Abstract
Purpose
We compared and analyzed the short term results of high flexion total knee arthroplasty (TKA) with mobile-bearing and fixed bearing designs.
Materials and Methods
We studied 32 patients that had undergone TKA with LPS-Flex Mobile and 34 patients with LPS-Flex Fixed using an electromagnetic navigation system between January 2010 and June 2010, and were followed up for at least 1 year.
Results
Knee Society Functional Score (KSFS) and Knee Society Knee Score (KSKS) of the mobile-bearing group were 94.5 and 93.8 points, respectively, and were 48.2 and 45.3 points preoperatively, whereas those of the fixed-bearing group were 95.1 and 94.2 points, respectively, and were 49.5 and 46.9 points preoperatively. Postoperative mechanical axis deviation and implant position of the femoral and tibial component both on the coronal and sigittal planes showed no significant differences between the two groups. Range of motion (ROM) and maximal flexion angle (MFA) of the knee joint also showed no significant differences between the two groups. The possibility of crossed-legged sitting and kneeling position also showed no significant differences between the two groups.
Conclusions
Clinical and radiologic parameters, ROM and MFA of knee joints showed no significant differences in both the groups, but long term follow-up results may be necessary, including survival rate.
Keywords: Knee joint, High flexion total knee arthroplasty, Electromagnetic navigation system, Mobile-bearing, Fixed-bearing
Introduction
The goals of total knee arthroplasty (TKA) are to relieve pain, maintain knee function and kinematics, and restore stability and range of motion (ROM) to facilitate daily activities. Of these, restoration of ROM has been considered important especially in Eastern countries where high flexion is required for religious and social activities. Factors that can be associated with ROM include the cause of disease, preoperative joint deformity and ROM, age, gender, surgical technique, implant fixation strength, postoperative rehabilitation, and implant design1).
Since first introduced in TKA for optimal component positioning and lower limb alignment, navigation systems have been improved with rapid development of computer technology to allow for soft tissue balancing and flexion-extension gap balancing, and accordingly have contributed to the accuracy of TKA2).
In this study, we analyzed the results of high flexion TKA using one of the most recently developed navigation systems, the electromagnetic navigation system, to compare the influence of two different implant designs (mobile-bearing and fixed bearing designs) on ROM including maximal flexion angle and clinical and radiographic results. The mobile-bearing implant used was NexGen LPS-Flex Mobile Knee (NexGen, Legacy Posterior-Stabilized flexion Mobile, Zimmer, Warsaw, IN, USA) whereas the fixed-bearing implant was NexGen LPS-Flex Fixed Knee (NexGen, Legacy Posterior-Stabilized flexion Fixed, Zimmer).
Materials and Methods
1. Materials
Of the patients that had undergone TKA by the same surgeon between January 2010 and June 2010 at our institution, 67 patients with a minimum follow-up of one year were randomly selected for this study. The implants used were the LPS-Flex Mobile knee in 32 patients and LPS-Flex Fixed knee in 34 patients. In six of the patients with bilateral TKA, the mobile-bearing prosthesis was used on one side and the fixed-bearing on the other side. In all patients, an electromagnetic navigation system (Zimmer Computer Assisted Solutions Electromagnetic Quad-Sparing) was used. The mean follow-up period was 14.5 months (range, 12 to 18 months) and the mean age of the patients was 67.5 years (range, 60 to 78 years) in the mobile-bearing group and 68.5 years (range, 61 to 77 years) in the fixed-bearing group. The cause of injury was degenerative arthritis in all patients. The mean preoperative ROM was 118° in both groups and no notable intergroup difference could be found regarding flexion contracture (Table 1).
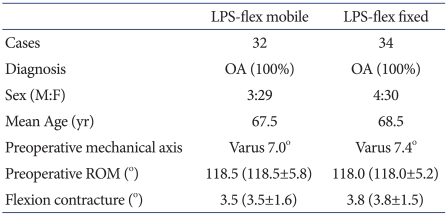
Table 1.
Demographic Parameters of Both Treatment Groups in This Study
ROM: range of motion.
