. lack of political support, poor user acceptance, or health-care practitioners’ lack of familiarity with teleconsultation and tele-electrocardiography) and ways to overcome them (e.g. community involvement, training of health-care practitioners in the use of teleconsultation and tele-electrocardiography, and adaptation of local work routines to accommodate use of the telehealth system). These meetings were also attended by the Telehealth Network’s clinical staff, whose members gave lectures on topics chosen in accordance with the questions most frequently asked during teleconsultations. The meetings provided an opportunity for users and clinical staff to develop a comfortable relationship with one another.
To ensure the quality of decentralized clinical services, a quality control office was established and charged with implementing standard protocols, providing an auditing system and promoting clinical research. Auditing consisted of assessing agreement between different cardiologists’ EKG readings. In January 2011, a sample of 905 EKGs was randomly and blindly selected, and every EKG was read by a second network cardiologist, also randomly selected. This cardiologist was not told that the EKG s/he was reading had already been interpreted. Subsequently, a senior cardiologist from Minas Gerais’ teaching hospital [Hospital das Clínicas da Universidade Federal de Minas Gerais] with strong expertise in reading EKGs assessed agreement between the two previous examiners and his readings provided the “gold standard”.
User satisfaction was constantly monitored by the system by means of the following questions, which were sent to users after they received the response to their teleconsultation: (i) “Did the teleconsultation avoid the patient’s referral?” (ii) “Did the teleconsultation answer your question?” (iii) “What is your level of satisfaction with the teleconsultation system?” The first question explores activity efficiency, defined as the number of patient referrals avoided divided by the total number of telehealth activities. The second question gauges the response given by the specialist to the teleconsultations. The third question assesses users’ general satisfaction with the system. From January to October 2011, 13 828 teleconsultations were performed and 1284 users responded to the survey.
Cost-effective analyses were conducted and the following economic indicators were developed: implementation cost per site, unitary activity cost (i.e. cost per activity) and patient referral cost (i.e. cost per referral). Implementation costs were broken down into travel and equipment. The unitary activity cost (Ca) was the total operational cost of the system divided by the number of activities. The patient referral cost (Cr ) comprised fixed costs (infrastructural maintenance) and variable costs. Data on the first two indicators were collected from the network management system. Patient referral costs were investigated during visits conducted from August 2009 to August 2011at 86 municipalities within the Telehealth Network. Since telehealth cannot eliminate all referrals and since expenditure is affected, in turn, by activity efficiency (Ea), the savings to the health system (S) can be calculated as follows:
| (1) |
where Na is the number of activities. All costs were converted to United States dollars (US$) (at the August 2011 exchange rate of 1.80 Brazilian reais per US$).
Results
The network covers around 9 265 820 inhabitants of Minas Gerais, or 47.2% of the population of the state. From June 2006 to December 2011, 825 349 EKGs and 33 042 teleconsultations were performed. This is equivalent to a daily average of 1450 remote EKGs and 77 teleconsultations (Fig. 1) and to an annual average of 540 EKGs and 30 teleconsultations per municipality. The Telehealth Network has now become an essential component of the health-care system in those municipalities.
Fig. 1.
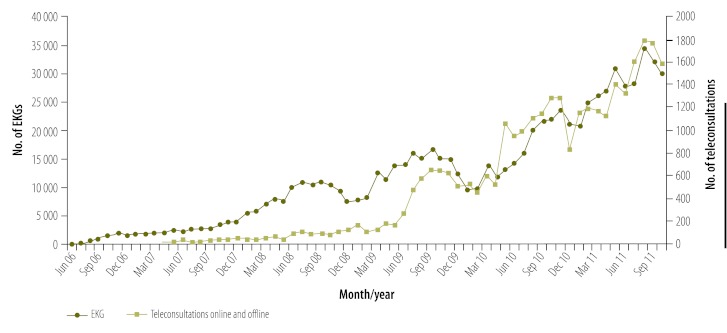
Electrocardiograms (EKGs) and teleconsultations conducted through the Telehealth Network of Minas Gerais, Brazil, June 2006–October 2011
The majority of teleconsultations were performed offline, and the specialties most in demand were internal medicine, dermatology and nursing. The most frequent types of questions pertained to pharmacological treatment and disease aetiology. Approximately 6000 health professionals have been trained through the Telehealth Network. Presently, the service engages 42 technical and administrative staff, 36 health professionals on duty and 43 specialists, including physicians and other health-care professionals.
Auditing showed a 9.4% rate of disagreement with respect to EKG abnormalities that were substantial enough to potentially alter case management. Discordant opinions were discussed between the clinical coordinator and the cardiologists to establish protocols based on standard guidelines for EKG analysis and a structured format for reporting.
The satisfaction survey showed that 80.8% of the teleconsultations had averted a referral (i.e. 80.8% activity efficiency), 97.3% of the surveyed users felt that the teleconsultation had replied to their question, and 97.1% were satisfied with the network.
