Abstract
Variable sensitivity to T-cell-receptor (TCR)- and IL-7-receptor (IL-7R)-mediated homeostatic signals among naïve T cells has thus far been largely attributed to differences in TCR specificity. We show here that even when withdrawn from self-peptide-induced TCR stimulation, CD8+ T cells exhibit heterogeneous responses to interleukin-7 (IL-7) that are mechanistically associated with IL-7R expression differences that correlate with relative CD5 expression. Whereas CD5hi and CD5lo T cells survive equivalently in the presence of saturating IL-7 levels in vitro, CD5hi T cells proliferate more robustly. Conversely, CD5lo T cells exhibit prolonged survival when withdrawn from homeostatic stimuli. Through quantitative experimental analysis of signaling downstream of IL-7R, we find that the enhanced IL-7 responsiveness of CD5hi T cells is directly related to their greater surface IL-7R expression. Further, we identify a quantitative threshold in IL-7R-mediated signaling capacity required for proliferation that lies well above an analogous threshold requirement for survival. These distinct thresholds allow subtle differences in IL-7R expression between CD5lo and CD5hi T cells to give rise to significant variations in their respective IL-7-induced proliferation, without altering survival. Heterogeneous IL-7 responsiveness is observed similarly in vivo, with CD5hi naïve T cells proliferating preferentially in lymphopenic mice or lymphoreplete mice administered with exogenous IL-7. However, IL-7 in lymphoreplete mice appears to be maintained at an effective level for preserving homeostasis, such that neither CD5hi IL-7Rhi nor CD5lo IL-7Rlo T cells proliferate or survive preferentially. Our findings indicate that IL-7R-mediated signaling not only maintains the size but also impacts the diversity of the naïve T-cell repertoire.
Keywords: IL-7, naïve T cells, homeostasis, signaling
Homeostatic survival and proliferation of naïve CD8+ T cells are dependent upon signaling from T-cell receptor (TCR) binding to self-peptide major histocompatibility complex (spMHC), as well as interleukin-7 (IL-7) binding to the IL-7 receptor (IL-7R).1, 2 Competition for a diverse pool of cognate spMHCs is believed to maintain diversity in the T-cell repertoire.1, 2, 3 Conversely, studies manipulating cytokine levels in vivo4, 5, 6 led to the conclusion that IL-7 availability regulates the overall size of the naïve T-cell population, but not necessarily its clonal composition.7, 8 The notion that IL-7 provides equal homeostatic support across the mature CD8+ T-cell pool has been put into question by recent studies suggesting that IL-7R signaling may also vary with TCR specificity.9 Signaling differences among T cells have been proposed to arise through cross-talk between TCR and IL-7R signaling pathways,9 and through increased ability to access or respond to IL-7 by T cells, with stronger or more frequent engagement with cognate spMHC.10, 11, 12, 13 In either scenario, active TCR engagement and signaling is generally believed to predominantly underlie heterogeneity among T cells in their responses to homeostatic cues.
Differences in the responsiveness of T cells to homeostatic signals have been well characterized in lymphopenic hosts. Although naïve T cells in lymphoreplete hosts are normally quiescent,1, 2 T-cell expansion can occur in lymphopenic hosts, termed lymphopenia-induced proliferation (LIP).1 Rates of LIP among different naïve T-cell clones vary depending upon the specificity of their TCRs, and correlate with their CD5 expression levels.11, 13 CD5 is a negative regulator of TCR signaling14 that is upregulated upon spMHC engagement.15 Thus, CD5 expression levels are thought to reflect the strength of TCR–spMHC interactions.15, 16, 17, 18 On the basis of these data, variations in LIP have been attributed to differences in the avidity of T cells for cognate spMHC,11, 13 with the implicit assumption that naive T cells bearing different TCRs have equal IL-7R signaling capacity. Examinations of the lifespan of naïve T cells have also implicitly presumed that T cells survive equally well in the absence of dedicated homeostatic cues.19, 20, 21, 22
Nonetheless, expression levels of key homeostatic signaling components, including IL-7R8 and CD5,17 are known to vary among naïve CD8+ T-cell clones. These differences in expression have been attributed to the interaction of T cells with heterogeneous IL-7 and spMHC environments,9, 15, 23 but they could also reflect cell-intrinsic differences in signaling pathways among mature T cells. To explore this possibility, we tested the assumption that IL-7 signaling and responsiveness is intrinsically uniform among distinct mature naïve CD8+ T-cell clones in the absence of TCR stimulation. We found that CD5 expression stratifies CD8+ T-cell populations with heterogeneous functional responsiveness to IL-7 as revealed by varying proliferation, survival and induction of CD8α expression. Importantly, this differential responsiveness was controlled by differences in the level of surface IL-7Rα expressed by the cells, with distinct quantitative thresholds in downstream signaling associated with survival and proliferation. Thus, the qualitative behavior of different T-cell populations can be explained in terms of their capabilities with respect to reaching these signaling thresholds. Similar response heterogeneities are found in vivo, where manipulation of IL-7 levels led to modulation of the relative abundance of CD5hiIL-7Rhi and CD5loIL-7Rlo clones. These results suggest a role for IL-7 in regulating the size and composition of the naïve T-cell repertoire complementary to that of spMHC interactions,3, 12, 13, 24 and may offer useful insight in the design of IL-7-based immunotherapies.
Results
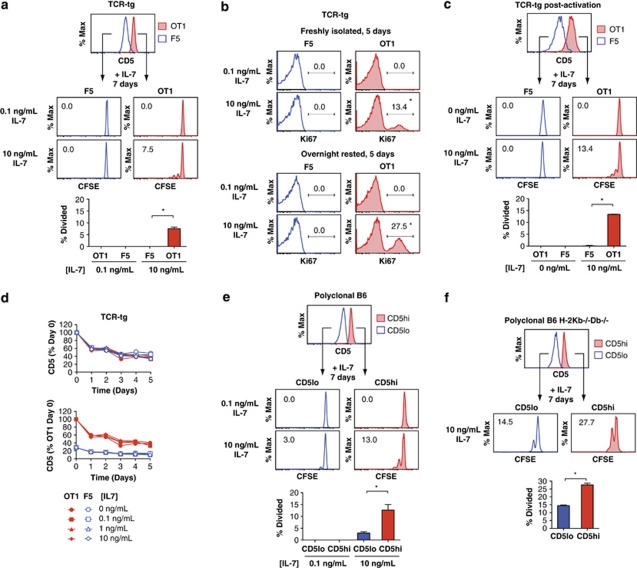
CD5hi naïve CD8+ T cells have enhanced IL-7-induced proliferation
We first asked whether CD8+ T cells with a common genetic background but distinct antigen specificities respond equivalently to IL-7 stimulation alone. We isolated naïve (CD44lo) CD8+ T cells from OT-1 and F5 TCR-transgenic (TCR-tg) B6.Rag1−/− mice (hereafter referred to as OT-1 or F5 cells) (Supplementary Figure 1a). Both OT-1 and F5 cells are selected in the H-2b MHC background, but OT-1 cells exhibit markedly greater LIP than F5 cells.11 We found that in vitro IL-7 stimulation alone had disparate effects on naïve OT-1 and F5 cells: when OT-1 and F5 cells were cultured at low density in flat-bottom tissue culture plates to minimize cell–cell contact with 10 ng ml−1 of IL-7 for 7 days, a fraction of the OT-1 cells proliferated with 1–3 rounds of division, whereas essentially none of the F5 cells divided (Figure 1a). No proliferation was seen for either cell type when treated with a lower dose of IL-7 (0.1 ng ml−1), sufficient for maintaining cell viability, suggesting that proliferation does not arise solely from the residual effects of homeostatic stimulation received in vivo before isolation. Differences in proliferation were also apparent when measured as the fraction of cells expressing the nuclear proliferation antigen Ki67 after 5 days of culture in IL-7 containing medium (Figure 1b). Furthermore, the fraction of Ki67+ proliferating cells increased when cells were rested overnight (∼16 h) in cytokine-free media before IL-7 treatment. IL-7-induced proliferation differences were also maintained for OT-1 and F5 cells that are activated and differentiated into memory-like cells in vitro (Figure 1c).
Figure 1.
CD5 expression levels stratify a hierarchy in the IL-7-induced proliferation capacities of CD8+ T cells. (a) CD5 surface expression of freshly isolated OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells (top panel) and their proliferation when cultured in vitro at low density (∼2 × 105 cells per ml) with 0.1 or 10 ng ml−1 of IL-7, as assayed by CFSE dilution after 7 days (middle panels), and quantified as the fraction of cells divided (bottom panel). (b) Proliferation of OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells when cultured in vitro at low density with 0.1 or 10 ng ml−1 of IL-7 as measured by the fraction of cells expressing the nuclear proliferation antigen Ki67 for cells either freshly isolated (top panels) or rested overnight (16 h) in cytokine-free media before stimulation (bottom panels). *P<0.05 between 0.1 and 10 ng ml−1 conditions and between fresh and rested cells. (c) As described in a, except for OT-1 and F5 TCR-tg CD8+ memory-like cells generated in vitro through activation of naïve (CD44lo) OT-1 and F5 TCR-tg CD8+ T cells with plate-coated anti-CD3 and 20 ng ml−1 IL-2 for 3 days, followed by incubation with 40 ng ml−1 IL-15 for 3 days and overnight rest in cytokine-free media before IL-7 stimulation. (d) Decay of CD5 surface expression of freshly isolated OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells cultured with 0, 0.1, 1 or 10 ng ml−1 IL-7, normalized to initial expression for each cell type (top panel), or to initial CD5 expression on OT-1 cells (bottom panel). (e) As described in a, except for freshly isolated C57BL/6 naïve (CD44lo) CD8+ T cells, sorted into CD5hi and CD5lo expressing fractions. (f) As described in a, except for freshly isolated naïve H-2Kb−/−Db−/− (CD44lo) CD8+ T cells from C57BL/6.Rag1−/− mice transplanted with C57BL/6.H-2Kb−/−Db−/− bone marrow, sorted into CD5hi and CD5lo expressing fractions. Data (a–f) are representative of two independent experiments (error bar=±1s.d.).
Naïve OT-1 and F5 T cells are known to express different levels of CD5,11 (Figure 1a) and we found that differences in their relative CD5 levels were maintained after activation and differentiation in vitro (Figure 1c). CD5 is often used as a surrogate measure of the strength of spMHC-mediated signaling based on the requirement for continuous TCR engagement with spMHC to maintain CD5 levels.15 Indeed, we observed that CD5 levels on OT-1 and F5 cells decayed over time in culture, and that decay was independent of IL-7 stimulation (Figure 1d and Supplementary Figure 1b). However, OT-1 cells maintained their approximately threefold higher level of CD5 at all time points, suggesting that basal CD5 expression levels are intrinsic to particular T-cell clones.