Considering that the preoperative ROM could affect the postoperative ROM3,4), we excluded patients who had ≤90° of ROM preoperatively. There were no particular instructions for knee flexion exercises and the same rehabilitation protocol was prescribed in both groups.
2. Clinical Assessment
The clinical results were graded according to the Knee Society Knee Score (KSKS) and Knee Society Functional Score (KSFS). Patient satisfaction and preference were assessed according to the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score5), a questionnaire for measuring pain, stiffness, and function. Postoperative pain was evaluated using the visual analog scale (VAS). A patient's ability to kneel and sit cross-legged was assessed through interview or observation during follow-up.
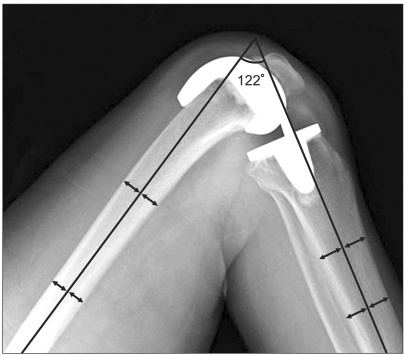
Physical examination and goniometric measurement have been commonly used in the assessment of ROM and maximal flexion angle. However, we used a radiographic measurement method devised by Edwards et al.6) to reduce measurement errors and increase reproducibility. We measured the angle formed by lines drawn down the mid-shafts of the tibia and femur on the lateral radiographs taken with the knee in full extension and full flexion preoperatively, as well as at the final follow-up (Fig. 1).
Fig. 1.
Radiological measurements of mid-lines of the femur and tibia.
3. Radiographic Assessment
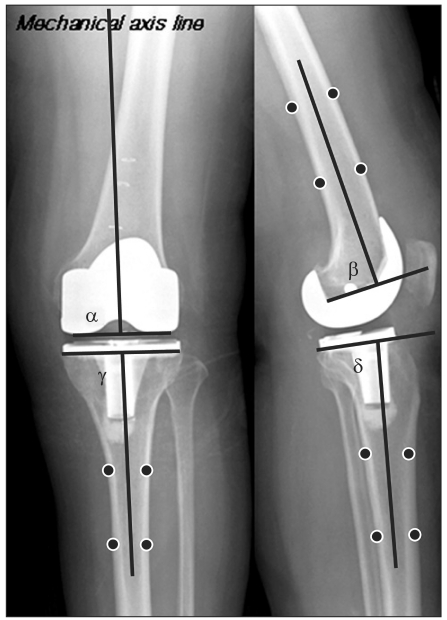
Radiographic assessment was done by the same surgeon three times per patient and the mean value was used for analysis. The mechanical axis deviation was measured as the difference in the angle between the femoral mechanical axis and the tibial mechanical axis on the weight bearing long leg anteroposterior radiographs taken preoperatively and postoperatively. The femoral and tibial component positions in the sagittal and coronal planes were assessed using the method of Seon and Song7). The coronal inclination of the femoral component was measured as the medial angle between the mechanical axis and the bottom of the component on the anteroposterior radiographs and the sagittal inclination as the angle with the femoral shaft on the lateral views. The desired sagittal inclination was defined as 90°. The coronal and sagittal tibial component positions were assessed in a similar manner. The bisecting line of the tibial shaft was used as a reference for sagittal tibial component positioning. The desired tibial component inclination was defined as 90° in the coronal plane and 86o in the sagittal plane (Fig. 2).
Fig. 2.
Implant position angle (α: coronal medial inclination of femoral component, β: sagittal posterior slope of femoral component, γ: coronal medial inclination of tibial component, δ: sagittal posterior slope of tibial component).
4. Surgical Technique
All the operations were performed by the same surgeon using a medial parapatella approach. To increase articulation curvature during flexion, an additional 2 mm posterior femoral bone cut was performed. The anterior portion of the tibial component was removed to avoid interference with the patella and the posterior cam mechanism was modified to facilitate high flexion.
