Abstract
The peripheral giant cell granuloma (PGCG) is a reactive exophytic lesion of the gingiva and alveolar ridge that usually occurs as a result of local irritating factors such as plaque, calculus, chronic infections, chronic irritation, tooth extraction, improperly finished fillings, unstable dental prosthesis, and impacted food which originates from the periosteum or periodontal ligament. This article presents management of an unusual PGCG located on the partially edentulous mandible.
Keywords: Chronic irritation, excision, exophytic growth, food impaction, peripheral giant cell granuloma
Introduction
The peripheral giant cell granuloma (PGCG), also known as a giant-cell epulis, giant-cell reparative granuloma, osteoclastoma, or giant-cell hyperplasia, is a reactive exophytic lesion of gingiva and alveolar ridge which originates from the periosteum or periodontal ligament.[1,2] The lesion can develop at any age, though it is more common between the fifth and sixth decades of life, and shows a slight female predilection.[3,4] Even though there is no clear evident etiology, it is thought that it may be due to plaque, calculus, constant trauma, tooth extraction, overhanging restorations, unstable dental prosthesis, chronic infections, and food impaction.[5–8] Clinical appearance of PGCGs can present as polyploidy or nodular lesions, primarily bluish red with a smooth shiny or mamillated surface, stalky or sessile base, small and well demarcated.[9,10] Histological features of PGCG reveal a non-capsulated mass of tissue containing a large number of young connective tissue cells and multinucleated giant cells. Hemorrhage, hemosiderin, inflammatory cells, and newly formed bone or calcified material may also be seen throughout the cellular connective tissue.[1,11] PGCG is a soft tissue lesion that infrequently affects the underlying bone, although the latter may undergo superficial erosion.[8,12] The PGCG may cause underlying bone resorption and less commonly underlying teeth. These lesions are not painful unless they are traumatized.
Case Report
A 65-year-old man was referred to Narayana Dental College & Hospital, Nellore, had an intraoral swelling on partially edentulous mandibular alveolar ridge extending from mesial aspect of right mandibular canine region to distal aspect of left mandibular second premolar region, measuring 6 × 5 × 5 cm [Figures 1 and 2]. The patient had noticed the lesion 2 years back and it gradually increased in size. The lesion was well-defined, sessile, hyperplastic, exophytic growth, and normal in color with bluish red tinge on the entire surface of the lesion. On palpation, the lesion was non-tender, soft in consistency extending to the floor of the mouth lingually and into the buccal vestibule buccally. Orthopantomograph [Figure 3] and occlusal view [Figure 4] revealed that there is no bony involvement of the lesion and family history of the patient was non-contributory. Extraoral findings were absent. After thorough clinical and radiological examination, it was decided to perform incisional biopsy due to the extensive size of the lesion and expected wound management complication. During biopsy, it was noted that the lesion bled profusely, which was controlled by physical pressure. The specimen was sent for histopathological examination after the incisional biopsy.
Figure 1.

Intraoral swelling – facial view
Figure 2.

Intraoral swelling – occlusal view
Figure 3.
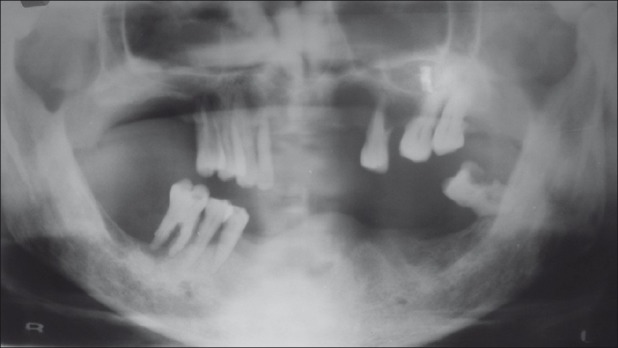
OPG showing no evidence of bone involvement
Figure 4.
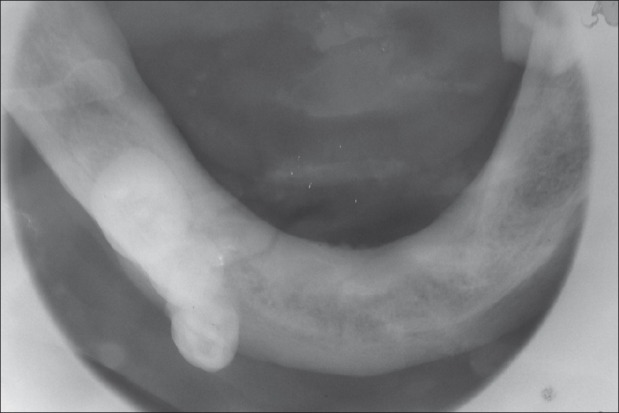
Occlusal radiograph showing no evidence of bone involvement
As the lesion was exophytic and hyperplastic in nature, differential diagnosis includes central giant cell granuloma and fibroma.[10,13] Due to extravasated deoxygenated erythrocytes at the periphery and various amounts of hemosiderin pigment, the mucosa appeared bluish red to pale pink. So, the differential diagnosis also includes hemangioma, lymphangioma, metastatic tumors of gingiva, nevi, other nodular melanomas, PGCG, and other inflammatory hyperplastic lesions.[14] Even though the lesion was exophytic in nature, absence of ossification did not support the central giant cell granuloma and presence of vascularity did not support the fibroma. Most hemangiomas are present since birth, whereas the present lesion was of relatively recent onset. Absence of a history of primary tumor elsewhere and absence of uneven bone destruction under the exophytic lesion ruled out the chance of possible metastasis to gingiva. Oral nevi and nodular melanomas occur less frequently and almost all cases are firmer on the palpation. Except for the amelanotic varieties, they are usually dark. Finally, a nodular melanoma has a history of rapid growth. In contrast, the present lesion was bluish red to pale pink in color and slowly progressing in nature. Soft to firm consistency, bluish red color, slow-growing nature, recent in onset, location on the gingiva and residual alveolar ridge, presence of vascularity, hyperplastic and exophytic growth clinically supports inflammatory hyperplastic lesions. But the presence of excess number of disseminated giant cells in connective tissue stroma along with hemorrhage, hemosiderin pigment, and inflammatory cells [Figures 5 and 6] in histological examination excludes other inflammatory hyperplastic lesions and confirms PGCG.[13,15]
Figure 5.
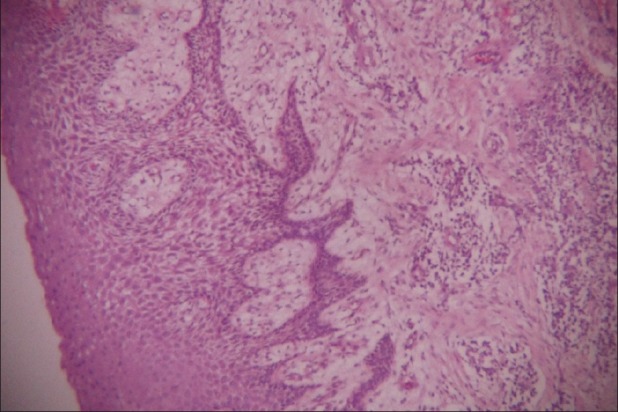
Histopathological view of lesion (hematoxylin and eosin X40)
Figure 6.
