Abstract
Rabson-Mendenhall syndrome (RMS) is a rare syndrome manifested by extreme insulin resistance with hyperinsulinemia, acanthosis nigricans, tooth dysplasia and growth retardation. Our patient was first noted at the age of 8 months due to pigmentations on skin-folded areas. Initial laboratory tests showed normal fasting glucose (69 mg/dL). Fasting insulin level was severely elevated, up to 554.6 µIU/mL, and c-peptide level was increased, up to 13.81 ng/mL. However, hemoglobin A1c was within normal range (4.8%). He is now 11 yr old. His growth development followed the 5-10th percentile and oral hypoglycemic agents are being administered. The last laboratory results showed insulin 364.1 µIU/mL, C-peptide 4.30 ng/mL, and hemoglobin A1c 7.6%. The boy was a compound heterozygote for the c.90C > A and c.712G > A mutations of the insulin receptor gene, INSR, which are nonsense and missense mutations. In summary, we report the first Korean case of RMS, which was confirmed by two novel mutations of the INSR.
Keywords: Rabson-Mendenhall Syndrome; Insulin Resistance; Receptor, Insulin; INSR
INTRODUCTION
The human insulin receptor is a heterotetramer consisting of two extracellular α subunits and two transmembranous and intracellular β subunits. The α subunits mediate insulin binding and β subunits have tyrosine kinase activity (1). Insulin binds to the α subunit of the receptor and stimulates autophosphorylation and kinase activity of the β subunit (2). The human insulin receptor is coded by the gene INSR, and INSR mutations result in insulin resistance (3).
There are three types of insulin resistance syndromes. One, referred to as type A, includes insulin resistance, acanthosis nigricans, hirsutism, and polycystic ovarian disease in a patient who is usually not obese. The second syndrome is leprechaunism, which presents with severe hyperglycemia due to insulin resistance, hyperinsulinemia, acanthosis nigricans, hirsutism, thick skin with lack of subcutaneous fat, distended abdomen, enlarged genitalia in the male, dysmorphic features (elfin-like face, lowset ears, promitent eyes, thick lips), and growth retardation (4, 5). Children afflicted with leprechaunism die within the first 2 yr of life (6). The last one is Rabson-Mendenhall Syndrome (RMS), which is manifested with severe insulin resistance with hyperinsulinemia, acanthosis nigricans, tooth and nail dysplasia, growth retardation, and pineal hyperplasia. Although patients with RMS usually survive beyond 1 year of age, they develop constant hyperglycemia followed by diabetic ketoacidosis and death.
Here, we describe clinical findings in the first Korean RMS patient and report two novel mutations of INSR, which were confirmed by clinical, biochemical, and molecular findings.
CASE DESCRIPTION
The male patient was admitted to the hospital at the age of 8 months due to pigmentations on skin-folded areas, gingival hyperplasia, and hirsutism, on 28 December 1999. He was born as the first child to healthy non-consanguineous Korean parents at 38 weeks of gestation; birth weight and length were 2,450 g (10-25th percentile) and 47 cm (25-50th percentile). Neonatal screening tests including 17-hydroxyprogesterone were normal. Length and body weight were within the 5-10th percentile at 8 months old. His face was coarse, with epicanthal folds, and low set ears. The hair was curled and bristly. Initial laboratory tests showed normal fasting glucose, 69 mg/dL (reference range; RR, 60-100 mg/dL). Fasting insulin level was severely elevated, up to 554.6 µIU/mL (RR, 7-24 µIU/mL), and c-peptide level was increased, up to 13.81 ng/mL (RR, 0.4-2.2 ng/mL). However, the percent of glycosylated hemoglobin (HbA1c) was within normal range; 4.8% (RR, 4.5%-6.5%). AST and ALT were slightly elevated, to 51 U/L (RR, 15-55 U/L) and 49 U/L (RR, 5-45 U/L). We performed an intravenous glucose tolerance test to rule out insulin resistance syndromes. Fasting glucose and insulin level were normal; 57 mg/dL, 3.7 µIU/mL. After IV administration of glucose (0.3 g/kg), rapid increase of glucose level up to 204 mg/dL was observed after 2 min, and insulin level was extremely elevated up to 2,508 µIU/mL. Maximal elevation of insulin level was 3,300 µIU/mL after 4 min, which suggested extreme hyperinsulinemia to glucose load. However, hyperglycemia was not demonstrated usually. Therefore, we did not administer any type of hypoglycemic agents. Results of skin biopsy of the pigmented neck revealed acanthosis nigricans.