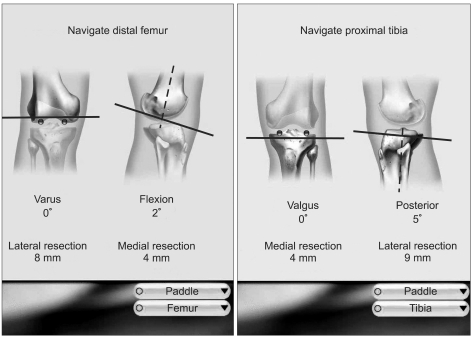
The preoperative and postoperative mechanical axes and extent of bone resection could be evaluated using an electromagnetic navigation system in all cases. In particular, varus/valgus femoral resection, degree of flexion/extension, varus/valgus tibial resection, and posterior tilt could be assessed in real time during bone resection of the distal femur and the proximal tibia by placing a paddle on the resection surface (Fig. 3). After bone resection, lower limb alignment was assessed using the navigation system with a temporary implant or an inserted spacer. After implant fixation, the alignment was evaluated and corrected intraoperatively if needed.
Fig. 3.
A display screen in the electomagnetic navigation during resection of the distal femur and proximal tibia (real time information).
For the LPS-Flex Mobile bearing knee, any osteophytes that could cause soft tissue tension were thoroughly removed and subperiosteal release of the medial and lateral collateral ligaments at their insertion sites was performed. Flexion/extension gaps were measured intraoperatively using a gapper in several trial tests to confirm mediolateral stability prior to soft tissue balancing. For the LPS-Flex Mobile bearing knee, tibial resection preceded femoral resection, whereas it was vice versa for the LPS-Flex Fixed bearing knee.
5. Rehabilitation
Quadriceps femoris strengthening exercises were initiated immediately after surgery. From the 2nd postoperative day, active joint movement exercises were performed in tandem with passive exercises using CPM devices to facilitate rapid ROM recovery. Weight-bearing ambulation was allowed after suture removal at the 2nd postoperative week.
6. Statistical Analysis
Statistical analysis was performed using SPSS ver. 12.0 (SPSS, Inc., Chicago, IL, USA). KSKS, KSFS, WOMAC score, VAS for pain, and ROM and maximal flexion angle before surgery and at the last follow-up were analyzed using an independent sample t-test. Patient ability to kneel and sit cross-legged was assessed using the chi-square test.
Results
1. Clinical Results
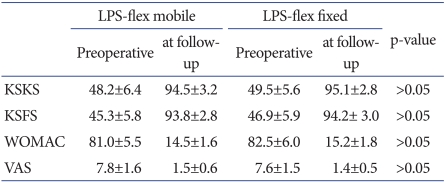
There were no statistically significant intergroup differences in the KSKS and KSFS (p>0.05). In the mobile-bearing group, the mean KSKS and KSFS increased from 48.2 (48.2±6.4) preoperatively to 94.5 (94.5±3.2) at the last follow-up and from 45.3 (45.3±5.8) preoperatively to 93.8 (93.8±2.8) at the last follow-up, respectively. In the fixed-bearing group, the mean KSKS and KSFS increased from 49.5 (49.5±5.6) preoperatively to 95.1 (95.1±2.8) at the last follow-up and from 46.9 (46.9±5.9) preoperatively to 94.2 (94.2±3.0) at the last follow-up (p>0.05). The mean WOMAC score decreased in both groups, from 81.0 (81.0±5.5) preoperatively to 14.5 (14.5±1.6) at the last follow-up in the mobile-bearing group and from 82.5 (82.5±6.0) preoperatively to 15.2 (15.2±1.8) at the last follow-up in the fixed-bearing group (p>0.05). There were no notable intergroup differences in the mean VAS pain score (p>0.05) (Table 2). The mean VAS pain score improved from 7.8 (7.8±1.6) preoperatively to 1.5 (1.5±0.6) at the last follow-up in the mobile-bearing group and from 7.6 (7.6±1.5) preoperatively to 1.4 (1.4±0.5) at the last follow-up in the fixed-bearing group.
Table 2.
Clinical results according to KSKS, KSFS, and VAS
KSKS: Knee Society Knee Score, KSFS: Knee Society Functional Score, VAS: Visual Analogue Scale, WOMAC: Western Ontario and McMaster Universities Arthritis Index.
