Abstract
Simultaneous bilateral spontaneous rupture of the quadriceps tendon is a very rare condition and only a few cases have been reported in the literature. The etiology is not clear yet. But it occurs infrequently in patients with chronic metabolic disorders. A 30-year-old female patient with simultaneous bilateral spontaneous quadriceps tendon rupture visited our hospital. She had chronic renal failure and her parathyroid hormone level was elevated due to parathyroid adenoma. We report a surgical repair of both quadriceps tendons of a patient with chronic renal failure as well as management of hyperparathyroidism.
Keywords: Quadriceps tendon, End-stage renal failure, Parathyroid hormone
Extensor mechanism injuries without significant history of trauma were seldom reported, and simultaneous bilateral quadriceps tendon rupture is relatively rare. Although it was first reported in 19491), the exact mechanism is not clear yet. Patients with bilateral quadriceps tendon rupture have chronic metabolic diseases such as chronic renal failure and elevated parathyroid hormone2,3). We present a case of bilateral spontaneous rupture of the quadriceps tendon in a patient with chronic renal disease due to the deleterious effect of elevated parathyroid hormone.
Case Report
A 30-year-old woman was presented to our hospital for acute onset of pain in both knees with an inability to extend the knees after a trivial fall following a minor slip. On the physical examination, swelling of the anterior aspect of the distal thigh, bruised skin dimpling at upper pole area (Fig. 1) and inferior displacement of the patella were identified. Evaluation of range of motion revealed complete loss of active knee extension.
Fig. 1.
Gross photograph of left knee shows dimpling or defect of suprapatella lesion.
On her past medical history, she had been on hemodialysis for the past 8 years due to chronic renal failure secondary to lupus nephritis. But, she had received no treatment for the elevated level of parathyroid hormone due to lack of any symptoms.
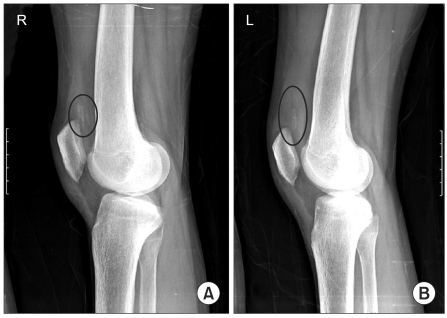
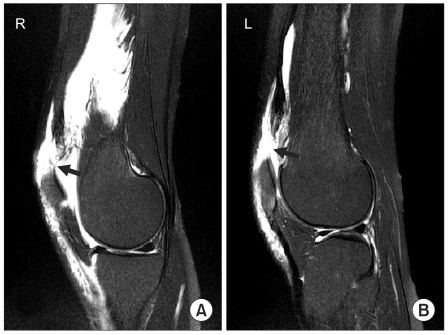
On plain radiographs, there was no fracture around patella upper pole, but irregular calcific deposits in the supra-patella area where quadriceps tendons insert and patella Baja were seen (Fig. 2). On sagittal T2-weighted magnetic resonance imaging (MRI), quadriceps tendons of both knees appeared ruptured, high signal intensity was observed, and moderate degree knee joint effusion and soft tissue hemorrhage around the ruptured tendons were seen (Fig. 3). Other findings were not remarkable.
Fig. 2.
Both lateral view (A: right knee, B: left knee) of knee standing position show obliteration of the quadriceps tendon with inferior patellar displacement without fracture. Dystrophic calcifications of the quadriceps femoris tendon are shown on both supra- patella area (black circle).
Fig. 3.
T2 weight MRI of both knees. Quadriceps tendon is completely disrupted at the patellar attachment site (black arrow). On T2 weight sagittal MR imaging (A: right knee, B: left knee), joint space is enlarged with effusion fluid and extensive deep and superficial soft tissue edema is seen around quadriceps tendon.
The hematochemical analysis revealed the following values (and their reference values): parathyroid hormone (PTH) 1,701 pg/mL (normal range, NL 15.0-65.0 pg/mL), uric acid 6.2 mg/dL (NL 2.5-8 mg/dL), creatinine 9.1 mg/dL (NL 0.5-1.3 mg/dL), serum alkaline phosphatase 671 IU/L (NL<130 IU/L), calcium 9.2 mg/dL (NL 8.4-10.2 mg/dL), and phosphorus 4.4 mg/dL (NL 2.5-5.6 mg/dL).