Maintenance of relative CD5 expression levels led us to hypothesize that CD5 expression stratifies T-cell populations with varying IL-7 sensitivity. We sorted polyclonal naïve (CD44lo) CD8+ T cells from B6 mice into CD5hi and CD5lo populations, and examined their responsiveness to IL-7 (Figure 1e). As with TCR-tg cells, a greater fraction of polyclonal CD5hi T cells proliferated when cultured with 10 ng ml−1 of IL-7 for 7 days compared with CD5lo cells, whereas neither subset proliferated at a lower dose of 0.1 ng ml−1 IL-7 (Figure 1e). Cells also maintained their relative CD5 expression levels (Supplementary Figure 1b). To ensure that the differences in IL-7 responsiveness observed in this experimental system were not due to self-peptides presented on class I MHC on the T cells themselves, we generated naïve CD8+ T cells lacking class I MHC by reconstituting B6.Rag1−/− mice with bone marrow from syngeneic H-2 Kb−/−Db−/− mice (Supplementary Figure 1c). Similar differences in IL-7-induced proliferation were observed when we compared CD5hi and CD5lo H-2 Kb−/−Db−/− CD8+ T cells (Figure 1f), confirming that the differential response to IL-7 is due to intrinsic differences in the ability of cells to respond to IL-7. These data show that CD5 expression levels stratify the naïve CD8+ T-cell repertoire in terms of proliferation responses to the homeostatic cytokine IL-7, with higher CD5 levels marking cells with more robust proliferation.
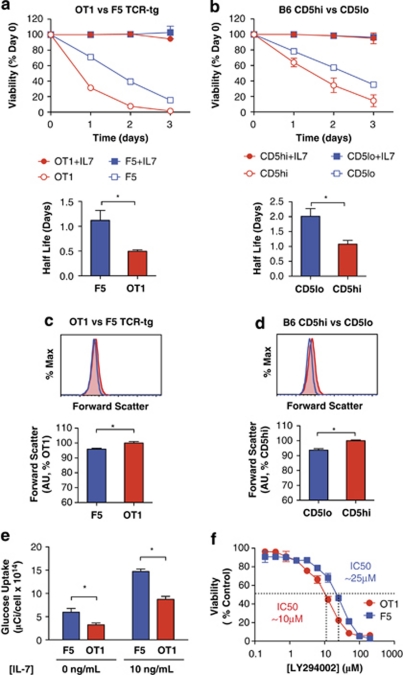
CD5lo naïve CD8+ T cells have prolonged cytokine-independent survival
We next compared the survival of CD5hi versus CD5lo T cells in IL-7-supplemented, as well as cytokine-free cultures. Both OT-1 and F5 naïve T cells exhibited ∼100% survival over 3 days in the presence of saturating doses of IL-7 (Figure 2a). However, F5 cells survived better in vitro than OT-1 cells in the absence of IL-7. Polyclonal CD5hi and CD5lo naïve CD8+ T cells behaved similarly to their TCR-tg counterparts, with CD5lo cells surviving better in cytokine-deprived culture (Figure 2b). Thus, while CD5hi and CD5lo CD8+ T cells possess different capacities to proliferate in response to IL-7, they also exhibit disparate abilities to survive in the absence of homeostatic stimuli.
Figure 2.
CD5lo naïve CD8+ T cells have prolonged cytokine and TCR-independent survival, increased glucose uptake and lower sensitivity to PI3K inhibition. Viability, as measured by DAPI exclusion, over 3 days for: (a) OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells, and (b) C57BL/6 naïve (CD44lo) CD8+ T cells sorted into CD5hi or CD5lo expressing fractions, for cells rested in cytokine-free media overnight (16 h) and then treated±10 ng ml−1 IL-7 in vitro in low density (∼2 × 105 cells per ml) culture (top panel). Mean half-lives of cytokine-deprived cells are indicated in the bottom panel. Cell size as estimated by forward scatter for (c) OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells, and (d) C57BL/6 polyclonal naïve (CD44lo) CD8+ T cells sorted into CD5hi or CD5lo expressing fractions. (e) Radioactive glucose uptake for OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells cultured 16 h±10 ng ml−1 IL-7 and incubated for 45 min with 0.1 mM 3H-2-deoxy-D-glucose (4 μCi ml−1). (f) Sensitivity of viability to PI3K inhibition for OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells rested overnight (16 h) in cytokine-free media and then treated 24 h with varying doses of the PI3K inhibitor LY294002. The LY294002 IC50 for the viability of OT-1 and F5 T cells is shown to be 10 and 25 μM, respectively. Data (a–f) are representative of two independent experiments (error bar=±1s.d.). *P<0.05.
We suspected that differences in proliferation capacity, and survival in the absence of cytokines between T cells might be reflected in their metabolic state. Both F5 and polyclonal CD5lo T cells have slightly decreased forward scatter, a correlate of cell size, which may indicate that they are more quiescent than their CD5hi counterparts (Figures 2c and d). T-cell quiescence is characterized by efficient energy metabolism that is driven by oxidative phosphorylation, and is directed to homeostatic processes rather than anabolic growth.25 CD5lo T cells may therefore support their prolonged survival in cytokine-withdrawn conditions through more efficient metabolic processes.
Homeostatic survival is reliant upon glucose metabolism, and IL-7 supports survival in part by increasing glucose uptake via upregulation of the Glut1 glucose transporter.26 To determine whether OT-1 and F5 cells differed in glucose uptake, we measured their radioactive glucose incorporation by following overnight culture in the presence or absence of IL-7. Although both cells increased glucose uptake with IL-7 treatment, remarkably F5 cells had greater uptake than OT-1 in both the presence and absence of IL-7 (Figure 2e). Greater intrinsic glucose uptake in relatively quiescent F5 cells may therefore support prolonged cell survival in cytokine-depleted conditions, whereas in the presence of cytokine, both cells may have sufficient glucose uptake for survival.
Phosphoinositide 3-kinase (PI3K) is a critical mediator of glucose uptake.26 We therefore hypothesized that F5 cells might have increased PI3K signaling activity compared with OT-1 cells. Pharmacological inhibition of PI3K using LY294002 did not significantly decrease OT-1 or F5 survival over 24 h in the presence 0.1 ng ml−1 IL-7 (data not shown). However, F5 cells had lower sensitivity to PI3K inhibition in the absence of cytokine, with a half-maximal inhibitory concentration (IC50) of 25 μM LY294002 compared with 10 μM for OT-1 cells (Figure 2f). Similar differences in sensitivity were observed with a second PI3K inhibitor, PI-103 (data not shown), buttressing the notion that greater baseline PI3K activity in CD5lo T cells may support their prolonged survival in cytokine-deprived conditions.
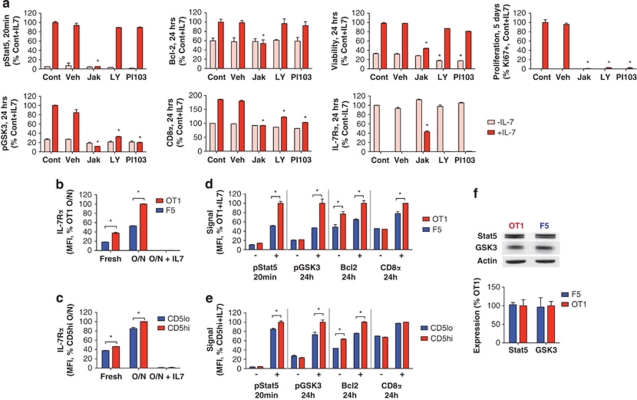
CD5hi naïve CD8+ T cells have higher IL-7R expression and IL-7-induced signaling
To define the underlying mechanisms determining IL-7 responsiveness, we next examined IL-7-dependent signaling pathway activation. IL-7 is thought to support T-cell survival and proliferation through activation of the Jak/Stat and PI3K/Akt signaling pathways,27 though the roles of the individual pathways have yet to be fully clarified.2 To determine reliance on Jak- and PI3K-induced signaling for IL-7-induced responses, OT-1 cells were treated with IL-7 or cytokine-free media in the presence of the Jak family inhibitor, Jak Inhibitor I, or the PI3K inhibitors, PI-103 or LY294002, and their signaling and responses were measured by flow cytometry (Figure 3a). All IL-7-induced downstream signaling and responses monitored—Stat5 phosphorylation (pStat5) at 20 min, GSK3 phosphorylation (pGSK3), CD8α and Bcl2 expression, IL-7Rα suppression, viability at 24 h, and proliferation at 5 days—were dependent on Jak-mediated signaling. In contrast, PI3K activity was critical only for a subset of responses. IL-7-induced proliferation, pGSK3 and CD8α were PI3K dependent, whereas pStat5, Bcl2, viability and IL-7Rα suppression were unaffected by PI3K inhibition. In the absence of IL-7, viability decreased with PI3K inhibition, independent of Bcl2 expression. This suggests that cytokine-independent survival may depend upon basal PI3K activity, whereas PI3K-independent survival increases in Bcl2, and other anti-apoptotic proteins may dominate survival in the presence of IL-7. However, proliferation required both Jak and PI3K activity. We could not explicitly test if PI3K is directly activated by IL-7 stimulation, as Jak-independent indicators of PI3K signaling (for example, Akt phosphorylation) could not be reliably quantified in this assay.
Figure 3.
