Abstract
Background:
In India the incidence of end stage renal disease (ESRD) is increasing day by day and the option for the treatment of ESRD is dialysis or transplantation. In the present scenario, due to the cost of treatment normal people can afford only hemodialysis rather than transplantation. Since the cost of hemodialysis differs across the country, research is needed to evaluate its exact cost.
Aim:
This study is to analyze the healthcare cost of hemodialysis in a private hospital of South India.
Materials and Methods:
This is a prospective, observational study carried out in a tertiary care hospital. Patients who are undergoing routine hemodialysis in this hospital were selected for the study. Patient data as well as cost details were collected for a period of six months. Thirty patients were selected for the study and a total of 2160 dialysis sessions were studied. Patient perspective was taken for the analysis of cost. Both direct and indirect costs were analyzed. This includes cost of dialysis, investigations, erythropoietin, food, transportation, lost wages etc. Socioeconomic status of the patient was also studied.
Result:
The total cost per session was found to be around Rs. 4500. Fifty six percent contributes direct medical cost whereas 20% contributes direct non medical cost. Twenty four percent cost was due to indirect costs. Since the patients are paying from their own pocket, only the upper or upper middle class patient can undergo hemodialysis regularly.
Conclusion:
These findings are important to find out the impact of cost of hemodialysis on patients suffering from ESRD. Further studies related to costs and outcome, otherwise known as pharmacoeconomic studies, are needed to analyze the pros and cons of renal replacement therapy and to improve the quality of life of ESRD patients. Thus pharmacoeconomical studies are needed to realize that government has to take initiative to provide insurance or reimbursement for the common people.
Keywords: Cost analysis, end stage renal disease, hemodialysis, pharmacoeconomics
Pharmacoeconomic evaluations have become an important tool in therapeutic decision making especially in chronic illness where there is limited resources.[1] It can be defined as the study of how individuals choose to allocate scarce pharmaceutical and health resources among competing alternatives and opt to distribute the products and services among members of the society.[2] According to International Society for Pharmacoeconomics and Outcome Research (ISPOR), pharmacoeconomics is the field of study that evaluates the behavior of individuals, firms, and markets relevant to the use of pharmaceutical products, services, and programs and which frequently focuses on the costs and consequences of that use.[3]
Newer diagnostic and therapeutic measures have emerged because of the advances in the medical field. This prolongs the life span of humans as well as increases the burden on chronic illness such as diabetes, hypertension, renal failure, etc. Despite these advances in medical fields, chronic renal failure is becoming a global threat particularly in developing countries. Levey et al. reported that chronic renal failure become one of the public health problem worldwide because of its incidence and prevalence, economic burden and poor quality of life.[4] The worldwide incidence of chronic renal failure has doubled in the last 15 years,[5] and its progression to end stage disease has been expected to be doubled during next 15 years.[6] Various studies reported that[7] the demand for renal replacement therapy, that is the treatment option for end stage renal disease, increases which in turn become a burden for healthcare services.[5,8] It is evident from the worldwide data that more than one million end stage renal disease (ESRD) patients are on renal replacement therapy where as two more million patients are in need of that.[9]
In India, it is reported that the progression of chronic kidney disease (CKD) to ESRD is rapid due to the factors such as lack of medical facilities, poor control of risk factors and delayed referral to nephrologists.[10] The prevalence of CKD and ESRD are estimated as 7852 and 1870 per million, respectively.[11,12] Majority of the patients about 60% will discontinue the therapy within 3 months.[10]
It is estimated that in India about 1 00 000 person suffering from ESRD each year, of which only about 20 000 get treated.[13] Over 3/4th of the people suffering from ESRD, especially from rural area, are not treated at all. That may be due to the factors such as lack of awareness of the disease and lack of treatment options; and the affordability is hindered by low income, minor reimbursement for chronic illness and non availability of insurance.[14,15] Every year, the patients opting renal replacement therapy increases approximately by 10%. According to the report in 2003, there are almost 80 000 people suffering from severe renal failure and only 650 dialysis centers are available.[16]
Most of the dialysis units are in the private sector[17] and the average hemodialysis cost anywhere in India range between Rs. 1200 and Rs. 2000 per session. When calculating the cost of hemodialysis in private hospitals, it comes around Rs. 12 000 per month and 1 40 000 per year.[17] In addition to this they have to pay for erythropoietin, lab test, consultation fee, etc. This becomes a nightmare for the common Indian people who cannot afford the expense. Many of them purposefully quit the sessions and their condition worsens terribly. Various studies have been carried out on cost of hemodialysis in different areas. In a study by Elsharif et al., the annual cost of hemodialysis was found to be US $ 6847.00 and they concluded that hemodialysis in Sudan is less expensive than transplantation. But when we compare with Indian scenario, the cost of hemodialysis in Sudan is more expensive than in India.[18] Another study in Barbados reported that 80.7% of the cost of hemodialysis was due to the direct medical cost.[19]
In contrast to that patient had to pay a nominal amount in government hospital for the dialysis.[17] Since the government hospitals are crowded with patients, they are not providing maintenance hemodialysis.[13] The growing kidney failure population and high cost of renal replacement therapy needs the economic evaluation of chronic illness.[20,21]
Studies revealed that there were slightly more men than women suffering from renal disease. This proposes that life style such as smoking and alcoholism also play a vital role in the progression of disease.[22,23] In India the number of death due to ESRD was 3.78 million in 1990 (40.4% of all death) and is expected to increase up to 7.73 million in 2020 (66.7% of all death).[24] Due to delayed diagnosis and failure to take suitable measures to prevent the progression of renal failure may result in end stage renal disease at young stage itself.[25,26]
Pharmacoeconomics is an important tool in the socioeconomic studies of healthcare system over the world especially in developing countries.[27–30] The exact detail of the total cost of hemodialysis in India according to the patient perspective was not found in any literature. The burden of end stage renal disease can be realized only if the costs are analyzed in patient perspective. This is the first study to analyze the direct as well as indirect cost of hemodialysis in a tertiary care hospital of South India. Since renal replacement therapy is an expensive treatment modality, it is very essential to assess the outcome of therapy in terms of quality of life, since this may be influenced by various factors such as comorbid conditions, age, dialysis frequency, infection/inflammation, etc.
This study gives the complete details of the cost associated with hemodialysis in a private sector on patient perspective.
Materials and Methods
A prospective analysis was carried out in Amrita Institute of Medical Sciences, Kerala which is a tertiary care hospital, to compare the outcome of hemodialysis patients from different socioeconomic status. Patients coming on outpatient basis were selected for the study. Patients were allotted in different shifts either in morning, afternoon or evening, based on their preferences. The study was approved by the institutional review board. The patients were followed up for a period of 6 months. The patient sociodemographics, cost details of dialysis, adverse reactions occurred during dialysis, cost to manage such adverse reactions, regularity, affordability, outcome and patient satisfaction to dialysis, etc. were collected prospectively.
Patient allotment and data collection
A total of 79 patients were undergoing dialysis per week in three different shifts during the study period. Thirty patients who were above the age of 18 years were selected. Sampling was done and every second patient in the OP was selected for the study. For simple analysis, patients undergoing dialysis thrice in a week, without considering the duration of dialysis were included in the study. Patients with major illness such as severe cardiac or neurological problems and those who avail reimbursement were excluded. Data of 2160 dialysis sessions of the 30 patients were analyzed. Based on the education, occupation and income, patients were categorized into upper, middle, and lower socioeconomic classes. Various parameters analyzed were compared among these groups.
Cost analysis
Patient perspective was taken for the analysis of cost component and the details were collected by direct patient interview. Details of direct medical cost, direct non-medical cost and indirect cost were analyzed. Direct medical cost includes cost of hemodialysis, laboratory investigation, erythropoietin, AV fistula, blood transfusion, X-ray and medications whereas direct non-medical costs include cost of food, transportation, and extra family care. Cost of lost wages was included in the indirect cost. In addition to this, cost arise due to complications, hospitalization, etc. were also included. Other costs such as intangible cost and opportunity costs were excluded. From the data obtained, overall costs of hemodialysis per session as well as total cost for a period of 6 months were calculated.
The patient data were collected by using the patient data collection form and by the direct patient interview. Patient's demographics, socioeconomic status, comorbid conditions, cost of therapy, regularity, and affordability of hemodialysis, etc. were incorporated in the data collection form. Socioeconomic status was also studied using Kuppuswamy's scale since the hospital is located in urban area, and the patients are also from such places. Consultation from physician, nursing staff, and dialysis staff were taken whenever necessary. Outcomes were compared between patients of different socioecomic status in order to assess regularity, affordability, clinical condition and satisfaction.[31,32] Statistical tests (Pearson correlation) were applied to analyze the data using statistical package for the social sciences (SPSS) version 14.
Results
Out of 79 patients undergoing hemodialysis during the study period, 30 patients were selected based on the inclusion and exclusion criteria, which is given in detail in the methodology section. Sampling was also done to prevent bias. Among these 30 patients, 22 were males and 8 were females. The sociodemographics as well as the comorbid conditions of the patients were given in Table 1. Majority of the patients were in the age group of 51–60 with a mean age of 49.72 ± 13.2 and associated with comorbid conditions. Diabetes and hypertension were found to be the predominant causes compared to other disease states. Out of this, six patients were suffered from diabetes where as 13 patients had hypertension. Five patients had both diabetes and hypertension. Duration of renal failure as well as duration of dialysis was also calculated and the result was 4.2 ± 1.6 and 2.8 ± 1.8 years, respectively. All the patients were on dialysis thrice in a week.
Table 1.
Sociodemographics data
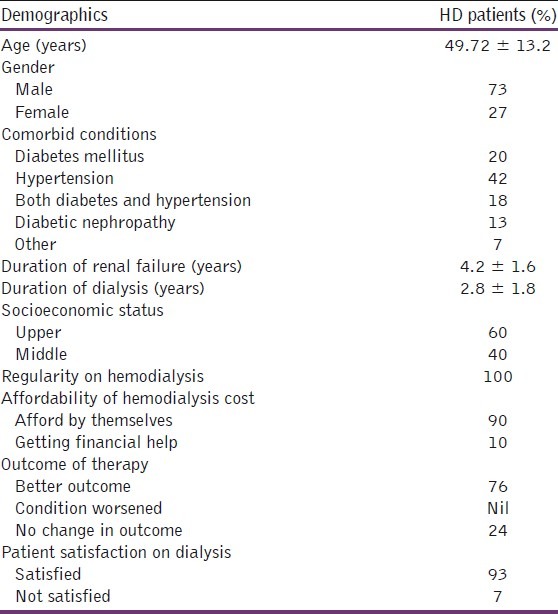
Socioeconomic status of the patients was also calculated according to modified Kuppuswamy scale based on their educational qualification, occupation, and annual income.[33] It was found that 18 patients were on upper class and 12 were on middle class. Lower class patients were not there, that may be due to the fact of non-affordability. This was assessed with the help of a questionnaire by Erika. All the 18 patients on upper socioeconomic class were regular on dialysis and were able to afford the cost by themselves. The patients from middle class family were also regular on dialysis, but three patients could afford it with the financial help of friends or relatives. Such details were captured during the patient interview.
Clinical outcome was also analyzed to assess whether the patients had better, worse or no change in outcome. By doing a comprehensive survey, we asked the patients to rate their clinical outcome on a visual analog scale from 1 (worsen the condition after treatment) to 5 (improved very much after the treatment). Fifteen patients on upper class and eight from middle class experiences better clinical outcome. The correlation between the socioeconomic status and parameters such as regularity, affordability, outcome and patient satisfaction were tested. It revealed that there is no significant correlation between socioeconomic status and regularity, affordability or outcome. Analysis of patient satisfaction[31,32] showed that all the patients from upper class were satisfied with the dialysis modality while two patients from the middle class family were not at all satisfied with the treatment. Patient satisfaction scale was used in order to evaluate this and the result showed 26.5 ± 1.2 VS 18.4 ± 2.6; P<0.001. (upper vs. middle). The sociodemographic details along with the regularity, affordability, clinical outcome and patient satisfaction were given in Table 1.
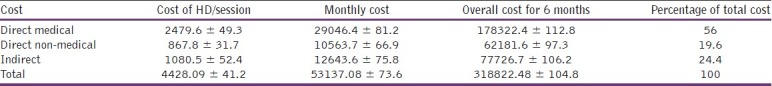
The cost of each session of dialysis and the overall cost for 6 months were calculated and found that the direct cost is more than the indirect costs. Details of the categorization of costs were given in the cost analysis section of methodology. Fifty six percent of the total cost was contributed by direct medical cost and 19.6% was for the direct non-medical cost. Indirect cost was calculated based on the number of missed working hours and the percentage of current income compared to the income that the patients had before they entered the dialysis procedure. The details were shown in Table 2.
Table 2.
Cost analysis of hemodialysis treatment
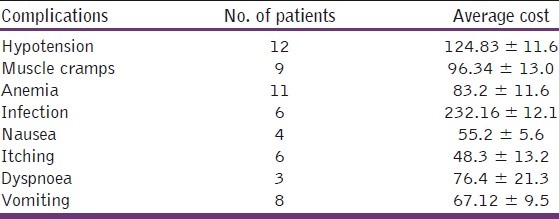
Since the patients had different co morbidities, the management cost of comorbid conditions were also analyzed. Table 3 illustrates the details of comorbidities. The side effects experienced during dialysis were also studied. The major complications were muscle cramps, nausea, itching, dyspnoea, vomiting and anemia. These were also properly managed and the additional expenses were provided in Table 4.
Table 3.
Additional costs according to comorbid conditions
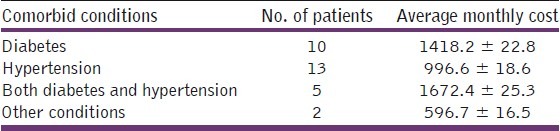
Table 4.
Additional cost to manage the complications occurred during dialysis
Discussion
Dialysis is an expensive therapy. The average cost per session was found to be Rs. 4428, which is difficult to afford by the common people. The cost to manage the co morbid conditions may further aggravate the situation. Since diabetes and hypertension are the major contributing factor of renal failure that has to be managed properly in its initial stage itself. The lifelong treatment of renal failure along with diabetes and hypertension significantly increase the burden on patients and decreases the outcome also. A study conducted by Rao et al. showed that diabetes is the main cause of poor outcome along with cardiovascular risk.[34]
Studies revealed that the mean age of ESRD patients on hemodialysis in developing countries is lower (32-42 years) than the developed countries (60–63 years).[34,35] Our study is also consistent with this, with a mean age of 49.72 ± 13.2. The reason for the progression of renal failure may be the delay in detecting the renal disease, late referral, and failure to introduce preventive measures. Jha illustrates that 70% of the dialysis centers are in private sector and are accessible for upper income patients’ only.[36] In this study, we found that 10% of the study population find difficult to afford it.
According to the report of Kher, 60% of the hemodialysis patients were lost to follow up within 3 months because of its high cost.[13] Another study conducted by Mani described that only 4% of people can pay from their own resources, 63% from their employers or charity, 30% will sell the property or jewellery, and 20% will take loan.[37] The study conducted by Abraham illustrates that the proportionate hemodialysis cost in low income countries is about five times greater than in developed countries.[22] This may lead to dropout and further complication of the diseased state.[19]
According to the socioeconomic status of the patient, only upper and middle class people can afford the hemodialysis service offered by the private sector. Patients on low economic status take pain for the regular dialysis and to manage the complications. Since they cannot afford the costs in private hospitals, they usually approach public hospitals.
Patients from the middle income family face difficulty in affording the costs for the management of co morbid conditions along with the dialysis cost. This will affect the clinical outcome as well as the satisfaction with the treatment. Upper class patients’ experiences better clinical outcome as well as patient satisfaction when compared to middle class people because they were able to manage the cost without affecting much to their daily life. There is no significant difference in the regularity as well as affordability even though the middle class people face a lot of problems.
Research is necessary in this area to quantify the cost of therapy at the public sector. Studies have to be conducted to evaluate the cost and outcome of hemodialysis patients approaching public vs private hospitals. The quality of life of patients at both the centers also should be evaluated in order to assess the cost effectiveness. If the patients achieve better quality of life at the public sector, government has to take initiative to commence more dialysis centers at the public level. Recently various non-governmental organizations as well as charity trusts are coming up in order to provide more cost-effective management. Drugs mainly for hypertension as well as diabetes supplying at free of cost will also help the patients to reduce the overall burden of renal failure.
Strength and Weakness of the Study
This is the first study to analyze the direct as well as indirect cost of hemodialysis in a tertiary care hospital of South India. From this observational study, we could found that 75.6% of the cost was due to direct costs (direct medical and non-medical costs) and 24.4% was due to indirect costs. This information can be a basis for future studies of pharmacoeconomic evaluations.
The main limitation of the study is its duration. This analyzes the data of 6 months only and not extrapolated. Another major limitation is that this data is from a single center. The information could have been much valuable if it is a multicenter study.
Conclusions
The dialysis modality for the ESRD patients remains the most preferred resources. The non availability or less availability of dialysis unit in public sector compared to private sector, and also lack of reimbursing or insurance scheme to the dialysis patients are the major concerns in a country like India. Only the upper or upper middle class people can afford hemodialysis due to its high cost.
They are also several approaches to reduce the annual cost of renal replacement therapy (RRT). Obviously in long term, the most important factor is to reduce the number of patients with ESRD. This can be achieved by preventing the progression of renal disease. In India, the most frequent causes of ESRD are diabetes and hypertension. Early detection and treatment of these diseases play a vital role in the prevention of progression of renal failure and to postpone the need of RRT to an extent. A clinical pharmacist can be really helpful to prevent this progression of ESRD by providing patient counseling about lifestyle modification and educating the risk group and motivating them for regular check up and adhering to the treatment. And also better helping hands from the government sector like more hemodialysis unit, insurance and reimbursement scheme to the patients can provide better patient outcome in our country. Long-term studies are needed to assess the cost and consequences of the treatment modalities of ESRD patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Juan GP, Luke V, Sally CS, Sarah W. Hemodialysis for ESRD: A cost effectiveness analysis of treatment options. Int J Tech Ass Healthcare. 2005;21:32–9. doi: 10.1017/s026646230505004x. [DOI] [PubMed] [Google Scholar]
- 2.Revikumar KG, Miglani BD. A Text book of Pharmacy Practice. 1st ed. Nasik, India: Career Publication; 2009. Pharmacoeconomics and Quality of Life; pp. 443–95. [Google Scholar]
- 3.Pashos CL, Klein EG, Wanke LA. 1st ed. Princeton, NJ: International Society for Pharmacoeconomics and Outcome Research; 1998. ISPOR Lexicon. [Google Scholar]
- 4.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National kidney foundation practice guidelines for chronic kidney disease: Evaluation, classification and stratification. Ann Intern Med. 2003;139:137–47. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 5.Dash SC, Agarwal SK. Incidence of chronic kidney disease in India. Nephrol Dial Transplant. 2006;21:232–3. doi: 10.1093/ndt/gfi094. [DOI] [PubMed] [Google Scholar]
- 6.Minneapolis: USRDS; 2007. US Renal Data System. USRDS 2007 annual data report: Atlas of end stage renal disease in the United States, National Institute of Health. [Google Scholar]
- 7.Hallan SI, Vikse BE. Relationship between chronic kidney disease prevalence and end stage renal disease risk. Curr Opin Nephrol Hypertens. 2008;17:286–91. doi: 10.1097/MNH.0b013e3282f8b177. [DOI] [PubMed] [Google Scholar]
- 8.Daphne K, Panagiotis NZ, Nikolaos M, Lycurgus LL. Economic evaluation of hemodialysis: Implications for technology assessment in Greece. Int J Tech Ass Healthcare. 2005;21:40–6. doi: 10.1017/s0266462305050051. [DOI] [PubMed] [Google Scholar]
- 9.Prodjosudjadi W, Suhardjono A. End stage renal disease in Indonesia: Treatment development. Ethn Dis. 2009;19(1 Suppl 1):S1-33–6. [PubMed] [Google Scholar]
- 10.Ballal HS. The burden of chronic kidney disease in a developing country, India. Ouest. 2007;9:12–9. [Google Scholar]
- 11.Agarwal SK, Dash SC, Irshad M, Raju S, Singh R, Pandey RM. Prevalence of chronic renal failure in adults in Delhi, India. Nephrol Dial Transplant. 2005;20:1638–42. doi: 10.1093/ndt/gfh855. [DOI] [PubMed] [Google Scholar]
- 12.Mani MK. Prevention of chronic renal failure at the community level. Kidney Int Suppl. 2003;(83):S86–9. doi: 10.1046/j.1523-1755.63.s83.17.x. [DOI] [PubMed] [Google Scholar]
- 13.Kher V. End stage renal disease in developing countries. Kidney Int. 2002;62:350–62. doi: 10.1046/j.1523-1755.2002.00426.x. [DOI] [PubMed] [Google Scholar]
- 14.Nick K, Dimitris N, John M. A socioeconomic comparison of hemodialysis and peritonial dialysis in Greece. Int J Healthc Tech Manage. 2005;13:296–306. [Google Scholar]
- 15.Crealey GE, Sturgess IK, McElnay JC, Hughes CM. Pharmaceutical care programmes for the Elderly: Economic issues. Pharmaeconomics. 2003;21:455–65. doi: 10.2165/00019053-200321070-00001. [DOI] [PubMed] [Google Scholar]
- 16.Sakhuja V, Sud K. End stage renal disease in India and Pakistan: Burden of disease and management issues. Kidney Int. 2003;63:S115–8. doi: 10.1046/j.1523-1755.63.s83.24.x. [DOI] [PubMed] [Google Scholar]
- 17.Khanna U. The economics of dialysis in India. Ind J of Nephrology. 2009;19:1–4. doi: 10.4103/0971-4065.50671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elsharif ME, Elsharif EG, Gadour WH. Cost of hemodialysis and kidney transplantation in Sudan- A single center experience. Iran J Kidney Dis. 2010;4:282–4. [PubMed] [Google Scholar]
- 19.Adomakoh SA, Adi CN, Fraser HS, Nicholson GD. Dialysis in Barbados: The cost of hemodialysis provision at the queen elizabeth hospital. Rev Panam Salud Publica. 2004;16:350–5. doi: 10.1590/s1020-49892004001100009. [DOI] [PubMed] [Google Scholar]
- 20.Salonen T, Reina T, Oksa H, Sintonen H, Pasternack A. Cost analysis of renal replacement therapies in Finland. Am J Kidney Dis. 2005;42:1228–38. doi: 10.1053/j.ajkd.2003.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Lee H, Manns B, Taub K, Ghali WA, Dean S, Johnson D, et al. Cost analysis of ongoing care of patient with ESRD: The impact of dialysis modality and dialysis. Am J Kidney Dis. 2002;40:611–22. doi: 10.1053/ajkd.2002.34924. [DOI] [PubMed] [Google Scholar]
- 22.Abraham G, Jayaseelan T, Matthew M, Padma P, Saravanan AK, Lesley N, et al. Resource settings have a major influence on the outcome of maintenance hemodialysis patients in South India. Hemodial Int. 2010;14:211–7. doi: 10.1111/j.1542-4758.2010.00441.x. [DOI] [PubMed] [Google Scholar]
- 23.Manandhar DN, Chhetri PK, Tiwari R, Lamichhane S. Evaluation of dialysis adequacy in patients under hemodialysis and effectiveness of dialysere reuses. Nepal Med Coll J. 2009;11:107–10. [PubMed] [Google Scholar]
- 24.Modi GK, Jha V. The incidence of ESRD in India: A population based study. Kidney Int. 2006;70:2131–3. doi: 10.1038/sj.ki.5001958. [DOI] [PubMed] [Google Scholar]
- 25.Hooi LS. Incidence of end stage renal failure in Johore, Malaysia. Med J Malaysia. 1994;49:360–8. [Google Scholar]
- 26.Croxson BE, Ashton T. A cost effectiveness analysis of the treatment of ESRF. NZ Med J. 1990;103:171–4. [PubMed] [Google Scholar]
- 27.Zelmer JR. The economic burden of end stage renal disease in Canada. Kidney Int. 2007;72:1122–9. doi: 10.1038/sj.ki.5002459. [DOI] [PubMed] [Google Scholar]
- 28.Tediosi F, Bertolini G, Parazzini F, Mecca G, Garattini L. Cost analysis of dialysis modalities in Italy. Health Serv Manage Res. 2001;14:9–17. doi: 10.1177/095148480101400102. [DOI] [PubMed] [Google Scholar]
- 29.Ardine GW, Paul GR. Economic evaluation of ESRD treatment. Health Policy. 1998;44:215–32. doi: 10.1016/s0168-8510(98)00017-7. [DOI] [PubMed] [Google Scholar]
- 30.Gardner TI, Dardis R. Cost effectiveness analysis of ESRD treatments. Med Care. 1987;25:25–34. doi: 10.1097/00005650-198701000-00004. [DOI] [PubMed] [Google Scholar]
- 31.RAND, KDQOL-SF™ User's manual. 1993 [Google Scholar]
- 32.DiMatteo MR, Hays R. The significance of Patient's Perceptions of Physician conduct: A study of patient satisfaction in a family practice center. J Community Health. 1980;6:18–34. doi: 10.1007/BF01324054. [DOI] [PubMed] [Google Scholar]
- 33.Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74:1131–2. [PubMed] [Google Scholar]
- 34.Rao M, Juneja R, Shirley Rd, Jacob CK. Hemodialysis for end stage renal disease in Southern India.A perspective from a tertiary care center. Nephrol Dial Transplant. 1998;13:2494–500. doi: 10.1093/ndt/13.10.2494. [DOI] [PubMed] [Google Scholar]
- 35.Mittal S, Kher V, Gulati S, Agarwal LK, Arora P. Chronic renal failure in India. Ren Fail. 1997;19:763–70. doi: 10.3109/08860229709037216. [DOI] [PubMed] [Google Scholar]
- 36.Jha V, Chugh KS. Dialysis in developing countries: Priorities and obstacles. Nephrology. 1996;2:65–72. [Google Scholar]
- 37.Mani MK. The management of end stage renal disease in India. Artif Organs. 1998;22:182–6. doi: 10.1046/j.1525-1594.1998.06070.x. [DOI] [PubMed] [Google Scholar]


