Abstract
Aim:
The present study was conducted to determine and compare the shear bond strengths of Conventional glass ionomer; Resin-modified glass ionomer; Polyacid-modified composite and Composite Resin, and to assess and determine the mode of failure (adhesive, cohesive, mixed).
Materials and Methods:
Occlusal dentin of 40 extracted human teeth were randomly divided into four groups of ten teeth, each based on the restorative materials tested as follows: Group I: Conventional Glass Ionomer Cement (Control); Group II: Resin-modified Glass Ionomer Cement; Group III: Polyacid-modified Composite Resin; Group IV: Hybrid Composite Resin. The bonded materials were subjected to shear bond strength (SBS) testing in a Instron Universal Testing Machine (UTM) at a crosshead speed of 0.5 mm/min. The bond failure location was examined by the use of a stereomicroscope at 10× magnification. The mean SBS of Groups I–IV obtained was 3.81, 9.71, 11.96 and 18.16 MPa, respectively. Comparison of mean shear bond strengths of all groups was done by one way ANOVA test and comparison of means in between groups by the Student's t test.
Conclusion:
It is concluded that the compomer restorative materials show higher shear bond strength than conventional glass-ionomer and resin-modified glass-ionomer, but less than composite resin.
Keywords: Composite resin, glass ionomer cements, shear bond strength
Introduction
Wilson and Kent in 1972 have introduced Glass Ionomer Cement into dentistry which had certain inherent physical and chemical properties such as physicochemical bonding to enamel and dentin, biocompatibility with pulp and anticariogenecity.[1] The disadvantages of conventional glass ionomer cements like brittleness, lack of strength, toughness and poor resistance to wear led to introduction of resin-modified glass ionomer restorative materials in 1990s and compomer or polyacid – modified composite resin, which is a single component material with the advantages of both composites and glass ionomers. The next adhesive material of choice is the composite resin, which is retained by micromechanical bonding to etched enamel or conditioned dentin.
Normal tooth structure transfers external biting loads through enamel into dentin as compression that are distributed over a large internal volume of tooth structure and thus local stresses are lower. A restored tooth tends to transfer stress differently than an intact tooth. Any force on the restoration produces compression, tension or shear along the tooth/restoration interface,[2] leading to complex stress distributions; a combination of compressive, tensile and shear stresses. Since the process of mastication is one of indentation, basically related to shearing phenomenon, the true nature of adhesive strength of the materials at the interface is depicted by the shear bond strength. The quality and efficacy of bonding of these adhesive materials is reflected in their mode of failure – either cohesive, adhesive or mixed. The number of cohesive failures within the dentinal substrates increases with increasing bond strengths.[3]
This present study was thus undertaken to determine and compare the shear bond strengths of Conventional glass ionomer (Fuji IX GP), Resin-modified glass ionomer (Fuji II LC), Polyacid-modified composite resin (Compoglass – F), Composite Resin (Z-250), and to assess and determine the mode of failure (adhesive, cohesive, mixed) exhibited by all the materials after debonding.
Materials and Methods
Forty caries free human permanent molars extracted for periodontal reasons were obtained, thoroughly cleaned of soft tissue debris, calculus and stored in distilled water till further use. They were embedded in self-cure acrylic resin with the help of aluminum molds of 1.5 cm × 1.5 cm × 5 cm such that the occlusal surfaces were parallel to acrylic resin block surface. The occlusal surfaces were made flat with a double-faced diamond disk until a clean dentinal surface was exposed. The prepared dentin surfaces were then polished with 180, 320, and 600 grit wet silicon carbide paper to simulate the production of a smear layer. All the prepared specimens were then stored in distilled water for 24 h at 37°C and were then randomly divided into four groups of ten teeth each based on the restorative materials tested as follows [Figure 1]:
Figure 1.

Restorative materials used in the study
Group I: Conventional Glass Ionomer Cement - Fuji IX GP - Control
Group II: Resin-modified Glass Ionomer Cement – Fuji II LC
Group III: Polyacid-modified Composite Resin – Compoglass F
Group IV: Hybrid Composite Resin – Z – 250
A Teflon mold was used to bond the restorative materials as follows: [Figure 2]
Figure 2.