CD5hi naïve CD8+ T cells have higher IL-7R expression and IL-7-induced signaling. (a) IL-7-induced signaling and responses under Jak and PI3K inhibition. OT-1 TCR-tg naïve (CD44lo) CD8+ T cells were cultured overnight (16 h) and then treated with±10 ng ml−1 IL-7 in the presence of untreated media control (Cont), vehicle (Veh), 1 μM Jak Inhibitor I (Jak), 10 μM LY294002 (LY) or 10 μM PI-103 (PI-103). Stat5 phosphorylation (pStat5; 20 min), GSK3 phosphorylation (pGSK3; 24 h), CD8α (24 h), Bcl2 (24 h), viability (24 h), proliferation (%Ki67, 5 days) and IL-7Rα levels (24 h) were measured by flow cytometry and quantified as the population median staining normalized to the IL-7-treated control samples, except for IL-7Rα, which are normalized to the untreated control. *P<0.05 between Veh and Cont conditions. Surface IL-7Rα expression of (b) OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells and (c) C57BL/6 naïve (CD44lo) CD8+ T cells sorted into CD5hi or CD5lo expressing fractions, for cells freshly isolated from lymph nodes or cells cultured overnight (O/N; 16 h)±10 ng ml−1 IL-7. IL-7-induced signaling in (d) OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells and (e) C57BL/6 naïve (CD44lo) CD8+ T cells sorted on CD5hi or CD5lo expressing fractions, as assessed by pStat5 at 20 min, and pGSK3, Bcl2 and surface CD8α expression at 24 h, in cells rested overnight and then treated with±10 ng ml−1 IL-7. (f) Total expression of Stat5, GSK3 and β-actin (loading control) as assessed by SDS-poly acrylamide gel electrophoresis (top panel) and quantified by densitometry (bottom panel) in OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells rested overnight in cytokine-free media. Data (a–f) are representative of two independent experiments (error bar=±1s.d.). *P<0.05.
We next compared differences in IL-7-dependent signaling pathway activation between CD5hi and CD5lo T cells. We first characterized IL-7Rα surface expression of OT-1 and F5 cells. As IL-7 signaling suppresses transcription of IL-7Rα,23 and in vivo IL-7 levels may differ between OT-1 and F5 mice, we compared IL-7Rα expression in both freshly isolated T cells and cells placed in cytokine-free culture for 16 h (Figure 3b and Supplementary Figure 2a). Freshly isolated OT-1 cells had approximately twofold higher IL-7Rα expression than F5 cells, and this relative difference was maintained by following cytokine-free culture, exposing a higher ‘basal' (that is, uninhibited) receptor expression in OT-1 cells. In contrast, culture of either OT-1 or F5 cells for 16 h with 10 ng ml−1 of IL-7 completely suppressed surface IL-7Rα expression. Polyclonal naïve CD8+ CD5hi and CD5lo T cells also showed more modest but statistically significant differences in IL-7Rα levels (Figure 3c and Supplementary Figure 2a), consistent with CD5 levels marking intrinsic differences in IL-7R expression.
To determine whether these modest differences in IL-7Rα expression elicit differential signaling pathway activation, we measured levels of pStat5 and pGSK3 and increases in Bcl2 and CD8α expression, following IL-7 stimulation. T cells were rested overnight before measuring signaling to eliminate the potential effects of heterogeneous signaling received in vivo. OT-1 cells treated with IL-7 showed higher pStat5 (at 20 min) and pGSK3 (at 24 h) than F5 cells (Figure 3d and Supplementary Figure 2b), which was independent of total Stat5 or GSK3 expression (Figure 3f). Differences in IL-7-induced pStat5 between OT-1 and F5 cells could also be seen immediately following isolation, when IL-7Rα is partially suppressed (Supplementary Figure 2c). IL-7 also induced a greater increase in CD8α expression at 24 h in OT-1 cells (Figure 3d). Although the fold induction of Bcl2 at 24 h was comparable between the two cells, OT-1 cells had higher basal and IL-7-induced Bcl2 levels. Polyclonal naïve CD8+ CD5hi and CD5lo cells exhibited the same trends as TCR-tg cells, although the differences were less pronounced, reflecting the smaller differences in their initial IL-7Rα expression (Figure 3e and Supplementary Figure 2b). These results demonstrate that even mild differences in baseline IL-7R levels between CD5hi and CD5lo cells are associated with significant differences in IL-7-induced signaling pathway activation.
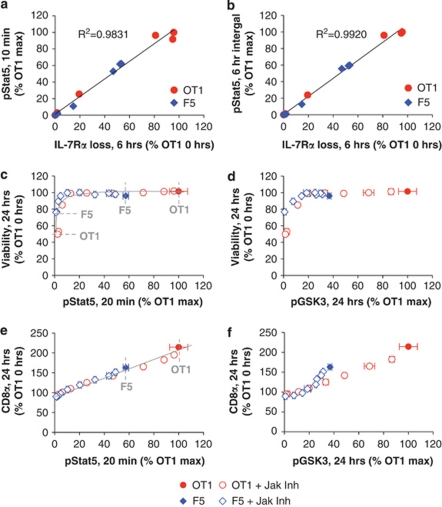
IL-7R expression thresholds naïve CD8+ T-cell responses to IL-7
We undertook a detailed quantitative analysis of IL-7-induced signaling in CD5hi and CD5lo cells to determine whether observed signaling differences were directly attributable to differences in IL-7R expression and could explain variations in responses to IL-7. To elucidate the relationship between IL-7R expression and signaling, OT-1 and F5 cells were treated with varying IL-7 doses and their pStat5 and IL-7Rα surface expression dynamics were measured over 6 h (Supplementary Figure 3a). Both OT-1 and F5 cells showed the same linear relationship between loss of surface IL-7Rα at 6 h and the level of Stat5 signaling induced (quantified either as the pStat5 level at 10 min or integrated over 6 h) (Figures 4a and b). This indicates equivalent proximal signaling per receptor in OT-1 and F5 cells, and that the enhanced signaling capacity of OT-1 cells is directly related to their higher IL-7R expression.
Figure 4.
IL-7R expression thresholds naïve CD8+ T-cell responses to IL-7. Linear relationship between loss of surface IL-7Rα at 6 h with (a) Stat5 phosphorylation at 10 min, and (b) Stat5 phosphorylation integrated over 6 h, for OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells rested overnight and treated with IL-7 concentrations of 0–10 ng ml−1. Relationship of IL-7-induced signaling to (c, d) viability at 24 h, and (e, f) CD8α expression at 24 h for signaling quantified as either (c, e) Stat5 phosphorylation at 20 min or (d, f) GSK3 phosphorylation at 24 h, for OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells rested overnight (16 h) in cytokine-free media, and then treated with 1 ng ml−1 of IL-7 and varying concentrations of Jak Inhibitor I (0.001–1 μM) to titrate down signaling. Additional supporting data and description of the design and motivation for titrating signaling via varying the dose of a Jak Inhibitor can be found in Supplementary Figures 3b–e. Data (a–f) are representative of two independent experiments (error bar=±1s.d.).
We next asked whether OT-1 and F5 cells translated a given amount of signaling into equivalent functional responses. Differences in IL-7R expression between OT-1 and F5 cells yield unequal IL-7 depletion and signal durations in low-IL-7-dose conditions, resulting in incorrect inference of relationships between induced signaling and responses across varying IL-7-dose conditions (Supplementary Figures 3b and c). Greater IL-7 depletion by OT-1 cells results in less sustained IL-7Rα downregulation and CD8α induction, and lower viability after extended culture compared with F5 cells (Supplementary Figures 3d and e). To circumvent effects of heterogeneous IL-7 depletion, we took advantage of the reliance of all downstream IL-7-induced responses on Jak activity (Figure 3a), and titrated the level of signaling by treating cells with a high dose of IL-7 (1 ng ml−1) and varying amounts of Jak Inhibitor I (Supplementary Figure 3b). OT-1 and F5 cells exhibited common relationships between induced IL-7 signaling (20 min or 24 h pGSK3) and viability or CD8α expression at 24 h, but had different dynamic ranges (Figures 4c-f). Viability responses to IL-7 signaling were nonlinear and readily saturated, with ∼100% survival induced by very low levels of signaling (Figures 4c and d). Thus, uninhibited IL-7-induced signaling capacities of OT-1 and F5 cells, though reaching different maxima, were sufficient to yield complete survival of either T cell at high IL-7 doses. In contrast, although OT-1 and F5 cells also shared a common relationship between signaling and induction of CD8α, this relationship was linear (Figures 4e and f), and F5 cells could not achieve the maximum CD8α induction seen in OT-1 cells.
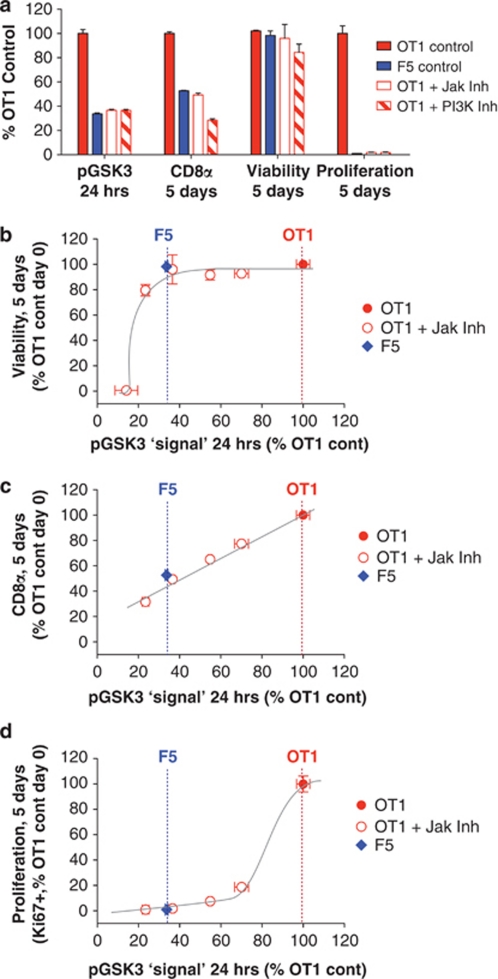
We hypothesized that similar to CD8α induction and viability, there may exist a common threshold level of IL-7 signaling required to promote T-cell proliferation, which was not met by F5 cells. We initially sought to test this hypothesis by determining whether increasing IL-7R expression in F5 cells would allow for their proliferation. However, retroviral transduction of IL-7Rα into F5 bone marrow-derived stem cells did not affect the surface IL-7R expression in mature F5 T cells in a Rag1−/− bone marrow reconstitution assay, possibly reflecting tight control of IL-7R expression during development (data not shown). We therefore adopted an alternate approach, and asked whether lowering IL-7-induced signaling in OT-1 cells to levels achievable by F5 cells abolished proliferation. OT-1 cells were treated with 10 ng ml−1 IL-7 and a dose of Jak inhibitor (0.0625 μM Jak Inhibitor I) or PI3K inhibitor (1 μM PI-103) sufficient to bring their IL-7-induced signaling at 24 h to levels in untreated F5 cells (Figure 5a). GSK3 phosphorylation was used as convenient indicator of integrated signaling activity in both Jak- and PI3K-dependent pathways (Figure 3a). In uninhibited OT-1 cells, ∼26% of cells expressed the nuclear proliferation antigen, Ki67, after 5 days, whereas F5 cells had no Ki67+ fraction. The OT-1 proliferating fraction disappeared upon Jak or PI3K inhibition of signaling to F5 levels, but had little or no effect on survival (Figure 5a). To further determine how much signaling was required for proliferation, we again stimulated OT-1 cells with IL-7, titrated their induced signaling by varying the dose of Jak Inhibitor I and compared their signal–response relationships to uninhibited F5 cells. Viability and CD8α expression showed quickly saturating and linear relationships to pGSK3 signaling, respectively (Figures 5b and c), as observed at earlier time points (Figures 4d and f). In contrast, proliferation sharply increased over a very narrow range of pGSK3 signaling (Figure 5d). Furthermore, this sharp increase in proliferation occurred above ∼70% of the maximum OT-1 signaling, which is well above the maximum signaling obtainable by F5 cells, as well as the threshold signaling level required for survival (Figure 5b). These data suggest that the IL-7 signaling network encodes distinct signaling thresholds for different downstream responses, with the capacity to achieve different responses determined by surface IL-7R expression.
Figure 5.
Proliferation requires higher threshold IL-7R signaling capacity than survival. (a) Comparison of IL-7-induced responses in OT-1 cells with signaling reduced to levels achievable by F5 cells. 24-h GSK3 phosphorylation and 5-day CD8α surface expression, viability and Ki67+ proliferating fraction following stimulation with 10 ng ml−1 IL-7 for uninhibited OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells compared with OT-1 cells treated with 0.0625 μM of Jak Inhibitor I or 1 μM of the PI3K inhibitor PI-103. Relationships between IL-7-induced signaling at 24 h (GSK3 phosphorylation) and the following responses at 5 days: (b) viability, (c) CD8α surface expression and (d) proliferation as measured by % Ki67+ cells, for OT-1 TCR-tg naïve (CD44lo) CD8+ T cells treated with 10 ng ml−1 IL-7 and varying doses of Jak Inhibitor I, compared with uninhibited F5 cells. Responses are normalized to uninhibited OT-1 controls, and the dashed vertical lines indicate signaling levels in uninhibited OT-1 and F5 cells. Data (a–d) are representative of two independent experiments (error bar=±1s.d.).
IL-7 influences relative abundance of CD5hiIL-7Rhi and CD5loIL-7Rlo T cells in vivo
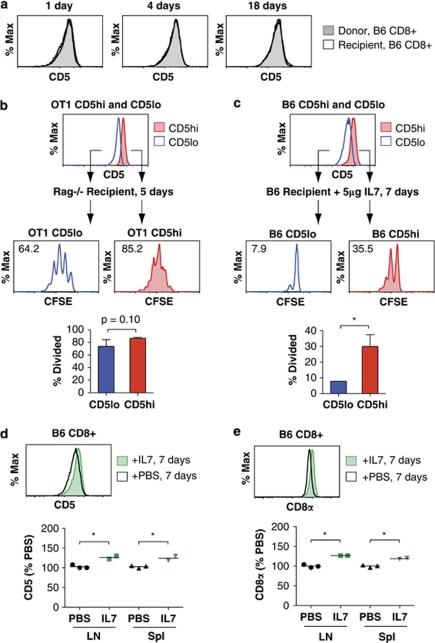
We sought to determine whether IL-7 causes selective proliferation or persistence of CD5hi and CD5lo T cells in vivo, even in the presence of other homeostatic stimuli. The amount of IL-7 in vivo is thought to be highly limiting, which could favor the relative survival of CD5lo cells. To test this, we transferred naïve B6.Thy1.2+ CD8+ T cells into age- and sex-matched B6.Thy1.1+ mice and followed their CD5 profile over 3 weeks (Figure 6a). Although the number of transferred cells declined steadily (Supplementary Figure 4a), there was no change in their CD5 profile compared with the naïve CD8+ T cells of the recipient. As minimal proliferation of naïve T cells is observed in untreated lymphoreplete hosts,1, 2 maintenance of the CD5 profile should require equivalent turnover and rates of thymic export between CD5hi and CD5lo clones. Thus, IL-7 levels in lymphoreplete mice favor neither CD5hi- nor CD5lo-expressing T cells and can be said to maximize the diversity of CD5 expression.
Figure 6.
Manipulation of in vivo IL-7 shifts the abundance of CD5hiIL7Rhi and CD5loIL7Rlo CD8+ T-cell subsets. (a) CD5 expression profiles of donor versus recipient polyclonal naïve (CD44lo) CD8+ T cells followed over 3 weeks for donor C57BL/6.Thy1.2+ CD44lo CD8+ T cells adoptively transferred into congenic age- and sex-matched C57BL/6.Thy1.1+ recipients. (b) CD5 expression of OT-1 TCR-tg naïve (CD44lo) CD8+ T cells sorted into CD5hi and CD5lo expressing fractions (top panel) and their proliferation 5 days after adoptive transfer into syngeneic Rag1−/− hosts, as assessed by CFSE dilution of donor cells recovered from recipient spleens (middle panels) and quantified as the fraction of cells divided (bottom panel). (c) CD5 expression of C57BL/6.Thy1.2+ naïve (CD44lo) CD8+ T cells sorted into CD5hi and CD5lo expressing fractions (top panel) and their proliferation 7 days after adoptive transfer into lymphoreplete C57BL/6.Thy1.1+ hosts given 5 μg IL-7 by mini-osmotic pump infusion over 7 days, as assessed by CFSE dilution of donor cells recovered from recipient spleens (middle panels) and quantified as the percent of cells divided (bottom panel). Comparison of the (d) CD5 and (e) CD8α surface expression profiles of CD8+ T cells recovered from the lymph nodes of lymphoreplete C57BL/6 mice given PBS versus 5 μg IL-7 by mini-osmotic pump over 7 days. A minimum of two mice were used for each experimental condition. Data are representative of two independent experiments (error bar=±1s.d.). *P<0.05.
Excess IL-7 present during lymphopenia or exogenous IL-7 therapy induces proliferation of naïve T cells in vivo.1, 2 Demonstrating that naïve T cells have intrinsically heterogeneous responsiveness to IL-7 in vivo is difficult, as these cells may simultaneously receive different levels of spMHC signaling. We therefore exploited the fact that even within a population of TCR-tg T cells, there is some variance in CD5 expression. We sorted naïve OT-1 cells into CD5hi and CD5lo populations with an ∼2.5-fold difference in mean CD5 levels but with equivalent TCR expression (Figure 6b and Supplementary Figures 4b and c). Naïve OT-1 cells sorted into CD5hi and CD5lo populations showed a small but statistically significant difference (∼4%) in their median IL-7Rα surface expression levels (Supplementary Figure 4c). Though small, this difference is, as expected, correspondingly smaller than the ∼15% difference observed for polyclonal CD5hi and CD5lo T cells (Figure 3c). At 5 days post transfer into syngeneic Rag1−/− hosts, on an average 85% of CD5hi OT-1 cells had undergone division compared with 74% of CD5lo OT-1 cells (Figure 6b). Thus, even in the presence of spMHC, T cells expressing the same TCR can have small differences in IL-7R levels and accompanying IL-7-driven proliferation in vivo.
We then asked whether exogenous IL-7 treatment in polyclonal lymphoreplete mice might produce similar effects. Naïve CD8+ CD5hi and CD5lo T cells (Supplementary Figure 4d) were transferred into congenic Thy1.1+ mice bearing mini-osmotic pumps that released 5 μg IL-7 over 7 days (Figure 6c). A greater fraction (35%) of CD5hi T cells underwent division than CD5lo T cells (7.9%). No proliferation was seen in control mice receiving PBS only (data not shown). We observed modest but significant shifts towards higher CD5 expression in the total CD8+ T-cell population of mice receiving IL-7 versus PBS over 7 days (Figure 6d), and increased IL-7R-mediated signaling reflected by an increase in total CD8α expression (Figure 6e). Although modulation of CD5 expression arising from cross-talk between IL-7 and TCR signaling cannot be formally excluded, in vitro IL-7 independence of CD5 expression (Figure 1d) and enhanced CD5hi T-cell subset proliferation upon IL-7 treatment (Figure 6c) suggests that the latter contributes significantly to skewing of CD5 expression. These results demonstrate that IL-7 therapy could modulate the composition of the naïve T-cell repertoire in part by inducing selective proliferation of CD5hi cells.
IL-7R levels suggest effective in vivo IL-7 concentrations supporting homeostasis
We wondered whether the observed in vitro and in vivo behaviors could be related via an ‘effective homeostatic concentration' of IL-7, at which the diversity of CD5/IL-7R expression among CD8+ T cells in vivo is maintained. Serum IL-7 concentrations in lymphoreplete mice have been measured,28 but may not reflect the local availability of IL-7 in lymphoid organs.8, 29, 30 Moreover, other homeostatic cytokines that also signal through the common γ-chain, such as IL-15, may support survival and LIP of T cells in vivo (reviewed in 2), but concomitantly repress IL-7Rα and induce CD8α expression through signaling pathways shared with IL-7R.9, 23 We therefore considered the possibility that IL-7Rα and CD8α expression on freshly isolated CD8+ cells might provide an operational indicator of the magnitude of overall effective homeostatic cytokine signaling received in vivo, rather than presuming translation to a precise and specific IL-7 concentration. Comparison of the IL-7Rα expression of freshly isolated OT-1 and F5 cells to receptor levels of the same cells following 24 h in vitro treatment with varying doses of IL-7, indicated that in vivo cytokine exposures correspond to in vitro IL-7 concentrations ranging from 0.01 to 0.1 ng ml−1 (Figure 7a). Interestingly, over this range of IL-7 concentrations in vitro, OT-1 and F5 cells had equivalent viability (Figure 7b), but neither proliferated (Figure 7c). This mirrored the behavior we observed with adoptively transferred T cells in lymphoreplete hosts (Figure 6a), allowing for a homeostatic balance between CD5hi and CD5lo T cells in vivo.
Figure 7.