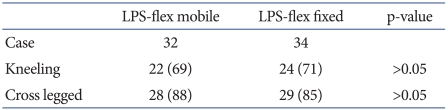
2. Kneeling and Cross-Legged Sitting
Significant intergroup differences were not identified in the ability to kneel and sit cross-legged through observation or interview during the follow-up (p>0.05) (Table 3). Kneeling and cross-legged sitting was possible in 22 and 28 cases, respectively, in the mobile bearing group (n=32) and in 24 and 29 cases, respectively, in the fixed-bearing group (n=34).
Table 3.
Daily Living Results from the Possibility of the Kneeling Position and Cross-Legged Sitting Position
Values are presented as number (%).
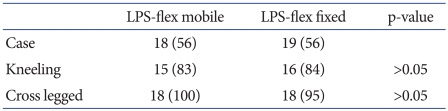
No remarkable intergroup differences were noted in patients with ≥130° maximal flexion angle (high flexion) (p>0.05) (Table 4). The number of patients with ≥130° maximal flexion angle was 18 in the mobile-bearing group and 19 in the fixed-bearing group. Kneeling and cross-legged sitting was possible in 15 and 18 cases, respectively, in patients with high flexion in the mobile-bearing group and in 16 and 18 cases, respectively, in patients with high flexion in the fixed-bearing group.
Table 4.
Daily Living Results from the Possibility of the Kneeling Position and Cross-legged Sitting Position in MFA Over 130° Groups
Values are presented as number (%).
MFA: maximal flexion angle.
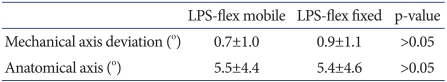
3. Radiographic Results
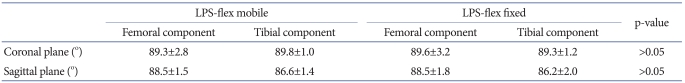
On the lower limb alignment, the mechanical axis deviation was more varus in the fixed-bearing group (0.9°±1.1°) than in the mobile-bearing group (0.7°±1.0°), but there was no significant difference between the groups. The coronal inclination of femoral component coronal and tibial component was 89.3°±2.8° and 89.8°±1.0°, respectively, in the fixed-bearing group and 89.6°±3.2° and 89.3°±1.2°, respectively, in the mobile-bearing group. The sagittal inclination of femoral component and tibial component was 88.5°±1.5° and 86.6°±1.4° in the fixed-bearing group and 88.5°±1.8° and 86.2°±2.0° in the mobile-bearing group. Thus, the coronal and sagittal implant positioning was satisfactory in both groups, which showed no significant intergroup differences (Tables 5, 6).
Table 5.
Radiologic Results of Limb Alignment after Total Knee Arthroplasty
Table 6.
Radiologic Results of Implant Position after Total Knee Arthroplasty
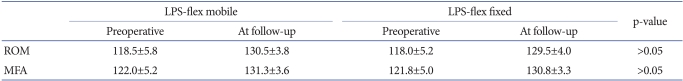
4. ROM and Maximum Knee Flexion
There were no statistically significant intergroup differences in ROM and maximal flexion angle (p>0.05). The mean ROM increased from 118.5 (118.5±5.8) preoperatively to 130.0 (130.0±3.8) at the last follow-up in the mobile-bearing group and from 118.0 (118.0±5.2) preoperatively to 129.5 (129.5±4.0) at the last follow-up in the fixed-bearing group. The mean maximal flexion angle increased from 122.0 (122.0±5.2) preoperatively to 131.1 (131.1±3.6) at the last follow-up in the mobile-bearing group and from 121.8 (121.8±5.0) preoperatively to 130.8 (130.8±3.3) at the last follow-up in the fixed-bearing group (p>0.05) (Table 7) (Figs. 4, 5).
Table 7.
Radiologic Results of the Range of Motion (ROM) and Maximal Flexion Angle (MFA)
Fig. 4.
A 66-year-old woman visited our clinic with pain in both knees for 7 years (A). We performed left total knee arthroplasty using Zimmer LPS-Flex Mobile (B). At the last follow up (14 months after total knee arthroplasty), flexion contracture of left knee joint was 0°, and KSKS was 96 points, which was 50 points preoperatively, and KSFS was 95 points, which was 48 points preoperatively, and WOMAC score was 12 points, which was 85 points preoperatively. Maximal flexion angle of left knee joint was 138°, which was 120° preoperatively, and cross-legged sitting position and kneeling position were all possible (C). KSKS: Knee Society Knee Score, KSFS: Knee Society Functional Score, WOMAC: Western Ontario and McMaster Universities Arthritis Index.