The economic analysis showed that travel costs were reduced from an average of US$ 2240 per site in the programme’s 82 original municipalities to US$ 305 per site in the 328 municipalities that joined the network in 2009–2010. Equipment costs remained approximately constant at US$ 2500 per site, on average, during all phases of network expansion. The average cost per patient referral was US$ 63.60 (US$ 23.42 fixed cost and US$ 40.18 variable cost), whereas the average telehealth activity cost amounted to US$ 6.03. For a total of 759 656 activities, an activity efficiency of 80.8% and a variable referral cost of US$ 40.18 per referral, the telehealth system generated a saving for the public health system of US$ 20 081 840 between June 2006 and October 2011. An investment of US$ 9 000 000 was required to obtain this benefit. Hence, the cost–benefit ratio was 2.24 to 1.
Discussion
In this paper we have described the development of a large, public, state-wide telehealth system that supports primary care professionals in remote regions of the Brazilian state of Minas Gerais as part of a government strategy to fulfil the constitutional premise of universal access to high-quality health care. Combining assistance and in-service education with simple and inexpensive technology, the telehealth model has been shown to be effective, technically feasible and economically viable. To the best of our knowledge, this telehealth project is one of the most successful to have been described in the scientific literature until now.
The valuable lessons learnt in the course of conducting our study are listed in Box 1. In Box 2 we offer recommendations for implementing a successful telehealth programme based on our experience with the Telehealth Network of Minas Gerais, although some are contained in other guidelines.15 Initially network implementation and maintenance were difficult; the Internet connection was poor at the beginning of the project and health-care practitioners had to be trained continually because of the high turnover in the workforce in remote municipalities. Furthermore, in the Brazilian public health system, telehealth activities are not reimbursable. Hence, the programme’s funding is always dependent on specific health department budgets. A stable source of funding will be essential for the sustainability of the telehealth programme.
Box 1. Summary of main lessons learnt.
Telehealth requires a collaborative network of educational and research institutions, government, technology providers and funders to achieve its full potential.
To be successful, a telehealth service must meet the real needs of local health professionals, use simple and low-cost technology and have some face-to-face components (e.g. personal visits to the municipalities, workshops and training sessions).
Telehealth must use technology as a means for delivering health-care benefits; to be economically beneficial, it must be applied to address problems for which there is a high service demand.
Box 2. Recommendations for implementing a successful telehealth programme based on experience with the Telehealth Network of Minas Gerais.
Collaborative network
Telehealth is an innovative tool, but many aspects – technologies, processes and methodologies – have yet to be developed fully. To enable telehealth to reach its full potential, all new knowledge and technologies developed in educational contexts and research institutions must be shared with technology providers within a government strategy that embraces telehealth.
Real needs
Telehealth activities must meet the real needs of all users (health managers and professionals as well as patients).2–4,11,12 Because it is a new technology, telehealth faces the barrier of user resistance to a new work process.
Telehealth users have a natural tendency to resist altering their work routine unless doing so clearly leads to improved solutions to frequently encountered problems.13,14
Simple, low-cost technology
Technology is a tool intended to improve health care, but it is not telehealth’s foremost objective. The technology used must be simple, inexpensive and appropriate for its users and the local infrastructure.2
Virtual and personal process
Although telehealth is essentially a virtual process, it has a human component. The establishment of a strong relationship between users and providers is one of the most important determinants of system acceptance and utilization. Users and providers should know each other personally, and it is important to promote different opportunities to hold face-to-face meetings (site visits, workshops, training sessions, etc.).2
Economic viability
To be economically viable and compensate for high fixed costs, a telehealth programme must be used relatively frequently. Hence, telehealth is most beneficial in fields for which there is a high demand. The cost-benefit ratio also depends on the degree to which the telehealth service can avert other major costs, such as referrals to distant centres, specialized consultations and expensive tests.7 Moreover, the choice of low-cost, commercially available equipment can reduce implementation costs.
This report has limitations. Although we have demonstrated that primary care physicians look favourably upon the Telehealth Network, we did not evaluate whether the programme reduced the high turnover rate among these professionals. Moreover, we did not evaluate the impact of the telehealth programme on the health status of the population and are therefore unable to say whether the programme has prolonged patients’ lives or improved their health.5 Both of these questions require future study.
Conclusion
A telehealth programme developed to support primary care professionals in Minas Gerais, Brazil, has produced good results overall at relatively little cost. Initially conceived as a research project, it developed into a state-wide public health strategy covering hundreds of municipalities and thousands of patients. The project’s simplicity and interoperability and the international standards adopted for implementing the fully-developed model should make for easy replication in other parts of the world. Furthermore, the lessons learnt during this experience will help programmes of a similar nature elsewhere achieve good results.
Funding:
The Telehealth Network of Minas Gerais was funded by the State Government of Minas Gerais, by its Health Department [Secretaria de Estado da Saúde de Minas Gerais] and its research agency FAPEMIG [Fundação de Amparo à Pesquisa de Minas Gerais], and by the Brazilian Government, including the Health Ministry and the Science and Technology Ministry and its research and innovation agencies, CNPq [Conselho Nacional de Desenvolvimento Científico e Tecnológico] e FINEP [Financiadora de Estudos e Projetos]. The funding organizations did not limit the conduct of the research as planned and the authors have at all times retained full control of all primary data.
Competing interests:
None declared.
References
- 1.Paim J, Travassos CF, Almeida CF, Bahia LF, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377:1778–97. doi: 10.1016/S0140-6736(11)60054-8. [DOI] [PubMed] [Google Scholar]
- 2.Alkmim MB, Ribeiro AL, Carvalho GG, Pena M, Figueira RM, Carvalho MB. Success factors and difficulties for implementation of a telehealth system for remote villages: Minas Telecardio Project case in Brazil. J eHealth Technol Appl. 2007;5:197–202. [Google Scholar]
- 3.Jennett PA, Affleck Hall L, Hailey D, Ohinmaa A, Anderson C, Thomas R, et al. The socio-economic impact of telehealth: a systematic review. J Telemed Telecare. 2003;9:311–20. doi: 10.1258/135763303771005207. [DOI] [PubMed] [Google Scholar]
- 4.Kirigia JM, Seddoh A, Gatwiri D, Muthuri LH, Seddoh J. E-health: determinants, opportunities, challenges and the way forward for countries in the WHO African Region. BMC Public Health. 2005;5:137. doi: 10.1186/1471-2458-5-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deshpande A, Khoja S, McKibbon A, Jadad AR. Real-time (synchronous) telehealth in primary care: systematic review of systematic reviews (Technology Report No. 1002008) Ottawa: Canadian Agency for Drugs and Technologies in Health; 2008. [Google Scholar]
- 6.Ribeiro AL, Alkmim MB, Cardoso CS, Carvalho GG, Caiaffa WT, Andrade MV, et al. Implantação de um sistema de telecardiologia em Minas Gerais: projeto Minas Telecardio. Arq Bras Cardiol 20109570–8.Portuguese 10.1590/S0066-782X2010005000060 [DOI] [PubMed] [Google Scholar]
- 7.Andrade MV, Maia AC, Cardoso CS, Alkmim MB, Ribeiro AL.Custo-benefício do serviço de telecardiologia no Estado de Minas Gerais: projeto Minas Telecardio. Arq Bras Cardiol 201197307–16.Portuguese 10.1590/S0066-782X2011005000080 [DOI] [PubMed] [Google Scholar]
- 8.Cardoso CS, Ribeiro AL, Castro RL, César CC, Caiaffa WT. Implementation of a cardiology care program in remote areas in Brazil: influence of governability. Rural Remote Health. 2010;10:1472. [PubMed] [Google Scholar]
- 9.Oliveira GL, Cardoso CS, Ribeiro AL, Caiaffa WT.Satisfação de médicos com o cuidado às doenças cardiovasculares em municípios de Minas Gerais: Escala Cardiosatis-EQUIPE. Rev Bras Epidemiol 201114240–52.Portuguese 10.1590/S1415-790X2011000200006 [DOI] [PubMed] [Google Scholar]
- 10.Cardoso CS, Bandeira M, Ribeiro AL, Oliveira GL, Caiaffa WT.Escalas de satisfação com o atendimento às doenças cardiovasculares: CARDIOSATIS usuário e equipe. Cien Saude Colet 201116Suppl 11401–7.Portuguese 10.1590/S1413-81232011000700075 [DOI] [PubMed] [Google Scholar]
- 11.Moehr JR, Schaafsma J, Anglin C, Pantazi SV, Grimm NA, Anglin S. Success factors for telehealth–a case study. Int J Med Inform. 2006;75:755–63. doi: 10.1016/j.ijmedinf.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Ohinmaa A, Hailey D, Roine R. Elements for assessment of telemedicine applications. Int J Technol Assess Health Care. 2001;17:190–202. doi: 10.1017/S0266462300105057. [DOI] [PubMed] [Google Scholar]
- 13.Gagnon MP, Godin G, Gagné C, Fortin JP, Lamothe L, Reinharz D, et al. An adaptation of the theory of interpersonal behaviour to the study of telemedicine adoption by physicians. Int J Med Inform. 2003;71:103–15. doi: 10.1016/S1386-5056(03)00094-7. [DOI] [PubMed] [Google Scholar]
- 14.Whitten P, Love B. Patient and provider satisfaction with the use of telemedicine: overview and rationale for cautious enthusiasm. J Postgrad Med. 2005;51:294–300. [PubMed] [Google Scholar]
- 15.Whitten P, Holtz B. Provider utilization of telemedicine: the elephant in the room. Telemed J E Health. 2008;14:995–7. doi: 10.1089/tmj.2008.0126. [DOI] [PubMed] [Google Scholar]