IL-7R level on CD8+ T cells suggests effective in vivo IL-7 concentrations supporting homeostasis. (a) Surface IL-7Rα expression of OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells rested overnight in cytokine-free media and treated 24 h with varying IL-7 concentrations ranging from 0.0001–100 ng ml−1, compared with the IL-7Rα expression of freshly isolated cells, indicating effective in vivo homeostatic cytokine concentrations reflect in vitro IL-7 concentrations of 0.01–0.1 ng ml−1 at the level of receptor suppression. (b) 24-h viability and (c) 5-day proliferation (%Ki67+ fraction) for OT-1 and F5 TCR-tg naïve (CD44lo) CD8+ T cells treated with varying IL-7 concentrations in vitro as described in a, showing that over the effective in vivo IL-7 concentration range indicated in a, both cell types survive, but do not proliferate. Bioassay for effective in vivo IL-7 levels in which (d) 106 2C Thy1.1+ Rag1−/− naïve (CD44lo) CD8+ T cells were transferred into Thy1.2+ B6, OT-1 Rag1−/−, 2C Rag1−/−, F5 Rag1−/− or Rag1−/− hosts (minimum of three mice per recipient type), and (e) the relative effective IL-7 levels between hosts were inferred from the IL-7Rα and CD8α expression of Thy1.1+ donor cells. (f) IL-7Rα expression of donor cells showed a strong linear correspondence with number of CD8+ T cells in recipient spleens. Data are representative of two independent experiments (error bar=±1 s.d.).
We wanted to determine whether our estimates of effective in vivo homeostatic cytokine concentrations in OT-1 and F5 TCR-tg mice also applied to wild-type lymphoreplete mice. To extend our assay to compare the relative effective homeostatic cytokine levels between mice, we adoptively transferred congenic 2C Thy1.1+ Rag1−/− T cells into B6, Rag1−/−, OT-1, 2C and F5 hosts (Figure 7d), and compared the relative IL-7Rα and CD8α expression on the transferred cells in the recipient spleens after 18 h (Figures 7e and f). This assay indicated that Rag1−/− mice have relatively higher levels of available homeostatic cytokines, whereas homeostatic cytokine levels were similar among OT-1, 2C, F5 and B6 mice, albeit with subtle differences in the order: F5>2C>B6>OT-1 (Figure 7e). We do not observe significant differences in recovery of donor cells between recipients reflecting relative survival (data not shown), though mild differences in survival would likely not be apparent on the examined timescale of <1 day. These data additionally indicate that the effective in vivo homeostatic cytokine concentration in B6 mice also corresponds to in vitro IL-7 concentrations of 0.01–0.1 ng ml−1. Donor cell IL-7Rα expression showed a strong correlation with the number of CD8+ T cells in the spleens of the recipient mice (Figure 7f), supporting the notion that in vivo homeostatic cytokine levels scale with the number of T cells consuming cytokine.7, 8
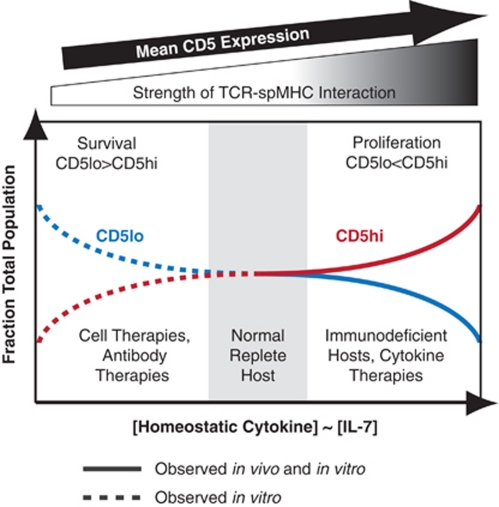
Altogether, these data are consistent with a novel model in which physiological levels of homeostatic cytokines contribute to maintaining diversity of CD5/IL-7R expression in the naïve CD8+ T-cell population by supporting T-cell survival without clone-selective proliferation (Figure 8). Increasing IL-7 levels would consequentially provide capability for selective proliferation of CD5hiIL-7Rhi T-cells, whereas, conversely, depleting IL-7 may conceivably favor selective persistence of CD5loIL-7Rlo T cells.
Figure 8.
Model for the role of IL-7 in the homeostasis of CD5 distributions in the CD8+ T-cell repertoire. Model depicting IL-7-mediated homeostasis in the diversity of CD5 expression among the naïve CD8+ T-cell repertoire. At effective IL-7 concentrations in normal lymphoreplete hosts, the diversity of CD5 expression is preserved. High [IL-7] shifts the CD8+ T-cell population towards high CD5 expression because of the selective proliferation of CD5hi cells, whereas low [IL-7] may conceivably favor a population with low CD5 expression because of the selective survival of CD5lo subsets.
Discussion
Although IL-7 has a well-established role in supporting naive CD8+ T-cell homeostasis, it has been generally believed that these cells have a uniform intrinsic reliance on, and responsiveness to, available cytokines. Instead, differences in the homeostatic survival and proliferation of T cells have been so far attributed to variations in the strength and/or frequency with which T cells can actively engage cognate spMHC through their unique TCRs.1, 2 Our study here reveals an additional, complementary layer of functional heterogeneity amongst CD8+ T cells in their responsiveness to IL-7, even when removed from TCR stimulation. Relative CD5 expression was found to be a stable, heritable and IL-7-independent marker for T cells differing in their proliferation and survival responses to IL-7 stimulation. Interestingly, we find that although all T cells survive in response to IL-7 stimulation, only CD5hi cells proliferate. Conversely, CD5lo cells have a survival advantage in the absence of homeostatic stimulation. Importantly, variations in IL-7 responsiveness between T-cell clones were shown to be relevant even in the context of other homeostatic stimuli in vivo, with elevated IL-7 levels leading to selective proliferation of CD5hi T cells independent of TCR specificity. Although the enhanced LIP of CD5hi T-cell clones has been previously attributed to their greater avidity for spMHC,11, 13 our data suggest that differential IL-7 responsiveness may also potentiate proliferation. Moreover, it suggests that both IL-7R and TCR signaling contribute to the diversity of the T-cell pool, and that IL-7 does not strictly control population size alone.
Although we found CD5 expression to be a useful marker for heterogeneous IL-7 responsiveness, subtle correlated differences in IL-7R expression were found to mechanistically underlie varying IL-7 sensitivities. Although IL-7R expression is known to vary across the T-cell pool, differences have predominantly been attributed to heterogeneous extracellular environments, and considered insufficient for generating response diversity.8, 9, 15, 23, 31 Nonetheless, our quantitative analysis of IL-7R-mediated signaling reveals shared nonlinear signal-response relationships across T-cell clones that can generate striking differences in functional responses via comparably small variations in receptor expression. A threshold level of signaling required for proliferation well above that required for survival also explains why all T cells could survive, but only those with critically high levels of IL-7Rα could proliferate in response to high doses of IL-7. Thus, although differences in the IL-7-dose requirements for proliferation versus survival have been identified,32 our study reveals that proliferation occurs heterogeneously across polyclonal T-cell populations, and is dictated by the level of receptor expression-limited signaling produced by an individual T cell. Accordingly, signaling thresholds defined here at the population level are likely even more striking when examined for individual cells. We find that even among naïve T cells from TCR-tg Rag−/− mice, CD5 expression marks variation in mean IL-7R levels and different proliferation capacities at elevated IL-7 levels in vivo (Figure 6b, Supplementary Figure 4c). There remains considerable variation in IL-7R expression even within these populations, and this may also explain why only a fraction of the population proliferates.
Very recently, Cho et al.33 also reported enhanced responsiveness of CD5hi CD8+ T cells to IL-7, and demonstrated that the selective proliferation of CD5hi CD8+ T cells also extends to stimulation by common γ-chain cytokines IL-2 and IL-15. These differences in sensitivity and signaling capacity were attributed to higher expression of GM1-containing lipid rafts in CD5hi cells, proposed to enhance signaling from cytokine receptors primarily via receptor clustering. Our measurements here indicate that the downstream signaling generated per receptor is essentially equivalent in CD5hi versus CD5lo T cells (Figures 4a and b), and that even the modest quantitative differences in receptor number per cell that were observed by Cho et al., as well as ourselves, can explain the differences in their responses to IL-7. Cho et al.33 also find that lipid-raft expression levels and homeostatic cytokine responsiveness rely upon sustained TCR contact with spMHC, although notably residual cytokine responsiveness persists in MHC-I knockout T cells even after resting for several days in MHC-I deficient hosts. We observe heterogeneous IL-7 responsiveness in MHC-I deficient cells that is correlated with CD5 levels (Figure 1f). We also find that these proliferation differences are transiently increased after first resting the cells overnight in cytokine-free media (Figure 1b), presumably resulting from increased IL-7R expression (Figure 3b). We further see decay in CD5 expression once cells are withdrawn from spMHC (Figure 1c), but this decrease occurs over many days, and the relative expression between T-cell clones is maintained. Persistent effects of TCR signaling received before cell isolation might similarly give rise to long-term differences in expression of other signaling network mediators regulating cytokine responsiveness, including IL-7Rα, though defining the mechanisms involved in establishing and maintaining their expression requires further study. Independent of whether long-term ‘covert' TCR signaling underlies varying cytokine responsiveness, our data highlight that even mild quantitative differences in cytokine receptor expression can have a surprisingly critical role in directly giving rise to substantive functional differences in proliferation responses.
Diversity in CD5, CD8α and IL-7Rα expression amongst naïve T cells in vivo has been largely attributed to extrinsic heterogeneities in the local spMHC and IL-7 environments.9, 15, 23, 31 On the basis of the requirement of naïve T cells to engage spMHC for the maintenance of their CD5 levels in vivo,15 CD5 expression has been interpreted as a surrogate measure for the strength of spMHC-induced signaling in the periphery.11, 13, 15, 17 However, we find that differences in basal CD5 levels among naive T cells are stably maintained even after withdrawal from spMHC signals. Similarly, although the broad distribution of IL-7R expression among naïve T cells in vivo has been attributed solely to the heterogeneity in the spatio-temporal presentation of IL-7 between T cells cycling in and out of lymphoid organs,8 our data suggest that intrinsic differences in basal IL-7R expression also contribute to the heterogeneity in IL-7R expression levels in naïve CD8+ T cells. Although we find that variable IL-7R expression is sufficient to explain heterogeneous IL-7 responsiveness of mature T cells, the observed correlation between CD5 and IL-7R levels may reflect underlying co-regulation of these genes that is established during T-cell development, and possibly reinforced by interactions in the periphery. For instance, CD5 expression in T cells is thought to reflect the strength of thymic selection,18 and signaling network changes during selection may also predetermine IL-7R expression levels in mature T cells. Although determination of potential developmental connections was outside the scope of this study, future work should address the role of TCR signaling received during thymic selection versus interactions with spMHC in the periphery in maintaining differences in expression patterns between CD5hi and CD5lo cells.