At 13 months old, his fasting glucose was checked, up to 128 mg/dL with glucosuria (+++); therefore, a low-sugar diet and oral hypoglycemic agent (metformin 250 mg/day) therapy were started. At the age of 18 months, he started growth hormone therapy due to poor height gain and low IGF-1 level of 14.3 ng/mL (RR, 31-160 ng/mL). However, we stopped growth hormone therapy after 3 months, due to minimal effect and hyperglycemia. At the age of nine years old, he was admitted to our hospital due to poor glycemic control (HbA1c 11.0%), thereafter, additional oral hypoglycemic agents (metformin 500 mg bid, glimepiride 2 mg bid, and voglibose 0.2 mg tid) have been administered until now, with HbA1c less than 8%.
He is now 11 yr old. Acanthosis nigricans lesions have shown improvement, and dark skin color has brightened. Protrusion of lips, teeth crowding, macrodontia, and abnormal dentition (Fig. 1) are observed. Severe growth retardation has not been demonstrated; weight of 5-10th percentile and height of 10-25th percentile. Body mass index is 15.7 kg/m2. Developmental state and neurologic examination are normal.
Fig. 1.
Dentition photographs were taken at the age of 10 yr old. Note the abnormal dentition, which includes proclined upper and lower incisors (A), and crowding on lower teeth, macrodontia (B).
Recent laboratory tests performed at the age of 10 yr still showed increased insulin resistance and subsequent hyperglycemia; insulin 364.1 µIU/mL (RR, 7-24 µIU/mL), C-peptide, 4.30 ng/mL (RR, 0.4-2.2 ng/mL), Hb A1c 7.6%. Hyperandrogenism was not demonstrated; testosterone, 0.08 ng/mL (RR, 0.03-0.1 ng/mL). His dental age was advanced, compared with chronologic age. Bone ages fit with his chronological age. He has not experienced diabetic ketotic acidosis, and has had no complications until now.
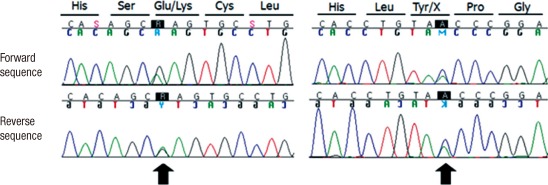
For identification of the underlying genetic defect, we performed molecular genetic testing for the INSR gene. After informed consent had been obtained, blood samples were collected from the patient. Genomic DNA was isolated from peripheral blood leukocytes using the Wizard Genomic DNA Purification Kit (Promega, Madison, WI, USA). Primers designed by the authors were used for amplification of all coding exons and their flanking intronic sequences of the INSR gene by polymerase chain reaction using a thermal cycler (Model 9700; Applied Biosystems, Foster City, CA, USA). Direct sequencing was performed using the same primer sets and the BigDye Terminator Cycle Sequencing Ready Reaction kit (Applied Biosystems, Rotkreuz, Switzerland) on the ABI Prism 3130xl genetic analyzer (Applied Biosystems, Foster City, CA, USA). In result, two novel variations were identified (Fig. 2). One is a C to A transversion at nucleotide position 90 (c.90C > A) in exon 1, replacing tyrosine to a premature stop codon at codon 30 (p.Tyr30X). The other is a G to A transition at the nucleotide position 712 (c.712G > A) in exon 3, replacing glutamic acid with lysine at codon 238 (p.Glu238Lys).
