Abstract
Posterior cruciate ligament (PCL) injuries associated with multiple ligament injuries can be easily diagnosed, but isolated PCL tears are less symptomatic, very difficult to diagnose, and frequently misdiagnosed. If a detailed investigation of the history of illness suggests a PCL injury, careful physical examinations including the posterior drawer test, dial test, varus and valgus test should be done especially if the patient complains of severe posterior knee pain in >90° of flexion. Vascular assessment and treatment should be done to avoid critical complications. An individualized treatment plan should be established after consideration of the type of tear, time after injury, associated collateral ligament injuries, bony alignment, and status of remnant. The rehabilitation should be carried out slower than that after anterior cruciate ligament reconstruction.
Keywords: Posterior cruciate ligament, Diagnosis, Treatment
Introduction
Posterior cruciate ligament (PCL) injuries often go undiagnosed because a popping sound is not as distinctive as in anterior cruciate ligament (ACL) injuries and swelling is not severe in sports injuries. However, early diagnosis and treatment is critical to prevent serious complications that can result from combined vascular injuries. Compared to the ACL, the PCL has a high potential for spontaneous healing1-6), thus requires different treatment approaches. For proper treatment, the surgeon should be fully aware of the collateral ligament injuries that affect posterior stability, lower limb alignment, and the relationship between the posterior tibial slope and ligament instability.
In this review, we describe and discuss the diagnosis and treatment methods of PCL injuries based on our experience and a review of the literature.
Diagnosis and Treatment
1. Diagnosis
1) History of illness and mechanism of injury
The most common mechanisms of PCL injuries include pretibial trauma, hyperflexion, and hyperextension of the knee4). Fowler and Messieh7) reported that, isolated PCL injuries were common in athletes and hyperflexion was the most frequent mechanism of injury. In most of the PCL injuries caused by hyperflexion, the posteromedial bundle remains intact and only the anterolateral bundle is ruptured7,8). However PCL tears mostly occur in combination with other injuries. According to Fanelli and Edson9), about 95% of the PCL injuries in an emergency department setting were combined with other ligament injuries. The PCL can also be torn in a car accident because a posterior force is applied to the tibia when the knee in a flexed position hits the dashboard. This can be combined with posterolateral ligament injuries if the anteromedial aspect of the knee strikes the dashboard with a varus force applied10).
2) Physical examination
A careful vascular examination of the lower extremities is essential because a PCL injury can be accompanied by a popliteal artery injury. If the pulses are weak or the ankle-brachial index is ≤0.8, an intimal tear should be suspected and arteriography should be performed. If blood flow disruption below the knee is obvious, arteriography should be omitted to prevent delay in treatment10).
Acute PCL injuries present with joint swelling and about 10° to 20° of restriction in further flexion due to pain. Chronic PCL injuries may present with limited activity such as having difficulty in climbing slopes due to lethargy and pain in the anterior and medial areas of the knee rather than instability. The posterior drawer test is the most accurate test for PCL injuries. At 90° of knee flexion, posterior sagging of the tibia is observed on the affected side. If the tibia is pulled forward or the quadriceps is contracted with the knee flexed to 90° (quadriceps active test), anteroposterior instability of the knee is noted10). However, these tests can be unreliable for detecting acute PCL injuries with severe swelling11). In contrast, the sensitivity of the posterior drawer test increases for the detection of chronic PCL injuries because of the absence of swelling and pain in further flexion12).
A presence of ≥10 mm posterior translation requires tests for posterolateral ligament complex (PLC) injuries. The presence of tenderness and an arcuate fracture in fibula head suggest acute a PLC injury, but a diagnosis of chronic PLC injury should be based on various test results. In the dial test, the thigh-foot angle is measured with an external rotation force applied to the knees flexed to 30° and 90°. If the angle on the affected side is ≥10°-15° greater than the contralateral side at 30° of flexion only, at 90° of flexion only, and at both 30° and 90° of flexion, the diagnosis is an isolated PLC injury, an isolated PCL injury, and a combination of PCL and PLC injury, respectively. Posterior translation is greater in combined injuries of the PCL and PLC than in an isolated injury8,10,12).
Considering that the dial test can be misleading in cases of minor injuries13), it is recommended to reduce the tibia with an anterior force during the test. To better assess posterior subluxation of the tibia, the examiner should palpate with 4 fingers posterolateral translation of the posterolateral condyle of the tibia with respect to the posterolateral condyle of the femur with an assistant holding the knees flexed to 90° 4,14).
The posterolateral drawer test, external rotation recurvatum test, and reverse pivot shift test can also be used to assess injuries to the posterolateral structures. However, a positive external rotation recurvatum test is more indicative of an ACL injury than a PCL injury15) and the reverse pivot shift test should be used with care because the test may yield positive results in about 30% of normal knees12).
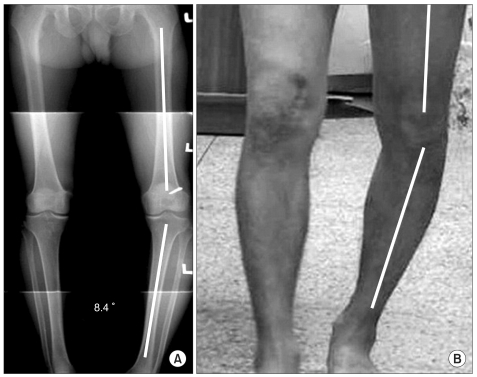
Combined PLC injuries have much influence on the prognosis of PCL injury treatments. This is why the exact assessment of PLC injuries is important. However, it may be impossible to detect PLC injuries with a single test. Therefore, it is recommended to palpate the articular surface during various tests with suspicion of PLC injuries and determine the diagnosis based on the test results. Besides, the overall lower limb alignment should be assessed for varus malalignment and gait for instability such as varus thrust (Fig. 1)10,16).
Fig. 1.
(A) Varus aligned lower limb. (B) Varus thrust during gait.
3) Imaging
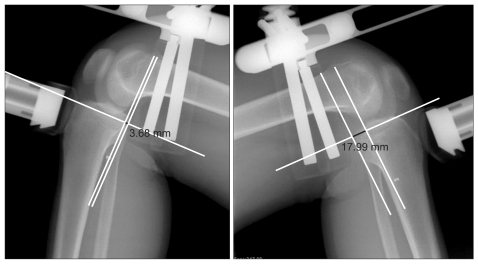
Radiography is a valuable tool in diagnosing PCL injuries. The presence of a fracture can be determined on the anteroposterior, lateral, and Merchant views of the knee. The lower limb alignment, especially the presence of varus malalignment, can be evaluated on the standing radiographs. The presence and degree of instability can be assessed on stress radiographs. Especially, PCL injuries can be best visualized on posterior stress radiographs (Fig. 2)10,17,18). A presence of ≥10 mm posterior translation on posterior stress radiographs may suggest posterolateral ligament injuries combined with PCL injuries19).
Fig. 2.
Posterior draw stress view.
External rotation valgus stress radiogram is useful in assess ing PLC injuries20) and ultrasound can be used to evaluate the degree of instability21).
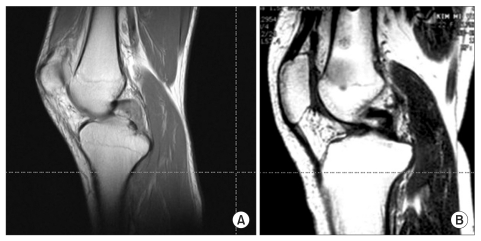
Magnetic resonance imaging (MRI) has 96 to 100% accuracy for the detection of acute PCL injuries and can determine the location and severity of an injury and other damages to the cartilage and ligaments. Bone bruise patterns on MRI can be helpful in identifying the mechanism of injury. In acute PCL injuries, bone bruises are often located anterior to the tibia (Fig. 3). In chronic PCL injuries (Fig. 4), MRI scans may appear to be normal if the ligament healed spontaneously10). The popliteofibular ligament, an important structure in posterolateral instability of the knee, may not be clearly visualized on MRI22).
Fig. 3.
Bone bruise pattern in posterior cruciate ligament (PCL) injury. Arrow indicates bone bruise in the anterior portion of lateral tibial plateu that occurred in a patient with grade III PCL injury shows vector of force and injury mechanism.
Fig. 4.
(A) In acute posterior cruciate ligament (PCL) injuries, T1-weighted sagittal view, ligament has been torn with the frayed ends being clearly visualized. (B) In chronic PCL injuries, T1-weighted sagittal view, MRI scans may appear normal when grade I and II injuries are present.