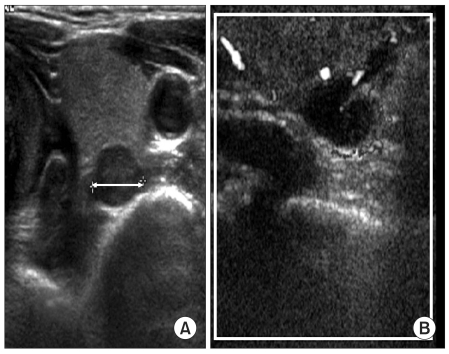
We suspected secondary hyperparathyroidism based on her past medical history and laboratory findings. On ultrasonography of the neck, multiple well-demarcated homogeneous hypoechoic masses were found (Fig. 4). These findings are compatible with tertiary hyperparathyroidism secondary to chronic renal failure, in which PTH secretion occurs independent of blood calcium concentration and autonomous parathyroid function develops.
Fig. 4.
Neck ultrasonogram. Multiple well-demarcated multiple homogeneous hypoechoic mass are shown. Multiple parathyroid adenomas can be suspected. At 8 mm sized homogeneous hypoechoic nodule (A, white arrow). No cervical lymph node enlargement is seen (B).
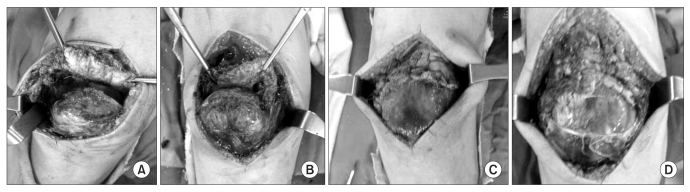
Quadriceps tendon repair was carried out on both knees. Both quadriceps tendons were completely avulsed and ruptured at the tendon insertion sites without bony fragment. The avulsed tendons' ends were ragged with some dystrophic calcifications and the upper border of patellae was softened due to some degree of bone resorption. Around the rupture on superior pole of both patellae, debridement of nonviable surrounding tissues preceded the repair surgery (Fig. 5A, 5B). At first, we sutured the proximal tear site with a non-absorbable number 5 ethibond suture material by Krakow's method, and subsequently made three vertical tunnels from the supra-patella lesion to distal pole of patella on each knee. The suture ends were passed through the patella tunnels and tied distally to the surrounding soft tissues using pull-out technique (Fig. 5C, 5D). Postoperative rehabilitation protocol included immobilization of both knees in extension for 6 weeks. From the 7th postoperative week, gradual weight-bearing and gait training with braces were allowed. At 12 weeks after surgery, the braces were removed because the range of motion and strength of both knees increased.
Fig. 5.
Intra operation gross photograph (A: pre-suture right knee, B: pre-suture left knee, C: post-suture right knee, D: post- suture left knee).
During the rehabilitation period, we consulted a general surgeon and a nephrologist. The general surgeon recommended medical treatment considering her young age and side effects of parathyroidectomy, such as hypoparathyroidism. The nephro logist prescribed vitamin D analog and recommended close monitoring of the parathyroid hormone level. Elevated serum parathyroid hormone level was normalized at 6 months postoperatively. So far we have closely monitored her parathyroid hormone level.
At 18 months postoperatively, the patient had minor weakness during knee extension, but did not complain of any disability and returned to previous daily activities.
Discussion
Simultaneous bilateral spontaneous rupture of the quadriceps tendon is uncommon, and have been described as a complication of various diseases, such as, secondary hyperparathyroidism, systemic lupus erythematosus, diabetes mellitus, gout, rheumatoid arthritis, obesity, and end stage chronic renal failure4). However, the exact mechanism leading to rupture of tendon is still not entirely understood. Some authors pointed out the relationship between the duration of hemodialysis and occurrence of spontaneous tendon rupture, presence of tendinopathy and accumulation of uremic toxin and beta 2-microglobulin amyloid2). The first case of simultaneous bilateral spontaneous rupture of the quadriceps tendon with secondary hyperparathyroidism in a patient on chronic hemodialysis was reported by Preston and Adicoff5). Since then, many authors have described that secondary hyperparathyroidism and its sequel play a major role in the pathogenesis of tendon rupture. In this report, our patient was affected by tertiary hyperparathyroidism. We found multiple parathyroid adenoma in ultrasound examination and noticed that autonomous parathyroid function had developed.