A study by Park et al.9 has suggested that mutual feedback between TCR and IL-7R signaling pathways underlies correlations between IL-7R, CD5 and CD8α expression among naïve T cells. In what is termed the ‘co-receptor tuning' model, IL-7R signaling induces the transcription of CD8α to increase TCR signaling, which negatively feeds back to reduce IL-7R signaling, which in turn reduces CD8α and increases IL-7Rα expression. Reduced CD8α expression on CD5hi T cells is proposed to ‘tune down' their excessive TCR signaling. A lack of IL-7-induced Stat5 phosphorylation in freshly isolated CD5hi male HY TCR-tg CD8+ T cells has been used to support this model. However, our studies did not reveal any signaling defects in freshly isolated naïve OT-1 or polyclonal CD5hi CD8+ T cells (Supplementary Figure 2c and data not shown). This may reflect differences in their thymic development compared with the male HY T cells used in the Park et al. study, which, unlike OT-1 cells, are selected on agonist ligands. The ‘co-receptor tuning' model is also supported by a positive correlation of IL-7Rα, and inverse correlation of CD8α, with CD5 expression for a panel of freshly isolated TCR-tg cells. However, our data suggest that increased receptor expression may reflect intrinsic differences in the basal level of IL-7Rα expressed rather than signal inhibition reducing negative feedback. These trends in CD5, CD8α and IL-7Rα expression may also be partly explained by decreased effective IL-7 levels in TCR-tg mice bearing T cells with higher CD5 expression (Figure 6).
Recent studies have shed light on intra- and extra-cellular mechanisms regulating the ability of T cells to compete for, and respond to, TCR and IL-7R signals. Stronger or more frequent interactions with spMHC may provide preferred access to IL-7 localized at the surface of antigen-presenting cells and/or signal for IL-7 production,10, 34 and cytokine stimulation appears in some cases to ‘prime' T cells for more robust responses to antigen stimulation.35, 36, 37 Yet inhibition of IL-7R signaling by TCR signals has also been proposed to balance overall homeostatic signaling between T-cell clones.9 It remains unclear if and how these complex interactions quantitatively mediate or accentuate differences in TCR–spMHC affinities during homeostasis and under perturbations in the cytokine environment. Rather than attempting to mimic the complex in vivo environment and identify the nature and extent of cross-talk between IL-7 and spMHC-induced signaling, we chose to carefully quantify IL-7-induced responses in the absence of spMHC, and then determine whether differences in IL-7 sensitivity persist upon reintroduction of other complex homeostatic cues in vivo. Our study demonstrates intrinsic variations in IL-7 responsiveness across T-cell clones that are not fully balanced by other homeostatic signaling in vivo upon acute changes in IL-7 concentration. Moreover, T-cell proliferation under supra-physiological IL-7 concentrations in vivo is more robust than achievable by IL-7 stimulation alone, emphasizing the critical role of spMHC signals.
Our data support the novel finding that reduced IL-7 sensitivity and spMHC affinity in CD5lo T cells is accompanied by an increased capacity to survive in the absence of homeostatic cues. This coupling may be critical for maintaining and restoring a dynamic homeostatic balance between T cells with different abilities to compete for, and respond to, limited homeostatic resources. Although defining mechanisms supporting prolonged basal survival requires studies beyond the scope of this paper, our data point to intrinsic differences in metabolic function between CD5hi and CD5lo T cells. CD5lo T cells have reduced size, indicative of a more quiescent state and preferential utilization of mitochondrial respiration.25 Further, F5 cells exhibit enhanced IL-7-independent glucose uptake, and reduced sensitivity to inhibition of PI3K activity essential for glucose uptake and other processes supporting survival.38 Further, the balance of pro- versus anti-apoptotic proteins regulates susceptibility to apoptosis, and PI3K activity and glucose uptake are known to impact the expression, activity and stability of these proteins.39, 40, 41, 42, 43, 44 CD5lo cells may have lower basal expression of pro-apoptotic factors, such as Bim,45 than CD5hi cells, whereas CD5hi cells compensate via their enhanced ability to signal for IL-7-dependent increases in anti-apoptotic proteins, such as Bcl2 (Figures 3d and e).
Interestingly, recent studies suggest elevated PI3K activity in CD5lo cells could be connected to their decreased IL-7R expression. Kerdiles et al.46 demonstrated that Foxo1, a target of PI3K, is a transcription factor for IL-7R. Knocking out Foxo1, or inhibition of the PI3K phosphatase PTEN lead to decreased IL-7Rα expression in CD8+ T cells. Decreased sensitivity to PI3K inhibition in F5 cells (Figure 3e) is consistent with lower PTEN activity, and our preliminary studies support decreased Foxo1 expression in F5 cells relative to OT-1 cells (data not shown). These data could suggest an interesting model whereby PI3K activity regulates basal IL-7Rα levels and survival in the absence of cytokine, which in turn regulates the ability to activate Jak-dependent signaling pathways in the presence of IL-7.
Because of its diverse role in lymphocyte development and function, IL-7 has prospective therapeutic uses in restoring compromised immune systems following chemotherapy or viral infections, and as an adjuvant for vaccines and cancer immunotherapies.47, 48, 49 Two rhIL-7 phase I clinical trials have recently shown an IL-7-dose-dependent increase in CD8+ and CD4+ T-cell numbers,50, 51 and a concomitant increase in the diversity of TCR Vβ usage.51 Our results raise an additional mechanism by which IL-7 affects the diversity of the T-cell repertoire: regulating the diversity of TCR-spMHC avidities, indicated by CD5 expression, via correlated differences in their IL-7R expression and IL-7 responsiveness. Although TCR Vβ diversity increases with IL-7 therapy, our model suggests that the homeostatic diversity of CD5 expression amongst T-cell clones is maximized at physiological IL-7 levels. Our findings suggest that this equilibrium is achieved by maintaining an IL-7 level that does not promote selective proliferation or persistence of CD5hi or CD5lo cells. This may result from balancing IL-7 production with the overall size of the T-cell population consuming IL-7.7, 8 Notably, we have shown here that IL-7 treatment can result in the preferential expansion of CD5hi T cells, which are potentially autoreactive and have been proposed to contribute to the development and progression of autoimmune disorders.52, 53 Nevertheless, this effect may prove to be beneficial in the use of IL-7 as an adjuvant in cancer immunotherapies.48, 54 Enhanced IL-7R signaling has also been proposed to contribute to T-cell leukemogenesis.55 Thus, although IL-7 therapies may expand overall T-cell numbers, it may have the unintended consequence of preferentially expanding undesirable T-cell population subsets. Given the increasing interest in IL-7-based therapies, further investigation of the intrinsic differences in the signaling networks across T-cell populations will help us understand the clinical impact of skewing the T-cell repertoire towards a CD5hi or CD5lo phenotype.
Methods
Mice
C57BL/6J (B6) mice, and B6.CD90.1/Thy1.1 congenic mice (B6.PL-Thy1a/CyJ) were purchased from the Jackson Laboratory (Bar Harbor, ME, USA). OT-1, 2C and F5 TCR-tg mice were backcrossed onto the B6.Rag1−/− background for >20 generations. B6.H-2Kb−/−Db−/− mice were obtained from Taconic Farms (Hudon, NY, USA). Sub-lethally irradiated (600 rads) B6.Rag1−/− mice, which were reconstituted with bone marrow from B6 H-2Kb−/−Db−/− mice, were used as a source of H-2Kb−/−Db−/− double-deficient CD8+ T cells, as previously described.56, 57 All mice used were maintained according to the institutional guidelines, and age- and sex-matched mice, between 6 and 16 weeks of age, were used for experiments.
Flow cytometry
Cells were suspended in phosphate-buffered saline (PBS) containing 0.5% bovine serum albumin, 0.1% NaN3 and 2.5 μg ml−1 Fc Block for 10 min at 4 °C and incubated with fluorescently tagged antibodies for 40 min at 4 °C. For detection of intracellular signaling, Live/Dead Fixable Blue Dead Cell Stain (Invitrogen, Carlsbad, CA, USA) was added to cells for 10 min before fixation with 4% formaldehyde for 10 min and permeabilization with 90% methanol for >2 h at −20 °C. Cells were washed twice and then resuspended in PBS with 0.5% bovine serum albumin and 2.5 μg ml−1 Fc Block (2.4G2) (BD Biosciences, San Diego, CA, USA) for 10 min at 4 °C before addition of fluorescently tagged antibodies against intracellular and cell surface antigens for 40 min at room temperature. Nonspecific background fluorescence was determined by staining with isotype-matched antibodies. Cells were washed twice before multi-parameter flow cytometric detection on a BD LSRII (Becton Dickinson, San Jose, CA, USA). Cell viabilities for live cells were determined by addition of 1.5 mM DAPI (Invitrogen). CFSE staining was performed as described previously.11 The following monoclonal antibodies were used: Bcl2 (3F11), Stat5 (89), pStat5 Y694 (47), Ki67 (B56), Mouse IgG1, κ isotype (MOPC-21) (BD Biosciences), pGSK3 (37F11), GSK3 (9315), β-Actin (8H10D10) (Cell Signaling Technologies, Danvers, MA, USA), IL-7Rα/CD127 (SB/199), CD5 (53-7.3), CD44 (IM7), CD69 (H1.2F3), CD62L (MEL-14), TCR, CD8α (53-6.7), CD25 (PC61), CD122 (TM-b1),Thy1.1/CD90.1 (OX-7), Thy1.2/CD90.2 (30-H12), H-2Kb/Db (28-8-6), mouse IgG2α,κ isotype (MOPC-173), Rat IgG2α,κ isotype (RTK2758) and Rat IgG2β,κ isotype (RTK4530) (Biolegend, San Diego, CA, USA).