4) Instrumented examination
The KT-1000 can be used to assess anteroposterior instability, but may be less accurate than Telos stress radiography12).
5) Arthroscopy
PCL lesions can be visualized with arthroscopy in acute cases. They may appear to be healed in chronic cases, but arthroscopy will reveal ACL pseudolaxity where the ACL appears lax due to posterior translation of the proximal tibia but the laxity resolves when an anterior force is applied to the tibia. Care should be taken not to misinterpret this pseudolaxity as an indication of ACL injuries. An abnormal contact can also be observed between the medial femoral condyle and the medial meniscus anterior horn due to the posterior translation of the proximal tibia.
PLC ruptures can be visualized with arthroscopy or evidenced by hemorrhage in some cases. However, it is more common to identify a "lateral gutter drive through sign" that can be observed by inserting the arthroscope into the posterolateral aspect of the knee or tension of the popliteus tendon23,24).
2. Treatment Principles
Conservative treatment is indicated for PCL injuries with 5 to 10 mm posterior instability (grade I and II) and surgical treatment is recommended for PCL injuries with ≥10 mm posterior instability (grade III) or with combined collateral ligament injuries or avulsion fractures10). However, the natural history, healing potential, and the influence of remnant, alignment, and posterolateral ligaments should be taken into consideration in determining treatment plans.
1) Natural history
Surgical treatment of less than moderate isolated PCL injuries (grade I and II) still remains controversial. Short-term results of nonoperative treatment have been reported successful in many studies. However, there are studies showing unfavorable long-term results including degeneration of the tibiofemoral cartilage in the medial compartment and increased tibiofemoral pressure and meniscal strain25-27), which eventually led to arthritis. In the study of Dejour et al.28), osteoarthritis occurred eventually in the patients in whom the isolated rupture of the PCL was functionally well tolerated for 3 to 18 months. According to Clancy et al.29), degenerative arthritis was observed in 80% of the patients after nonoperative treatment. Likewise, nonoperative treatment of grade I and II isolated PCL injuries have been associated with functional limitation and early degenerative arthritis in many studies. Therefore, surgical treatment of grade II PCL injuries can be considered as an option if a hot spot is shown on bone scan of highly active patients10) or the surgeon is competent1).
2) Healing potential
Acute PCL tears, especially those within substance, can be treated with conservative measures because of the ligament's high healing potential2-6). However, when PCL injuries are combined with PLC injuries, the PCL should be treated with reconstruction and the PLC with repair or reconstruction because the PLC tears do not heal with conservative treatment, which eventually leads to instability and cartilage degeneration30).
3) Remnant
Remnants are observed in most PCL injuries because the ligament has a high chance of spontaneous healing3-6,31,32). It has been known that preservation of the remnant fibers during operative treatment of PCL injuries plays a pivotal role in obtaining successful outcomes1,32,33). If remnant fibers are observed, retensioning of the remnant PCL fiber31), stent procedure32), single-bundle or double-bundle PCL reconstruction with PCL remnant preservation, albeit technically challenging, can be performed depending on the quality of the PCL remnants. If no remnant is present, albeit controversial34), double-bundle PCL reconstruction may be an appropriate procedure4,35).
4) Alignment
Left untreated, varus malalignment may increase the risk of treatment failure after PLC and PCL reconstruction. Therefore, if varus malalignment is present, an osteotomy should be carried out even in acute cases of PCL combined with PLC injuries16,36). Improvements can be made with varus malalignment correction alone and then subsequent reconstruction procedures may become unnecessary. An increase in tibial slope results in an anterior shift of the resting position of the tibia relative to the femur and anterior tibial translation under an axial load11,37). A varus osteotomy may improve posterolateral instability and make PLC reconstruction unnecessary38,39).
5) Collateral ligaments
Medial collateral ligament injuries are rare but may have an influence on the PCL. Therefore, reconstruction is required if a ≥12 mm increase in the medial gap is observed at 30° of knee flexion40,41). Posterolateral ligament injuries should be aggressively treated because left untreated, it results in severe posterior translation that has been associated with most of the PCL reconstruction failure cases42-44). The classification of posterolateral structure injuries has yet to be established. According to Fanelli et al., type A injury was defined as increased external rotation only due to popliteus tendon and popliteofibular ligament injuries, type B as ≤10 mm varus instability and increased external rotation, and type C as ≥10 mm varus instability and increased external rotation. They suggested that type A and B injuries can be conservatively treated and type C injuries should be surgically treated. Kannus45) also recommended operative treatment for grade III injuries. The most common surgical reconstruction procedures include primary repair, posterolateral complex advancement, biceps femoris tendon tenodesis, and anatomic posterolateral corner reconstruction45-47).
6) Rehabilitation
In contrast to ACL rehabilitation, PCL rehabilitation should be carried out at a slow pace48). Depending on the patient's condition and the surgeon's intraoperative judgment, appropriate joint exercises that allow early joint motion within a safe range should be determined. Although some differences exist among studies in terms of the appropriate timing and method, the rule of thumb is as follows. Postoperatively, there is a tendency to posterior translation in flexion of the knee, especially in active flexion. In addition, the tendon graft becomes weak by the 6th postoperative week and requires protection. Therefore, during the 2nd and 3rd postoperative week, the knee should be immobilized in an extended position with a padded posterior splint or a long leg brace. Quadriceps femoris muscle strengthening exercise and straight leg raising exercise are started immediately after surgery for synergy effect. To prevent joint adhesion, joint exercises should be performed in anteroposterior and mediolateral directions. Passive flexion exercise is performed with the tibia pulled forward until 90° of flexion is achieved by the 4th to 6th postoperative week. For isolated PCL injuries, weight bearing can be helpful in maintaining muscle strength even before the 6th postoperative week without the risk of posterior translation because the tibial slope increases the tendency to anterior tibial translation. However, for combined PCL injuries, partial-weight bearing is allowed soon after surgery and progressed to full weight-bearing at the 6th to 12th postoperative week. In addition, passive range of motion should be gradually increased to 140° of flexion avoiding active contraction of the hamstrings. From the 12th postoperative week when collagen fibers become organized, flexion exercise is permitted, light jogging is allowed 3 to 6 months after surgery, and sports activities are allowed 6 months after surgery2,4,48).
Conclusions
An early and accurate diagnosis of a PCL rupture should be based on the history of illness, vascular examination to exclude vascular damages, and physical examination for the assessment of PCL and collateral ligament injuries and radiographic examination. Once a diagnosis is established, appropriate treatment plans should be determined according to the time of injury, rupture pattern, presence of remnant, combined collateral ligament injuries, alignment, and tibial slope.
References
- 1.Ahn JH, Yang HS, Jeong WK, Koh KH. Arthroscopic transtibial posterior cruciate ligament reconstruction with preservation of posterior cruciate ligament fibers: clinical results of minimum 2-year follow-up. Am J Sports Med. 2006;34:194–204. doi: 10.1177/0363546505279915. [DOI] [PubMed] [Google Scholar]
- 2.Jung YB, Kim JS, Jung HJ, Jeong PH. Conservative treatment of acute isolated injuries to the posterior cruciate ligament: prospective study. J Korean Knee Soc. 2002;14:193–199. [Google Scholar]
- 3.Jung YB, Kwon YS, Jin WJ, Kim TH, Lee TJ. Healing potential of the transected posterior cruciate ligament of the rabbit. J Korean Knee Soc. 2002;14:90–102. [Google Scholar]
- 4.Jung YB, Lee YS. Current trend of treatment of PCL and PL corner injury. J Korean Arthrosc Soc. 2005;9:1–8. [Google Scholar]
- 5.Jung YB, Tae SK, Yang DL, Han JN, Song IS, Kang IK. Magnetic resonance imaging on posterior cruciate ligament injury: van the PCL hea. J Korean Knee Soc. 2000;12:172–179. [Google Scholar]
- 6.Lee BK, Eom GS, Kee YC. Posterior laxity after conservative treatment of the acute injured posterior cruciate ligament. J Korean Knee Soc. 2003;15:97–101. [Google Scholar]
- 7.Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15:553–557. doi: 10.1177/036354658701500606. [DOI] [PubMed] [Google Scholar]
- 8.Harner CD, Hoher J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26:471–482. doi: 10.1177/03635465980260032301. [DOI] [PubMed] [Google Scholar]
- 9.Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients: Part II. Arthroscopy. 1995;11:526–529. doi: 10.1016/0749-8063(95)90127-2. [DOI] [PubMed] [Google Scholar]
