Abstract
We measured selenium, zinc, copper and manganese concentrations in the human milk of Korean mothers who gave birth to preterm infants, and compared these measurements with the recommended daily intakes. The samples of human milk were collected postpartum at week-1, -2, -4, -6, -8, and -12, from 67 mothers who gave birth to preterm infants (< 34 weeks, or birth weight < 1.8 kg). All samples were analyzed using atomic absorption spectrophotometry. The concentrations of selenium were 11.8 ± 0.5, 11.4 ± 0.8, 12.7 ± 0.9, 11.4 ± 0.8, 10.8 ± 0.9, and 10.5 ± 1.3 µg/L, zinc were 7.8 ± 0.5, 9.1 ± 0.8, 7.2 ± 0.9, 8.0 ± 0.8, 7.4 ± 0.9, and 6.6 ± 1.2 mg/L, copper were 506 ± 23.6, 489 ± 29.4, 384 ± 33.6, 356 ± 32.9, 303 ± 35.0, and 301 ± 48.0 µg/L and manganese were 133 ± 4.0, 127 ± 6.0, 125 ± 6.0, 123 ± 6.0, 127 ± 6.0, and 108 ± 9.0 µg/L at week-1, -2, -4, -6, -8, and -12, respectively. The concentrations of selenium and zinc meet the daily requirements but that of copper is low and of manganese exceeds daily requirements recommended by the American Academy of Pediatrics, Committee on Nutrition.
Keywords: Preterm; Milk, Human; Selenium; Zinc; Copper; Manganese
INTRODUCTION
Human milk is the most appropriate nutrition for newborn infants, and breast feeding provides many well-known benefits to infants and mothers (1-5). If the milk has insufficient nutrients, however, growth-rate reduction, caloric reduction, delay of bone organization, osteoporosis, and fractures can occur (6-10). Previous research has reported differences in human milk composition among different races (11), thus, different countries have developed different fortifiers for human milk.
The diet of Korean people has become more westernized in recent years, so the nutrients needed to fortify human milk may need to be adjusted. In the present study, we examined the levels of trace minerals in the human milk of Korean mothers who delivered premature infants and compared to the recommended daily requirements, as these infants are particularly vulnerable in the extrauterine environment, and thus would benefit the most from human milk produced by their own mothers.
MATERIALS AND METHODS
Subjects
Human milk was obtained from 67 mothers who delivered preterm infants with gestational ages less than 34 weeks, or with birth weights less than 1.8 kg. All mothers who were vegetarians, or who took multivitamins or medications to enhance human milk production, were excluded. All mothers in the study consumed from 2,000-2,500 calories per day during the study period.
Collection of human milk samples
Samples of human milk were collected using manual expression, or by using an electric pump, at the end of postpartum week 1, 2, 4, 6, 8, and 12. Each mother was instructed to express milk in the early morning prior to afternoon visit to NICU, either in the maternity ward or at home. The human milk was placed in a plain test tube shielded by aluminum foil, and stored at -70℃, prior to analysis.
Analysis of selenium, zinc, copper, and manganese
All minerals were measured from 20 µL samples of the human milk using an atomic absorption spectrophotometer (AAS) and a Zeeman effect graphite furnace (Model 4110ZL, Perkin Elmer, Boston, MA, USA). The AAS consisted of spectrometers, a Zeeman background corrector, a Transversely Heated Graphite Atomizer (THGA) graphite tube, and hollow-cathode lamps.
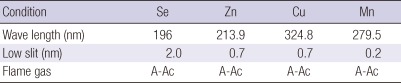
Samples were diluted 10-fold, diluted 100-fold, and diluted 1,000-fold for the measurement of the selenium (Se) and copper (Cu), the manganese (Mn), and zinc (Zn), respectively. All tools needed for preprocessing were immersed in 10% HNO3 for 24 hr, soaked in triple-distilled water for 24 hr, washed in triple-distilled water three times, and fully dried at room temperature. Table 1 describes the AAS analysis conditions (12).
Table 1.
Conditions used for atomic absorption spectrophotometry (12)
Se, selenium; Zn, zinc; Cu, copper; Mn, manganese; A-Ac, Air-Acetylene.
Statistical analysis
All results were analyzed using SAS 9.1. Measurements are reported as "means ± standard deviations" or "means ± standard errors". Random effects models were used to identify differences among lactation stages (at 1, 2, 4, 6, 8, and 12 weeks). A P value less than 0.05 was considered significant.
Ethics statement
The institutional review board of the Asan Medical Center reviewed and approved the study protocol (IRB 204-0111). All of participating mothers provided informed consent.
RESULTS
General characteristics of subjects
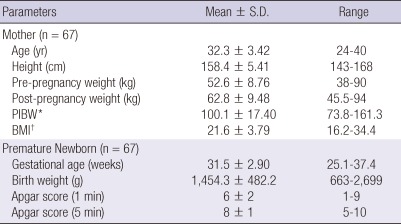
Table 2 shows the clinical characteristics of the 67 women and their infants.
Table 2.
General characteristics of subjects
*PIBW = (weight [kg]/IBW [kg]) × 100. Where [IBW(ideal body weight, kg)]: ≥ 161 cm: (Height [cm] -100) × 0.9. 150-160 cm: (Height [cm] -150)/2 + 50. < 150 cm: (Height [cm] -100) × 1.0. †BMI = (weight [kg]/length [m2]). PIBW, Percent of ideal body weight; BMI, Body mass index.
The ratio of percent ideal body weight (PIBW) of the pre-pregnancy weight to the standard weight of target subjects was 97% (range 90%-110%), and the mean body mass index (BMI) was 21.6 kg/m2.
Changes in the trace mineral content of the milk during the lactation period
A total of 44 samples were collected at postpartum week-1, while 32 samples were collected at week-2, 22 samples were collected at week-4, 26 samples were collected at week-6, 22 samples were collected at week-8, and 9 samples were collected at week-12.
The American Academy of Pediatrics, Committee on Nutrition has guidelines for the recommended intake of trace elements for preterm infants (CON/AAP, 2009) (13). These recommendations are based on the assumption that an infant consumes 100 kcal of human milk. Preterm human milk have a coloric density of 67 kcal/100 mL. Thus, for each trace element, we plotted the changes in the absolute concentration in the preterm human milk, as well as the changes as a function of caloric intake.
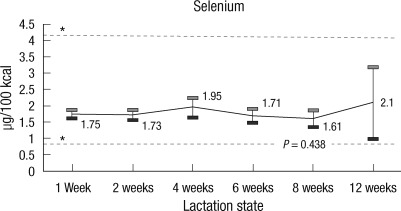
Selenium
The mean concentration of selenium was 11.8 ± 0.5 µg/L at week-1,11.4 ± 0.8 µg/L at week-2, 12.7 ± 0.9 µg/L at week-4, 11.4 ± 0.8 µg/L at week-6, 10.8 ± 0.9 µg/L at week-8, and 10.5 ± 1.3 µg/L at week-12. These differences were not statistically significant (P > 0.05). The mean concentrations of selenium during the first 12 weeks of lactation satisfied the CON/AAP recommendation of 0.9-4.1 µg/100 kcal (Fig. 1).
Fig. 1.
Amount of selenium in human preterm milk at different stages of lactation. *Recommendation by American Academy of Pediatrics, Committee on Nutrition (CON/AAP, 2009): 0.9-4.1 µg/100 kcal.
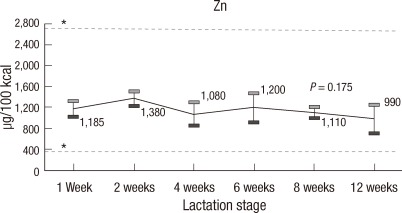
Zinc
The mean concentration of zinc was 7.8 ± 0.5 mg/L at week-1, 9.1 ± 0.8 mg/L at week-2, 7.2 ± 0.9 mg/L at week-4, 8.0 ± 0.8 mg/L at week-6, 7.4 ± 0.9 mg/L at week-8, and 6.6 ± 1.2 mg/L at week-12. The concentration of zinc declined, especially after the second week of lactation, but this change was not statistically significant (Fig. 2, P > 0.05). Again, the mean concentrations of zinc during the first 12 weeks of lactation satisfied the CON/AAP recommendation of 340-2,700 µg/100 kcal (Fig. 2).
Fig. 2.
Amount of zinc in human preterm milk at different stages of lactation. *Recommendation by American Academy of Pediatrics, Committee on Nutrition (CON/AAP, 2009): 340-2,700 µg/100 kcal.
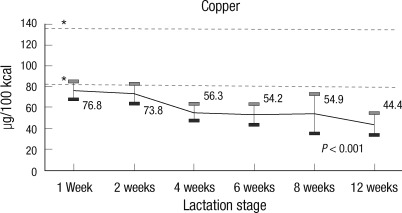
Copper
The mean concentration of copper was 506 ± 23.6 µg/L at week-1, 489 ± 29.4 µg/L at week-2, 384 ± 33.6 µg/L at week-4, 356 ± 32.9 µg/L at week-6, 303 ± 35.0 µg/L at week-8, and 301 ± 48.0 µg/L at week-12. The random effects Model test indicated a significant decline in the mean concentration of copper during the lactation period (Fig. 3, P < 0.05). The mean concentrations of copper were, at all times, below the CON/AAP recommendation of 80-1,366 µg/100 kcal (Fig. 3).
Fig. 3.
Amount of copper in human preterm milk at different stages of lactation. *Recommendation by American Academy of Pediatrics, Committee on Nutrition (CON/AAP, 2009): 80-136 µg/100 kcal.
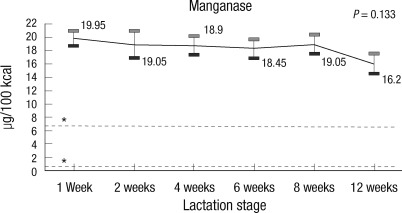
Manganese
The mean concentration of manganese was 133 ± 4.0 µg/L at week-1, 127 ± 6.0 µg/L at week-2, 125 ± 6.0 µg/L at week-4, 123 ± 6.0 µg/L at week-6, 127 ± 6.0 µg/L at week-8, and 108 ± 9.0 µg/L at week-12. The mean concentration decreased slightly from week-8 to week-12, but it was not statistically significant (Fig. 4, P > 0.05).
Fig. 4.
Amount of manganese in preterm human milk at different stages of lactation. *Recommendation by American Academy of Pediatrics, Committee on Nutrition (CON/AAP, 2009): 0.5-6.8 µg/100 kcal.
The mean concentrations of manganese were, at all times, higher than the CON/AAP recommendations of 0.5-6.8 µg/100 kcal (Fig. 4).
DISCUSSION
Trace elements are an essential part of the human diet. Deficiencies in certain trace elements in preterm infants may increase the risk of abnormal development (14, 15).
Selenium is considered essential trace elements for infants (16) and is best known for its role as an antioxidant (16, 17). Selenium accumulates during the third trimester of pregnancy, thus, premature infants have lower tissue and plasma concentrations of selenium than do full-term infants (16). Preterm infants have increased risks of bronchopulmonary dysplasia, retinopathy of prematurity, sepsis, and necrotizing colitis, conditions in which oxygen free radicals appear to play a role (18). These infants would benefit most by consuming human milk containing antioxidants (18). In our study, the amount of selenium in the human milk satisfied the CON/AAP recommendations, but not the recommendations of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN), the latter recommends (4.5-9 µg/100 kcal) (19). These recommendations differ because of geographic differences in the amount of selenium stored in the infant body, the dietary habits of different populations, and geological differences in the soils of different regions (20).
