Abstract
Bilateral quadriceps tendon rupture is an unusual injury, but may be encountered in patients with various chronic diseases after minor trauma. This article presents a case of bilateral quadriceps tendon rupture of a 38-year-old woman with chronic renal failure. Surgical repair was performed using a bone tunnel technique with a nonabsorbable suture and a suture anchor. Postoperative magnetic resonance imaging confirmed complete healing of the repair site, and clinically active extension with 120 degrees of range of motion was achieved.
Keywords: Quadriceps tendon, Bilateral rupture, Chronic renal failure, Primary repair
The advent of hemodialysis has extended the life expectancy and improved the quality of life of patients with chronic renal failure, but the incidence of secondary complications is also increasing. In particular, quadriceps tendon rupture, albeit rare, may occur after minor trauma in patients treated for chronic renal failure1-4). Domestically, only one case of bilateral quadriceps tendon rupture combined with chronic renal failure has been reported5), though internationally, it has been documented by several authors1,2,4,6-8). Here, we report the surgical treatment results of bilateral quadriceps tendon rupture in a patient with chronic renal failure and include a review of relevant literature.
Case Report
A 39-year-old female patient visited our clinic with complaints of tenderness in anterior knees and an inability to walk after losing her footing on stairs. Her medical history included insulin treatment for diabetes diagnosed 20 years previously, and a 10-year history of dialysis for end-stage renal failure secondary to diabetic neuropathy. Ambulation was not limited before the incident. Physical examination revealed tenderness at the insertion sites of quadriceps tendons into bilateral patellae, slight swelling, and no active movement of either knee joint. Plain radiography revealed calcification of the quadriceps tendons (Fig. 1). On sagittal T2-weighted magnetic resonance images (MRIs), complete ruptures at tendon-osseous junctions were observed (Fig. 2). Blood test results showed chronic anemia (white blood cell count 3,300/mm2; hemoglobin level 10.0 g/dL; and platelet count 100,000/mm2) and hyperparathyroidism secondary to chronic renal failure (BUN, 35.5 mg/dL; Cr, 7.7 mg/dL; ALP, 419.5 IU/L; intact Parathyroid hormone (iPTH), 1,940 pg/mL; calcium, 8.1 mg/dL; and phosphate, 3.9 mg/dL).
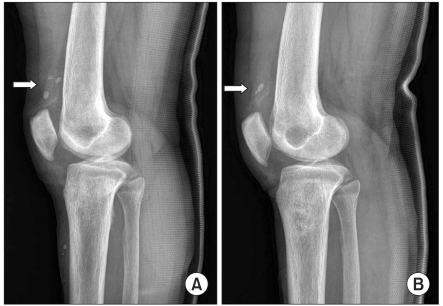
Fig. 1.
Lateral radiographs of right (A) and left (B) knees showing patella baja and calcification of quadriceps tendons (arrows).
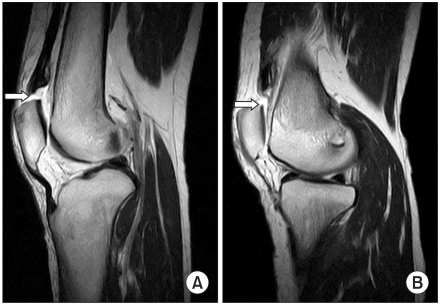
Fig. 2.
Preoperative sagittal T2-weighted magnetic resonance images of the right (A) and left (B) knees showing complete disruption at the distal quadriceps tendo-osseous junctions (arrow).
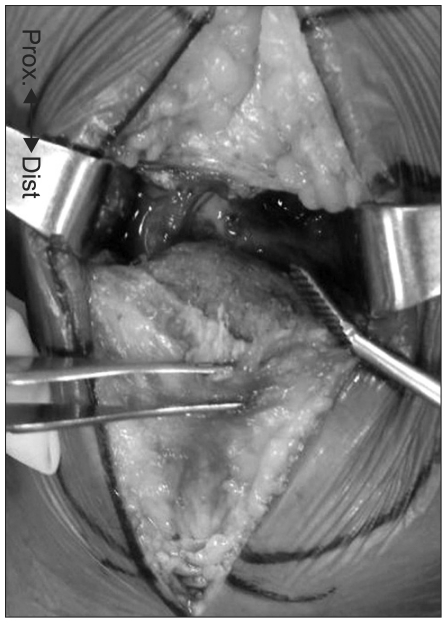
The ruptured quadriceps tendons and the superior aspect of patellae were exposed via a median approach. Based on the observations that there was no severe soft tissue damage, the quadriceps tendons were completely ruptured at the tendon-osseous junction, and the surface was smooth, we suspected that the rupture was not caused by severe trauma and there was chronic erosion at bone-tendon attachment sites (Fig. 3). Soft tissues on the surface were sufficiently removed and bleeding was elicited from bone surfaces to promote tendon to bone healing (Fig. 4). Six bone tunnels were created and quadriceps tendons were sutured to proximal patellae with non-absorbable sutures using a Krackow technique (Fig. 5). Sutures were added medially and laterally using two Bio-Mini Revo (Linvatec, Largo, FL, USA) bio-absorbable suture screws.