Fig. 5.
A 77-year-old woman visited our clinic with both knee pain for 7 years (A). We performed left total knee arthroplasty using Zimmer LPS-Flex Fixed (B). At the last follow-up (13 months after total knee arthroplasty), flexion contracture of left knee joint was 0°, and KSKS was 94 points, which was 49 points preoperatively, and KSFS was 95 points, which was 51 points preoperatively, and WOMAC score was 13 points, which was 84 points preoperatively. Maximal flexion angle of left knee joint was 140°, which was 119° preoperatively, and cross-legged sitting position and kneeling position were all possible (C). KSKS: Knee Society Knee Score, KSFS: Knee Society Functional Score, WOMAC: Western Ontario and McMaster Universities Arthritis Index.
5. Complications
Polyethylene component wear, posterior instability, component loosening, or infection was not observed in any of the patients during the ≥1 year follow-up period. Complications requiring revision surgery were not noted during the short-term follow-up period.
Discussion
The primary goal of TKA is to alleviate pain but it is more favorable to restore normal knee function8). Postoperative ROM is especially important for Asian patients who frequently squat or sit in a cross-legged position9).
Goodfellow and O'Connor10) introduced a mobile-bearing knee system in 1976 to address component loosening and wear, the two most common issues of TKA. High flexion knee system is a recent invention for overcoming ROM restriction. The mechanism that hinders knee flexion remains unclear, but the ability to restore posterior femoral translation has been considered crucial for improving range of flexion after TKA11,12). A decrease in posterior femoral translation causes impingement of the posterior edge of the tibial component on the femoral shaft, thus constraining flexion motion11-13). High flexion knee system was designed to increase posterior femoral translation for high flexion12,13).
We used the high-flexion LPS-Flex total knee system in this study. An additional 2 mm posterior femoral bone resection was performed to extend the posterior condyle of the femoral component by 2 mm and increase the articular contact area and thus posterior femoral translation for high flexion. In addition, the stress on the polyethylene implant was reduced, which contributed to the low incidence of component wearing. The LPS-Flex Mobile system is a mobile bearing implant designed to allow for a total of 50° of axial rotation (internal rotation, 25° and external rotation, 25°) of the polyethylene insert in the tibial component during knee flexion. Therefore, we used a technique similar to the 'gap technique' for soft tissue balancing in the mobile-bearing group: after tibial resection, internal/external stability was confirmed by measuring the flexion/extension gaps in several trial tests. In contrast, 'measured resection technique' where femoral resection precedes tibial resection, was used in the fixed-bearing group. In our opinion, comparisons of the postoperative lower limb alignment and coronal/sagittal implant positions between the groups should be performed in further studies.
A navigation system was used to improve accuracy of TKA in this study. Therefore, a range of errors could be identified at every step of the surgery and the surgeon could give real time feedback based on surgical experience and intraoperative data to achieve ideal values14). There are many studies showing that navigation-assisted TKA produces more satisfactory results than the established TKA in terms of implant positioning and lower limb alignment that are associated with long-term longevity15-18).
Mobile-bearing knee prostheses are more effective in reducing fatigue wear because the enlarged contact surface causes less stresses compared to fixed-bearing ones19) and in lowering stresses on the bone-implant interface and risk of loosening, which potentially increases implant longevity10,20). Another advantage is that the motion between the tibial component and the polyethylene insert can be adjusted to minimize backside wear21).
