Abstract
Objective
A core feature of e-prescribing is the electronic exchange of prescription data between physician practices and pharmacies, which can potentially improve the efficiency of the prescribing process and reduce medication errors. Barriers to implementing this feature exist, but they are not well understood. This study's objectives were to explore recent physician practice and pharmacy experiences with electronic transmission of new prescriptions and renewals, and identify facilitators of and barriers to effective electronic transmission and pharmacy e-prescription processing.
Design
Qualitative analysis of 114 telephone interviews conducted with representatives from 97 organizations between February and September 2010, including 24 physician practices, 48 community pharmacies, and three mail-order pharmacies actively transmitting or receiving e-prescriptions via Surescripts.
Results
Practices and pharmacies generally were satisfied with electronic transmission of new prescriptions but reported that the electronic renewal process was used inconsistently, resulting in inefficient workarounds for both parties. Practice communications with mail-order pharmacies were less likely to be electronic than with community pharmacies because of underlying transmission network and computer system limitations. While e-prescribing reduced manual prescription entry, pharmacy staff frequently had to complete or edit certain fields, particularly drug name and patient instructions.
Conclusions
Electronic transmission of new prescriptions has matured. Changes in technical standards and system design and more targeted physician and pharmacy training may be needed to address barriers to e-renewals, mail-order pharmacy connectivity, and pharmacy processing of e-prescriptions.
Keywords: Electronic prescribing, e-prescribing, CPOE, clinical pharmacy information systems, community pharmacies, electronic health records, EMR, EHR
Introduction
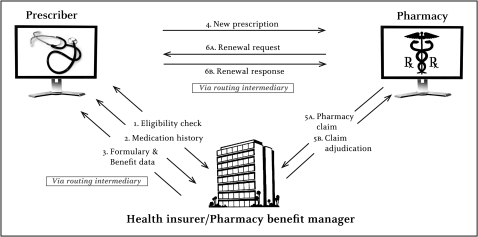
Physician use of electronic prescribing (e-prescribing) systems to generate legible and complete prescriptions could potentially reduce medication errors and improve physician practice and pharmacy efficiency by mitigating pharmacists' need for clarification.1 Another important e-prescribing feature is the two-way electronic exchange of prescription data between physicians and pharmacies. Physicians can transmit new prescriptions directly from their e-prescribing systems into pharmacy information systems as well as respond to pharmacies' electronic renewal authorization requests once medication refills are exhausted (see box 1 and figure 1).
Box 1. Electronic prescription transmission.
When physician practices and pharmacies use the e-prescribing routing features of their computer systems, the prescription data are transmitted as follows (see figure 1):
New prescriptions
Once a physician completes a new prescription and selects the option to send it electronically, it is transmitted through the e-prescribing vendor to the electronic prescription routing intermediary's network. From there, the prescription is typically routed through the pharmacy system vendor or the pharmacy's central corporate server to the chosen pharmacy location. Staff are alerted to the e-prescription arrival on the pharmacy system's display screen, for example, with an icon or new work log entry, and the prescription is opened in the work queue for processing. If the pharmacy does not accept e-prescriptions, the intermediary converts the prescription to a fax.
Renewals
Once refills are exhausted, at the request of the patient, the pharmacy sends an electronic renewal authorization request—also known to users as a ‘refill’ request—to physicians for approval. The renewal authorization request is logged into the pharmacy and practice system message queues pending approval. The physician reviews the request and has three options: (1) to approve it as transmitted; (2) to make changes to a limited number of fields, such as number of refills; or (3) to deny it. Authorization is sent back to the pharmacy as a new prescription that is linked to the old prescription by a unique identifying code. This linkage allows the pharmacy system to auto-populate the necessary data from the existing prescription. If the physician denies the request, the physician typically selects a reason, such as ‘following with a new prescription’ for a change in dosage or to make other substantial prescription modifications. The new prescription references the prescription number of the denied request to allow the pharmacy staff to delete the initial renewal request. Alternatively, the physician can initiate an e-renewal, in which case the pharmacist handles the renewal as a new prescription.
Figure 1.
E-prescribing information exchange. Source: adapted from Bell DS, Straus SG, Belson D, et al. A toolset for e-prescribing implementation in physician offices; figure 2.1 (prepared by RAND Corporation under contract no. HHSA 290-2006-00017, TO #4, AHRQ publication no. 11-0102-EF). Rockville, MD: Agency for Healthcare Research and Quality, 2011 (in press).
Although research on the effects of electronic transmission is limited, physicians appear to save time, primarily from electronic renewals.2 3 Moreover, electronic transmission of both new prescriptions and renewals has the potential to streamline workflow for other practice and pharmacy staff and minimize interruptions from phone and fax communications.2–7 Pharmacy staff also may save time processing prescriptions that do not have to be entered manually.7–9 Reducing manual entry has the potential to lower the rate of prescription errors as well.7 10–12
Despite these and other potential e-prescribing benefits, e-prescription volume has been low, although it is growing as physicians respond to Federal financial incentive programs.13 14 Medicare began paying bonuses to qualifying physicians using electronic health record (EHR) or stand-alone e-prescribing systems under the Medicare Electronic Prescribing Incentive Program in 2009. Physicians can qualify for substantially larger payments through the Medicare and Medicaid Electronic Health Records Incentive Programs (EHR Incentive Programs), starting in 2011. To receive incentives, physicians must fulfill requirements to demonstrate that they are meaningful users of certified EHRs, including generating and transmitting more than 40% of all prescriptions to pharmacies electronically, excluding prescriptions for controlled substances. This threshold is expected to rise as program requirements become more stringent.15 E-prescribing volume likely will grow further as new standards are implemented to support e-prescribing of controlled substances.
To maximize the benefits of electronic prescription transmission, including improved efficiency and reduced medication errors, both physician practice and pharmacy staff must use the feature routinely. However, not all physicians who use health information technology (IT) applications to generate prescriptions have systems that support electronic transmission of new prescriptions or renewals, and even when these features are available, physicians do not always use them.6 13 16–21 Similarly, not all community and mail-order pharmacies have the ability to receive new prescriptions electronically or to send electronic renewal requests, and even if they do, staff may not use these features routinely.8 13 Pharmacies have faced additional challenges, including delays in receiving or being alerted to new e-prescriptions, continued need to manually enter or edit prescription data, and the need to follow-up with physicians to resolve gaps, errors, or lack of clarity in e-prescriptions.7 8 10 22
Most studies that identify e-prescribing barriers are based on data from 2007 or earlier and do not explore electronic transmission in detail. This study focuses on how electronic transmission features are being used for new prescriptions and renewals, the facilitators of and barriers to use, and the effects on pharmacies' prescription processing. The study also explores strategies to support more effective use of these features. The data were collected as part of a broader qualitative research project to better understand recent experiences of physician practices and pharmacies using advanced e-prescribing features.23
Methods
Participants
Sampling frames of physician practices and community pharmacies actively using e-prescribing in 12 Community Tracking Study (CTS) sites were developed from lists of physicians and pharmacies registered with Surescripts—the dominant electronic prescription transmission network in the USA—which were obtained from the company's website. Since 1996, the CTS has monitored healthcare market changes in 12 communities through periodic site visit interviews with leaders of local healthcare organizations, including physician practices.24 CTS sites were selected to be nationally representative of metropolitan areas with populations over 200 000 (see table 1 for sites). Stratifying the sampling frame by CTS sites allowed comparisons of practice and pharmacy e-prescribing experiences within and across markets that vary by factors that may be related to e-prescribing experiences, including relative market shares of local and national pharmacies, e-prescription volume, and state e-prescribing regulations.25 26
Table 1.
Characteristics of participating physician practices
| Characteristic | Number of practices (N=24)* |
| Specialty | |
| Primary care | 16 |
| Medical or surgical specialty | 5 |
| Multispecialty | 3 |
| Number of physicians | |
| 1–9 | 12 |
| 10–49 | 7 |
| 50–500 | 5 |
| Practice ownership | |
| Physician | 17 |
| Hospital | 6 |
| Faculty practice | 1 |
| Type of e-prescribing system† | |
| Part of electronic health record system | 17 |
| Stand-alone system | 7 |
| Number of years prescriptions sent electronically | |
| <2 | 12 |
| 2+ | 12 |
| Estimated percentage of prescriptions sent electronically | |
| <70 | 6 |
| 70+ | 17 |
| Unknown | 1 |
Two practices were interviewed in each of the 12 Community Tracking Study (CTS) sites: Boston; Cleveland; Greenville, South Carolina; Indianapolis; Lansing, Michigan; Little Rock, Arkansas; Miami; northern New Jersey; Orange County, California; Phoenix; Seattle; and Syracuse, New York.
Twelve different commercial e-prescribing vendors were represented. Among the 17 practices using electronic health record systems, vendors included: Allscripts (4), eClinicalWorks (2), Epic (3), GE Centricity (2), GEMMS, McKesson, MedENT, NextGen (2), and one homegrown system. Stand-alone e-prescribing system vendors used in the remaining seven practices included: Allscripts (2), InstantDX, Prematic, RelayHealth (2) and DrFirst, which was integrated into a Greenway Medical Technologies electronic health record system.
Physician practices that participated in the CTS previously or were suggested by CTS respondents were selected purposefully from the sampling frame to vary in size, specialty, and type of e-prescribing system (EHR vs stand-alone). In each practice, the CTS contact was asked to identify an experienced physician user, and an additional respondent such as an IT manager or nurse if needed, to capture both clinical and operational perspectives on the practice's e-prescribing experiences.
