Abstract
Novel methods, such as Internet-based interventions, are needed to combat the spread of HIV. While past initiatives have used the Internet to promote HIV prevention, the growing popularity, decreasing digital divide, and multi-functionality of social networking sites, such as Facebook, make this an ideal time to develop innovative ways to use online social networking sites to scale HIV prevention interventions among high-risk groups. The UCLA HOPE [Harnessing Online Peer Education] study is a longitudinal experimental study to evaluate the feasibility, acceptability, and preliminary effectiveness of using social media for peer-led HIV prevention, specifically among African American and Latino Men who have Sex with Men (MSM). No curriculum currently exists to train peer leaders in delivering culturally aware HIV prevention messages using social media. Training was created that adapted the Community Popular Opinion Leader (C-POL) model, for use on social networking sites. Peer leaders are recruited who represent the target population and have experience with both social media and community outreach. The curriculum contains the following elements: discussion and role playing exercises to integrate basic knowledge of HIV/AIDS, awareness of sociocultural HIV/AIDS issues in the age of technology, and communication methods for training peer leaders in effective, interactive social media-based HIV prevention. Ethical issues related to Facebook and health interventions are integrated throughout the sessions. Training outcomes have been developed for long-term assessment of retention and efficacy. This is the first C-POL curriculum that has been adapted for use on social networking websites. Although this curriculum has been used to target African American and Latino MSM, it has been created to allow generalization to other high-risk groups.
Keywords: HIV prevention, social networking, facebook, c-pol, popular opinion leader
Introduction
The Internet has emerged as a popular setting for MSM to seek sexual partners. An online survey of MSM found that 82% had used the Internet to find a sexual partner (Chiasson et al., 2007). MSM cite that they are able to find sexual partners without fear of discrimination (Chiasson et al., 2007; Kim, Kent, McFarland, & Klausner, 2001; Ross, Rosser, & Stanton, 2004). Furthermore, MSM are more likely to negotiate sexual preferences and disclose HIV status on the Internet (Bolding, Davis, Hart, Sherr, & Elford, 2005; Carballo-Diéguez, Miner, Dolezal, Rosser, & Jacoby 2006; Liau, Millett, & Marks, 2006). However, Men who use the Internet to seek Sex with Men (MISM) are more likely to engage in UAI and have multiple sex partners (Benotsch, Kalichman, & Cage, 2002; Carballo-Diéguez et al., 2006; Chiasson et al., 2007; Kim et al., 2001; Liau et al., 2006; McFarlane, Bull, & Rietmeijer, 2000). MISM are therefore a population at-risk for sexually transmitted infections (STIs) and HIV/AIDS.
Since MISM are at risk for HIV/AIDS, yet may be more open to discuss sexual issues without fear of stigma, there is an opportunity to use the Internet to promote HIV prevention. The Internet provides a cost-effective method to reach MSM across a wide geographic range, including those who are not close to HIV services (Bowen, Williams, Daniel, & Clayton, 2008). An online survey of men who visited gay chat sites had favorable views towards health care workers using the sites (Bolding, Davis, Sherr, Hart, & Elford, 2004). Interventions that utilize online education modules have shown significant decreases in UAI (Bowen et al., 2008; Chiasson, Shaw, Humberstone, Hirshfield, & Hartel, 2009; Rosser et al., 2010). Taken together, the Internet appears to be an effective method of delivering HIV prevention.
While current online HIV prevention research has been on predominantly Caucasian participants, the majority of risk in the United States falls on African-American and Latino MSM (CDC, 2007). Cultural barriers in the African American and Latino communities provide additional challenges to HIV prevention, including difficulty in discussing issues such as homosexuality, drug use, or sex outside of marriage (Gonzalez et al., 2009; Laurencin, Christensen, & Taylor, 2008; Williams 2003). Gender roles (such as the Latino concept of “machismo”) may motivate sexual risk behavior and create stigma that prevents discussion and HIV testing (Gonzalez et al., 2009; Jarama, Kennamer, Poppen, Hendricks, & Bradford, 2005; Operario, Smith, & Kegeles, 2008). In addition, lower socioeconomic status may limit an individual’s access to healthcare and HIV services (Gonzalez et al., 2009; Laurencin et al., 2008; Loue, 2006).