Clinical results of TKA using mobile-bearing and fixed-bearing implants have been addressed in various studies. Woolson et al.22) reported that there were no significant differences between the mobile-bearing implant group (57 cases) and fixed-bearing implant group (45 cases) in terms of the KSKS, KSFS, pain score, and postoperative flexion angle. Ranawat et al.23) used mobile-bearing and fixed-bearing implants during TKA in 26 patients and found no notable differences between the two implants in terms of the KSKS and KSFS, postoperative ROM and maximal flexion angle, knee pain, and patient satisfaction. Lampe et al.24) used navigation in 52 cases of mobile-bearing knee replacement and 48 cases of fixed-bearing knee replacement. At ≥2 years postoperatively, no significant differences were noted in the KSKS and KSFS, Oxford knee score, and ROM. Kim et al.25) performed 116 cases of bilateral TKAs using a mobile-bearing implant and a fixed-bearing implant on each side and found no significant differences between the two types of implants in terms of the ROM, KSKS, pain score, patient satisfaction, and polyethylene wear.
In contrast, Price et al.26) reported that the KSKS and pain score at 1 year after surgery were higher, albeit slightly, in the mobile-bearing group although the ROM was similar between the groups with 105.3°. Luring et al.27) reported that the mediolateral stability was higher in the mobile-bearing group after PCL retaining TKA. Sohn et al.28) followed 32 patients that underwent bilateral TKA using a mobile-bearing implant and a fixed-bearing implant on each side and noted that the postoperative subjective satisfaction and preference evaluated using the WOMAC score was higher in the mobile-bearing group although the two implants did not result in differences in the KSKS, KSFS, and postoperative ROM.
In this study, significant intergroup differences were not observed in the KSKS and KSFS, WOMAC score, ROM and maximal flexion angle, and possibility of kneeling and sitting cross-legged (p>0.05). The radiographic results showed that there were no notable intergroup differences in the postoperative mechanical axis deviation and the femoral and tibial component positions in the sagittal and coronal planes (p>0.05). However, we think these results should be confirmed by further studies with longer follow-up periods.
Conclusions
The clinical results of high-flexion TKA were satisfactory in both the mobile-bearing and fixed-bearing group. There were no significant intergroup differences regarding the clinical results (KSS, KSFS, and WOMAC score), radiological results (ROM and maximal flexion angle), and possibility of kneeling and sitting cross-legged. However, these results should be verified in long-term follow-up studies that address the longevity of the implants.
References
- 1.Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA. Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br. 1993;75:950–955. doi: 10.1302/0301-620X.75B6.8245090. [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M. Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng. 2006;128:867–871. doi: 10.1115/1.2354201. [DOI] [PubMed] [Google Scholar]
- 3.Lizaur A, Marco L, Cebrian R. Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J Bone Joint Surg Br. 1997;79:626–629. doi: 10.1302/0301-620x.79b4.7242. [DOI] [PubMed] [Google Scholar]
- 4.Stern SH, Insall JN. Total knee arthroplasty in obese patients. J Bone Joint Surg Am. 1990;72:1400–1404. [PubMed] [Google Scholar]
- 5.Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum. 1989;18:14–17. doi: 10.1016/0049-0172(89)90010-3. [DOI] [PubMed] [Google Scholar]
- 6.Edwards JZ, Greene KA, Davis RS, Kovacik MW, Noe DA, Askew MJ. Measuring flexion in knee arthroplasty patients. J Arthroplasty. 2004;19:369–372. doi: 10.1016/j.arth.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Seon JK, Song EK. The accuracy of lower extremity alignment in a total knee arthroplasty using computer-assisted navigation system. J Korean Orthop Assoc. 2004;39:566–571. [Google Scholar]
- 8.Cho WS, Park JH, Kim JM, Hwang WY, Nam TS. Factors affecting range of motion after total knee arthroplasty. J Korean Orthop Assoc. 2003;38:683–688. [Google Scholar]