Because less research exists on pharmacy e-prescribing experiences, pharmacies were oversampled relative to physician practices to support more in-depth study. The pharmacy sampling frame was stratified by local and national ownership (see table 2 for more detail). While a few national companies account for a substantial proportion of pharmacy locations in the USA, the same information system is typically used across locations, so locally owned pharmacies were oversampled to capture more variation in e-prescribing experiences. The corporate headquarters of some national companies were contacted to select pharmacy locations to participate. Other pharmacies were selected through recommendations from professional associations and physician respondents or recruited directly. In each pharmacy location, the pharmacist-in-charge was asked to participate. Other experts, including representatives of vendors, e-prescribing intermediaries, and state pharmacy associations, were identified to provide context for the user interviews.
Table 2.
Characteristics of participating community pharmacies
| Characteristic | Number of community pharmacies (N=48)* |
| Ownership | |
| Local (within state) | |
| Independent—three or fewer locations | 16 |
| Independent—regional/local chain drug store, supermarket, provider-owned, and other | 8 |
| Total | 24 |
| National (multi-state) | |
| Chain drug store | 15 |
| Supermarket | 3 |
| Mass merchant | 6 |
| Total | 24 |
| Estimated average prescriptions per week | |
| 200–750 | 11 |
| 751–1750 | 16 |
| >1750 | 16 |
| Unknown | 5 |
| Pharmacy information system | |
| Home-grown | 19 |
| Commercial vendor† | 29 |
| Number of years prescriptions received electronically | |
| <2 | 32 |
| 2+ | 13 |
| Unknown | 3 |
| Estimated percentage of prescriptions received electronically | |
| ≤5% | 15 |
| 6%–14% | 11 |
| 15%–24% | 8 |
| 25%+ | 11 |
| Unknown | 3 |
Four pharmacies were interviewed in each of the 12 Community Tracking Study (CTS) sites: Boston; Cleveland; Greenville, South Carolina; Indianapolis; Lansing, Michigan; Little Rock, Arkansas; Miami; northern New Jersey; Orange County, California; Phoenix; Seattle; and Syracuse, New York.
Thirteen different pharmacy information system vendors were represented among the 29 participating pharmacies using commercial systems, including: McKesson (including Enterprise, PharmaServ, and Condor products) (11), QS/1 (4), PDX (3), Transaction Data Systems Rx30 (2), as well as nine other vendors.
Data collection and analysis
Six researchers formed two-person teams, consisting of a lead interviewer and a note-taker, to conduct 30–60 min telephone interviews between February and September 2010. Semi-structured protocols were tailored to each respondent type and included questions on IT systems; implementation and use of e-prescribing features, including electronic routing of new prescriptions and renewals; and pharmacy processing of e-prescriptions. (See supplementary online appendix 1 for selected protocols.) Interview team members jointly reviewed the interview transcriptions for accuracy.
The six-person research team used an iterative process to develop and refine emerging themes and to ensure data saturation based on a rolling review of the transcripts. Codes were developed using the ‘integrated’ approach described by Bradley and colleagues in which a ‘start list’ is developed from the literature and then refined based on the data.27–29 The interview transcripts were coded and further analyzed by the four study authors using Atlas.ti qualitative software. Data tables were used along with the transcripts to systematically confirm and further refine themes, and weigh the evidence supporting each finding.28 The principal investigator and another researcher first summarized a small sample of transcripts in preliminary table shells developed using project themes and codes, then met to resolve discrepancies and modify the shells as needed. The two other researchers completed summaries of the remaining practice and pharmacy transcripts, respectively; all transcripts and summaries were also reviewed by the principal investigator. The authors met regularly to resolve conflicts and reach consensus on the data tables and study findings.27
Results
A total of 114 telephone interviews were conducted with representatives of 97 organizations. Twenty-four physician practices participated, two in each CTS site. Forty-eight community pharmacies also participated, divided between local and national companies, with four pharmacies per site. For each participating national chain drug store, pharmacists were interviewed at a minimum of three different locations. National respondents included representatives of three mail-order pharmacies and three chain pharmacy headquarters and 21 other experts.
Tables 1 and 2 provide more descriptive information on participating physician practices and community pharmacies, respectively. About 70% of practices used EHRs, while the remainder used stand-alone e-prescribing systems, closely representative of the national distribution of physicians registered on Surescripts in 2009.13 Practices and pharmacies used a variety of system vendors and the sample included both early and later adopters.
More than two-thirds of practices estimated they sent at least 70% of prescriptions electronically. Physicians selected other transmission modes—such as print, fax, or phone—when necessary, for example, when prescribing controlled substances, when a patient did not need a prescription filled immediately or expressed a preference for a printed prescription, or when a pharmacy was unable to receive e-prescriptions.
In contrast, more than half of community pharmacists estimated their pharmacy received <15% of prescriptions electronically, with national pharmacies more likely to receive a higher proportion. This rate was low, in part, because many physicians did not transmit any prescriptions electronically. Moreover, community pharmacies noted receiving numerous computer-generated prescriptions that were faxed or printed, sometimes outnumbering e-prescriptions.
Physician and pharmacy respondents generally noted overall satisfaction with e-prescribing and perceived improvements in efficiency and patient safety. However, respondents identified some substantial challenges to fully realizing the anticipated benefits from the transmission and processing of e-prescriptions.
Electronic transmission
New prescriptions
Most respondents expressed satisfaction with the electronic transmission of new prescriptions. Despite the complexity of prescription routing through multiple parties, respondents reported true transmission failures were rare. However, about one-third each of physician practices and community pharmacies noted that, on a daily basis, patients arrived to pick up orders before the pharmacy had received the e-prescription. Practice respondents were more likely to attribute the problem to pharmacy staff being inadequately trained to identify new e-prescriptions, with problems reportedly diminishing as pharmacy staff gained e-prescribing experience. Pharmacists, however, believed that incoming e-prescriptions were easily identified and were more likely to point to physician delays in transmitting the prescriptions or, less commonly, transmission to the wrong pharmacy. Pharmacies typically resolved transmission problems by calling physicians for verbal orders.
Prescription renewals
Physicians and community pharmacists found that the electronic renewal process was not as consistently successful as new prescription routing and was more difficult to integrate into organization workflows. Respondents, nonetheless, highlighted the time-saving advantages of the electronic renewal process when working properly. A physician respondent from a small family-medicine practice noted, ‘Previously, someone had to get the fax, distribute it, get the approval and call or fax it in…. Now the physician gets… a refill request to their inbox right away and can deny or accept it in seconds. It eliminates handoffs. So instead of 24 h, the turnaround time is an hour.’ On the pharmacy side, according to a manager of a mass-merchant pharmacy, ‘The physician sends me back the exact same everything…. The e-prescription is married to something in my system, so five keystrokes and it's ready to go.’
While both physicians and pharmacies stand to benefit from the increased efficiency of electronic renewals, more than one-quarter of the participating community pharmacies, including 11 of the 24 local pharmacies and three national pharmacies, did not send electronic renewal authorization requests. Eight of these pharmacies lacked the functionality, and the rest chose not to use the feature, mainly to avoid Surescripts transaction fees. Similarly, one-third of physician practices were not set up to receive e-renewal requests or received them infrequently.
Among practices that did receive e-renewal requests, respondents identified ways in which the renewal process broke down, resulting in inefficiencies. For example, they reported that local and national pharmacies able to receive e-prescriptions from the practice did not consistently request renewal authorizations electronically and sometimes sent multiple requests for the same prescription using different means, even after the physician had responded electronically. As one physician explained, ‘Sometimes the patient will call, the pharmacy will fax, and [send something via] Surescripts, all for the same patient, the same prescription, on the same day. That is cumbersome.’
Pharmacists explained that follow-up is necessary if physicians do not respond in a timely way, for example, within 24 h as Surescripts recommends. A pharmacist from a national pharmacy chain explained, ‘Our system automatically generates the request. If they [don't] respond, that's where we run into problems. We fax the next day because we can't send a duplicate request electronically.’ Another pharmacist noted that his system is set up to automatically resend an e-fill request every 72 h until the initial request is marked as complete.
Inconsistent pharmacy renewal request methods reinforced inconsistent modes of response from physician offices, making it more difficult for both parties to ensure that the prescription is filled and that their systems are updated. Pharmacists reported that physicians often approve electronic requests by fax or phone. They also noted that physicians often mistakenly deny the request and then send the same prescription as a new order. In contrast, multiple physician respondents noted that they typically try to respond to all renewal requests electronically, regardless of delivery mode, to capture the prescription in their e-prescribing system and to convey to the pharmacy that they are enabled for electronic renewals.
When physicians transmitted prescription renewals without responding to a pharmacy request, pharmacists typically had to enter the prescriptions as if they were new, losing efficiencies from auto-population. Both pharmacies and physician practices also had to manually update their systems' message queues, for example, by deleting any pending requests.
Mail-order pharmacy connectivity
Electronic routing for new prescriptions and renewals with mail-order pharmacies posed additional challenges, with about three-quarters of the physician practices experiencing difficulties. Many practices were not sure which mail-order pharmacies accepted e-prescriptions and believed that, even when a mail-order company did accept them, the process was unreliable. According to a nurse in one practice, ‘We are nervous about sending electronically to mail orders. The success rate isn't high…. If it doesn't go through, I will fax it. We can lose four or five days though… finding out that it never went through.’ Respondents also largely noted that renewal authorization requests from mail-order pharmacies were received only by fax. In response to these challenges, some practices first tried electronic routing for new prescriptions or renewal responses, followed by faxing or printing the prescription if unsuccessful. Others simply avoided electronic communication altogether by routinely faxing or printing all mail-order prescriptions.
Practice respondents were surprised by these challenges, expecting electronic routing to function identically for community and mail-order pharmacies. However, as mail-order pharmacy respondents explained, few e-prescribing vendors that were Surescripts-certified to e-prescribe with community pharmacies were also certified for new prescriptions with mail-order pharmacies, and even fewer were certified for mail-order renewals. As a result, while some practice respondents believed they were sending prescriptions electronically when they selected mail-order pharmacies from the e-prescribing directory, the mail-order pharmacies noted most e-prescriptions from Surescripts were delivered by fax. For the same reason, most mail-order renewal requests also were sent by fax. These connectivity barriers arose because the new Surescripts organization, formed from a merger of SureScripts and RxHub in 2008, continued to maintain two legacy transmission networks.
Some mail-order pharmacies addressed these barriers by converting all e-prescriptions to images and processing them with fax and paper prescriptions in a single workflow, while others maintained dual workflows, processing e-prescriptions separately. Since the time of the interviews, transmission network changes have been implemented to enable more e-prescribing vendors to route new prescriptions electronically to mail-order pharmacies, but changes to support e-renewals lag.
Pharmacy processing of e-prescriptions
Most pharmacies received new e-prescriptions directly into their pharmacy systems for processing. However, two mail-order pharmacies and six community pharmacies—including local and national retailers—continued to manually enter all e-prescriptions. Most of these pharmacies, though, were implementing new systems with automated processing.
The majority of the remaining pharmacies processed e-prescriptions similarly. Once the pharmacy staff were alerted to a new e-prescription and opened it, the system attempted to match the patient and physician. Staff sometimes had to manually select the correct individual from a computer-generated list of options or create a new profile.
Staff then processed each prescription element, either clicking on the information in the view screen to import it into the corresponding pharmacy system field or visually verifying the information if the field was auto-populated. Pharmacists reported that the necessary fields were typically complete in e-prescriptions, unlike paper prescriptions. When needed, pharmacy staff typed in or edited text in a field or selected an entry from computer-generated options. Three prescription fields commonly required manual manipulation—medication name, quantity, and patient instructions (also known as the Signatura or ‘Sig’).
Medication name
When physicians select a medication, the data field typically contains a single string with the drug name, strength, and dosage form, which is transmitted to the pharmacy along with the Food and Drug Administration National Drug Code (NDC). Although NDCs are used to standardize medication identification across systems using different drug-database vendors, there is no central, up-to-date source for a unique NDC for each clinically distinct drug.7 If the NDCs in the e-prescription and the pharmacy system do not match, the data cannot be auto-populated and the pharmacist must rely on the transmitted information to manually select a medication from the pharmacy database.
Moreover, both physician and pharmacist respondents explained that physicians must select medications with more specificity when e-prescribing, making decisions about packaging, drug form, or other features that commonly are made by pharmacists for hand-written prescriptions, sometimes leading to more pharmacy follow-up. In an example provided by an independent pharmacist, ‘A doctor might pick ‘minocycline tablet, 100 mg.’ He wouldn't intentionally select this because it's seven times more expensive than capsules…. In the past, the doctor would have called in simply ‘minocycline.’ I would pick ‘capsules’ in the system because I know the cost difference. When the doctor puts in ‘minocycline tablets,’ I, as a pharmacist, can't change that. I have to give what they said.’ Physician respondents confirmed this problem, as one physician in a small practice noted, ‘No longer now can I just say ‘potassium,’ I have to pick if it's a tablet, capsule, or liquid—you used to just let the pharmacist and patient deal with that.’
Physicians elaborated on the challenges in selecting the intended medication given the overwhelming number of different forms and strengths of medications available in a search query. A physician respondent observed, ‘On my preference list, there are 19 adult and pediatric dosings for amoxicillin. If you don't have a preference list, you're searching in the general database, which is an absolute nightmare. There are two full screens with 60 entries for variations on the theme of amoxicillin… and that's a good situation.’ As another example of ‘over-specification,’ physicians may have to choose from among different generic drug manufacturers. Pharmacists noted that stores stock only a limited number of manufacturers of any particular generic, making it difficult for the pharmacy system to match to the manufacturer specified in the e-prescription. Physicians and pharmacists also noted the serious problem of ‘fat fingers,’ or inadvertently selecting a drug with a similar spelling but a different clinical purpose than the intended medication.
Quantity
Pharmacists and physicians both noted that physicians face challenges accurately specifying quantities for prepackaged or multi-use medications—such as pill packs, syringes, inhalers, or creams—in e-prescriptions. E-prescribing systems typically list such medications by the container or package, rather than the individual dosing units, which can cause physician confusion in selecting the appropriate quantity. Pharmacists commented that callbacks were typically unnecessary, but staff must be trained to recognize and correct this type of problem, especially since pharmacists must specify the quantity of the active ingredient on insurance claims. Observed a pharmacist in a national chain location, ‘With inhalers, prescribers usually enter the quantity ‘1,’ if you don't change that, you'll be billing (the insurer) for 1 g but it weighs 17 g so you'll be shorting yourself. It's the same with Enbrel, an injection medication that is 3.92 g. You have the potential to lose $3000 if someone is not paying attention.’