Zinc is a co-factor for numerous enzymes, and it is required for normal fetal growth and development. Like selenium, it accumulates during the third trimester of pregnancy (21). Our results are in accordance with those of Atkinson et al. (22) and Yamawaki et al. (23), in that, in our study, the amount of zinc in the human milk decreased in relation to the lactation time. However, as with the results reported by Yamawaki et al., this change was not statistically significant. Moreover, in our study, the concentration of zinc, at all lactation stages, satisfied the recommendations of CON/AAP and ESPGHAN.
Copper is also a co-factor for many enzymes. Copper is mainly stored in the liver, and it accumulates dramatically during the third trimester. Thus, preterm infants, tend to have lower copper stores than full-term infants (24). In our study, the concentration of copper was maximal at week-1 and then gradually declined over time, just as also reported by Mendelson et al. (25). The reason for these changes is unknown. These observations may suggest that newborn infants require larger amounts of these minerals due to the lower volume of milk intake in their early life (26). In our study, the mean concentration of copper in human milk was, at all times, lower than the intake recommended by CON/AAP and ESPGHAN (Fig. 3). However, the symptoms and signs of preterm infants with copper deficiency including hypochromic anemia, neutropenia, osteoporosis, and delayed bone age (27) were not investigated in this study. The reason for the observation of low copper in the preterm human milk produced by Korean mothers is uncertain, but it could be due to geographical effects and/or nutritional preferences. In particular, consumption of copper rich foods (beef, mollusks, crustaceans, mushrooms, chocolate, and nuts) may have been insufficient in the study populations of mothers with preterm infants (28). The simple addition of one pack of commercially available Korean human milk fortifier to 60-120 mL of human milk would have increased the total copper intake to 34-69 µg/100 kcal.
The clinical significance of manganese deficiency in preterm and low birth weight (LBW) infants is unknown, thus, the correct amount of manganese to be added to infant formula has not been established. However, excessive manganese can lead to central nervous system toxicity, and Friel et al. have proposed that 40 µg/day of manganese is sufficient for preterm or LBW infants who require total parenteral nutrition (29). In our study, the concentrations of manganese were higher than those recommended by CON/AAP (Fig. 4) and, lower than those recommended by Friel et al., but within the range recommended by ESPGHAN (6.3-25 µg/100 kcal).
According to the study in which concentration of trace minerals were compared in between the colostrums of Korean mothers who delivered preterm infants and term infants, the concentration of zinc, copper and manganese were reportedly below in colostrums of preterm infant than term infant. When the reported concentrations were compared with our data obtained for preterm colostrums, the concentrations of copper and manganese were less but zinc concentration was similar (30). We suspect that these results may differ because of changing in diet habits and nutritional status of Korean mothers over time.
The limitation of this study is that there were progressively fewer samples as the lactation period progressed. This was unavoidable, and was mainly due to the inadequate production of human milk by some mothers. Also, we did not measure the serum levels of the trace minerals in the infants, therefore, we cannot definitively conclude that the infants had adequate or inadequate levels of dietary trace minerals. Furthermore, the levels of trace mineral were not compared with human milk produced from mothers of full term infants. We suggest that future large scale studies be conducted to investigate the levels of micronutrients in preterm human milk and full term human milk, so as to provide accurate supplementation and to improve outcomes.
In conclusion, in the human milk of Korean mothers who deliver preterm infants, the zinc and selenium levels satisfy the recommended concentrations, but that the level of copper is below the recommended concentration. The manganese in the preterm human milk exceeds the recommendation of CON/AAP, but is within the recommendation of ESPGHAN.
Footnotes
This study was supported by a grant (2004-2005) from the Asan Institute for Life Sciences, Seoul, Korea.
