Abstract
Street-based female sex workers constitute a vulnerable population for HIV, as they are often enmeshed in chronic patterns of substance use, sexual risk, homelessness, and violent victimization. This study examined the specific contributions of victimization history and abuse-related traumagenic factors to mental health functioning and sexual risk behaviors, while considering the impact of environmental risk factors as well. Using targeted sampling strategies, we enrolled 562 Miami-based female sex workers into an intervention trial testing the relative effectiveness of two alternative case management conditions in establishing linkages with health services and reducing risk for HIV. Lifetime prevalence of abuse was extremely elevated at 88%. Nearly half reported abuse before the age of 18, while 34% reported violent encounters with “dates” or clients in the past 90 days. Serious mental illness (SMI) was quite common, with 74% reporting severe symptoms of depression, anxiety, or traumatic stress. For those with histories of abuse, SMI appeared to mediate the association between abuse-related trauma and unprotected sex behaviors. Mental health treatment would appear to be an important component of effective HIV prevention among this vulnerable group, and should form part of a compendium of services offered to female sex workers.
Introduction
Serious mental illness (SMI) is increasingly recognized as a significant risk factor for HIV infection (Blank & Eisenberg, 2007; McKinnon et al., 2002; Rosenberg et al., 2001). Generally defined as a past year mental disorder encompassing both DSM-IV criteria and functional impairment (Epstein et al. 2004), SMI is thought to increase HIV-related vulnerability through direct links to behavioral repertoires characterized by substance use, and high risk sexual behaviors, including multiple partners, infrequent condom use, and sex trading (Carey et al. 1997; Meade et al., 2009; Meade & Sikkema, 2005; Perehinets et al., 2006; Rosenberg et al., 2001). Environmental risk factors, such as poverty and homelessness, are also more prevalent among persons with SMI (Blank & Eisenberg, 2007), and these factors indirectly increase vulnerability to HIV (Kilbourne et al., 2002; Surratt & Inciardi, 2004).
Street-based female sex workers constitute an especially vulnerable population for HIV, as they are often enmeshed in chronic patterns of substance use, sexual risk, homelessness, and violent victimization (Davis, 2000; Kurtz et al., 2004; Surratt et al., 2004). Difficult personal histories, as well as harsh social and economic realities, tend to fuel risky sexual behaviors among female sex workers (Surratt & Inciardi 2010; Inciardi 1995), and the omnipresent risk of violent victimization in the context of sex work represents an acute threat to women’s health, safety, and well-being. Although previous research has indicated that levels of psychological distress, including depression, anxiety, and traumatic stress, are extremely elevated in this population (El-Bassel et al., 2001; Farley & Barkan, 1998; Gidycz et al., 1993; Maher, 1997; Sterk & Elifson, 1990; Surratt et al., 2005), studies that examine female sex workers’ victimization histories and SMI as predictors of sexual risk taking are rare.
Among non-sex worker populations, there are well-documented connections between childhood abuse, adult violence, poor mental health functioning and elevated risk for HIV (Meade et al., 2009; Messman-Moore & Long, 2000). Researchers in child sexual abuse have offered an explanatory “traumagenic” model to elucidate these connections, in which psychological functioning is affected by betrayal, stigmatization, traumatic sexualization, and feelings of powerlessness (Finkelhor 1987). Although the literature supports several elements of the traumagenic model, other researchers recommend a more inclusive ecological explanatory framework (Grauerholz 2000). From this perspective, behaviors and lifestyle factors that promote contact with potential perpetrators, or impair women’s ability to accurately evaluate risk situations, are potentially important explanatory elements.
Within this context, this paper documents the prevalence of childhood abuse, recent victimization, and SMI among a sample of substance abusing, street-based female sex workers in Miami, Florida. We examine the associations among violence, mental health and sexual risk taking behaviors, while considering the impact of both traumagenic and environmental factors. We assess the unique and cumulative impact of childhood abuse and recent sex work violence on SMI and unprotected sex in order to gauge the relative contributions of these factors to sexual risk taking among these vulnerable women.
Methods
Target Population and Study Eligibility
Data were drawn from a randomized intervention trial that tested the effectiveness of two case management protocols in linking African American sex workers with health services and reducing HIV risk behaviors. Clients were randomly assigned to: 1) a Strengths-Based/Professional-Only (PO) Condition, in which a professional case manager partnered with the client to set and achieve service goals; or, 2) a Strengths-Based/Professional Peer (PP) Condition in which a professional case manager and a former sex worker peer worked with the client to develop service goals and linkages. Both interventions provided five structured case management sessions over a two-month period.
Eligible participants were African American women ages 18 to 50 who had: a) traded sex for money or drugs at least 3 times in the past 30 days; and, b) used cocaine, crack, or heroin 3 or more times a week in the past 30 days.
Study Recruitment
Participants were recruited through traditional targeted sampling strategies (Watters & Biernacki, 1989). The recruitment team included professional outreach workers and active sex workers indigenous to the target areas, which provided access to many potential participants. The project’s intervention center was established to the north of downtown Miami near two of the major sex work hubs in the county.
Study Procedures
Telephone screening for eligibility included questions about the recency and frequency of drug use and sex work behaviors. Eligible recruits were scheduled for appointments at the project intervention center. After informed consent, the baseline interview was conducted, which took approximately one hour. Follow-up assessments were conducted 3 and 6 months after the baseline contact. Clients were paid a $25 stipend upon completion of each interview. Study protocols were approved by the University of Delaware’s Institutional Review Board, and a Certificate of Confidentiality from the U.S. National Institutes of Health was obtained.
Data Collection and Measures
Trained female interviewers conducted computer-assisted personal interviews. The Global Appraisal of Individual Needs (GAIN, v. 5.4; Dennis et al., 2002) was the primary assessment instrument, capturing information on demographics, substance use, physical and mental health status, services utilization, homelessness, violence, and sexual risk behaviors.
Independent Variables
The primary independent variables were substance dependence, victimization history, and abuse-related traumagenic factors.
Substance Dependence
Dependence was assessed using the TCU Drug Screen II (IBR, 2006), which consists of nine items measuring past year drug use severity. Endorsement of three or more items (e.g. using more or longer than intended, using in unsafe situations) approximates DSM-IV-R criteria for dependence. The alpha reliability coefficient for the TCU Drug Screen was 0.8.
Victimization
1) Child abuse. Participants answered four dichotomous (yes/no) items measuring lifetime physical, sexual, and emotional abuse. Those who endorsed lifetime abuse were asked for the age of first abuse; abuse onset prior to age 18 was categorized as a dichotomous child abuse variable. 2) Recent dating violence was measured by seven count items of past 90 day violent episodes by a paying partner, including physical assault and rape. These were collapsed to a dichotomous variable indicating the presence or absence of date violence in the specified time period.
Traumagenic factors related to abuse experiences (including duration and severity of abuse, type and relation of perpetrator) were queried in six dichotomous (yes/no) items. Traumagenic factors were examined as a continuous variable from 0–6 based on the number of items endorsed.
Dependent variables
The outcome measures in this analysis were SMI and unprotected vaginal sex.
SMI
Mental health subscales in the GAIN are based on DSM-IVR criteria: 9 items assess depression symptoms, 12 items assess anxiety symptoms, and 13 items assess stress disorders related to trauma, all over a 12 month period (Bohlig & Dennis, 1996; Dennis et al., 2002). In all cases, higher scores indicate greater problem severity. Summary scores yield classifications of: none/minimal (0–1), moderate (2–5) and severe (6–9) for depression; none/minimal (0–1), moderate (2–6), and severe (7–12) for anxiety, and none (0), moderate (1–4) and severe (5–13) for traumatic stress. Alpha reliability coefficients for the depression, anxiety, and traumatic stress scales were 0.83, 0.87, and 0.8, respectively. Participants classified as “severe” on any subscale were categorized as displaying SMI.
Unprotected vaginal sex
Unprotected vaginal sex was treated as a dichotomous variable, with 0 indicating no unprotected vaginal sex in the past 90 days, and 1 indicating at least one occasion of unprotected vaginal sex, including all partner types. This cut point provides a useful distinction between female sex workers enacting 100% condom use and those who are inconsistent users, and allows for comparison with the existing literature among female sex workers.
Data Analysis
All analyses were conducted using the Predictive Analytics Software (PASW, formerly SPSS) version 18; only baseline data are reported here. Descriptive statistics were computed on the number of participants who reported experiencing child abuse, recent dating violence, and the prevalence of abuse-related traumagenic factors.
Chi-square and t-tests examined differences in socio-demographics, substance dependence and homelessness, as well as abuse-related factors (traumagenic factors, child abuse, dating violence), across our outcome measures: SMI and unprotected vaginal sex.
Logistic regression models examined whether specific abuse history, along with traumagenic factors, were associated with SMI or unprotected vaginal sex, while controlling for factors that were significant in the descriptive analyses. Moderation effects were tested by computing interaction terms for specific abuse history and traumagenic factors. Models examined child abuse, traumagenic factors, and child abuse*traumagenic factors regressed on unprotected vaginal sex and SMI. Dating violence, traumagenic factors, and dating violence* traumagenic factors were also regressed on the two outcomes in separate models. Subsequently, a mediation model was tested a priori utilizing the Baron and Kenny (1986) approach. The mediating variable is SMI (0 versus 1); 1 indicates “severe” on any subscale (Depression, Anxiety, Traumatic Stress), and 0 otherwise.
Results
Five hundred and sixty two eligible clients completed baseline interviews between 2007 and 2010. The mean age was 39.3 years. Substance use in the previous ninety days included: alcohol (88.5%), crack (70.7%), powder cocaine (60%), and marijuana (68.4%). Eighty-eight percent of participants indicated lifetime histories of physical, sexual and/or emotional abuse. Just under 50% of the sample reported abuse before age 18, while 34% reported violent encounters with dates in the past 90 days. The mean for traumagenic factors was 4.1.
Table 1 presents descriptive information on demographic and substance use characteristics, as well as information on participants’ abuse histories, stratified by SMI.
Table 1.
Selected Characteristics of Drug-Involved FemaleSex Workers by Serious Mental Illness, Miami, Florida, 2006–2010(N=562)
| Variable | SMI (depression, anxiety, OR trauma) (n=416) | No SMI (n=146) | p value |
|---|---|---|---|
| Age (mean) | 38.8 | 40.8 | .012 |
| Education | |||
| % High school or more | 46.2 | 53.4 | .130 |
| Monthly income | |||
| $<1,000 | 35.1 | 31.5 | .480 |
| $1,001–$1,999 | 28.4 | 33.6 | |
| $2,000 + | 36.5 | 34.9 | |
| Homeless (% yes in past 90 days) | 59.1 | 42.5 | .000 |
| Substance dependence (% yes) | 95.7 | 76.0 | .000 |
| Abuse before age 18 (% yes) | 57.5 | 26.7 | .000 |
| Violence from ‘dates’ (% yes in past 90 days) | 41.2 | 13.7 | .000 |
| Abuse-related traumagenic factors1 (mean) | 4.4 | 3.2 | .000 |
| Unprotected vaginal sex (% yes in past 90 days)2 | 52.6 | 37.5 | .002 |
N=493, includes only those reporting any historyof abuse;
Excludes 7 women who reported no vaginal sex at baseline.
SMI was prevalent, with 74% of the sample reporting severe symptoms of depression, anxiety, or traumatic stress. Younger age, current homelessness, and past year substance dependence were each associated with a significantly higher likelihood of SMI. Child abuse, recent date violence, and traumagenic factors emerged as strong correlates of SMI.
Table 2 presents similar descriptive information on the sample, stratified by unprotected vaginal sex. Overall, 49% reported at least one occasion of unprotected vaginal sex in the past 90 days. Older age and past year substance dependence were associated with a significantly higher likelihood of unprotected vaginal sex, as were recent date violence and abuse-related traumagenic factors.
Table 2.
Selected Characteristics of Drug-Involved FemaleSex Workers by Past 90 Day Unprotected Vaginal Sex, Miami, Florida, 2006–2010 (N=555)1
| Variable | Unprotected vaginal sex (n=270) | No Unprotected vaginal sex (n=285) | p value |
|---|---|---|---|
| Age (mean) | 40.3 | 38.4 | .008 |
| Education (% high school or more) | 51.1 | 45.6 | .195 |
| Monthly income | |||
| $<1,000 | 37.4 | 31.2 | .284 |
| $1,001–$1,999 | 27.4 | 31.6 | |
| $2,000 + | 35.2 | 37.2 | |
| Homeless (% yes in past 90 days) | 57.0 | 53.7 | .427 |
| Substance dependence (% yes) | 94.1 | 87.0 | .005 |
| Abuse before age 18 (% yes) | 52.2 | 47.0 | .220 |
| Violence from ‘dates’ (% yes in past 90 days) | 42.8 | 26.0 | .000 |
| Abuse-related traumagenic factors2 (mean) | 4.34 | 3.97 | .003 |
| Severe mental illness (% yes to either severe depression, anxiety, OR trauma) | 80.0 | 68.4 | .002 |
Excludes 7 women who reported no vaginal sex at baseline;
N=486, includes only those reporting any history of abuse.
Table 3 presents the logistic regression models examining the impact of abuse history, and possible moderating effects of traumagenic factors, on SMI and unprotected sex. For both outcomes, Model 1 includes child abuse*traumagenic factors; Model 2 includes date violence*traumagenic factors.
Table 3.
Logistic Regression Models Predicting SMI and Unprotected Vaginal Sex among Drug-Involved FemaleSex Workers, Miami, Florida, 2006–2010
| Serious Mental Illness | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Unadjusted | Adjusted1 | ||||||||||
| OR | 95% CI
|
p-value | Model 1
|
Model 2
|
||||||||
| OR | 95% CI
|
p-value | OR | 95% CI
|
p-value | |||||||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Age | 0.97 | 0.95 | 0.99 | .012 | 0.96 | 0.93 | 0.99 | .010 | 0.96 | 0.93 | 0.99 | .013 |
| Substance dependence2 | 6.97 | 3.80 | 12.78 | .000 | 8.14 | 3.62 | 18.31 | .000 | 8.17 | 3.64 | 18.29 | .000 |
| Days homeless past 90 | 1.01 | 1.005 | 1.014 | .000 | 1.01 | 1.00 | 1.01 | .093 | 1.00 | 1.00 | 1.01 | .139 |
| Date violence2 | 4.42 | 2.65 | 7.36 | .000 | 1.90 | 1.03 | 3.51 | .040 | 4.54 | 0.69 | 29.76 | .114 |
| Child abuse2 | 3.71 | 2.45 | 5.61 | .000 | 0.79 | 0.18 | 3.43 | .756 | 1.80 | 1.06 | 3.06 | .030 |
| Traumagenic factors | 1.75 | 1.49 | 2.05 | .000 | 1.45 | 1.15 | 1.83 | .002 | 1.65 | 1.34 | 2.04 | .000 |
| Child abuse*trauma factors | 1.33 | 1.20 | 1.47 | .000 | 1.24 | 0.86 | 1.79 | .253 | ---- | ---- | ---- | ---- |
| Date viol*trauma factors | 1.37 | 1.21 | 1.55 | .000 | ---- | ---- | ---- | ---- | 0.81 | 0.53 | 1.25 | .343 |
| Unprotected Vaginal Sex
| ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Unadjusted | Adjusted3 | ||||||||||
| OR | 95% CI
|
p-value | Model 1
|
Model 2
|
||||||||
| OR | 95% CI
|
p-value | OR | 95% CI
|
p-value | |||||||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Age | 1.03 | 1.01 | 1.05 | .009 | 1.03 | 1.01 | 1.05 | .010 | 1.03 | 1.01 | 1.05 | .012 |
| Substance dependence2 | 2.37 | 1.28 | 4.37 | .006 | 1.39 | 0.70 | 2.76 | .345 | 1.41 | 0.71 | 2.81 | .323 |
| Date violence2 | 2.13 | 1.49 | 3.05 | .000 | 1.82 | 1.22 | 2.72 | .003 | 1.03 | 0.26 | 4.06 | .962 |
| Child abuse2 | 1.23 | 0.88 | 1.72 | .221 | 0.95 | 0.28 | 3.22 | .938 | 0.89 | 0.60 | 1.33 | .571 |
| Traumagenic factors | 1.21 | 1.06 | 1.37 | .004 | 1.18 | 0.97 | 1.44 | .105 | 1.13 | 0.96 | 1.33 | .149 |
| Child abuse*trauma factors | 1.04 | 0.96 | 1.11 | .333 | 0.99 | 0.75 | 1.30 | .919 | ---- | ---- | ---- | ---- |
| Date viol*trauma factors | 1.16 | 1.07 | 1.25 | .000 | ---- | ---- | ---- | ---- | 1.14 | 0.84 | 1.53 | .396 |
Multivariate logistic regression (N=493), adjusting for other variables in the model.
Reference category is ‘no’.
N=486.
In both SMI models the odds of SMI were approximately 8 times greater among substance-dependent women than non-dependent women. In model 1, recent dating violence was associated with greater odds of SMI; in model 2 child abuse was associated with greater odds of SMI. Traumagenic factors were positively associated with SMI in models 1 and 2; for every additional traumagenic factor endorsed in model 1, there was a 45% increase in the odds of SMI. Model 2 showed a 65% increase in the odds of SMI for every additional traumagenic factor endorsed. No interactions between traumagenic factors and abuse type were significant in either SMI model.
When examining unprotected vaginal sex, older age emerged as a strong predictor in both models 1 and 2. Recent date violence was associated with increased odds of unprotected sex in model 1. Traumagenic factors did not reach statistical significance in either model. No interactions between traumagenic factors and abuse type were significant in either unprotected sex model.
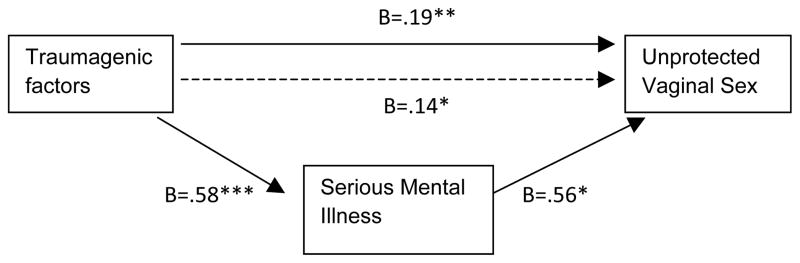
Traumagenic factors had a significant association with SMI and unprotected vaginal sex in the bivariate analyses. Based on these findings, we tested a model to examine whether SMI mediated the relationship between traumagenic factors and unprotected vaginal sex, controlling for age and substance dependence.
Traumagenic factors predicted both the outcome variable, unprotected vaginal sex (p<.01), and the mediator, SMI (p=.00). Controlling for traumagenic factors, SMI also predicted unprotected vaginal sex (p=.03). Finally, in a regression model that included both traumagenic factors and SMI as potential predictors of unprotected vaginal sex, the impact of traumagenic factors reduced and the association between SMI and unprotected sex was significant (p=.03). This provides evidence that SMI carries part of the influence of traumagenic factors to unprotected vaginal sex. Subsequently, a Sobel test was computed for mediation. The result (p=.03; 2-tailed) demonstrates that the indirect effect of traumagenic factors through SMI is significant.
Discussion
This study documented elevated levels of victimization among drug-involved street-based female sex workers. For 70%, age of first abuse preceded the age of entry into sex work, indicating that in large part these women’s lives were marked by violence well before their involvement in sex trading began. Nevertheless, sex work appeared to potentiate circumstances for victimization, as 34% reported dating violence within just the 90 days prior to interview. This proportion, while alarming, is consistent with the findings from prior studies of female sex workers (Church et al., 2001; El-Bassel et al., 2001).
SMI was documented in 74% of participants. While extraordinary, this finding appears reasonable given their extensive violence and victimization histories. The prevalence of SMI found here far exceeds that for the U.S. general population (~6%) (Kessler et al., 2001; 2005), and is much greater than the prevalence of psychological distress reported among women prisoners and chronic drug using women, where rates of depression approximate 10–11% (Hutton et al., 2001; Johnson et al., 2003). More troubling still is the lack of resources available to serve the mental health needs of these women; just 21% of those with SMI reported receiving any recent mental health care.
Multivariate analyses identified several factors associated with SMI and increased sexual risk. Consistent with prior research on co-morbid psychiatric and substance abuse problems (Devieux et al., 2007; Kalichman et al., 2005), substance dependence was associated with SMI in our sample. Both recent dating violence and child abuse history had strong direct effects on SMI. This resonates with prior research (Meade et al., 2009; Messman et al., 2000), which documented substantial contributions of child and adult victimization to psychological distress among women. Dating violence also had a direct impact on unprotected sex. This is not surprising, as violence would be expected to directly limit women’s choice in sexual encounters and their ability to enact safe sex, regardless of mental health status.