T-cell purification, cell sorting and in vitro culture
CD8+ T cells were purified from single cell suspensions of lymph nodes or spleen using an EasySep mouse CD8+ T cell enrichment kit (Stem Cell Technologies, Vancouver, BC, Canada). For enrichment of the naïve lymphocyte fraction, T cells stained with phycoerythrin-conjugated anti-CD44 were removed using either fluorescent cell sorting or anti-phycoerythrin microbeads (Miltenyi Biotech, Auburn, CA, USA). For all experiments that involve sorting on CD5 expression, T cells expressing the maximum 20% and the minimum 20% levels of CD5 were sorted into CD5hi and CD5lo fractions. Purified T cells were cultured in complete RPMI-1640 medium containing 10% fetal calf serum at 37 °C and 5% CO2. Cells were assayed either immediately following isolation or, where indicated, cells were rested overnight (∼16 h) in medium without cytokine to eliminate any TCR and cytokine signaling before treatment. Unless otherwise indicated, cells were cultured at densities of 2–3.5 × 105 cells per ml. Recombinant murine IL-7 (Peprotech, Rocky Hill, NJ, USA) was added to the culture media at concentrations ranging from 0.0001 to 100 ng ml−1. OT-1 and F5 memory-like T cells were generated by activation on plate-coated anti-CD3 antibody (BD Biosciences) for 3 days in the presence of 20 ng ml−1 mIL-2 (Peprotech) and by differentiation in 40 ng ml−1 mIL-15 (Peprotech) for an additional 3 days after washing thrice with cytokine-free media. Finally, the response to IL-7 was measured after the cells were cultured overnight without any cytokines after washing thrice with cytokine-free media. The PI3K inhibitors LY2904002 (0.1–200 μM), PI-103 (0.01–10 μM) and the Jak family inhibitor, Jak Inhibitor I (0.004–2 μM) (Calbiochem, EMD Biosciences, Gibbstown, NJ, USA) were added to the culture for 30 min before cytokine addition, at the indicated concentrations.
Western blot analysis of total protein expression
T cells were cultured in cytokine-free media for 16 h, and viable T cells were isolated by Ficoll-Paque Plus gradient separation (GE Healthcare, Piscataway, NJ, USA). T cells were lysed in RIPA lysis buffer (Thermo Scientific, Rockford, IL, USA) containing PhosStop Phosphatase Inhibitor, Complete Mini Protease Inhibitor (Roche, Indianapolis, IL, USA) and 0.1 M phenylmethylsulphonyl fluoride. Lysates equivalent to 6 × 105 cells were subjected to SDS-poly acrylamide gel electrophoresis (Invitrogen) and blots were probed with antibodies against Stat5 (BD Biosciences), β-actin and GSK3 (Cell Signaling Technologies), and imaged on the LICOR Odyssey Infrared Imaging System (Licor Biosciences, Lincoln, NE, USA).
Glucose uptake
Glucose uptake was measured as previously described,32 with minor modifications. T cells were cultured for 24 h in presence or absence of 10 ng ml−1 IL-7. Viable cells were isolated by Ficoll-Paque Plus gradient separation. T cells (8.5 × 105) were incubated for 30 min in serum- and glucose-free RPMI 1640 media. Glucose uptake was initiated by adding labeled 2-deoxy-D[1-3H] glucose (Amersham Pharmacia Biosciences, Schenectady, NY, USA) to a final concentration of 0.1 mM (4 μCi ml−1). Cells were incubated for 45 min at 37 °C, washed thrice in cold glucose- and serum-free RPMI 1640 media and solubilized in 525 μl of 1% SDS. Radioactivity in 470 μl of the sample was measured by liquid scintillation.
IL-7 infusion
IL-7 (or PBS) was administered to mice by subcutaneous implantation of mini-osmotic pumps (#1007D, Alzet, Cupertino, CA, USA). Before implantation, mini-osmotic pumps that release 0.5 μl h−1 over 7 days were filled with 100 μl of PBS or PBS containing 5 μg of IL-7 (Peprotech). Pumps were implanted into a 2-cm-long subcutaneous pocket over the right flank created through a 0.5 cm mid-scapular incision and closed using a wound clip with application of a Betadine (Purdue Pharma, Stamford, CT, USA) antiseptic on the incision site. Lymph nodes and spleen were harvested after 7 days.
Adoptive transfer assays
For all experiments involving adoptive transfer of T cells, purified naïve CD8+ T cells were resuspended in Hank's buffered salt solution and injected retro-orbitally into age- and sex-matched recipients.
Bioassay for comparison of in vivo IL-7 levels across mice
In all, 106 purified Thy1.1+ 2C TCR-tg naïve CD8+ T cells were adoptively transferred into syngeneic Thy1.2+ mice, and the relative IL-7 levels in vivo in different recipients were determined by comparing IL-7Rα and CD8α expression on the Thy1.1+ donor cells recovered from the recipient spleens and lymph nodes after 18 h. A minimum of three mice of each genotype were examined for each experiment.
Statistical analysis
GraphPad Prism software (GraphPad Software, La Jolla, CA, USA) was used for statistical analysis. P-values were calculated with two-tailed Student's t-test. P-values of less than 0.05 were considered significant.
Acknowledgments
We thank Drs Alfred Singer, Herman Eisen and Ching-Hung Shen for advice and discussion. This work was supported in part by NIH grants AI69208 (to JC) and GM068762 (to DAL), and the MIT Cancer Center Core Grant for facilities, and fellowships from the Siebel Foundation and the MIT NCI Integrative Cancer Biology Program (to MJP). DJI is an investigator of the Howard Hughes Medical Institute.
The authors declare no conflict of interest.
Footnotes
The Supplementary Information that accompanies this paper is available on the Immunology and Cell Biology website (http://www.nature.com/icb)
Supplementary Material
References
- Takada K, Jameson SC. Naive T cell homeostasis: from awareness of space to a sense of place. Nat Rev Immunol. 2009;9:823–832. doi: 10.1038/nri2657. [DOI] [PubMed] [Google Scholar]
- Surh CD, Sprent J. Homeostasis of naive and memory T cells. Immunity. 2008;29:848–862. doi: 10.1016/j.immuni.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Mahajan VS, Leskov IB, Chen JZ. Homeostasis of T cell diversity. Cell Mol Immunol. 2005;2:1–10. [PubMed] [Google Scholar]
- von Freeden-Jeffry U, Vieira P, Lucian LA, McNeil T, Burdach SE, Murray R. Lymphopenia in interleukin (IL)-7 gene-deleted mice identifies IL-7 as a nonredundant cytokine. J Exp Med. 1995;181:1519–1526. doi: 10.1084/jem.181.4.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiselhart LA, Humphries CA, Gregorio TA, Mou S, Subleski J, Komschlies KL. IL-7 administration alters the CD4:CD8 ratio, increases T cell numbers, and increases T cell function in the absence of activation. J Immunol. 2001;166:3019–3027. doi: 10.4049/jimmunol.166.5.3019. [DOI] [PubMed] [Google Scholar]
- Mertsching E, Burdet C, Ceredig R. IL-7 transgenic mice: analysis of the role of IL-7 in the differentiation of thymocytes in vivo and in vitro. Int Immunol. 1995;7:401–414. doi: 10.1093/intimm/7.3.401. [DOI] [PubMed] [Google Scholar]
- Fry TJ, Mackall CL. The many faces of IL-7: from lymphopoiesis to peripheral T cell maintenance. J Immunol. 2005;174:6571–6576. doi: 10.4049/jimmunol.174.11.6571. [DOI] [PubMed] [Google Scholar]
- Mazzucchelli R, Durum SK. Interleukin-7 receptor expression: intelligent design. Nat Rev Immunol. 2007;7:144–154. doi: 10.1038/nri2023. [DOI] [PubMed] [Google Scholar]
- Park JH, Adoro S, Lucas PJ, Sarafova SD, Alag AS, Doan LL, et al. Coreceptor tuning': cytokine signals transcriptionally tailor CD8 coreceptor expression to the self-specificity of the TCR. Nat Immunol. 2007;8:1049–1059. doi: 10.1038/ni1512. [DOI] [PubMed] [Google Scholar]
- Agenes F, Dangy JP, Kirberg J. T cell receptor contact to restricting MHC molecules is a prerequisite for peripheral interclonal T cell competition. J Exp Med. 2008;205:2735–2743. doi: 10.1084/jem.20070467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge Q, Bai A, Jones B, Eisen HN, Chen J. Competition for self-peptide-MHC complexes and cytokines between naive and memory CD8+ T cells expressing the same or different T cell receptors. Proc Natl Acad Sci USA. 2004;101:3041–3046. doi: 10.1073/pnas.0307339101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Y, Legrand N, Freitas AA. The clone size of peripheral CD8T cells is regulated by TCR promiscuity. J Exp Med. 2006;203:1643–1649. doi: 10.1084/jem.20052174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kieper WC, Burghardt JT, Surh CD. A role for TCR affinity in regulating naive T cell homeostasis. J Immunol. 2004;172:40–44. doi: 10.4049/jimmunol.172.1.40. [DOI] [PubMed] [Google Scholar]
- Tarakhovsky A, Kanner SB, Hombach J, Ledbetter JA, Muller W, Killeen N, et al. A role for CD5 in TCR-mediated signal transduction and thymocyte selection. Science. 1995;269:535–537. doi: 10.1126/science.7542801. [DOI] [PubMed] [Google Scholar]
- Smith K, Seddon B, Purbhoo MA, Zamoyska R, Fisher AG, Merkenschlager M. Sensory adaptation in naive peripheral CD4T cells. J Exp Med. 2001;194:1253–1261. doi: 10.1084/jem.194.9.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raman C. CD5, an important regulator of lymphocyte selection and immune tolerance. Immunol Res. 2002;26:255–263. doi: 10.1385/IR:26:1-3:255. [DOI] [PubMed] [Google Scholar]
- Azzam HS, DeJarnette JB, Huang K, Emmons R, Park CS, Sommers CL, et al. Fine tuning of TCR signaling by CD5. J Immunol. 2001;166:5464–5472. doi: 10.4049/jimmunol.166.9.5464. [DOI] [PubMed] [Google Scholar]
- Azzam HS, Grinberg A, Lui K, Shen H, Shores EW, Love PE. CD5 expression is developmentally regulated by T cell receptor (TCR) signals and TCR avidity. J Exp Med. 1998;188:2301–2311. doi: 10.1084/jem.188.12.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown IE, Mashayekhi M, Markiewicz M, Alegre ML, Gajewski TF. Peripheral survival of naive CD8+ T cells. Apoptosis. 2005;10:5–11. doi: 10.1007/s10495-005-6056-9. [DOI] [PubMed] [Google Scholar]
- Dowling MR, Hodgkin PD. Modelling naive T-cell homeostasis: consequences of heritable cellular lifespan during ageing. Immunol Cell Biol. 2009;87:445–456. doi: 10.1038/icb.2009.11. [DOI] [PubMed] [Google Scholar]