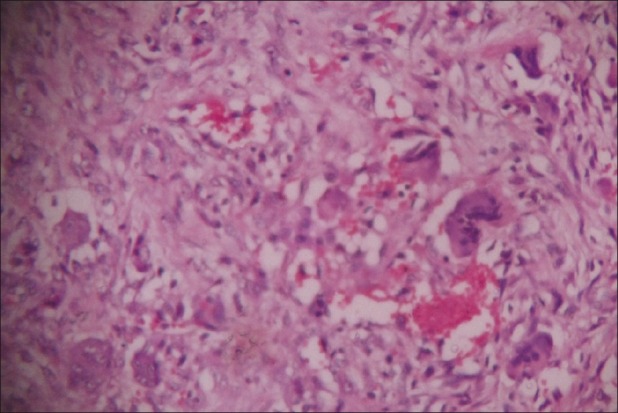
Histopathological view of lesion (hematoxylin and eosin X200)
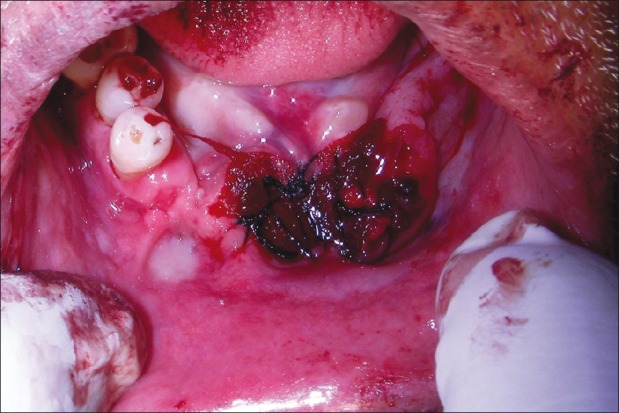
After arriving to diagnosis as PGCG, the lesion was excised [Figure 7] and four interrupted sutures were placed [Figure 8] to close the defect. While performing excision procedure, the lesion bled profusely. There were four prominent blood vessels that were originated from the base of the above mentioned swelling and were bleeding incessantly. The lesion was cauterized to achieve hemostasis since they are very close to bone and inaccessible to ligate.
Figure 7.

Excised specimen
Figure 8.
Intraoral view after excision with sutures
Discussion
PGCG is uncommon benign hyperplastic lesion of the oral mucosa which originates from the gingiva or mucoperiosteum of alveolar bone and is caused by local irritation and chronic trauma. PGCG is more common in mandible than in the maxilla and common in anterior region than posterior region. Clinically, PGCG is smooth, nodular brown, red or bluish nodule which is sessile or pedunculated.[1,2] Generally, PGCG size varies from 0.5 to 1.5 cm in diameter. Very few cases of 5 cm diameter PGCG were also reported in literature in which poor oral hygiene and food impaction are the major etiological factors in the lesion growth.[7,8] As of our knowledge, this is the first case report in which the lesion size (6 × 5 × 5 cm) exceeded 5 cm in diameter and confusing. Histopathologic characteristics of PGCG may be consistent with periodontal ligament or periosteum origin.[1,2] Histologically, PGCG is identified as a non-capsulated mass of tissue consisting of reticular and fibrillar connective tissue containing young connective tissue cells of ovoid or fusiform shape and multinuclear giant cells. The distinctive feature of PGCG is distinctive mainly due to excess number of giant cells that are disseminated in the connective tissue stroma.[8,10] The exact basis of giant cells is uncertain. Many opinions have been identified in the literature as osteoblasts, phagocytes, endothelial cells, and spindle cells are thought to be responsible for giant cell proliferation.[3] In our present case report, it could be because of chronic irritation and food impaction. Abnormal occlusal forces due to many missing teeth might have created tissue irritation on the areas of residual alveolar ridge. This might be an irritant factor for PGCG development. This could be further substantiated by food impaction. Dental resorption is extremely rare. Only two cases have been reported in literature.[16] In our case report, dental resorption is not observed since it is located on the edentulous ridge. The radiographic examination generally has no findings since it is confined to soft tissue without involving the bone. Because of the recurrence rate, approximately 10 to 15%, close follow-up is indicated.[3] Patient was reevaluated after 2 years [Figure 9] and 4 years [Figure 10] which is in line with recommendation discussed by and Nedir R et al.,[17] and there were no complaints or recurrence.
Figure 9.

Intraoral view during 2-year follow-up visit
Figure 10.