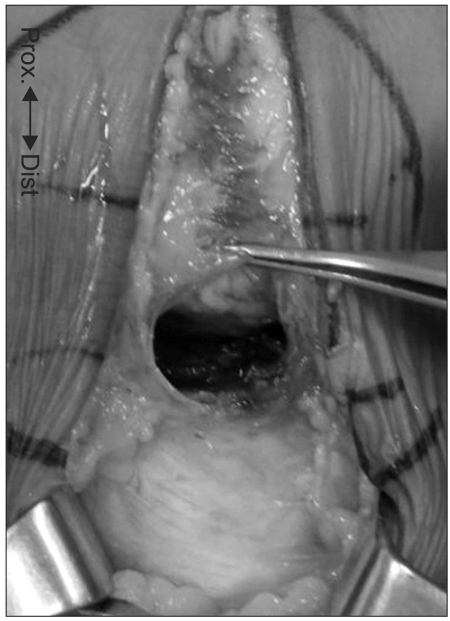
Fig. 3.
Smooth and round surface of a ruptured quadriceps tendon at the tendo-osseus junction.
Fig. 4.
Bleeding bony surface at the proximal pole of a patella after rasping.
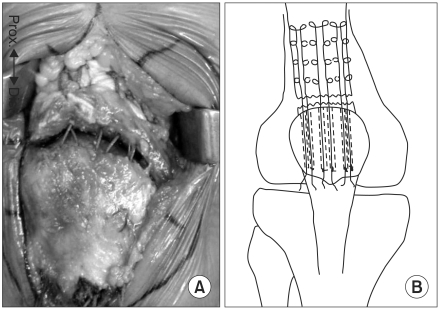
Fig. 5.
(A) Ruptured quadriceps tendons were sutured using a Krackow technique and nonabsorbable suture materials. (B) Schematic illustration of the operative technique.
Long-leg cast immobilization was maintained for two weeks and then replaced with cylindrical long-leg casts with knees in extension for 6 weeks. This was then followed by weight-bearing crutch walking. For 6 weeks, progressive joint movement exercises were performed with ACL braces in situ. At 4 months after surgery, the patient was pain free and range of motion of both knees improved to 0°-120°, active extension was possible, and quadriceps muscle strengths were of Medical Research Council grade V (normal). At 6 months after surgery, MRI confirmed that tendons were attached to the proximal poles of both patellae (Fig. 6).
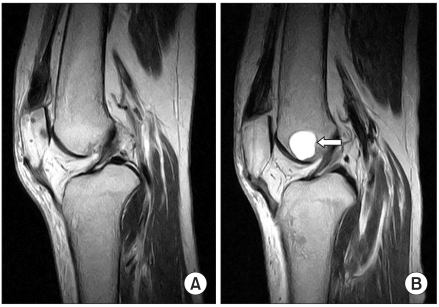
Fig. 6.
Sagittal T2-weighted magnetic resonance image of the right knee (A) and left knee (B) at 6 months after surgery showing a quadriceps tendon well attached to the patella proximal pole. A high signal intensity cystic lesion (2×2 cm sized) was found incidentally at the left distal femur (arrow).
Discussion
Bilateral quadriceps tendon rupture usually occurs after major trauma when the quadriceps muscles eccentrically contract with feet set on the floor. However, it may also occur after minor trauma in patients with chronic renal failure, gout, systemic lupus erythematosus, diabetes, rheumatoid arthritis, or secondary hyperparathyroidism, and in patients on various steroid treatments3,4).