References
- 1.Narayanan I, Prakash K, Gujral VV. The value of human milk in the prevention of infection in the high-risk low-birth-weight infant. J Pediatr. 1981;99:496–498. doi: 10.1016/s0022-3476(81)80360-5. [DOI] [PubMed] [Google Scholar]
- 2.Meinzen-Derr J, Poindexter B, Wrage L, Morrow AL, Stoll B, Donovan EF. Role of human milk in extremely low birth weight infants' risk of necrotizing enterocolitis or death. J Perinatol. 2009;29:57–62. doi: 10.1038/jp.2008.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Connor DL, Jacobs J, Hall R, Adamkin D, Auestad N, Castillo M, Connor WE, Connor SL, Fitzgerald K, Groh-Wargo S, et al. Growth and development of premature infants fed predominantly human milk, predominantly premature infant formula, or combination of human milk and premature formula. J Pediatr Gastroenterol Nutr. 2003;37:437–446. doi: 10.1097/00005176-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Ewer AK, Durbin GM, Morgan ME, Booth IW. Gastric emptying in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1994;71:F24–F27. doi: 10.1136/fn.71.1.f24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lucas A, Morley R, Cole TJ, Lister G, Leeson-Payne C. Breast milk and subsequent intelligence quotient in children born preterm. Lancet. 1992;339:261–264. doi: 10.1016/0140-6736(92)91329-7. [DOI] [PubMed] [Google Scholar]
- 6.Atkinson SA, Bryan MH, Anderson GH. Human milk feeding in premature infants: protein, fat and carbohydrate balances in the first 2 weeks of life. J Pediatr. 1981;99:617–624. doi: 10.1016/s0022-3476(81)80275-2. [DOI] [PubMed] [Google Scholar]
- 7.Czank C, Simmer K, Hartmann PE. Design and characterization of a human milk product for the preterm infant. Breastfeed Med. 2010;5:59–66. doi: 10.1089/bfm.2009.0028. [DOI] [PubMed] [Google Scholar]
- 8.Loui A, Raab A, Wagner M, Weigel H, Grüter-Kieslich A, Brätter P, Obladen M. Nutrition of very low birth weight infants fed human milk with or without supplemental trace elements: a randomized controlled trial. J Pediatr Gastroenterol Nutr. 2004;39:346–353. doi: 10.1097/00005176-200410000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Pettifor JM, Rajah R, Venter A, Moodley GP, Opperman L, Cavaleros M, Ross FP. Bone mineralization and mineral homeostasis in very low-birth-weight infants fed either human milk or fortified human milk. J Pediatr Gastroenterol Nutr. 1989;8:217–224. doi: 10.1097/00005176-198902000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Atkinson SA, Bryan MH, Anderson GH. Human milk: difference in nitrogen concentration in milk from mothers of term and premature infants. J Pediatr. 1978;93:67–69. doi: 10.1016/s0022-3476(78)80602-7. [DOI] [PubMed] [Google Scholar]
- 11.Rueda R, Ramírez M, García-Salmerón JL, Maldonado J, Gil A. Gestational age and origin of human milk influence total lipid and fatty acid contents. Ann Nutr Metab. 1998;42:12–22. doi: 10.1159/000012713. [DOI] [PubMed] [Google Scholar]
- 12.Ericson SP, McHalsky ML, Rabinow BE, Kronholm KG, Arceo CS, Weltzer JA, Ayd SW. Sampling and analysis techniques for monitoring serum for trace elements. Clin Chem. 1986;32:1350–1356. [PubMed] [Google Scholar]
- 13.Pediatric nutrition handbook. 6th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009. [Google Scholar]
- 14.Shaw JC. Trace elements in the fetus and young infant I Zinc. Am J Dis Child. 1979;133:1260–1268. doi: 10.1001/archpedi.1979.02130120052011. [DOI] [PubMed] [Google Scholar]