It has been suggested that these ethnicities have not been represented in these studies due to disparities in Internet access (Viswanath & Kreuter, 2007). However, a recent survey has shown no apparent ethnic differences in social media use (Chou, Hunt, Beckjord, Moser, & Hesse, 2009). Moreover, as Internet access increases among these ethnicities, studies have shown that they are also at risk for HIV. The Men’s INTernet Sex (MINTS) study was an online survey to evaluate Latino MSM use of the Internet to seek sexual partners. It showed that 98.5% had used the Internet to find a sexual partner, of which 43% had UAI (Rosser et al., 2009a). The second phase of the study, MINTS-II, evaluated sexual risk across several ethnicities, and showed a significantly increased risk among African American MSM to have UAI (Rosser et al., 2009b).
The UCLA HOPE (Harnessing Online Peer Education) study seeks to determine the acceptability, feasibility, and preliminary effectiveness of using online social networks (Facebook.com) to scale the Community Popular Opinion Leader (C-POL) model to increase HIV prevention among high-risk populations, with a focus on African American and Latino men who have sex with men (MSM). Participants join an online Facebook group related to HIV prevention and interact with community peer leaders trained in the fundamentals of HIV prevention and behavior change over a 12-week period. The data collected from this study are compared to results from previous studies of community-based testing to preliminarily determine whether social networks can be used to scale community-based HIV prevention methods.
While previous Internet studies have used a “Web 1.0” interface, the HOPE study uses the “Web 2.0” format on Facebook. In “Web 1.0,” the communication is one-way; that is, the user is a passive participant who receives the information from a single source (Thackeray, Neiger, Hanson & McKenzie, 2008). However, in “Web 2.0” there is two-way communication, in which the users have greater control over their content and experience, and have the capability to connect to others over the Internet for advice and support. Websites include blogs, wikis and social networking such as Facebook and Twitter. The result is an “architecture of participation,” in which social networking creates a dynamic experience where users are engaged and site retention is high (Bennett & Glasgow, 2009). Social media sites are largely visited by youth, those most at risk of STI/HIV infection (Young & Rice, 2011; Rice, Monro, Adhikari, & Young, 2010). Facebook receives exceedingly more visits in a month than gay websites, the CDC or HIV testing sites (Rietmeijer & McFarlane, 2009). With such statistics, surprisingly there is a lack of research pertaining to health promotion on social media sites (Bennett & Glasgow, 2009; Rietmeijer & McFarlane, 2009). Facebook has become an expansive online social community, and the HOPE study seeks to utilize this opportunity for HIV prevention.
To train peer leaders in the HOPE study, a new curriculum was created that focused on how to utilize social media websites for outreach to at-risk populations. We describe here the components of the curriculum and the method of evaluation.
Training Elements
Training of peer leaders is based on the Community Popular Opinion Leader (C-POL) model, in which influential members in a community can motivate change in behavior (Rogers, 1962). They can serve to legitimize a given intervention, provide feedback to outreach programs, act as role models, deliver health messages, and remain active in the community, adding stability to the intervention (Valente & Pumpuang, 2007). The C-POL approach has been extensively utilized and studied in HIV prevention both domestically and internationally (Amirkhanian et al., 2005; Jones et al., 2008; Kelly et al., 1991; Kelly et al., 1997; Kelly et al., 2006; McQuiston & Uribe, 2001; NIMH Collaborative HIV/STD Prevention Trial Group, 2010). While C-POL studies have traditionally targeted white MSM, more recent studies have adapted the C-POL method for Latino and African-American populations by including training that emphasized cultural barriers to HIV prevention (Jones et al., 2008; McQuiston & Uribe, 2001; Somerville, Diaz, Davis, Coleman, & Taveras, 2006). The HOPE study is the first to adapt the C-POL method to social networking sites.