Teflon mold used with sample in place to bond the restorative materials
Group I
The occlusal dentin was conditioned with 20% polyacrylic acid for 10 s, washed off with water for 10 s and blotted dry with the help of cotton pellets. Conventional Glass Ionomer cement was mixed according to manufacturer's directions and transferred to the properly oriented mold, condensed with the help of titanium-coated instrument and stainless steel condenser onto the dentin surface. Positive condensation pressure was applied with a Mylar strip for 4–5 min until the material has set.
Group II
The occlusal dentin was conditioned similar to Group I. The Resin Modified Glass Ionomer cement was manipulated according to manufacturer's directions and applied to the stabilized tooth similar to Group I and subjected to visible light curing for 20 s. The surface of the set cement was protected by application of two coats of varnish for Groups I and II.
Group III
The occlusal dentin was etched with 37% ortho phosphoric acid for 15 s rinsed for 10 s with water and blotted dry with the help of cotton pellets. Prime and Bond NT bonding agent was applied on to the surface and light cured for 10 s. The mounted teeth were then positioned in the stabilizing device with Teflon mold. The compomer restorative material was dispensed with the help of gun – tip placed into the mold, positive pressure applied with Mylar matrix and subjected to visible light curing for 40 s.
Group IV
The occlusal dentin was etched with 37% orthophosphoric acid for 15 s rinsed with water for 10 s and blotted dried with the help of cotton pellets. Two coats Adper Single Bond was applied with the help of a fully saturated disposable brush tip, dried for 2–5 s with air blast and light cured for 10 s each, hybrid composite resin (Z-250) was dispensed and condensed onto the dentin held in position by Teflon mold, subjected to visible light curing for 20 s.
The cured restorative materials were pushed out of the Teflon mold with a ball burnisher.
All the forty specimens were then stored in distilled water for 24 h at 37°C and then subjected to shear bond strength testing in a Universal Testing Machine (UTM) [Figure 3] at a crosshead speed of 0.5 mm/min, calculated as ratio of maximum load recorded at failure in Newtons to surface area of the bonded cylinders in square mm.
Figure 3.
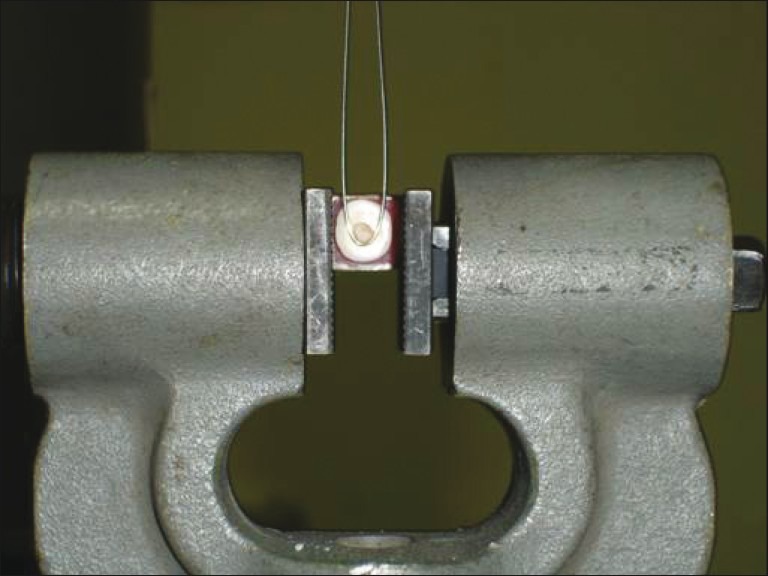
Sample in UTM during shear bond strength testing
The specimens of all groups were examined by the use of a stereomicroscope at 10× magnification to define the location of the bond failure, categorized as [Figures 4–7]:
Figure 4.
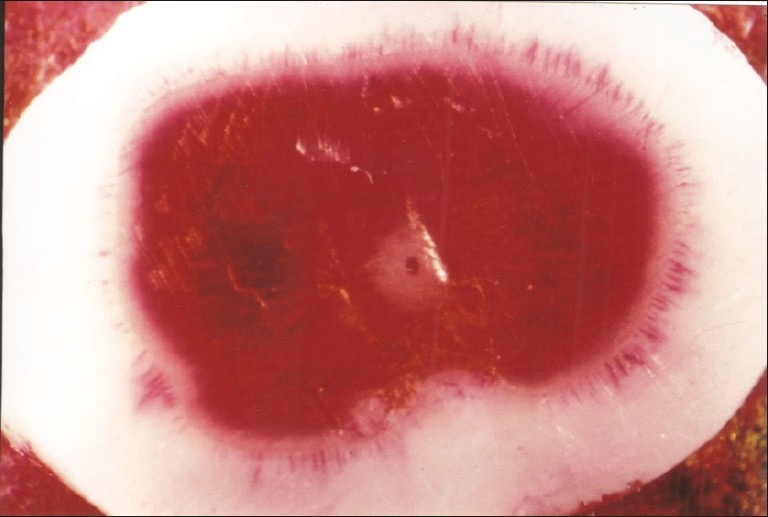
Adhesive failure
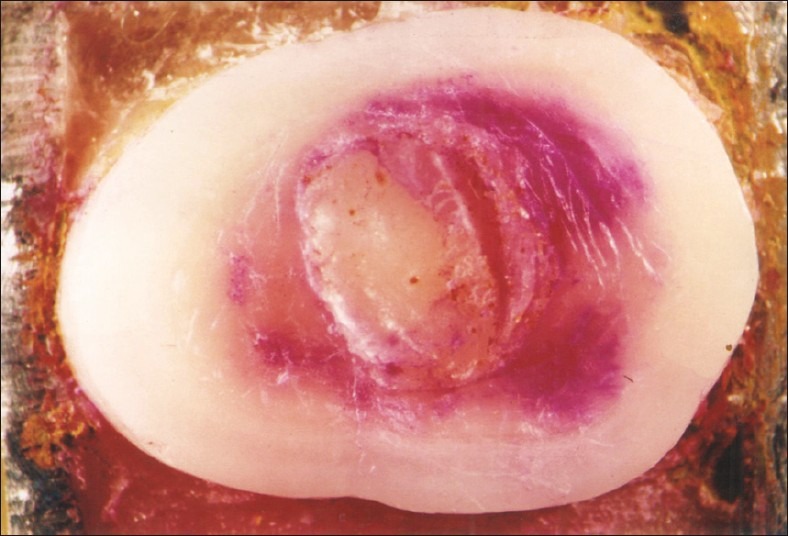
Figure 7.

Mixed failure
Figure 5.

Cohesive failure-dentin
Figure 6.
Cohesive failure within material
Adhesive failure: Occurring purely at restoration – dentin interface
Cohesive failure: Occurring purely within the material or purely within dentin
Mixed failure: Combination of the adhesive or any of the cohesive modes.
The results were as follows:[Table 1]:
Table 1.
Mean shear bond strengths (SBSs) of Groups I–IV
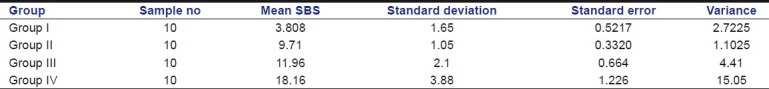
Group – I (Control)
The shear bond strengths for Group I (Fuji IX GP) ranged from 1.87 to 7.63 MPa with mean shear bond strength of 3.81 MPa.
Group II
The shear bond strength for Group II (Fuji II LC) ranged from 7.56 to 11.4 MPa with mean shear bond strength of 9.71 MPa, which was significantly higher than Group I and less than Group IV. Their difference in the mean shear bond strengths of Group II and III was not statistically significant.
Group III
The shear bond strengths of Group III (Compoglass F / Prime and Bond NT) ranged from 9.25 to 14.7 MPa with a mean of 11.96 MPa, which was found to be significantly less than group IV.
Group IV
The shear bond strengths of Group IV (Z – 250 / Adper single Bond) ranged from 11.5 to 21.9 MPa with a mean of 18.16 MPa, which was the highest of all groups and showed a statistically significant difference from Groups I, II and III.
Comparison of mean shear bond strengths of all groups was done by one way ANOVA test and comparison of means in between groups was done by Student's ‘t’ test [Tables 2 and 3].
Table 2.