Physiological homeostasis of body calcium and phosphate is regulated by the kidneys, intestines, and parathyroid. In patients with chronic renal failure, a decrease in glomerular filtration rate results in the retention of phosphorus, which leads to hypocalcemia, and decreased serum calcium concentrate causes a proportional increase in the parathyroid hormone level that results in high bone turnover that is caused by osteoclast stimulation to release calcium. As a result, subtendinous bone resorption at the quadriceps tendon insertion site occurs3,4). Dystrophic calcification and subperiosteal bone resorption can be observed on plain radiographs as in our patient. In this situation, repeated avulsion injuries can easily occur without major trauma. As result total tendon rupture can occur. The duration of dialysis was thought to be related to spontaneous tendon rupture6).
Clinical and physical examination, simple plain X-ray, ultrasonogram, and MRI are commonly used for the diagnosis of tendon ruptures7). Although extensor mechanism injuries are easily diagnosed by clinical findings, physical examination, plain radiography, and especially MRI are necessary for determining the site, extension and pattern of tendon rupture as well as for preoperative planning of repair or tendon reconstruction.
Conservative management using medication or cast immobilization is not sufficient for complete restoration of the quadriceps tendon function. In some case reports, Bunnel suture, Krakow stitch and suture-bone tunnel technique were used for quadriceps tendon repair3,8). Although several surgical techniques have been introduced in case reports the basic concept of treatment is to attach the ruptured tendons onto the patella by using non-absorbable suture material1,8). In our case, we sutured proximal tendon with using Krakow stitch to improve tissue grip, then passed the suture through three predrilled parallel vertical bone tunnels, and tied knots at inferior pole of patella with adequate tension.
Strict control of hyperphosphatemia, early use of vitamin D analogs, and, in recalcitrant cases, total parathyroidectomy with or without auto transplantation of a part of the parathyroid gland are needed to prevent these ruptures9). Clinicians should perform careful clinical assessment of the parathyroid hormone level and strict control of hyperphosphatemia using vitamin-calcium therapy.
In summary, bilateral spontaneous rupture of quadriceps tendon is a rare entity, and the role of elevated parathyroid hormone in end-stage renal disease patients seems to play an important role. Proper evaluation and management including surgical repair and medical treatment can result in satisfactory clinical and functional outcomes.
References
- 1.Steiner CA, Palmer LH. Simultaneous bilateral rupture of the quadriceps tendon. Am J Surg. 1949;78:752–755. doi: 10.1016/0002-9610(49)90317-7. [DOI] [PubMed] [Google Scholar]
- 2.De Franco P, Varghese J, Brown WW, Bastani B. Secondary hyperparathyroidism, and not beta 2-microglobulin amyloid, as a cause of spontaneous tendon rupture in patients on chronic hemodialysis. Am J Kidney Dis. 1994;24:951–955. doi: 10.1016/s0272-6386(12)81067-5. [DOI] [PubMed] [Google Scholar]
- 3.Shiota E, Tsuchiya K, Yamaoka K, Kawano O. Spontaneous major tendon ruptures in patients receiving long-term hemodialysis. Clin Orthop Relat Res. 2002;(394):236–242. doi: 10.1097/00003086-200201000-00028. [DOI] [PubMed] [Google Scholar]
- 4.Shah MK. Simultaneous bilateral rupture of quadriceps tendons: analysis of risk factors and associations. South Med J. 2002;95:860–866. [PubMed] [Google Scholar]
- 5.Preston FS, Adicoff A. Hyperparathyroidism with avulsion of three major tendons. Report of a case. N Engl J Med. 1962;266:968–971. doi: 10.1056/NEJM196205102661903. [DOI] [PubMed] [Google Scholar]
- 6.Bhole R, Flynn JC, Marbury TC. Quadriceps tendon ruptures in uremia. Clin Orthop Relat Res. 1985;(195):200–206. [PubMed] [Google Scholar]
- 7.Meneghello A, Bertoli M. Tendon disease and adjacent bone erosion in dialysis patients. Br J Radiol. 1983;56:915–920. doi: 10.1259/0007-1285-56-672-915. [DOI] [PubMed] [Google Scholar]
- 8.Richards DP, Barber FA. Repair of quadriceps tendon ruptures using suture anchors. Arthroscopy. 2002;18:556–559. doi: 10.1053/jars.2002.30729. [DOI] [PubMed] [Google Scholar]
- 9.Goodman WG. Medical management of secondary hyperparathyroidism in chronic renal failure. Nephrol Dial Transplant. 2003;18(Suppl 3):iii2–iii8. doi: 10.1093/ndt/gfg1002. [DOI] [PubMed] [Google Scholar]