Peer leader training for the HOPE Study required a curriculum that was not only culturally sensitive, but that also included role playing and educational modules that demonstrate how to maximize the potential of social media sites to deliver HIV prevention messages. Since the study “setting” is Facebook, all role-playing is completed on peer leader Facebook group pages to create a realistic experience. In this and other C-POL studies, the goal is for POLs to feel comfortable initiating everyday conversations about a sensitive topic like HIV/AIDS, while reinforcing the importance of their efforts. To do so, this requires interactive discussion, modeling, role-play and repetition (NIMH Collaborative HIV/STD Prevention Trial Group, 2007).
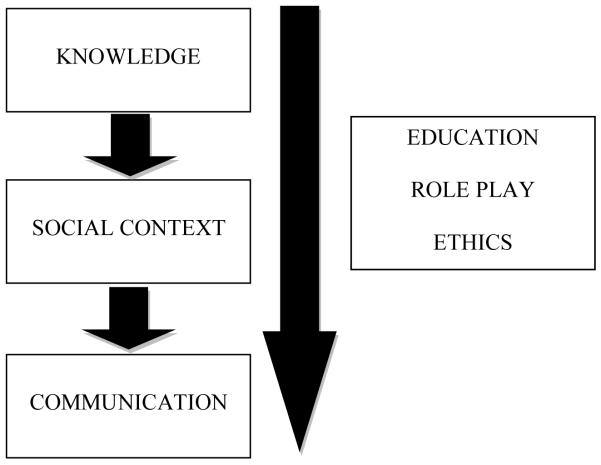
Training peer leaders in the HOPE study involved the following elements (Figure 1):
(1) Recruitment
(2) Knowledge
(3) Social Context
(4) Communication
(5) Ethics
Figure 1.
Elements of HOPE peer leader training. Short arrow signifies transition to next session, and long arrow indicates a component that is utilized in every session.
Recruitment
In order to obtain C-POLs, criteria for peer leaders in the HOPE Study are:
(1) Male
(2) Over 18 years old
(3) African American or Latino
(4) Has had sex with a man in the last 12 months
(5) Lives in Los Angeles area
(6) Experience using Facebook
(7) Experience as a POL or ability to be a leader in their community
(8) Interest is using social networking to educate others about health
Recruitment occurs online and by contacting community outreach organizations. Facebook and Myspace groups related to health outreach are asked to post fliers describing the study and eligibility criteria. Community-based outreach organizations are given similar fliers to distribute. Peer leaders are randomly assigned to either a Facebook group that would discuss topics in HIV/AIDS, or a control group that discussed general health topics.
Knowledge
In the first session, peer leaders are taught core facts about their group’s topic. Peer leaders in the HIV/AIDS group learn about HIV/AIDS prevalence in the MSM community, methods of transmission, prevention strategies, and myths around HIV/AIDS. Peer leaders in the control arm are taught about topics in general health, including nutrition, benefits of exercise, mental health and substance abuse. Both groups also receive instruction on home-based HIV testing kits that are available to all participants.
Role playing in the knowledge session seeks to teach peer leaders how to translate technical information into basic ideas suitable for social media. Each peer leader posts on the Facebook Wall a fact that they learned during the educational module. It is emphasized that Wall posts are a useful tool for providing general information available to all members in a group. Throughout the exercise, peer leaders can read each other’s posts to gain ideas and help each other create effective messages. In addition, peer leaders are asked to post five website links related to facts in HIV/AIDS or general health. The goal is to empower peer leaders to take advantage of useful sources on the Internet to share with the group while creating a list of trusted websites for accurate information about their topics (Young, 2011).
Social Context
This session focuses on stigma and the cultural barriers to prevention. Peer leaders learn about the basic epidemiology facing Latino and African American MSM, the unique cultural obstacles, and the consequences of stigma. They then discuss how to have a conversation with a person that is both sensitive to stigma and culture. In particular, the training attends to how social media (compared to offline communication) can be used to facilitate communication about stigmatizing or sensitive topics. Peer leaders in the control arm are taught about the general health risks of African Americans and Latinos, including diabetes, hypertension and obesity.
Before the session begins, the group is asked to utilize the “Group Chat” feature on Facebook. The training coordinator then begins a sentence “Javier, who works at the LGBT center, was walking down the street when he bumped into his friend. Javier asked how he was doing.” Each peer leader is then asked to provide a sentence to continue the story. The story, as created by the group, explores issues related to stigma and culture that the friend was having because he is a Latino MSM. This exercise seeks to encourage the topic of culture in their discussions and build comfort in addressing these issues, while describing how the chat feature can be utilized for more sensitive conversations. The session ends with one-on-one Facebook chats between peer leaders to reinforce these concepts.
Communication
The creation of effective health promotion messages is key to the C-POL method. Prior to this session, peer leaders are asked to try to initiate a conversation with current Facebook friends about HIV/AIDS prevention. During discussion, peer leaders talk about obstacles and receive feedback from the group. They then brainstorm methods to initiate a conversation and build trust with members in the Facebook group. Moreover, they practice “Facebook etiquette,” such as proper language, use of emoticons, and when to Wall post versus send a message (Figure 2).
Figure 2.
Examples of how features on Facebook can be used for HIV/AIDS prevention and education
With these ideas, peer leaders are asked to enter the Facebook group page and list short messages that can be used to attract participants’ attention and initiate further discussion (Table 1). This exercise seeks to build comfort in initiating conversations with the participants while encouraging the peer leaders to collaborate throughout the study to communicate health messages effectively.
Table 1.
Translating key concepts into Facebook messages. Examples of how the major educational elements can be adapted to the more casual setting of a social networking site such as Facebook.
| Topic | Key Concepts | Examples of Facebook Posts |
|---|---|---|
| Knowledge | Epidemiology, Signs and Symptoms, Testing, Treatment and Prevention Methods |
Wall post: Who can list the ways you can transmit HIV? |
|
Sharing a Link: I just found this amazing video talking about HIV symptoms, check it out! |
||
| Social Context | Challenges to HIV Prevention, Epidemiology of High Risk Groups, Cultural Barriers, Stigma |
Wall Post: Sometimes it’s really hard to tell people I’m gay. Anyone else feel the same way? |
|
Chat: Hi, I saw on the wall that you’re having a hard time with your family, do you want to talk about it? |
||
| Communication | How to Initiate a Conversation, Online Etiquette |
Wall Post: I’ve finally started this great exercise routine, send me a message if you want to find out more! |
|
Chat: Do you have a partner? I’d love to learn about him! |
||
Ethics
The use of social media in health promotion has lead to new ethical considerations that must be integrated into training and study protocol to ensure proper protection and support of peer leaders and participants. A recent case report outlined the potential ethical issues of using Facebook for HIV prevention (Bull et al., 2011). This included informed consent, comprehension of procedures, equity given a potential “digital divide” to internet access, confidentiality, and HIPAA data security.
These topics are addressed throughout the training process for the HOPE study. Prior to the first session, all peer leaders complete informed consent, and the study procedure is revisited during the introductory training session to ensure comprehension. While equity may remain an issue in Internet access, we have minimized the divide by focusing on populations that are considered to have decreased access. Confidentiality and privacy are central challenges on Facebook, with concerns of viewing private information, hacking, and changing privacy rules. The Facebook groups created for the study are customized to be “Secret,” so that the group cannot be found by search, members must be invited to join, and the group affiliation is not listed on a peer leader or participant’s profile page (Figure 2). In addition, participants are allowed to change their profile name or create a separate profile for the study to maintain anonymity. Importantly, peer leaders are instructed during the training to conduct all communication either on the group wall or in private messages and chats, and are given the responsibility to delete comments that are offensive to others or reveal private information. In addition, administrative staff monitors the group pages and have weekly discussions with peer leaders to ensure that privacy is upheld. Peer leaders and participants are notified when there are any changes in privacy settings by Facebook. All identifying data for the study complies with HIPAA regulations and storage of data is encrypted, firewall, and password protected. While more ethical issues will emerge as online research continues, we have sought to address major ethical concerns both in the training and study methods.
Evaluation
At the conclusion of the training, each peer leader should:
Develop proficiency in basic facts about HIV, with definite knowledge of the routes of transmission and methods of prevention
Be comfortable using Facebook, including writing a wall post, changing their status, writing a message, posting a link, and using the chat function
Understand that stigma and cultural traditions can create barriers in HIV prevention, and know how to approach those topics in a sensitive way
Learn basic communication skills to initiate conversations related to HIV/AIDS
Understand their role as a leader and responsibilities to regularly communicate with the members of the group
The HOPE training has been developed to allow for both quantitative and qualitative methods of evaluation. Prior to the training, peer leaders complete a questionnaire that includes past experience with Facebook features (Wall posts, chat, messaging and sharing a link) and a series of true/false questions related to HIV/AIDS and general health to evaluate knowledge. Comfort in using Facebook features and discussion of topics in sexual and general health is assessed using 5-point Likert scales (1 = very uncomfortable, 5 = very comfortable). After the training, the peer leaders complete the same questionnaire to evaluate changes in knowledge and comfort level. If peer leaders score above 70% in knowledge and are at least “comfortable” (score of 4 on Likert scale) in all categories, peer leaders receive certification and are assigned to a Facebook group.
To evaluate whether skills from the training are utilized throughout the study, peer leaders are asked to log their activities (i.e. wall post, message or chat). In addition, they are asked to indicate whether a given conversation is related to knowledge, stigma, or cultural context. Qualitative evaluation of Facebook wall discussions and interviews with peer leaders can provide further evidence of whether specific modalities from the training were utilized. As the HOPE study continues, the goal is to correlate the training outcomes with behavioral outcomes among participants, in order to determine the efficacy of the training in preparing peer leaders to initiate and effectively deliver HIV prevention messages on Facebook.
Conclusion
The Harnessing Online Peer Education (HOPE) study seeks to assess the feasibility, acceptability, and preliminary efficacy of using online social networks as a platform for delivering peer-led HIV prevention, with a particular focus on African American and Latino MSM. The primary stage of the study involves training peer leaders in effective HIV prevention communication, cultural awareness, and the role that technology can play in reducing stigma, and the use of the social networking site Facebook. As this is the first study to use Facebook for a peer-led HIV prevention intervention, we have described the creation of a new training curriculum that adapts the evidence-based Community Popular Opinion Leader (C-POL) method of HIV prevention to Facebook. To do so, we recruited peer leaders that matched the study population and had experience with both social networking and outreach. We then applied didactic discussions on knowledge, social context and communication to role playing exercises that occur entirely on Facebook. Concomitantly, we created a control arm that focuses on general health topics. In both groups, ethical considerations were emphasized to assure consent, comprehension of the study, equity and importantly privacy and confidentiality.
The creation of this curriculum is also meant as a tool for others interested in using social media in health promotion. Social networking sites such as Facebook are gaining immense popularity, and greater efforts should be made to utilize these sites for HIV prevention among a wide population. We hope that this guide creates a framework for how to deliver HIV prevention using social networking, and serves as the impetus for additional social-media based interventions.
Acknowledgements
The authors graciously acknowledge the National Institute of Mental Health (NIMH) for providing support for this project (Sean D. Young, K01 MH090884-01A1). The authors would greatly like to thank the support and guidance of Dr. Thomas Coates and Greg Szekeres.
References
- Amirkhanian YA, Kelly JA, Kabakchieva E, Kirsanova AV, Vassileva S, Takacs J, DiFranceisco WJ, McAuliffe TL, Khoursine RA, Mocsonaki L. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS. 2005;19(16):1897–905. doi: 10.1097/01.aids.0000189867.74806.fb. [DOI] [PubMed] [Google Scholar]
- Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health. 2009;30:273–92. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Arch Sex Behav. 2002 Apr;31(2):177–83. doi: 10.1023/a:1014739203657. 2002. [DOI] [PubMed] [Google Scholar]
- Bolding G, Davis M, Sherr L, Hart G, Elford J. Use of gay Internet sites and views about online health promotion among men who have sex with men. AIDS Care. 2004;16(8):993–1001. doi: 10.1080/09540120412331292453. [DOI] [PubMed] [Google Scholar]
- Bolding G, Davis M, Hart G, Sherr L, Elford J. Gay men who look for sex on the Internet: is there more HIV/STI risk with online partners? AIDS. 2005;19(9):961–8. doi: 10.1097/01.aids.0000171411.84231.f6. [DOI] [PubMed] [Google Scholar]
- Bowen AM, Williams ML, Daniel CM, Clayton S. Internet based HIV prevention research targeting rural MSM: feasibility, acceptability, and preliminary efficacy. J Behav Med. 2008;31(6):463–77. doi: 10.1007/s10865-008-9171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull SS, Breslin LT, Wright EE, Black SR, Levine D, Santelli JS. Case Study: An Ethics Case Study of HIV Prevention Research on Facebook: The Just/Us Study. J Pediatr Psychol. 2003 doi: 10.1093/jpepsy/jsq126. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carballo-Diéguez A, Miner M, Dolezal C, Rosser BR, Jacoby S. Sexual negotiation, HIV-status disclosure, and sexual risk behavior among Latino men who use the Internet to seek sex with other men. Arch Sex Behav. 2006;35(4):473–81. doi: 10.1007/s10508-006-9078-7. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Racial/ethnic disparities in diagnoses of HIV/AIDS--33 states, 2001-2005. MMWR Morb Mortal Wkly Rep. 2007;56(9):189–93. [PubMed] [Google Scholar]
- Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. J Acquir Immune Defic Syndr. 2007;44(2):235–43. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- Chiasson MA, Shaw FS, Humberstone M, Hirshfield S, Hartel D. Increased HIV disclosure three months after an online video intervention for men who have sex with men (MSM) AIDS Care. 2009;21(9):1081–9. doi: 10.1080/09540120902730013. [DOI] [PubMed] [Google Scholar]
- Chou WY, Hunt YM, Beckjord EB, Moser RP, Hesse BW. Social media use in the United States: implications for health communication. J Med Internet Res. 2009;11(4):e48. doi: 10.2196/jmir.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden MR, Gift TL, Brewer DD, Fleming M, Hogben M, St Lawrence JS, Thiede H, Handsfield HH. Peer referral for HIV case-finding among men who have sex with men. AIDS. 2006;20(15):1961–8. doi: 10.1097/01.aids.0000247118.74208.6a. [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Hendriksen ES, Collins EM, Durán RE, Safren SA. Latinos and HIV/AIDS: examining factors related to disparity and identifying opportunities for psychosocial intervention research. AIDS Behav. 2009;13(3):582–602. doi: 10.1007/s10461-008-9402-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarama SL, Kennamer JD, Poppen PJ, Hendricks M, Bradford J. Psychosocial, behavioral, and cultural predictors of sexual risk for HIV infection among Latino men who have sex with men. AIDS Behav. 2005;9(4):513–23. doi: 10.1007/s10461-005-9022-1. [DOI] [PubMed] [Google Scholar]
- Jones KT, Gray P, Whiteside YO, Wang T, Bost D, Dunbar E, Foust E, Johnson WD. Evaluation of an HIV prevention intervention adapted for Black men who have sex with men. Am J Public Health. 2008;98(6):1043–50. doi: 10.2105/AJPH.2007.120337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Diaz YE, Stevenson LY, Hauth AC, Brasfield TL, Kalichman SC, Smith JE, Andrew ME. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81(2):168–71. doi: 10.2105/ajph.81.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Sikkema KJ, McAuliffe TL, Roffman RA, Solomon LJ, Winett RA, Kalichman SC. Randomised, controlled, community-level HIV-prevention intervention for sexual-risk behaviour among homosexual men in US cities. Community HIV Prevention Research Collaborative. Lancet. 1997;350(9090):1500–5. doi: 10.1016/s0140-6736(97)07439-4. [DOI] [PubMed] [Google Scholar]
- Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16(2):139–50. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Amirkhanian YA, Kabakchieva E, Vassileva S, Vassilev B, McAuliffe TL, DiFranceisco WJ, Antonova R, Petrova E, Khoursine RA, Dimitrov B. Prevention of HIV and sexually transmitted diseases in high risk social networks of young Roma (Gypsy) men in Bulgaria: randomised controlled trial. BMJ. 2006;333(7578):1098. doi: 10.1136/bmj.38992.478299.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AA, Kent C, McFarland W, Klausner JD. Cruising on the Internet highway. J Acquir Immune Defic Syndr. 2001;28(1):89–93. doi: 10.1097/00042560-200109010-00013. [DOI] [PubMed] [Google Scholar]
- Kimbrough LW, Fisher HE, Jones KT, Johnson W, Thadiparthi S, Dooley S. Accessing social networks with high rates of undiagnosed HIV infection: The social networks demonstration project. Am J Public Health. 2009;99(6):1093–9. doi: 10.2105/AJPH.2008.139329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurencin CT, Christensen DM, Taylor ED. HIV/AIDS and the African-American community: a state of emergency. J Natl Med Assoc. 2008;100(1):35–43. doi: 10.1016/s0027-9684(15)31172-x. [DOI] [PubMed] [Google Scholar]
- Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sex Transm Dis. 2006;33(9):576–84. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- Loue S. Preventing HIV, eliminating disparities among Hispanics in the United States. J Immigr Minor Health. 2006;8(4):313–8. doi: 10.1007/s10903-006-9001-2. [DOI] [PubMed] [Google Scholar]
- McFarlane M, Bull SS, Rietmeijer CA. The Internet as a newly emerging risk environment for sexually transmitted diseases. JAMA. 2000;284(4):443–6. doi: 10.1001/jama.284.4.443. [DOI] [PubMed] [Google Scholar]
- McQuiston C, Uribe L. Latino recruitment and retention strategies: community-based HIV prevention. J Immigr Health. 2001;3(2):97–105. doi: 10.1023/A:1009565900783. [DOI] [PubMed] [Google Scholar]
- NIMH Collaborative HIV/STD Prevention Trial Group The community popular opinion leader HIV prevention programme: conceptual basis and intervention procedures. AIDS. 2007;21(Suppl 2):S59–68. doi: 10.1097/01.aids.0000266458.49138.fa. [DOI] [PubMed] [Google Scholar]
- NIMH Collaborative HIV/STD Prevention Trial Group Results of the NIMH collaborative HIV/sexually transmitted disease prevention trial of a community popular opinion leader intervention. J Acquir Immune Defic Syndr. 2010;54(2):204–14. doi: 10.1097/QAI.0b013e3181d61def. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Smith CD, Kegeles S. Social and psychological context for HIV risk in non-gay-identified African American men who have sex with men. AIDS Educ Prev. 2008;20(4):347–59. doi: 10.1521/aeap.2008.20.4.347. [DOI] [PubMed] [Google Scholar]