ANOVA Table
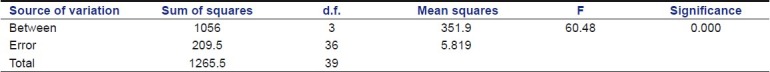
Table 3.
t-Test
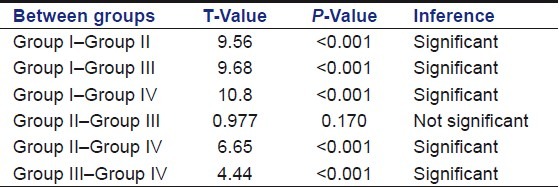
The analysis of results with ‘t’ test at 5% (0.0.5) level of significance revealed that all the groups exhibited statistically significant difference with each other except Groups II and III, which were statistically insignificant where P>0.05.
Failure mode of the all the specimens of Groups I, II, III, and IV under stereomicroscope revealed:
-
4.
Cohesive fracture within the restorative material of all the specimens of Group I
-
5.
Groups II and III specimens exhibited both adhesive and mixed failure. Of the mixed failure, Group II showed failure within the material, whereas Group III failed cohesively within dentin.
-
6.
Group IV exhibited predominantly mixed failure, which was mainly cohesive within dentin.
Discussion
Bond strength values are gross assessing tools for evaluating the efficacy of bonding restorative materials to dentin. Of the various tests, the shear bond strength is less technique sensitive to perform, highlighting the strength at the bonded interface.
The shear bond strengths of conventional glass ionomer cements obtained was 3.81 MPa.[4] The mode of failure recorded in the present study for conventional glass ionomer specimens was cohesive, which suggests that the values obtained were not the exact strength of the bonded interface but the strength of the material. Attempts to increase the strength of the material may lead to increased bond strength values.
The mean shear bond strength of Fuji II LC recorded was 9.71 MPa. The mode of failure recorded was predominantly mixed (cohesive within the material), which indicates that the values obtained were not clearly the strength of the bonded interface but due to inherent weakness of the material.[5–9]
The mean shear bond strengths of light-cured hybrid ionomer (RMGIC) materials are significantly (at least three times) higher than that of Conventional Glass Ionomer materials, which is due to the presence of light-activated resin component hydroxyethyl methacrylate (HEMA) with its superior wetting ability.[4,8,10–12] Conditioning of the dentin surface with polyacrylic acid results in removal of smear layer from surface and intertubular plugs and demineralizes the surface dentin. The HEMA of hybrid ionomers thus penetrates the exposed collagen network resulting in a small layer for micromechanical retention at the interface. The adsorption of a thin, strong polymer layer on dentin in glass ionomers was observed, which may be more rapid with the light-cured materials and also ion exchanges between the glass ionomers and dentin at their interface.[7] The improved adhesion values may also be because of the slowness of acid–base reaction, which makes the polyacid available for longer periods thus resulting in higher bond strengths.
The higher bond strength values obtained for Compomer (11.96 MPa) compared to Resin-modified Glass Ionomers could be explained by the etching of dentin that resulted in demineralized dentin with collagen network that is penetrated by the bonding agent, hybrid layer formation to form a micro mechanical bond.[13] The mean shear bond strengths obtained could be improved when better bonding systems are used along with the compomer materials, thus improvements in either the material or bonding systems can result in improved bond strengths.[14]
The bond strength of composite was greater than that of the compomer tested.[15] Though self-etching premiers (generation bonding systems) are in wide use, fifth generation bonding system has been used in the present study to bond hybrid composite resin as adhesive systems involving phosphoric acid etching were more dependable than self-etching adhesives when bonding resin composites.[16] Stereomicroscopic examination of the bonded interface after debonding revealed an adhesive failure as well as cohesive failure in dentine, which reveals that the value obtained is of the adhesive bond formed at the interface. The increased strength obtained due to both acid etching as well as that of the hybrid composite have resulted in pulling out of dentin resulting in a cohesive failure in dentin.
A restoration should thus be strong enough both adhesively and cohesively to counteract the forces of mastication acting on the tooth as well as the restoration. The present study revealed three types of failure modes – an adhesive failure, a cohesive failure (within material and dentin) and mixed failure. Clinically, it should be a restoration fail then the cohesive failure within the material that would be desirable as it leaves the tooth structure undisturbed for further preparation or removal of secondary caries as the situation demands. A cohesive failure within dentin causes damage to the intact tooth structure resulting in loss of sound tooth structure along with the restorative material. In the present study, the cohesive failure within material exhibited by Group I (Fuji IX GP) could be considered favorable compared to Group IV (Hybrid composite resin), which is the least desirable in clinical situations.
Conclusion
The results of the present study are of an in vitro study. The dentin – restorative material bond strength testing be done in conditions simulating in vivo but the complex intraoral environment prevents duplication of in vitro conditions. The in vitro information cannot be extrapolated directly to clinical situations. It has to be considered along with other evaluations to predict the performance of the materials tested. To date, no single testing condition in vitro has proven superior over other. Though there is no clear correlation between in vitro and in vivo retention, it can be assumed that if a restorative material exhibits lower bond strength under ideal laboratory test conditions, it is very likely that it may not be retained successfully in the oral environment and thus additional need for retention be thought of when applying clinically.
Acknowledgments
We thank DMRL, Hyderabad, for their help and support in testing the samples in Instron Universal Testing Machine.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Lacefield WR, Reindl MC, Retief DH. Tensile bond strength of glass-ionomer cement. J Prosth Dent. 1985;53:194–8. doi: 10.1016/0022-3913(85)90108-8. [DOI] [PubMed] [Google Scholar]
- 2.Mahler DB, Terkla LC. Analysis of stress in dental structures” DCNA: Symposium on dental materials. Philadelphia: WB Saunders; 1958. [Google Scholar]
- 3.Hagesawa T. Laboratory evaluation of experimental restorative systems containing 4-META. Am J Dent. 1994;7:212–6. [PubMed] [Google Scholar]
- 4.Burgers J, Norling B, Summit J. Resin Ionomer restorative materials: The New Generation. J Esthet Dent. 1994;6:207–15. doi: 10.1111/j.1708-8240.1994.tb00861.x. [DOI] [PubMed] [Google Scholar]
- 5.Mitra SB. Adhesion to dentin and physical properties of a light cured glass ionomer liner / base. J Dent Res. 1991;70:72–4. doi: 10.1177/00220345910700011201. [DOI] [PubMed] [Google Scholar]
- 6.Triana R, Prado C, Garro J, García-Godoy F. Dentin bond strength of fluoride releasing materials. Am J Dent. 1994;7:252–4. [PubMed] [Google Scholar]
- 7.Swift EJ, Jr, Pawlus MA, Vargas MA. Shear bond strengths of resin modified glass ionomers restorative materials. Oper Dent. 1995;20:138–43. [PubMed] [Google Scholar]
- 8.Fritz UB, Finger WJ, Uno S. Resin – modified glass ionomer cements: Bonding to enamel and dentin. Dent Mater. 1996;12:161–6. doi: 10.1016/s0109-5641(96)80015-7. [DOI] [PubMed] [Google Scholar]
- 9.McCaghren RA, Retief DH, Bradley EL, Denys FR. Shear bond strength of Light cured Ionomer to Enamel and Dentin. J Dent Res. 1990;69:40–5. doi: 10.1177/00220345900690010601. [DOI] [PubMed] [Google Scholar]
- 10.Burgess JO, Burkett L. Shear bond strength of four glass ionomers to enamel and dentin. J Dent Res. 1993;72 Abstract 2276:388. [Google Scholar]
- 11.Friedl KH, Powers JM, Hiller KA. Influence of difference factors on bond strength of Hybrid Ionomers. Oper Dent. 1995;20:74–80. [PubMed] [Google Scholar]
- 12.Kim Y, Hirano S, Hirasawa T. Physical properties of Resin Modified Glass Ionomers. Dent Mater J. 1998;17:68–76. doi: 10.4012/dmj.17.68. [DOI] [PubMed] [Google Scholar]
- 13.Glasspoole EA, Erickson RL, Davidson CL. Effect of enamel pretreatment on bond strength of compomer. Dent Mater. 2001;17:402–8. doi: 10.1016/s0109-5641(00)00098-1. [DOI] [PubMed] [Google Scholar]
- 14.Price RB, Hall GC. Invitro comparison of 10 minute versus 24 hrs shear bond strengths of six dentin bonding systems. Quintessence Int. 1999;30:122–134. [PubMed] [Google Scholar]
- 15.Jumlongrass D, White GE. Bond Strengths of composite resin and compomers in primary and permanent teeth. J Clin Ped Dent. 1997;21:223–9. [PubMed] [Google Scholar]
- 16.Goracci C, Bertelli E, Ferrari M. Bonding to worn or fractured incisal edges: Shear bond strength of new adhesive systems. Quintessence Int. 2004;35:21–7. [PubMed] [Google Scholar]