Fig. 2.
Direct sequencing of the INSR gene in our patient. Compound heterozygous for two mutations were identified: c.90C>A (p.Tyr30X) in exon 1 and c.712G>A (p.Glu238Lys) in exon 3 (arrows).
DISCUSSION
Leprechaunism and RMS are both autosomal recessive diseases with abnormal alleles for insulin receptors. Mutations in the INSR cause a spectrum of inherited insulin-resistance syndromes ranging from leprechaunism, in which afflicted children die in infancy, to type A insulin resistance, usually evident after puberty. RMS has an intermediate phenotype. Cells from most patients with leprechaunism show absent or severely impaired insulin binding to insulin receptor, whereas cells from patients with RMS retain some insulin binding capacity (7). Therefore, the severity of the phenotype seems to be determined by the degree of insulin resistance and that residual insulin binding capacity correlates with survival (8).
In this patient, several pieces of evidence, including hyperinsulinemia with insulin resistance, acanthosis nigricans, hirsutism, abnormal dental findings, and peculiar morphology suggested leuprechaunism or RMS. Our patient had showed relatively mild phenotype and lived longer than 2 yr, therefore he was diagnosed as RMS.
In most cases, nonsense mutations cause leprechaunism phenotype by reduction of insulin binding activity (8). Patients with leprechaunism had α subunit mutations or homozygosity in β subunit mutations, which tend to predict a more severe clinical course (9). Most patients with type A syndrome had heterozygous mutations in the β subunit, which affect kinase activity and result in a mild decrease in insulin binding capacity (8, 10). Reported mutations of RMS, located within the α subunit of the INSR gene, were homozygous mutations, including C284Y/C284Y (11), S323L/S323L (12), and heterozygous mutations including N15K/R1000X(β subunit) (13), C159F/R229C (7), and H209R/359S (14). Reported mutations of RMS, located within the β subunit of the INSR gene, were heterozygous mutations, including I1131T (10), R1131W (10), P970T (8), I1115T (10), I1116T (8), R1174W (8), and R1000X/N15K (α subunit) (13).
Previously, we cultured fibroblast cells from skin in this case and suggested the possible mechanism of insulin resistance at the molecular level; however, at that time, we failed to identify the mutation in the patient (6). Now, we have determined that this patient had one novel nonsense mutation (p.Y30X) and another novel missense mutation (p.E238K) within the α subunit of the INSR. Tyrosine 30 is in the extracellular L1 domain; however, the exact function of this region is unknown. Glutamic acid 238 is in the extracellular Furin-like Cystein-rich domain of α subunits. Some of these cysteines are thought to participate in maintenance of the structure of the insulin-binding site through establishment of disulfide bonds between α subunits (15). However, the cystein-rich domain does not appear to contain direct insulin/insulin receptor contact sites (16). Characterization of the naturally occurring point mutations P193L (17), H209R (18), and L233P (19) also suggests that this domain is important for insulin receptor processing and transport to the cell surface. In particular, close proximity to our p.E238K mutation, a missense mutation at amino acid position 233 in exon 3 (p.L233P), has previously been shown to completely block processing and transport of insulin receptor to the cell surface (19, 20), which would not alter qualitative insulin binding activities in vitro (7).
As described above, it is reported that only missense mutations were within α subunit of the INSR gene in RMS, and nonsense mutations in α subunits have only been found in leprechaunism. In conclusion, we report a case of two novel mutations in α subunit of the INSR; which is the first case of RMS where a nonsense mutation is located within the α subunit of the INSR.
ACKNOWLEDGMENTS
The study was supported by the Korea Healthcare Technology R&D Project; Grant sponsor: Ministry for Health, Welfare and Family Affairs, Republic of Korea; Grant number: A080588; Grant sponsor: Samsung Biomedical Research Institute; