Abstract
Melanotic neuroectodermal tumor of infancy is a very rare benign but locally aggressive neoplasm of neural crest origin with a high recurrence rate. It usually affects infants of less than 1 year of age. Most commonly, the lesion affects the maxilla followed by skull, mandible, brain and other extracranial sites. We report an 11-month-old female baby with a similar tumor involving the anterior region of maxilla along with a brief review of the literature and differential diagnosis. A wide surgical excision was performed by an intraoral approach. A 2-year follow-up of the patient showed no recurrence.
Keywords: Benign, maxilla, melanotic neuroectodermal tumor, neural crest
Introduction
Melanotic neuroectodermal tumor of infancy (MNTI) is a rare benign, non-ulcerative, painless, rapid expansile tumefaction of neural crest origin[1–3] with a high recurrence rate.[4] The rate of recurrence has been estimated at 15%, and the rate of malignant transformation at 6.6%.[3] Although classified as a benign lesion, it often grows very rapidly and, occasionally, invades the bone marrow diffusely without forming a fibrous capsule.[5] Approximately 92.8% of MNTIs occurred in the head and neck region of infants less than 1 year of age. Very rarely, the lesion is seen in adults, but oral cavity and jaws are not involved.[6] Gender predilection is still a matter of ambiguity, although Kruse-Losler et al. reported a higher prevalence in men (male/female: 1.48).[6] The majority of lesions arise in the maxilla (68–80%), followed by skull (10.8%), mandible (5.8%) and brain (4.3%).[7] It has also been reported in the extracranial sites like long bones epididymis, mediastinum, soft tissues of extremities, shoulder, ovary, uterus, thigh, etc.[3,5,8] The most frequent extracranial sites are genital organs.[1,9] Clinically, MNTI of the jaws appears as an expansive tumor mass, frequently involving tooth displacement.[6] It is a pigmented tumor, although the pigmentation cannot always be observed through the covering tissues.[3]
Case Report
An 11-month-old female baby presented to the Department of Oral Medicine and Radiology with an asymptomatic swelling in the anterior region of the maxilla. Her parents noticed the swelling at the age of 6 months, which was slowly progressive initially and started growing rapidly for the last 2 months, thus preventing the baby from feeding. There was no history of medication during pregnancy and no relevant medical history was present. Growth and development of the infant were normal for her age. On clinical examination, a non-pigmented, non-ulcerative, non-pedunculated swelling of size 4 cm × 3 cm was seen in the pre-maxilla region with facial asymmetry [Figure 1]. The swelling obliterated the gingivolabial sulcus pushing the upper lip forward and upwards with flaring of the lower part of the nose. The mucosa overlying the swelling was intact and both the primary central incisors (51, 61) were displaced apart [Figure 2]. On palpation, the swelling was non-tender, firm in consistency and non-fluctuant. There were no visible or palpable pulsations. Radiographically, the lesion appeared as a mixed radiolucent and radioopacity with ill-defined and irregular borders suggestive of both osteolytic and osteogenic reaction [Figure 3]. Routine laboratory investigations were within normal limits, except for urine levels of vanillyl mandelic acid (VMA) that were elevated, suggesting that the tumor is of a neuralcrest origin. The pre-operative diagnosis was made as MNTI based on the fine needle aspiration cytology report showing dual population of small neuroblast-like cells and large melanin-containing epithelial cells. An incisional biopsy of the tumor was performed under general anesthesia and the specimen was sent for histopathology. Microscopically [Figure 4], the specimen showed an intraosseous lesion that eroded the bone and was covered by intact overlying mucosa. Bone destruction was also seen at the periphery of the tumor while the center of the lesion did not contain any bone fragments. The background of the tumor was fibrotic and contained irregular islands of tumor cells. There appear to be two populations of tumor cells, the large melanotic (pigmented) type and the small (non-pigmented) type. On higher magnifications [Figure 5], the small cells had morphologic features of primitive neuroepithelial cells while the larger cells had features of melanocytes. Based on the above histopathologic findings, the lesion was finally diagnosed as MNTI. A conservative surgical excision of the tumor was performed under general anesthesia along with curettage of the surrounding normal bone and extraction of primary central incisors. The patient's recovery was uneventful, without any post-operative complications. There was no recurrence of the tumor in the 2-year follow-up period.
Figure 1.

Clinical presentation of the lesion in the anterior maxilla causing facial asymmetry
Figure 2.

Firm, non-ulcerated, non-pigmented, non-pedunculated swelling in the anterior maxilla with displacement of deciduous central incisors
Figure 3.

An IOPA Intraoral periapical radiograph showing a mixed radiolucent and radioopaque lesion with ill-defined and irregular borders
Figure 4.
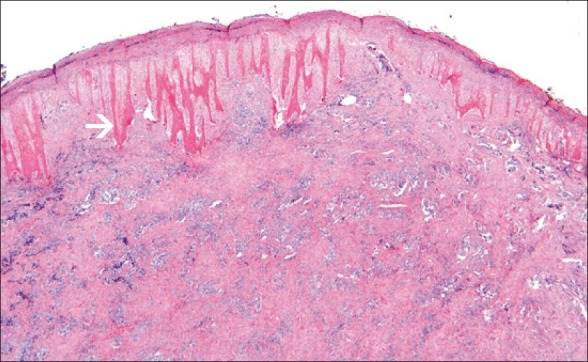
The background of the tumor as fibrotic and containing irregular islands of tumor cells. There appears to be two populations of tumor cells, the large melanotic (pigmented) type and the small (non-pigmented) type (×10)
Figure 5.
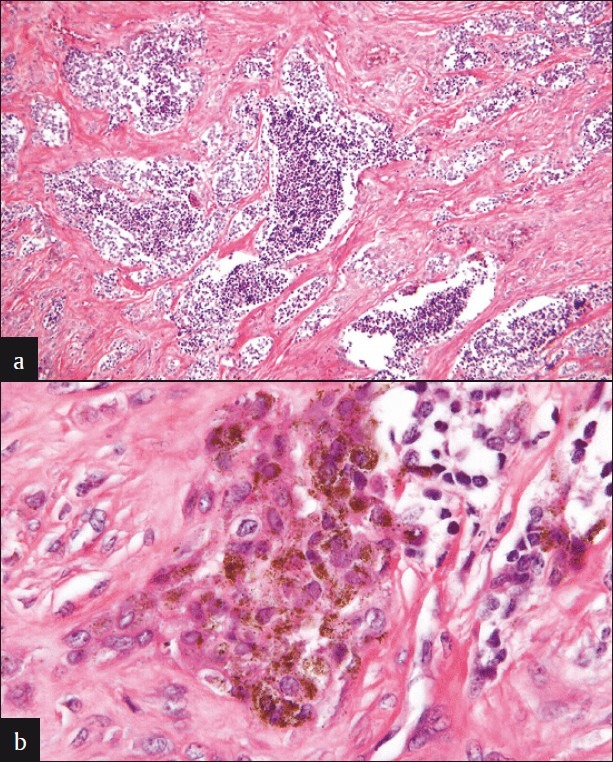
(a) Photomicrographs showing small cells having morphologic features of primitive neuroepithelial cells while the larger cells have features of melanocytes (b) Photomicrographs (higher magnifi cation) showing small cells having morphologic features of primitive neuroepithelial cells while the larger cells have features of melanocytes
Discussion
Krompecher described a pigmented tumor of the maxilla associated with a developing tooth and elements of dental lamina in a 2-month-old infant.[4] This was the first case to be reported and was designated as congenital melanocarcinoma.[8] Mummery and Pitts reported a case of pigmented maxillary tumor in a 5-month-old baby girl that arose from aberration of dental epithelium and was termed as melanotic epithelial odontoma.[4] Hal pert and Patzer (1947) reported a similar tumor that contained pigmented epithelium and was suggestive of ciliary body of the eye.[4] Small unpigmented cells that resemble neuroblasts from the retinal neuroepithelium were also present. They suggested that the tumor arose from the entrapment of retinal analge in the embryologic fusion lines of developing maxilla.[4] Stowens reported three cases of a tumor, and he believed that the tumor resembled the vomeronasal organ of Jacobson in several ways.[4] Misugs and colleagues (1965) suggested that the growth is derived from the neural crest.[8] Borello and Gorlin reported a case of MNTI in the maxilla in a 3-month-old boy where there was increased excretion of VMA, which returned to normal after the tumor was removed.[4] A high urinary level of VMA is common in tumors of neural crest origin. Because this tumor is common in infancy, they recommended the term MNTI.[4] VMA is a major urinary catabolite of catecholamines. An increase in its free form is regarded as a marker of neuroectodermal tumors.[3] The disappearance of high rates of VMA after MNTI surgical removal confirms the neurocrystopathic hypothesis.[3] A significant number of cases of MNTI with normal levels of VMA appear in the literature. However, a negative rate of VMA should not influence the diagnosis of MNTI, because not all the cells of neural crest are involved in the metabolism of catecholamines.[3] The histochemical and ultrastructural features of MNTI cells make them very similar to the neural crest cells.