Traumagenic factors were associated with SMI and unprotected sex. This is consistent with the traumagenic model of abuse (Finkelhor & Brown 1985), which suggests that feelings of betrayal, stigmatization, and powerlessness operate as powerful influences on psychological functioning and behavioral repertoires. Here, SMI partially mediated the relationship between traumagenic factors and unprotected vaginal sex. The mediation model indicates that abuse-related traumagenic factors were associated with both poorer mental health and greater sexual risk. This finding is particularly important for HIV prevention planning with street-based sex workers, as it suggests that identifying and treating SMI would reduce unprotected sex among this group. Given that 18.2% reported being HIV positive, the implications of such an approach for HIV transmission are significant.
Our findings should be viewed within the context of several limitations. The data were gathered through self report, and therefore HIV risk behaviors and mental health symptoms may have suffered from reporting biases. Although we are confident that the use of specially trained female staff mitigated such deficiencies, caution is warranted in interpretation. Because of the need for interview brevity with this hard-to-reach population, data included only a small subset of mental health conditions tapped by the Composite International Diagnostic Interview (CIDI), the gold standard for most psychiatric epidemiologic surveys (Kessler et al., 2005). As such, caution is warranted when comparing the prevalence of SMI in our study with those utilizing the CIDI instrument and clinical interviews. The cross-sectional data limit our ability to demonstrate causal relationships among the key variables. Finally, although the sample is large, women who participated may not have been representative of all street-based sex workers in Miami, and the findings may not be generalizable to other sex worker populations.
Despite these limitations, this study provided substantial evidence for the role of abuse-related traumagenic factors in predicting SMI and unprotected sex among female sex workers. Given the extensive histories of victimization and elevated prevalence of SMI, this population is in great need of mental health services. Nevertheless, prior research with female sex workers has documented many barriers to mental health care, including fear of being labeled as “crazy,” and distrust of mental health professionals (Surratt et al., 2005). These findings suggest the need to develop targeted, culturally relevant interventions for female sex workers that raise awareness of SMI and address cultural norms and stigma related to SMI diagnosis and treatment.
From a public health perspective, mental health treatment would appear to be an important component of effective HIV prevention among this vulnerable group, and should form part of a compendium of services offered to female sex workers. A primary recommendation would involve the integration of mental health care into locations where drug-involved female sex workers routinely visit, such as shelters, community clinics, and HIV testing sites. In resource-constrained settings, a useful secondary approach would include the integration of brief educational and intervention material related to SMI into routine practice, such as existing HIV testing and counseling protocols delivered at community agencies.
The challenges associated with implementing sustainable health promotion initiatives among highly marginalized female sex workers should not be understated. Although HIV risk behaviors among this population are clearly amenable to change through brief, individual-level interventions (Surratt & Inciardi, 2010), reductions in risk are unlikely to be sustained should the prevailing social conditions of homelessness, drug dependence, poverty, violence, isolation, and disconnection from community remain unchanged. In this regard, structural interventions appear essential for female sex workers (Basu et al., 2004; Blankenship et al., 2006; Kerrigan et al., 2006). The present study’s population of inner city women is in great need of advocacy and community mobilization approaches to promote a safer work environment, improved treatment by police, and increased access to mental and physical health care. Such multi-level interventions will pose difficult challenges among women who are drug dependent and who operate in a landscape of largely disorganized and independent street-based sex work. Nevertheless, community building among disenfranchised female sex workers represents a critical first step in this movement.
Figure 1.
Regression model depicting SMI mediating the relationship between abuse-related traumagenic factors and unprotected vaginal sex
* Indicates significance at p≤.05; ** indicates significance at p≤.01 *** indicates significance at p≤.001.
Acknowledgments
This research was supported by Grant Number R01DA013131 from the National Institute on Drug Abuse. The authors gratefully acknowledge Dr. James A. Inciardi, Principal Investigator of this study through 2009.
Literature Cited
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Basu I, Jana S, Rotheram-Borus MJ, Swendeman D, Lee SJ, Newman P, Weiss R. HIV prevention among sex workers in India. Journal of Acquired Immune Deficiency Syndromes. 2004;36:845–852. doi: 10.1097/00126334-200407010-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blank MB, Eisenberg MM. HIV and mental illness: Opportunities for prevention. Journal of Prevention and Intervention in the Community. 2007;33:1–4. doi: 10.1300/J005v33n01_01. [DOI] [PubMed] [Google Scholar]
- Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: Concepts, challenges and opportunities for research. Journal of Urban Health. 2006;83:59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohlig EM, Dennis ML. Development of an abbreviated symptom checklist: Preliminary analysis of the HSCL-90 in a methadone-maintenance population. Research Triangle Park, NC: Research Triangle Institute; 1996. [Google Scholar]
- Carey MP, Carey KB, Kalichman SC. Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illness. Clinical Psychology Review. 1997;17:271–291. doi: 10.1016/s0272-7358(97)00019-6. [DOI] [PubMed] [Google Scholar]
- Church S, Henderson M, Barnard M, Hart G. Violence by clients towards female prostitutes in different work settings: questionnaire survey. British Medical Journal. 2001;322:524–525. doi: 10.1136/bmj.322.7285.524. Retrieved from http://www.bmj.com/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis NJ. From victims to survivors: working with recovering street prostitutes. In: Weitzer R, editor. Sex for sale: prostitution, pornography, and the sex industry. New York: Routledge; 2000. pp. 139–158. [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker JI, Hodgkins D. Global Appraisal of Individual Needs - Initial (GAIN-I) Bloomington, IL: Chestnut Health Systems; 2002. [Google Scholar]
- Devieux JG, Malow RM, Lerner BG, Dyer JG, Baptista L, Lucenko B, Kalichman SC. Triple jeopardy for HIV substance using severely mentally ill adults. Journal of Prevention and Intervention in the Community. 2007;33:5–18. doi: 10.1300/J005v33n01_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Witte S, Wada T, Gilbert L, Wallace J. Correlates of partner violence among female street-based sex workers: Substance abuse, history of childhood abuse, and HIV risks. AIDS Patient Care and STDs. 2001;15:41–51. doi: 10.1089/108729101460092. Retrieved from http://www.liebertpub.com/products/product.aspx?pid=1. [DOI] [PubMed] [Google Scholar]
- Epstein J, Barker P, Vorburger M, Murtha C. DHHS Publication No. SMA 04-3905, Analytic Series A-24. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2004. Serious mental illness and its co-occurrence with substance use disorders, 2002. [Google Scholar]
- Finkelhor D. The trauma of child sexual abuse: Two models. Journal of Interpersonal Violence. 1987;2:348–366. doi: 10.1177/088626058700200402. [DOI] [Google Scholar]
- Finkelhor D, Brown A. The traumatic impact of child sexual abuse: A conceptualization. American Journal of Orthopsychiatry. 1985;55:530–541. doi: 10.1111/j.1939-0025.1985.tb02703.x. [DOI] [PubMed] [Google Scholar]
- Grauerholz L. An ecological approach to understanding sexual revictimization: Linking personal, interpersonal, and sociocultural factors and processes. Child Maltreatment. 2000;5:5–17. doi: 10.1177/1077559500005001002. [DOI] [PubMed] [Google Scholar]
- Hutton HE, Treisman GJ, Hunt WR, Fishman M, Kendig N, Swetz A, Lyketsos CG. HIV risk behaviors and their relationship to posttraumatic stress disorder among women prisoners. Psychiatric Services. 2001;52:508–513. doi: 10.1176/appi.ps.52.4.508. Retrieved from http://ps.psychiatryonline.org/ [DOI] [PubMed] [Google Scholar]
- Inciardi JA. Crack, crack house sex, and HIV risk. Archives of Sexual Behavior. 1995;24:249–269. doi: 10.1007/BF01541599. [DOI] [PubMed] [Google Scholar]
- Institute of Behavioral Research (IBR) The TCU Drug Screen II. 2006 Retrieved from: http://www.ibr.tcu.edu/pubs/datacoll/Forms/ddscreen-95.pdf.