- Rice E, Monro W, Adhikari A, Young SD. Internet use, social networking, and HIV/AIDS risk for homeless adolescents. J Adolesc Health. 2010;47(6):610–3. doi: 10.1016/j.jadohealth.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rietmeijer CA, McFarlane M. Web 2.0 and beyond: risks for sexually transmitted infections and opportunities for prevention. Curr Opin Infect Dis. 2009;22(1):67–71. doi: 10.1097/QCO.0b013e328320a871. [DOI] [PubMed] [Google Scholar]
- Rogers E. Diffusion of Innovations. Free Press; New York: 1962. [Google Scholar]
- Ross MW, Rosser BR, Stanton J. Beliefs about cybersex and Internet-mediated sex of Latino men who have Internet sex with men: relationships with sexual practices in cybersex and in real life. AIDS Care. 2004;16(8):1002–11. doi: 10.1080/09540120412331292444. [DOI] [PubMed] [Google Scholar]
- Rosser BR, Miner MH, Bockting WO, Ross MW, Konstan J, Gurak L, Stanton J, Edwards W, Jacoby S, Carballo-Diéguez A, Mazin R, Coleman E. HIV risk and the Internet: results of the Men’s Internet Sex (MINTS) Study. AIDS Behav. 2009a;13(4):746–56. doi: 10.1007/s10461-008-9399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser BR, Oakes JM, Horvath KJ, Konstan JA, Danilenko GP, Peterson JL. HIV sexual risk behavior by men who use the Internet to seek sex with men: results of the Men’s Internet Sex Study-II (MINTS-II) AIDS Behav. 2009b;13(3):488–98. doi: 10.1007/s10461-009-9524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser BS, Oakes JM, Konstan J, Hooper S, Horvath KJ, Danilenko GP, Nygaard KE, Smolenski DJ. Reducing HIV risk behavior of men who have sex with men through persuasive computing: results of the Men’s Internet Study-II. AIDS. 2010;24(13):2099–107. doi: 10.1097/QAD.0b013e32833c4ac7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville GG, Diaz S, Davis S, Coleman KD, Taveras S. Adapting the popular opinion leader intervention for Latino young migrant men who have sex with men. AIDS Educ Prev. 2006;18(4, Suppl A):137–48. doi: 10.1521/aeap.2006.18.supp.137. [DOI] [PubMed] [Google Scholar]
- Thackeray R, Neiger BL, Hanson CL, McKenzie JF. Enhancing promotional strategies within social marketing programs: use of Web 2.0 social media. Health Promot Pract. 2008;9(4):338–43. doi: 10.1177/1524839908325335. [DOI] [PubMed] [Google Scholar]
- Valente TW, Pumpuang P. Identifying opinion leaders to promote behavior change. Health Educ Behav. 2007;34(6):881–96. doi: 10.1177/1090198106297855. [DOI] [PubMed] [Google Scholar]
- Viswanath K, Kreuter MW. Health disparities, communication inequalities, and eHealth. Am J Prev Med. 2007;32(5, Suppl):S131–3. doi: 10.1016/j.amepre.2007.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PB. HIV/AIDS case profile of African Americans: guidelines for ethnic-specific health promotion, education, and risk reduction activities for African Americans. Fam Community Health. 2003;26(4):289–306. doi: 10.1097/00003727-200310000-00006. [DOI] [PubMed] [Google Scholar]
- Young SD. Recommendations for Using Online Social Networking Technologies to Reduce Inaccurate Online Health Information. Online J Health Allied Scs. 2011;10(2):2. [PMC free article] [PubMed] [Google Scholar]
- Young SD, Rice E. Online social networking technologies, HIV knowledge, and sexual risk and testing behaviors among homeless youth. AIDS Behav. 2011;15(2):253–60. doi: 10.1007/s10461-010-9810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]