- 9.Ritter MA, Campbell ED. Effect of range of motion on the success of a total knee arthroplasty. J Arthroplasty. 1987;2:95–97. doi: 10.1016/s0883-5403(87)80015-3. [DOI] [PubMed] [Google Scholar]
- 10.Goodfellow JW, O'Connor J. Clinical results of the Oxford knee. Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res. 1986;(205):21–42. [PubMed] [Google Scholar]
- 11.Li G, Schule SL, Zyontz SJ, Maloney WJ, Rubash HE. In: Improving flexion in total knee arthroplasty. Callaghan JJ, Rosenberg AG, Rubash HE, Simonian PT, Wickiowicz TL, editors. Vol. 2. Philadelphia: Lippincott Williams and Wilkins; 2003. pp. 1233–1234. [Google Scholar]
- 12.Walker PS, Garg A. Range of motion in total knee arthroplasty. A computer analysis. Clin Orthop Relat Res. 1991;(262):227–235. [PubMed] [Google Scholar]
- 13.Song YJ, Ha CW. Functional evaluation of high-flex total knee arthroplasty. J Korean Knee Soc. 2009;21:29–34. [Google Scholar]
- 14.Kanlic EM, Delarosa F, Pirela-Cruz M. Computer assisted orthopaedic surgery: CAOS. Bosn J Basic Med Sci. 2006;6:7–13. doi: 10.17305/bjbms.2006.3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ensini A, Catani F, Leardini A, Romagnoli M, Giannini S. Alignments and clinical results in conventional and navigated total knee arthroplasty. Clin Orthop Relat Res. 2007;457:156–162. doi: 10.1097/BLO.0b013e3180316c92. [DOI] [PubMed] [Google Scholar]
- 16.Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: comparison with conventional methods. J Arthroplasty. 2005;20:132–138. doi: 10.1016/j.arth.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Bathis H, Perlick L, Tingart M, Luring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–687. doi: 10.1302/0301-620x.86b5.14927. [DOI] [PubMed] [Google Scholar]
- 18.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618–626. doi: 10.1016/j.arth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Otto JK, Callaghan JJ, Brown TD. Gait cycle finite element comparison of rotating-platform total knee designs. Clin Orthop Relat Res. 2003;(410):181–188. doi: 10.1097/01.blo.0000062381.79828.67. [DOI] [PubMed] [Google Scholar]
- 20.Lee DC, Sohn OJ. A comparison of mobile-bearing and fixed-bearing total knee arthroplasties in osteoarthritic patients. J Korean Knee Soc. 2007;19:154–160. [Google Scholar]
- 21.Callaghan JJ, Squire MW, Goetz DD, Sullivan PM, Johnston RC. Cemented rotating-platform total knee replacement. A nine to twelve-year follow-up study. J Bone Joint Surg Am. 2000;82:705–711. [PubMed] [Google Scholar]
- 22.Woolson ST, Epstein NJ, Huddleston JI. Long-Term Comparison of Mobile-Bearing vs Fixed-Bearing Total Knee Arthroplasty. J Arthroplasty. 2011;26:1219–1223. doi: 10.1016/j.arth.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 23.Ranawat AS, Rossi R, Loreti I, Rasquinha VJ, Rodriguez JA, Ranawat CS. Comparison of the PFC Sigma fixed-bearing and rotating-platform total knee arthroplasty in the same patient: short-term results. J Arthroplasty. 2004;19:35–39. doi: 10.1016/j.arth.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 24.Lampe F, Sufi-Siavach A, Bohlen KE, Hille E, Dries SP. One year after navigated total knee replacement, no clinically relevant difference found between fixed bearing and mobile bearing knee replacement in a double-blind randomized controlled trial. Open Orthop J. 2011;5:201–208. doi: 10.2174/1874325001105010201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim YH, Kook HK, Kim JS. Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res. 2001;(392):101–115. doi: 10.1097/00003086-200111000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Price AJ, Rees JL, Beard D, Juszczak E, Carter S, White S, de Steiger R, Dodd CA, Gibbons M, McLardy-Smith P, Goodfellow JW, Murray DW. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br. 2003;85:62–67. doi: 10.1302/0301-620x.85b1.13233. [DOI] [PubMed] [Google Scholar]
- 27.Luring C, Bathis H, Oczipka F, Trepte C, Lufen H, Perlick L, Grifka J. Two-year follow-up on joint stability and muscular function comparing rotating versus fixed bearing TKR. Knee Surg Sports Traumatol Arthrosc. 2006;14:605–611. doi: 10.1007/s00167-005-0020-7. [DOI] [PubMed] [Google Scholar]
- 28.Sohn OJ, Lee DC, Cho JH. Comparision between mobile bearing and fixed bearing T.K.A. in the same patient. J Korean Orthop Assoc. 2008;43:200–206. [Google Scholar]