[3] Drooling and her associates found similarity in the microscopic appearance between this tumor and the developing pineal gland, and have suggested that the fetal pineal gland may be the precursor of this tumor.[8] The other synonyms of this tumor are pigmented epulis, melanotic ameloblastoma, melanoticprogonoma, melanotic adamantinoma and epithelial odontoma.[6,10] Clinically, MNTI is a rapidly growing, painless, expansile, non-ulcerative swelling especially occurring in the craniofacial region. Although MNTI tumor cells do produce melanin, the expected corresponding pigmentation is not always clinically evident, despite the lesion's name,[10] as seen in our case. MNTI occurred most frequently within the first 6 months of life, with a peak between the second and sixth months. Only 8.9% of the manifestations of MNTI were found at an age of more than 12 months.[6] The most common radiographic image is a large cavity of osteolysis with a well-delineated form without any specificity.[3] The image could be less marked from a simple thinning of the cortical bone to real bone destruction, with or without osteogenic reaction.[3] Extensive tumor calcification has been noted.[10] The margins of the radiolucency displace the adjacent bone and tooth buds, suggesting a tumor-like invagination within the dental follicle.[3] This image is poorly delineated, with heterogeneous content organized in the wheel spokes, which could lead to the diagnosis of an osteosarcoma.[3] Magnetic resonance imaging (MRI) with gadolinium enhancement gives the clearest images, allowing the distinction of the tissue components of this tumor.[3] The MRI reveals a hypodense mass within a heterogeneous well-delineated lesion on t1-t2-weighted images.[3] Microscopically, MNTIs are biphasic tumors with one cell population consisting of cuboidal epithelial cells with open vesicular nuclei clustered in alveolar or tubular patterns. These cells typically have abundant brown intracellular melanin granules. The second lesional cell is a small, dark, round cell with a hyperchromatic nucleus and minimal cytoplasma. It has the appearance of a neuroblast. The cells aggregate in loose nests or islands within the background of fibrovascular tisssue.[7]
Differential diagnosis
Oral and maxillofacial tumors rarely occur in the pediatric population compared with the adult population.[11] Most jaw swellings that occur in the infants are usually benign odontogenic cysts or tumors.[11] However, some lesions although benign tend to have an alarming growth rate. Therefore, there is a possibility of misdiagnosing them clinically as malignant lesions.[11] The clinical differential diagnosis of a rapidly growing swelling of the anterior maxilla in an infant includes congenital epulis, teratoma, neuroblastoma, Ewing's sarcoma, rhabdomyosarcoma, melanoma, congenital eruption cyst, Burkits lymphoma, Langerhans cell histiocytosis and hemangioma.
Congenital epulis is always present at birth, and can be alarmingly large and may interfere with the infant's ability to feed, as did the lesion reported in our case.[10] Congenital epulis is almost always reported to be pedunculated, whereas MNTI seemed to present sometime after birth and was sessile rather than pedunculated.[10] Teratomas can be differentiated from MNTI only by histopathology by the presence of multiple tissues, including teeth foreign to the sites from which they originate.[12] Neuroblastoma is a malignant tumor occurring in infants and young children, and may arise at any site in the sympathetic nervous system, most commonly in the abdomen. Metastatic neuroblastoma occurs most commonly in the mandible, presenting clinically by the deviation of the mandible on mouth opening, changes in occlusion, periorbital ecchymosis and Horner's syndrome, which are not seen in MNTI.[13] Ewing's sarcoma is a rare malignant tumor of neuroectodermal origin affecting the skeletal system, with long bones and pelvis being the most common locations. It affects mainly adolescents and young adults and is rarely seen before the age of 5 and after the age of 30 years. Its occurrence in the head and neck is rare and, when it occurs, it generally involves the mandible and less frequently the maxilla. Clinically, this tumor has an aggressive behavior, characterized by rapid growth and high probability of micrometastasis at diagnosis, whereas MNTI is painless, and the most common site is maxilla and usually occurs in infants less than 1 year of age.[14] Embryonal rhabdomyosarcoma occurs in children less than 15 years of age, and peak incidence occurs between 2 and 6 years. Clinically, these tumors exhibit a fast and aggressive growth, reaching large dimensions, and are generally painless. Most of the cases present in the oral cavity occur on the palate or the tongue. The patient may present with signs and symptoms of pain, paresthesia, loss of teeth or trismus as a result of advanced tumor stage, infiltrative growth and tumor location.[15] The most commonly affected intraoral sites are the tongue, soft palate, floor of the mouth and buccal mucosa.[15] MNTI can be differentiated by its painless nature, and the most common site of occurrence is the maxilla. Oral mucosal melanomas can be differentiated from MNTI in terms of age of occurrence (fourth to seventh decades) and site of occurrence, i.e. palate. Congenital eruption cyst occurs within the mucosa overlying the teeth that are about to erupt. It is not detectable on radiographic examination because there is usually no bone involvement, whereas MNTI usually presents as an osteolytic lesion.[16] Endemic type of Burkits lymphoma occurs in the jaws and facial bones, whereas the non-endemic types occur in other sites. The mean age of presentation is between 7 and 14 years,[17] whereas MNTI occurs in infants less than 1 year of age, and both the lesions can only be differentiated by histopathological means. The clinical manifestations of Langerhans cell histiocytosis may range from single or multifocal bone lesions to disseminated oral disease with multiorgan involvement.[18] Radiographically, teeth floating in air appearance is seen, and can be differentiated from MNTI by histopathology. Central hemangioma is frequently found in the vertebrae and skull and rarely develops in the jaws. The lesion produces a hard, non-tender, slow-growing swelling. The teeth in the vicinity may be loosened and have hypermobility and bleeding may occur from the gingiva around the necks of affected teeth exhibiting a pumping action.[19] Central hemangioma can be differentiated from MNTI by the presence of pulsations and bruit on auscultation and pumping action of the teeth along with bleeding from the necks of the affected teeth.[19]
Management
The treatment of choice consists of complete surgical excision, conservative surgical treatment, wide local excision and chemotherapy. Because of the benign nature of the tumor, most authors agree on a conservative surgical treatment.[3] This lesion is known to recur, with a reported recurrence rate of 10–15%.[1] Recurrence may be the consequence of incomplete removal, seeding during surgery or tumor multicentricity of the primary tumor.[7] In case of recurrence, extensive resection along with reconstructive surgery is indicated. Hence, clinical monitoring of the patient and radiological survey are essential. When a metastatic dissemination arises, the secondary lesions are only made up of few differentiated cells of neuroblastoid line, which is regarded as the aggressive component of the tumor. Chemotherapy is not a usual treatment procedure except for cases of confirmed metastatic diffusion. At the cellular level, the result of chemotherapy shows an impressive reduction of the neuroblastoid population.[3] Although little was known about chemotherapy, a neuroblastoma protocol was followed because of its molecular genetic similarity to neuroblastomas. In total, six cycles of neuroblastoma chemotherapy protocol can be administered. Vincristine day 1, isofosfamide days 1 and 2, carboplatin day 3 and etoposide day 4. After six courses, histological complete remission can be achieved.[7]
Conclusion
Although the majority of the tumors are benign, an average recurrence rate of 15–20% and a malignancy rate of 6.5% are reported in the literature. Hence, a careful follow-up is mandatory. Early clinical diagnosis and treatment at the appropriate time can prevent complications and metastasis. In our present case, early diagnosis and treatment were done and the patient was followed-up for 2 years without any recurrence.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Jain P, Saxena S, Aryya NC. Melanotic neuroectodermal tumour of infancy: A rare maxillary alveolar tumour. Eur J Plast Surg. 2003;26:35–7. [Google Scholar]
- 2.Chaudhary A, Wakhlu A, Mittal N, Misra S, Mehrotra D. Melanotic Neuroectodermal Tumor of Infancy: 2 Decades of clinical experience with 18 patients. J Oral Maxillofac Surg. 2009;67:47–51. doi: 10.1016/j.joms.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 3.Madrid C, Aziza J, Hlali A, Bouferrache K, Abarca M. Melanotic neuroectodermal tumour of infancy: A case report and review of the aetiopathogenic hypotheses. Med Oral Patol Oral Cir Bucal. 2010;15:e739–42. doi: 10.4317/medoral.15.e739. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal P, Saxena S, Kumar S, Gupta R. Melanotic neuroectodermal tumour of infancy: Presentation of a case affecting the maxilla. J Oral Maxillofac Pathol. 2010;14:29–32. doi: 10.4103/0973-029X.64309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta A, Trehan A, Marwaha RK, Sharma RK, Nijhawan R. Indian J Paediatr. 2002;69:725–6. doi: 10.1007/BF02722714. [DOI] [PubMed] [Google Scholar]
- 6.Kruse-Losler B, Gaertner C, Burger H, Seper L, Joos U, Kleinheinz J. Melanotic neuroectodermal tumor of infancy: Systematic review of the literature and presentation of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:204–16. doi: 10.1016/j.tripleo.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Neven J, Hulsbergen-van der Kaa C, Groot-Loonen J, de Wilde PC, Merkx MA. Recurrent melanotic neuroectodermal tumour of infancy: A proposal for treatment protocol with surgery and adjuvant chemotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:493–6. doi: 10.1016/j.tripleo.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Kalra N, Srivatsava D, Goswami A, Narang A, Rani U. Melanotic neuroectodermal tumour of infancy: A Case report. J Indian Soc Pedo Prev Dent. 2001;19:134–6. [PubMed] [Google Scholar]
- 9.Agarwal P, Agarwal V, Raina VK. Melanotic neuroectodermal tumour of infancy: Case report of an unusual tumor. Indian J Plast Surg. 2003;36:123–5. [Google Scholar]
- 10.McGuire TP, Gomes PP, Forte V, Sándor GK. Rapidly growing Intraoral Swelling Involving the Maxilla of an Infant. J Oral Maxillofac Surg. 2007;65:1595–9. doi: 10.1016/j.joms.2006.11.057. [DOI] [PubMed] [Google Scholar]
- 11.Renner LA, Abdulai AE. Melanoticneuroectodermal tumourinfancy (progonoma) treated by radical maxillary surgery. Ghana Med J. 2009;43:90–1. doi: 10.4314/gmj.v43i2.55322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiang YH, Zhou Q, Zheng JW, Wang YA. Mushroom-shaped teratoma of the soft palate in a neonate: Case report. Br J Oral Maxillofac Surg. 2010;48:e25–6. doi: 10.1016/j.bjoms.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Schell M, Bergeron C. Neuroblastoma. Orphanet encyclopedia. 2003. Oct, Available from: http://www.orpha.net/data/patho/GB/ukneuroblastoma.pdf .
- 14.Brazão-Silva MT, Fernandes AV, Faria PR, Cardoso SV, Loyola AM. Ewing's Sarcoma of the Mandible in a Young Child. Braz Dent J. 2010;21:74–9. doi: 10.1590/s0103-64402010000100012. [DOI] [PubMed] [Google Scholar]
- 15.Gordón-Núñez MA, Piva MR, Dos Anjos ED, Freitas RA. Orofacial Rhabdomyosarcoma: Report of a case and review of the literature. Med Oral Patol Oral Cir Bucal. 2008;13:E765–9. [PubMed] [Google Scholar]
- 16.Alemán Navas RM, Martínez Mendoza MG, Leonardo MR, Silva RA, Herrera HW, Herrera HP. Congenital eruption cyst: A case report. Braz Dent J. 2010;21:259–62. doi: 10.1590/s0103-64402010000300015. [DOI] [PubMed] [Google Scholar]
- 17.Valenzuela-Salas B, Dean-Ferrer A, Alamillos-Granados FJ. Burkitt's lymphoma: A child's case presenting in the maxilla: Clinical and radiological aspects. Med Oral Patol Oral Cir Bucal. 2010;15:e479–82. doi: 10.4317/medoral.15.e479. [DOI] [PubMed] [Google Scholar]
- 18.Guna SM, Ponnudurai A. Langerhans cell histiocytosis involving maxilla and mandible. J Dent, Tehran University of Medical Sciences. 2009;6:97–101. [Google Scholar]
- 19.Jindal SK, Sheikh S, Singla A, Puri N. Role of Radiology in Central Hemangioma of jaws. J Clin Exp Dent. 2010;2:e76–8. [Google Scholar]