- 15.Shaw JC. Trace elements in the fetus and young infant II Copper, manganese, selenium and chromium. Am J Dis Child. 1980;134:74–81. doi: 10.1001/archpedi.1980.02130130056017. [DOI] [PubMed] [Google Scholar]
- 16.Litov RE, Combs GF., Jr Selenium in pediatric nutrition. Pediatrics. 1991;87:339–351. [PubMed] [Google Scholar]
- 17.Dall'Agnola A, Beghini L. Post-discharge supplementation of vitamins and minerals for preterm neonates. Early Hum Dev. 2009;85:S27–S29. doi: 10.1016/j.earlhumdev.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Shah MD, Shah SR. Nutrient deficiencies in the premature infant. Pediatr Clin North Am. 2009;56:1069–1083. doi: 10.1016/j.pcl.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, Domellöf M, Embleton ND, Fusch C, Genzel-Boroviczeny O, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91. doi: 10.1097/MPG.0b013e3181adaee0. [DOI] [PubMed] [Google Scholar]
- 20.Tamari Y, Chayama K, Tsuji H. Longitudinal study on selenium content in human milk particularly during early lactation compared to that in infant formulas and cow's milk in Japan. J Trace Elem Med Biol. 1995;9:34–39. doi: 10.1016/S0946-672X(11)80006-4. [DOI] [PubMed] [Google Scholar]
- 21.Islam MN, Chowdhury AK, Siddika M, Hossain MA, Hossain MK. Effect of zinc on growth of preterm babies. Mymensingh Med J. 2009;18:125–130. [PubMed] [Google Scholar]
- 22.Atkinson SA, Whelan D, Whyte RK, Lönnerdal B. Abnormal zinc content in human milk. Risk for development of nutritional zinc deficiency in infants. Am J Dis Child. 1989;143:608–611. doi: 10.1001/archpedi.1989.02150170110034. [DOI] [PubMed] [Google Scholar]
- 23.Yamawaki N, Yamada M, Kan-no T, Kojima T, Kaneko T, Yonekubo A. Macronutrient, mineral and trace element composition of breast milk from Japanese women. J Trace Elem Med Biol. 2005;19:171–181. doi: 10.1016/j.jtemb.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 24.Lönnerdal B. Copper nutrition during infancy and childhood. Am J Clin Nutr. 1998;67:1046S–1053S. doi: 10.1093/ajcn/67.5.1046S. [DOI] [PubMed] [Google Scholar]
- 25.Mendelson R, Anderson GH, Bryan MH. Zinc, copper and iron content of milk from mothers of pretem and full-term infants. Early Hum Dev. 1982;6:145–151. doi: 10.1016/0378-3782(82)90101-3. [DOI] [PubMed] [Google Scholar]
- 26.Ohtake M, Tamura T. Changes in zinc and copper concentrations in breast milk and blood of Japanese women during lactation. J Nutr Sci Vitaminol (Tokyo) 1993;39:189–200. doi: 10.3177/jnsv.39.189. [DOI] [PubMed] [Google Scholar]
- 27.Cordano A. Clinical manifestations of nutritional copper deficiency in infants and children. Am J Clin Nutr. 1998;67:1012S–1016S. doi: 10.1093/ajcn/67.5.1012S. [DOI] [PubMed] [Google Scholar]
- 28.Casey CE, Neville MC, Hambidge KM. Studies in human lactation: secretion of zinc, copper and manganese in human milk. Am J Clin Nutr. 1989;49:773–785. doi: 10.1093/ajcn/49.5.773. [DOI] [PubMed] [Google Scholar]
- 29.Friel JK, Penney S, Reid DW, Andrews WL. Zinc, copper, manganese, and iron balance of parenterally fed very low birth weight preterm infants receiving a trace element supplement. JPEN J Parenter Enteral Nutr. 1988;12:382–386. doi: 10.1177/0148607188012004382. [DOI] [PubMed] [Google Scholar]
- 30.Lee YW, Moon SJ, Lee MJ, Moon HN, Hong SJ. A comparative study on the composition of preterm and full term human milk in colostrums. Korean J Nutr. 1995;28:127–136. [Google Scholar]