Patient instructions
Nearly half of pharmacists noted that patient instructions typically had to be rewritten for patients to understand. As an independent pharmacist explained, ‘A lot of times we can't copy the directions word for word because the patient doesn't understand them, just like with paper prescriptions. We have to go in and erase ‘t.i.d.’ and put in, ‘One tablet three times a day’.’ While some e-prescribing systems may facilitate writing instructions in English, pharmacists indicated that, even when not in Latin, Sigs often were written for the pharmacist and needed editing to be more patient-friendly.30
About a third of pharmacists noted another challenge: the potential for physicians to provide additional instructions in another field, such as the extended instruction or comment box, that contradict what is stored in the Sig field. This sometimes prompts callbacks, as a respondent at one local chain explained, ‘We'll see ‘Take one tablet.’ Then it will say below in the notes field, ‘Take two tablets in the morning.’ It's like the first part is automatically filled in for the doctor…. We normally look in patient history…. If we see one tablet used in the past, then we keep it at one tablet; otherwise we call the physician.’ While some physicians confirmed that this problem could arise in their e-prescribing system, it is unclear how dependent this problem is on specific system designs.
Discussion
Study findings suggest that use of electronic transmission features has matured relative to earlier research, with practices and community pharmacies reporting few barriers to electronic routing and receipt of new prescriptions. However, respondent reports suggest that challenges related to e-renewals, mail-order pharmacy connectivity, and pharmacy processing of select e-prescription fields remain. These challenges likely will become more salient for physician practices and pharmacies as e-prescription volume accelerates in response to Federal incentives. In addition, some physicians may be penalized inadvertently if they are unable to meet increasing threshold requirements under the EHR Incentive Programs for the proportion of prescriptions sent electronically because of challenges associated with mail-order prescriptions. While some challenges may be mitigated as physicians and pharmacies gain more experience, structural issues underlying these challenges likely will need to be addressed directly. A broad group of public and private stakeholders, including the Federal government, the National Council for Prescription Drug Programs (NCPDP) standards setting organization, vendors, and medical informatics researchers would need to work together to help support these efforts.
Increasing e-renewal reliability and efficiency
The e-renewal process may become more predictable if pharmacies and practices with e-prescribing that are still faxing renewals discontinue this practice when the Federal exemption for computer-generated fax transmissions under the Medicare Part D program expires on January 1, 2012.31 Study findings suggest that pharmacies and practices also may benefit from explicit guidance on incorporating the e-renewal process into workflows, for example, through implementation guides, best-practice tools, and targeted education, training, and support, particularly once users have gained some e-prescribing experience.32 33 There also may be opportunities to modify or enhance underlying technical standards and physician and pharmacy system design to better support electronic communication during the renewal process, for example, providing alerts if e-prescribers do not respond to renewal responses within a specific time period or supporting standardized approaches for pharmacy follow-up requests.
Improving mail-order pharmacy connectivity
Surescripts, mail-order pharmacies, and e-prescribing vendors are working on network and system changes to increase the proportion of practices that can communicate electronically with mail-order pharmacies, and this transition could possibly accelerate with the expiration of the Federal fax exemption. Practices may benefit from direct communication about these changes and education on how to most efficiently process mail-order prescriptions and renewals in the interim and after changes are implemented.
Reducing the need for pharmacy editing of e-prescriptions
Study findings on challenges to reconciling prescription data fields between practice and pharmacy systems are consistent with other recent research.7 34 To address challenges related to drug identifiers, experts have recommended that NCPDP consider using a new technical standard, RxNorm, a standardized nomenclature for clinical drugs, in place of NDC codes as the main identifier.7 RxNorm could help reduce drug selection inefficiencies and potential errors by better conveying physicians' clinical intent without requiring them to over-specify their choice and allowing pharmacists to use that information to select the most appropriate medication. E-prescribing vendors and drug database vendors also could explore ways to enhance system interfaces and drug selection tools and promote best practices so that physicians could more easily choose among clinically appropriate options and convey the correct quantity information regardless of dosage form.
To improve the quality of patient instructions in e-prescriptions, the Structured and Codified Sig Format is being incorporated into the NCPDP SCRIPT e-prescribing transaction standards.34 Moving from free text to a structured format may allow physicians to write more complete, clinically accurate, and unambiguous Sigs. Experts recently recommended that the Format be strengthened before it is made mandatory, and suggest a solution to address the potential for conflicting Sig information under the new standard.34 Meanwhile, e-prescribing vendors could explore ways to improve system design to mitigate the existing problems with conflicting Sigs. Other expert recommendations include providing additional physician training and developing best practices to encourage physicians to send amended prescriptions to the pharmacy to avoid repeating mistakes.35–37
Supporting e-prescribing expansion
Additional research on the barriers to and facilitators of two-way electronic communication will be increasingly important as pharmacies and physician practices not only expand use of existing e-prescribing features but also seek more electronic communication tools. Technical standards to support additional two-way electronic communication between practices and pharmacies, for example, to change or cancel a prescription and for clinical queries, have been incorporated into the NCPDP SCRIPT standard or are being developed; none are yet in widespread use.38
Study limitations
Because this is a qualitative study based on a small and purposeful sample, findings cannot be statistically generalized to all physicians and pharmacies using electronic prescription routing. Moreover, because respondent identification was purposeful and participation was voluntary, the sample may have been systematically biased about e-prescribing in a positive or negative way. However, respondents typically identified both facilitators of and barriers to effective electronic routing.