The cause of tendon rupture has not been established. Some authors attribute it to diminished local circulation, impaired collagen metabolism, repetitive microtrauma, tendon weakness and reduced tendon elasticity caused by calcification7). Petersen et al.7) described an avascular area in the deep portion of the tendon near the patellar groove where the patella articulates with the femur during flexion and degenerative changes occur. Most authors agree that bone resorption at tendon insertion sites caused by secondary hyperparathyroidism plays a significant role in the pathogenesis of tendon rupture6).
Bilateral quadriceps tendon rupture has been associated with the period of illness and of dialysis in patients with chronic renal failure8). In these patients, elevated parathyroid hormone levels result in renal osteodystrophy, vitamin D deficiency leads to osteomalacia, and collagen metabolism impairment and dystrophic calcification occur. Furthermore, tendon weakening is unavoidable when collagen is replaced by elastin due to chronic metabolic acidosis6,8).
The radiological diagnosis of tendon rupture and postoperative assessments of tendon-bone attachment can be made by sonography or MRI. In our patient, MRI was used to identify quadriceps tendon ruptures before surgery and to confirm tendon-bone attachments after rehabilitation at 6 months after surgery1).
Vastus lateralis muscle flaps, triangular flaps of the proximal quadriceps, Mersilene strip sutures, Dacron grafts, and bone tunnels can be used to repair tendon ruptures2). Choi et al.5) sutured a ruptured quadriceps ligament to the vastus intermedius, made 3 vertical holes in patellar bone, and used a pull-out suture technique. In the described case, we passed a nonabsorbable suture through 6 bone tunnels, sutured tendons to superior patellae using the Krackow suture technique, and performed additional attachments to bilateral sides of both patellae using Bio-Mini Revo (Linvatec) bioabsorbable suture screws to improve stability.
We report a case of bilateral quadriceps tendon rupture after minor trauma in a young chronic renal failure patient who had been on dialysis for a long-term period. Tendon repairs were performed successfully using non-absorbable sutures and bioabsorbable screws and the results were presented with a review of the literature. This case cautions that quadriceps tendon rupture may occur in young and active patients on dialysis for chronic renal failure.
References
- 1.Kim YH, Shafi M, Lee YS, Kim JY, Kim WY, Han CW. Spontaneous and simultaneous rupture of both quadriceps tendons in a patient with chronic renal failure. A case studied by MRI both preoperatively and postoperatively. Knee Surg Sports Traumatol Arthrosc. 2006;14:55–59. doi: 10.1007/s00167-005-0626-9. [DOI] [PubMed] [Google Scholar]
- 2.Lombardi LJ, Cleri DJ, Epstein E. Bilateral spontaneous quadriceps tendon rupture in a patient with renal failure. Orthopedics. 1995;18:187–191. doi: 10.3928/0147-7447-19950201-18. [DOI] [PubMed] [Google Scholar]
- 3.Matokovic D, Matijasevic B, Petric P, Crnkovic T, Skorvaga S. A case report of spontaneous concurrent bilateral rupture of the quadriceps tendons in a patient with chronic renal failure. Ther Apher Dial. 2010;14:104–107. doi: 10.1111/j.1744-9987.2009.00695.x. [DOI] [PubMed] [Google Scholar]
- 4.Shah MK. Simultaneous bilateral quadriceps tendon rupture in renal patients. Clin Nephrol. 2002;58:118–121. doi: 10.5414/cnp58118. [DOI] [PubMed] [Google Scholar]
- 5.Choi SW, Kim SR, Nam KW, Seo KB, Shin SJ, Seo JY, Kim GM, Bang HS. Spontaneous and simultaneous rupture of bilateral quadriceps tendons in a patient with chronic renal failure: a case report. Korean J Sports Med. 2010;28:132–136. [Google Scholar]
- 6.Mahlfeld K, Kayser R, Franke J, Grasshoff H. Bilateral and simultaneous quadriceps tendon rupture in secondary hyperparathyroidism. A case report. Zentralbl Chir. 1999;124:1045–1048. [PubMed] [Google Scholar]
- 7.Petersen W, Stein V, Tillmann B. Blood supply of the quadriceps tendon. Unfallchirurg. 1999;102:543–547. doi: 10.1007/s001130050448. [DOI] [PubMed] [Google Scholar]
- 8.Ribbans WJ, Angus PD. Simultaneous bilateral rupture of the quadriceps tendon. Br J Clin Pract. 1989;43:122–125. [PubMed] [Google Scholar]