- Stirk ER, Molina-Paris C, van den Berg HA. Stochastic niche structure and diversity maintenance in the T cell repertoire. J Theor Biol. 2008;255:237–249. doi: 10.1016/j.jtbi.2008.07.017. [DOI] [PubMed] [Google Scholar]
- Ciupe SM, Devlin BH, Markert ML, Kepler TB. The dynamics of T-cell receptor repertoire diversity following thymus transplantation for DiGeorge anomaly. PLoS Comput Biol. 2009;5:e1000396. doi: 10.1371/journal.pcbi.1000396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JH, Yu Q, Erman B, Appelbaum JS, Montoya-Durango D, Grimes HL, et al. Suppression of IL7Ralpha transcription by IL-7 and other prosurvival cytokines: a novel mechanism for maximizing IL-7-dependent T cell survival. Immunity. 2004;21:289–302. doi: 10.1016/j.immuni.2004.07.016. [DOI] [PubMed] [Google Scholar]
- Leitao C, Freitas AA, Garcia S. The role of TCR specificity and clonal competition during reconstruction of the peripheral T cell pool. J Immunol. 2009;182:5232–5239. doi: 10.4049/jimmunol.0804071. [DOI] [PubMed] [Google Scholar]
- Fox CJ, Hammerman PS, Thompson CB. Fuel feeds function: energy metabolism and the T-cell response. Nat Rev Immunol. 2005;5:844–852. doi: 10.1038/nri1710. [DOI] [PubMed] [Google Scholar]
- Wofford JA, Wieman HL, Jacobs SR, Zhao Y, Rathmell JC. IL-7 promotes Glut1 trafficking and glucose uptake via STAT5-mediated activation of Akt to support T-cell survival. Blood. 2008;111:2101–2111. doi: 10.1182/blood-2007-06-096297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Q, Li WQ, Aiello FB, Mazzucchelli R, Asefa B, Khaled AR, et al. Cell biology of IL-7, a key lymphotrophin. Cytokine Growth Factor Rev. 2005;16:513–533. doi: 10.1016/j.cytogfr.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Guimond M, Veenstra RG, Grindler DJ, Zhang H, Cui Y, Murphy RD, et al. Interleukin 7 signaling in dendritic cells regulates the homeostatic proliferation and niche size of CD4+ T cells. Nat Immunol. 2009;10:149–157. doi: 10.1038/ni.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimura K, Matsubara H, Sogoh S, Kita Y, Sakata T, Nishitani Y, et al. Role of glycosaminoglycans in the regulation of T cell proliferation induced by thymic stroma-derived T cell growth factor. J Immunol. 1991;146:2618–2624. [PubMed] [Google Scholar]
- Mazzucchelli RI, Warming S, Lawrence SM, Ishii M, Abshari M, Washington AV, et al. Visualization and identification of IL-7 producing cells in reporter mice. PLoS One. 2009;4:e7637. doi: 10.1371/journal.pone.0007637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada K, Jameson SC. Self-class I MHC molecules support survival of naive CD8T cells, but depress their functional sensitivity through regulation of CD8 expression levels. J Exp Med. 2009;206:2253–2269. doi: 10.1084/jem.20082553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swainson L, Kinet S, Mongellaz C, Sourisseau M, Henriques T, Taylor N. IL-7-induced proliferation of recent thymic emigrants requires activation of the PI3K pathway. Blood. 2007;109:1034–1042. doi: 10.1182/blood-2006-06-027912. [DOI] [PubMed] [Google Scholar]
- Cho JH, Kim HO, Surh CD, Sprent J. T cell receptor-dependent regulation of lipid rafts controls naive CD8(+) T cell homeostasis. Immunity. 2010;32:214–226. doi: 10.1016/j.immuni.2009.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini M, Pearson C, Seddon B. Regulation of T cell-dendritic cell interactions by IL-7 governs T-cell activation and homeostasis. Blood. 2009;113:5793–5800. doi: 10.1182/blood-2008-12-192252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramanathan S, Dubois S, Gagnon J, Leblanc C, Mariathasan S, Ferbeyre G, et al. Regulation of cytokine-driven functional differentiation of CD8T cells by suppressor of cytokine signaling 1 controls autoimmunity and preserves their proliferative capacity toward foreign antigens. J Immunol. 2010;185:357–366. doi: 10.4049/jimmunol.1000066. [DOI] [PubMed] [Google Scholar]
- Gagnon J, Chen XL, Forand-Boulerice M, Leblanc C, Raman C, Ramanathan S, et al. Increased antigen responsiveness of naive CD8T cells exposed to IL-7 and IL-21 is associated with decreased CD5 expression. Immunol Cell Biol. 2010;88:451–460. doi: 10.1038/icb.2009.109. [DOI] [PubMed] [Google Scholar]
- Ramanathan S, Gagnon J, Dubois S, Forand-Boulerice M, Richter MV, Ilangumaran S. Cytokine synergy in antigen-independent activation and priming of naive CD8+ T lymphocytes. Crit Rev Immunol. 2009;29:219–239. doi: 10.1615/critrevimmunol.v29.i3.30. [DOI] [PubMed] [Google Scholar]
- Manning BD, Cantley LC. AKT/PKB signaling: navigating downstream. Cell. 2007;129:1261–1274. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Heiden MG, Plas DR, Rathmell JC, Fox CJ, Harris MH, Thompson CB. Growth factors can influence cell growth and survival through effects on glucose metabolism. Mol Cell Biol. 2001;21:5899–5912. doi: 10.1128/MCB.21.17.5899-5912.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlob K, Majewski N, Kennedy S, Kandel E, Robey RB, Hay N. Inhibition of early apoptotic events by Akt/PKB is dependent on the first committed step of glycolysis and mitochondrial hexokinase. Genes Dev. 2001;15:1406–1418. doi: 10.1101/gad.889901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathmell JC, Fox CJ, Plas DR, Hammerman PS, Cinalli RM, Thompson CB. Akt-directed glucose metabolism can prevent Bax conformation change and promote growth factor-independent survival. Mol Cell Biol. 2003;23:7315–7328. doi: 10.1128/MCB.23.20.7315-7328.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alves NL, Derks IA, Berk E, Spijker R, van Lier RA, Eldering E. The Noxa/Mcl-1 axis regulates susceptibility to apoptosis under glucose limitation in dividing T cells. Immunity. 2006;24:703–716. doi: 10.1016/j.immuni.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Altman BJ, Coloff JL, Herman CE, Jacobs SR, Wieman HL, et al. Glycogen synthase kinase 3alpha and 3beta mediate a glucose-sensitive antiapoptotic signaling pathway to stabilize Mcl-1. Mol Cell Biol. 2007;27:4328–4339. doi: 10.1128/MCB.00153-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Coloff JL, Ferguson EC, Jacobs SR, Cui K, Rathmell JC. Glucose metabolism attenuates p53 and Puma-dependent cell death upon growth factor deprivation. J Biol Chem. 2008;283:36344–36353. doi: 10.1074/jbc.M803580200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouillet P, O'Reilly LA. CD95, BIM and T cell homeostasis. Nat Rev Immunol. 2009;9:514–519. doi: 10.1038/nri2570. [DOI] [PubMed] [Google Scholar]
- Kerdiles YM, Beisner DR, Tinoco R, Dejean AS, Castrillon DH, DePinho RA, et al. Foxo1 links homing and survival of naive T cells by regulating L-selectin, CCR7 and interleukin 7 receptor. Nat Immunol. 2009;10:176–184. doi: 10.1038/ni.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capitini CM, Chisti AA, Mackall CL. Modulating T-cell homeostasis with IL-7: preclinical and clinical studies. J Intern Med. 2009;266:141–153. doi: 10.1111/j.1365-2796.2009.02085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini M, Calzascia T, Elford AR, Shahinian A, Lin AE, Dissanayake D, et al. Adjuvant IL-7 antagonizes multiple cellular and molecular inhibitory networks to enhance immunotherapies. Nat Med. 2009;15:528–536. doi: 10.1038/nm.1953. [DOI] [PubMed] [Google Scholar]
- Sportes C, Gress RE. Interleukin-7 immunotherapy. Adv Exp Med Biol. 2007;601:321–333. doi: 10.1007/978-0-387-72005-0_35. [DOI] [PubMed] [Google Scholar]
- Rosenberg SA, Sportes C, Ahmadzadeh M, Fry TJ, Ngo LT, Schwarz SL, et al. IL-7 administration to humans leads to expansion of CD8+ and CD4+ cells but a relative decrease of CD4+ T-regulatory cells. J Immunother. 2006;29:313–319. doi: 10.1097/01.cji.0000210386.55951.c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sportes C, Hakim FT, Memon SA, Zhang H, Chua KS, Brown MR, et al. Administration of rhIL-7 in humans increases in vivo TCR repertoire diversity by preferential expansion of naive T cell subsets. J Exp Med. 2008;205:1701–1714. doi: 10.1084/jem.20071681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzascia T, Pellegrini M, Lin A, Garza KM, Elford AR, Shahinian A, et al. CD4T cells, lymphopenia, and IL-7 in a multistep pathway to autoimmunity. Proc Natl Acad Sci USA. 2008;105:2999–3004. doi: 10.1073/pnas.0712135105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartgring SA, van Roon JA, Wenting-van Wijk M, Jacobs KM, Jahangier ZN, Willis CR, et al. Elevated expression of interleukin-7 receptor in inflamed joints mediates interleukin-7-induced immune activation in rheumatoid arthritis. Arthritis Rheum. 2009;60:2595–2605. doi: 10.1002/art.24754. [DOI] [PubMed] [Google Scholar]
- Colombetti S, Levy F, Chapatte L. IL-7 adjuvant treatment enhances long-term tumor-antigen-specific CD8+ T-cell responses after immunization with recombinant lentivector. Blood. 2009;113:6629–6637. doi: 10.1182/blood-2008-05-155309. [DOI] [PubMed] [Google Scholar]
- Barata JT, Cardoso AA, Boussiotis VA. Interleukin-7 in T-cell acute lymphoblastic leukemia: an extrinsic factor supporting leukemogenesis. Leuk Lymphoma. 2005;46:483–495. doi: 10.1080/10428190400027852. [DOI] [PubMed] [Google Scholar]
- Perarnau B, Saron MF, Reina San Martin B, Bervas N, Ong H, Soloski MJ, et al. Single H2Kb, H2Db and double H2KbDb knockout mice: peripheral CD8+ T cell repertoire and anti-lymphocytic choriomeningitis virus cytolytic responses. Eur J Immunol. 1999;29:1243–1252. doi: 10.1002/(SICI)1521-4141(199904)29:04<1243::AID-IMMU1243>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- Schott E, Bertho N, Ge Q, Maurice MM, Ploegh HL. Class I negative CD8T cells reveal the confounding role of peptide-transfer onto CD8T cells stimulated with soluble H2-Kb molecules. Proc Natl Acad Sci USA. 2002;99:13735–13740. doi: 10.1073/pnas.212515399. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.