- 10.Wind WM, Jr, Bergfeld JA, Parker RD. Evaluation and treatment of posterior cruciate ligament injuries: revisited. Am J Sports Med. 2004;32:1765–1775. doi: 10.1177/0363546504270481. [DOI] [PubMed] [Google Scholar]
- 11.Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35:1443–1449. doi: 10.1177/0363546507304665. [DOI] [PubMed] [Google Scholar]
- 12.Lubowitz JH, Bernardini BJ, Reid JB., 3rd Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med. 2008;36:577–594. doi: 10.1177/0363546507312641. [DOI] [PubMed] [Google Scholar]
- 13.Bae JH, Choi IC, Suh SW, Lim HC, Bae TS, Nha KW, Wang JH. Evaluation of the reliability of the dial test for posterolateral rotatory instability: a cadaveric study using an isotonic rotation machine. Arthroscopy. 2008;24:593–598. doi: 10.1016/j.arthro.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Jung YB, Lee YS, Jung HJ, Nam CH. Evaluation of posterolateral rotatory knee instability using the dial test according to tibial positioning. Arthroscopy. 2009;25:257–261. doi: 10.1016/j.arthro.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade RF, Ly TV, Griffith C. The external rotation recurvatum test revisited: reevaluation of the sagittal plane tibiofemoral relationship. Am J Sports Med. 2008;36:709–712. doi: 10.1177/0363546507311096. [DOI] [PubMed] [Google Scholar]
- 16.Noyes FR, Barber-Westin SD, Albright JC. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. Am J Sports Med. 2006;34:1419–1430. doi: 10.1177/0363546506287743. [DOI] [PubMed] [Google Scholar]
- 17.Margheritini F, Mancini L, Mauro CS, Mariani PP. Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy. 2003;19:706–711. doi: 10.1016/s0749-8063(03)00399-2. [DOI] [PubMed] [Google Scholar]
- 18.Schulz MS, Russe K, Lampakis G, Strobel MJ. Reliability of stress radiography for evaluation of posterior knee laxity. Am J Sports Med. 2005;33:502–506. doi: 10.1177/0363546504269723. [DOI] [PubMed] [Google Scholar]
- 19.Sekiya JK, Whiddon DR, Zehms CT, Miller MD. A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90:1621–1627. doi: 10.2106/JBJS.G.01365. [DOI] [PubMed] [Google Scholar]
- 20.Chang CB, Seong SC, Lee S, Yoo JH, Park YK, Lee MC. Novel methods for diagnosis and treatment of posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 2007;89(Suppl 3):2–14. doi: 10.2106/JBJS.G.00582. [DOI] [PubMed] [Google Scholar]
- 21.Sekiya JK, Swaringen JC, Wojtys EM, Jacobson JA. Diagnostic ultrasound evaluation of posterolateral corner knee injuries. Arthroscopy. 2010;26:494–499. doi: 10.1016/j.arthro.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 22.LaPrade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med. 2000;28:191–199. doi: 10.1177/03635465000280020901. [DOI] [PubMed] [Google Scholar]
- 23.Feng H, Zhang H, Hong L, Wang XS, Zhang J. The "lateral gutter drive-through" sign: an arthroscopic indicator of acute femoral avulsion of the popliteus tendon in knee joints. Arthroscopy. 2009;25:1496–1499. doi: 10.1016/j.arthro.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Ferrari DA. Arthroscopic evaluation of the popliteus: clues to posterolateral laxity. Arthroscopy. 2005;21:721–726. doi: 10.1016/j.arthro.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 25.Pearsall AW, 4th, Hollis JM. The effect of posterior cruciate ligament injury and reconstruction on meniscal strain. Am J Sports Med. 2004;32:1675–1680. doi: 10.1177/0363546504265937. [DOI] [PubMed] [Google Scholar]
- 26.Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ. Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees. Arthroscopy. 2003;19:262–268. doi: 10.1053/jars.2003.50037. [DOI] [PubMed] [Google Scholar]
- 27.Van de Velde SK, Bingham JT, Gill TJ, Li G. Analysis of tibiofemoral cartilage deformation in the posterior cruciate ligament-deficient knee. J Bone Joint Surg Am. 2009;91:167–175. doi: 10.2106/JBJS.H.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dejour H, Walch G, Peyrot J, Eberhard P. The natural history of rupture of the posterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot. 1988;74:35–43. [PubMed] [Google Scholar]