Supplementary Material
Acknowledgments
We are grateful to the respondents for their willingness to share their time and insights. We would also like to thank Teresa Zayas Cabán, Jonathan White, and Terri Warholak for valuable input into the study design and earlier drafts of the paper.
Footnotes
Funding: This research was funded under contract number HHSA 290-05-0007 (03) from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services. The opinions expressed in this document are those of the authors and do not reflect the official position of AHRQ or the US Department of Health and Human Services.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.McKibbon KA, Lokker C, Handler SM, et al. Enabling Medication Management through Health Information Technology. (Prepared by the McMaster University Evidence-based Practice Center under Contract HHSA 290-2007-10060-I, AHRQ Publication No. 11-E008-EF). Rockville, MD: Agency for Healthcare Research and Quality, 2011. http://www.ahrq.gov/clinic/tp/medmgttp.htm (accessed Oct 2011). [Google Scholar]
- 2.Goldman RE, Dubéc C, Lapane KL. Beyond the basics: refills by electronic prescribing. Int J Med Inform 2010;79:507–14 [DOI] [PubMed] [Google Scholar]
- 3.Lapane KL, Rosen RK, Dubé C. Perceptions of e-prescribing efficiencies and inefficiencies in ambulatory care. Int J Med Inform 2011;80:39–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hollingworth W, Devine EB, Hansen RN, et al. The impact of e-prescribing on prescriber and staff time in ambulatory care clinics: a time motion study. J Am Med Inform Assoc 2007;14:722–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devine EB, Hollingworth W, Hansen RN, et al. Electronic prescribing at the point of care: a time–motion study in the primary care setting. Health Serv Res 2010;45:152–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DesRoches CM, Agarwal R, Angst CM, et al. Differences between integrated and stand-alone e-prescribing systems have implications for future use. Health Aff (Millwood) 2010;29:2268–77 [DOI] [PubMed] [Google Scholar]
- 7.Bell DS, O'Neill S, Reynolds K, et al. Evaluation of RxNorm in Ambulatory Electronic Prescribing. TR-941-CMS. Santa Monica, CA: Rand Corporation, 2011. http://www.rand.org/pubs/technical_reports/TR941 (accessed Oct 2011). [PMC free article] [PubMed] [Google Scholar]
- 8.Rupp MT, Warholak TL. Evaluation of e-prescribing in chain community pharmacy: best-practice recommendations. J Am Pharm Assoc (2003) 2008;48:64–70 [DOI] [PubMed] [Google Scholar]
- 9.Rupp MT. E-prescribing: the value proposition. America's Pharmacist. Alexandria, VA: National Community Pharmacists Association, 2005:23–6 [Google Scholar]
- 10.Warholak TL, Rupp MT. Analysis of community chain pharmacists' interventions on electronic prescriptions. J Am Pharm Assoc (2003) 2009;49:59–64 [DOI] [PubMed] [Google Scholar]
- 11.Knudsen P, Herborg H, Mortensen AR, et al. Preventing medication errors in community pharmacy: Frequency and seriousness of medication errors. Qual Saf Health Care 2007;16:291–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moniz TT, Seger AC, Keohane CA, et al. Addition of electronic prescription transmission to computerized prescriber order entry: effect on dispensing errors in community pharmacies. Am J Health Syst Pharm 2011;68:158–63 [DOI] [PubMed] [Google Scholar]
- 13.Surescripts Advancing Healthcare in America: 2009 National Progress Report On E-Prescribing. Surescripts LLC, 2010. http://www.surescripts.com/media/515306/2009_national-progress-report.pdf (accessed Oct 2011). [Google Scholar]
- 14.Government Accountability Office (GAO) Electronic Prescribing: CMS Should Address Inconsistencies in Its Two Incentive Programs That Encourage the Use of Health Information Technology (Publication No. GAO-11–159). Washington, DC: GAO, 2011. http://www.gao.gov/new.items/d11159.pdf (accessed Oct 2011). [Google Scholar]
- 15.HIT Policy Federal Advisory Committee Meaningful Use Workgroup Request for Comments Regarding Meaningful Use Stage 2. Washington, DC: US Department of Health and Human Services, Office of the National Coordinator for Health Information Technology, 2011. http://healthit.hhs.gov/media/faca/MU_RFC%20_2011-01-12_final.pdf (accessed Oct 2011). [Google Scholar]
- 16.Grossman JM. Even When Physicians Adopt E-prescribing, Use of Advanced Features Lags. Washington, DC: Center for Studying Health System Change, 2010. Issue Brief No. 133. [PubMed] [Google Scholar]
- 17.United States Department of Health and Human Services (DHHS), Office of Inspector General Medicare part D e-prescribing standards: Early assessment shows partial connectivity. (Report No. OEI-05-08-00320. 2009). Washington, DC: DHHS, 2009. http://oig.hhs.gov/oei/reports/oei-05-08-00320.pdf (accessed Oct 2011). [Google Scholar]