- Johnson SD, Cunningham-Williams RM, Cottler LB. A tripartite of HIV-risk for African American women: The intersection of drug use, violence, and depression. Drug and Alcohol Dependence. 2003;70:169–175. doi: 10.1016/S0376-8716(02)00345-9. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Malow R, Dévieux J, Stein JA, Piedman F. HIV risk reduction for substance using seriously mentally ill adults: Test of the information-motivation-behavior skills (IMB) model. Community Mental Health Journal. 2005;41:277–289. doi: 10.1007/s10597-005-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerrigan D, Moreno L, Rosario S, Gomez B, Jerez H, Barrington C, Weiss E, Sweat M. Environmental-structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. American Journal of Public Health. 2006;96:120–125. doi: 10.2105/AJPH.2004.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PB, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. Retrieved from http://archpsyc.ama-assn.org/ [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, Manderscheid RW, Rosenheck RA, Walters EE, Wang PS. The prevalence and correlates of untreated serious mental illness. Health Services Research. 2001;36:987–1007. Retrieved from http://www.hsr.org/ [PMC free article] [PubMed] [Google Scholar]
- Kilbourne AM, Herndon B, Anderson RM, Wenzel SL, Gelberg L. Psychiatric symptoms, health services, and HIV risk factors among homeless women. Journal of Health Care for the Poor Underserved. 2002;13:49–65. doi: 10.1353/hpu.2010.0189. Retrieved from http://www.press.jhu.edu/journals/journal_of_health_care_for_the_poor_and_underserved/ [DOI] [PubMed] [Google Scholar]
- Kurtz SP, Surratt HL, Inciardi JA, Kiley MC. Sex work and “date” violence. Violence Against Women. 2004;10:357–385. doi: 10.1177/1077801204263199. [DOI] [Google Scholar]
- McKinnon K, Cournos F, Herman R. HIV among people with chronic mental illness. Psychiatric Quarterly. 2002;73:17–31. doi: 10.1023/a:1012888500896. [DOI] [PubMed] [Google Scholar]
- Meade CS, Kershaw TS, Hansen N, Sikkema KJ. Long-term correlates of child abuse among adults with severe mental illness: Adult victimization, substance abuse, and HIV sexual risk behavior. AIDS and Behavior. 2009;13:207–216. doi: 10.1007/s10461-007-9326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. HIV risk behavior among persons with severe mental illness: A systematic review. Clinical Psychology Review. 2005;25:433–457. doi: 10.1016/j.cpr.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Messman TL, Long PJ, Siegfried NJ. The revictimization of child sexual abuse survivors: An examination of the adjustment of college women with child sexual abuse, adult sexual assault, and adult physical abuse. Child Maltreatment. 2000;5:18–27. doi: 10.1177/1077559500005001003. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ. Child sexual abuse and revictimization in the form of adult sexual abuse, adult physical abuse, and adult psychological abuse. Journal of Interpersonal Violence. 2000;15:489–501. doi: 10.1177/088626000015005003. [DOI] [Google Scholar]
- Perehinets I, Mamary E, Rose V. Conducting HIV prevention programs for severely mentally ill: An assessment of capacity among HIV prevention programs providers in the city and county of San Francisco. Californian Journal of Health Promotion. 2006;4:76–80. Retrieved from http://www.cjhp.org/ [Google Scholar]
- Rosenberg SD, Goodman LA, Osher FC, Swartz MS, Essock SM, Butterfield MI, et al. Prevalence of HIV, Hepatitis B, and Hepatitis C in people with severe mental illness. American Journal of Public Health. 2001;91:31–37. doi: 10.2105/ajph.91.1.31. Retrieved from http://ajph.aphapublications.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, Inciardi JA. HIV risk, seropositivity and predictors of infection among homeless and non-homeless women sex workers in Miami, Florida, USA. AIDS CARE. 2004;16:594–604. doi: 10.1080/09540120410001716397. [DOI] [PubMed] [Google Scholar]
- Surratt HL, Inciardi JA. An effective HIV risk reduction protocol for drug-using female sex workers. Journal of Prevention and Intervention in the Community. 2010;38:118–131. doi: 10.1080/10852351003640732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, Inciardi JA, Kurtz SP, Kiley MC. Sex work and drug use in a subculture of violence. Crime Delinquency. 2004;50:43–59. doi: 10.1177/0011128703258875. [DOI] [Google Scholar]
- Surratt HL, Kurtz SP, Weaver JC, Inciardi JA. The connections of mental health problems, violent life experiences, and the social milieu of the “stroll” with the HIV risk behaviors of female sex workers. Journal of Psychology & Human Sexuality. 2005;17:23–44. doi: 10.1300/J056v17n01_03. [DOI] [Google Scholar]
- Watters J, Biernacki P. Targeted sampling: options for the study of hidden populations. Social Problems. 1989;36:416–430. doi: 10.1525/sp.1989.36.4.03a00070. [DOI] [Google Scholar]