Intraoral view during 4-year follow-up visit
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Katsikeris N, Kakarantza-Angelopoulou E, Angelopoulos AP. Peripheral giant cell granuloma: Clinicopathologic study of 224 new cases and review of 956 reported cases. Int J Oral Maxillofac Surg. 1988;17:94–9. doi: 10.1016/s0901-5027(88)80158-9. [DOI] [PubMed] [Google Scholar]
- 2.Bodner L, Peist M, Gatot A, Fliss DM. Growth potential of peripheral giant cell granuloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:548–51. doi: 10.1016/s1079-2104(97)90118-9. [DOI] [PubMed] [Google Scholar]
- 3.Shafer WG, Hine MK, Levy BM. A textbook of oral pathol. 6th ed. Philadelphia: WB Saunders; 2009. pp. 130–2. [Google Scholar]
- 4.Motamedi MH, Eshghyar N, Jafari SM, Lassemi E, Navi F, Abbas FM, et al. Peripheral and cen-tral giant cell granulomas of the jaws: A demographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e39–43. doi: 10.1016/j.tripleo.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Anneroth G, Sigurdson A. Hyperplastic lesions of the gingi-va and alveolar mucosa. A study of 175 cases. Acta Odontol Scand. 1983;1:75–86. doi: 10.3109/00016358309162306. [DOI] [PubMed] [Google Scholar]
- 6.Grand E, Burgener E, Samson J, Lombardi T. Post-trau-matic development of a peripheral giant cell granuloma in a child. Dental Traumatol. 2008;24:124–26. doi: 10.1111/j.1600-9657.2006.00504.x. [DOI] [PubMed] [Google Scholar]
- 7.Kfir Y, Buchner A, Hansen LS. Reactive lesions of the gin-giva. A clinicopathological study of 741 cases. J Periodontol. 1980;51:655–61. doi: 10.1902/jop.1980.51.11.655. [DOI] [PubMed] [Google Scholar]
- 8.Etoz OA, Demirbas AE, Bulbul M, Akay E. The peripheral giant cell granuloma in edentulous patients. Report of three unique cases. Eur J Dent. 2010;4:329–33. [PMC free article] [PubMed] [Google Scholar]
- 9.Chaparro-Avendano Av, Berini-Aytes L, Escoda C Gay. Peripheral giant cell granuloma. A report of five cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2005;10:48–7. [PubMed] [Google Scholar]
- 10.Bansal P, Rohatgi S, Agnihothri A, Guptha A. Non – syndromic multiple impacted supernumerary teeth with peripheral giant cell granuloma. Contemp Clin Dent. 2011;2:41–4. doi: 10.4103/0976-237X.79309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gandara JM, Pacheco JL, Gándara P, Blanco A, García A, Madriñán P, et al. Granuloma periférico de célu-las gigantes. Revisión de 13 casos clínicos. Medicina Oral. 2002;7:254–9. [Google Scholar]
- 12.Flaitz CM. Peripheral giant cell granuloma: a potentially aggressive lesion in children. Pediatr Dent. 2000;22:232–3. [PubMed] [Google Scholar]
- 13.Wood NK, Goaz PW. Peripheral oral exophytic lesions. In: Wood NK, Goaz PW, editors. Text book of Differential diagnosis of oral and maxillofacial regions. 5th ed. St. Louis: Elsevier; 2006. pp. 141–2. [Google Scholar]
- 14.Wood NK, Goaz PW, Sawyer DR, editors. Text book of Differential diagnosis of oral and maxillofacial regions. 5th ed. St. Louis: Elsevier; 2006. Intraoral brown and bluish or black conditions; pp. 195–6. [Google Scholar]
- 15.Priddy RW. Inflammatory hyperplasias of the oral mucosa. J Can Dent Assoc. 1992;58:311–21. [PubMed] [Google Scholar]
- 16.Amler MH. Peripheral giant cell granuloma. NY State Dent J. 1992;58:38–9. [PubMed] [Google Scholar]
- 17.Nedir R, Lombardi T, Samson J. Recurrent peripheral giant cell granuloma associated with cervical resorption. J Periodontol. 1997;68:381–4. doi: 10.1902/jop.1997.68.4.381. [DOI] [PubMed] [Google Scholar]