- 18.Grossman JM, Gerland A, Reed MC, et al. Physicians' experiences using commercial e-prescribing systems. Health Aff (Millwood) 2007;26:w393–404 [DOI] [PubMed] [Google Scholar]
- 19.National Opinion Research Center (NORC) at the University Of Chicago. Findings from the Evaluation of E-Prescribing Pilot Sites. (Publication No. 07-0047-EF). Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2007 [Google Scholar]
- 20.Crosson JC, Isaacson N, Lancaster D, et al. Variation in electronic prescribing implementation among twelve ambulatory practices. J Gen Intern Med 2008;23:364–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang CJ, Patel MH, Schueth AJ, et al. Perceptions of standards- based electronic prescribing systems as implemented in outpatient primary care: a physician survey. J Am Med Inform Assoc 2009;16:493–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Community Pharmacists Association (NCPA) Statement of the National Community Pharmacists Association to the HIT Policy Committee Information Exchange Workgroup hearing on “Successes and Challenges Related to E-Prescribing”. 2010. http://www.ncpanet.org/pdf/leg/eprescribing012510.pdf (accessed Oct 2011). [Google Scholar]
- 23.Grossman JM, Boukus ER, Cross DA, et al. Physician Practices, E-Prescribing and Accessing Information to Improve Prescribing Decisions. Washington, DC: Center for Studying Health System Change, 2011; Research Brief No. 20. [PubMed] [Google Scholar]
- 24.Center for Studying Health System Change CTS Site Visits [Internet]. 2011. http://www.hschange.org/index.cgi?data=06 (accessed Oct 2011). [Google Scholar]
- 25.Pritts J, Jacobson R, Connors E. Privacy and Security Solutions for Interoperable Health Information Exchange: Report on State Prescribing Laws: Implications for E-Prescribing. (Prepared by RTI International under AHRQ Contract # 290-05-0015). Rockville, MD: Agency for Healthcare Research and Quality, 2009. http://library.ahima.org/xpedio/groups/public/documents/government/bok1_046375.pdf (accessed Oct 2011). [Google Scholar]
- 26.Surescripts 2009 State Progress Reports on E-Prescribing. Surescripts LLC, 2010. http://www.surescripts.com/about-e-prescribing/progress-reports/state-progress-reports.aspx (accessed Oct 2011). [Google Scholar]
- 27.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007;42:1758–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd edn Thousand Oaks, CA: Sage Publications, 1994 [Google Scholar]
- 29.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine de Gruyter, 1967 [Google Scholar]
- 30.Wolf MS, Shekelle P, Choudhry NK, et al. Variability in pharmacy interpretations of physician prescriptions. Med Care 2009;47:370–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US Department of Health and Human Services, Centers for Medicare & Medicaid Services Medicare Program; Payment Policies under the Physician Fee Schedule and Other Revisions to Part B for CY 2009; E-Prescribing Exemption for Computer-Generated Facsimile Transmissions; and Payment for Certain Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS); Final Rule. Federal Register Online, Vol. 73, No. 224, 19 Nov 2008; 42 CFR Parts 405, 409, 410, 411, 413, 414, 415, 423, 424, 485, 486, and 489. http://edocket.access.gpo.gov/2008/E8-26213.htm (accessed Oct 2011).
- 32.Bell DS, Straus SG, Belson D. A Toolset for E-Prescribing Implementation in Physician Offices (Prepared by RAND Corporation under Contract No. HHSA 290-2006-00017, TO #4, AHRQ Publication No. 11-0102-EF). Rockville, MD: Agency for Healthcare Research and Quality; In press. [Google Scholar]
- 33.Patel MH, Reynolds KA, Belson D. A Toolset for E-Prescribing Implementation in Independent Pharmacies (Prepared by RAND Corporation under Contract No. HHSA 290-2006-00017I, TO #4, AHRQ Publication No. 11-0101-EF). Rockville, MD: Agency for Healthcare Research and Quality; In press. [Google Scholar]
- 34.Liu H, Burkhart Q, Bell DS. Evaluation of the NCPDP structured and codified sig format for e-prescriptions. J Am Med Inform Assoc 2011;18:645–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh H, Mani S, Espadas D, et al. Prescription errors and outcomes related to inconsistent information transmitted through computerized order entry: a prospective study. Arch Intern Med 2009;169:982–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palchuk MB, Fang EA, Cygielnik JM, et al. An unintended consequence of electronic prescriptions: Prevalence and impact of internal discrepancies. J Am Med Inform Assoc 2010;17:472–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palchuk MB, Turchin A, Alexeyev A, et al. Reducing unintended consequences of e-prescribing on the path to nuanced prescriptions. AMIA Annu Symp Proc 2008:1079. [PubMed] [Google Scholar]
- 38.National Council for Prescription Drug Programs (NCPDP) E-Prescribing Fact Sheet. http://www.ncpdp.org/pdf/Eprescribing_fact_sheet.pdf (accessed Oct 2011).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.