- 29.Clancy WG, Jr, Shelbourne KD, Zoellner GB, Keene JS, Reider B, Rosenberg TD. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg Am. 1983;65:310–322. [PubMed] [Google Scholar]
- 30.Laprade RF, Wentorf FA, Olson EJ, Carlson CS. An in vivo injury model of posterolateral knee instability. Am J Sports Med. 2006;34:1313–1321. doi: 10.1177/0363546506286785. [DOI] [PubMed] [Google Scholar]
- 31.Jung YB, Jung HJ, Tae SK, Lee YS, Yang DL. Tensioning of remnant posterior cruciate ligament and reconstruction of anterolateral bundle in chronic posterior cruciate ligament injury. Arthroscopy. 2006;22:329–338. doi: 10.1016/j.arthro.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 32.Jung YB, Jung HJ, Song KS, Kim JY, Lee HJ, Lee JS. Remnant posterior cruciate ligament-augmenting stent procedure for injuries in the acute or subacute stage. Arthroscopy. 2010;26:223–229. doi: 10.1016/j.arthro.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 33.Lee BK, Eom GS, Lee JY, Cha JH. Posterior cruciate ligament reconstruction using hamstring tendon with preservation of posterior cruciate ligament remnant. J Korean Knee Soc. 2002;14:200–206. [Google Scholar]
- 34.Kohen RB, Sekiya JK. Single-bundle versus double-bundle posterior cruciate ligament reconstruction. Arthroscopy. 2009;25:1470–1477. doi: 10.1016/j.arthro.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL. Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med. 2000;28:144–151. doi: 10.1177/03635465000280020201. [DOI] [PubMed] [Google Scholar]
- 36.LaPrade RF, Wentorf F. Diagnosis and treatment of posterolateral knee injuries. Clin Orthop Relat Res. 2002;(402):110–121. doi: 10.1097/00003086-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32:376–382. doi: 10.1177/0363546503258880. [DOI] [PubMed] [Google Scholar]
- 38.Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med. 2007;35:1844–1850. doi: 10.1177/0363546507304717. [DOI] [PubMed] [Google Scholar]
- 39.Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32:60–70. doi: 10.1177/0363546503258907. [DOI] [PubMed] [Google Scholar]
- 40.Noyes FR, Barber-Westin SD. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33:646–654. doi: 10.1177/0363546504271210. [DOI] [PubMed] [Google Scholar]
- 41.Petersen W, Zantop T, Loerch S, Schanz S, Raschke M. Effect of sectioning the posteromedial structures on posterior tibial translation in the PCL deficient knee (SS-56) Arthroscopy. 2007;23:e28–e29. [Google Scholar]
- 42.Sekiya JK, Haemmerle MJ, Stabile KJ, Vogrin TM, Harner CD. Biomechanical analysis of a combined double-bundle posterior cruciate ligament and posterolateral corner reconstruction. Am J Sports Med. 2005;33:360–369. doi: 10.1177/0363546504268039. [DOI] [PubMed] [Google Scholar]
- 43.Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989;(246):208–216. [PubMed] [Google Scholar]
- 44.Wiley WB, Askew MJ, Melby A, 3rd, Noe DA. Kinematics of the posterior cruciate ligament/posterolateral corner-injured knee after reconstruction by single- and double-bundle intra-articular grafts. Am J Sports Med. 2006;34:741–748. doi: 10.1177/0363546505282615. [DOI] [PubMed] [Google Scholar]
- 45.Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83–88. doi: 10.1177/036354658901700114. [DOI] [PubMed] [Google Scholar]
- 46.Krukhaug Y, Molster A, Rodt A, Strand T. Lateral liga ment injuries of the knee. Knee Surg Sports Traumatol Arthrosc. 1998;6:21–25. doi: 10.1007/s001670050067. [DOI] [PubMed] [Google Scholar]
- 47.Noyes FR, Barber-Westin SD. Treatment of complex injuries involving the posterior cruciate and posterolateral ligaments of the knee. Am J Knee Surg. 1996;9:200–214. [PubMed] [Google Scholar]
- 48.Fanelli GC. Posterior cruciate ligament rehabilitation: how slow should we go? Arthroscopy. 2008;24:234–235. doi: 10.1016/j.arthro.2007.09.009. [DOI] [PubMed] [Google Scholar]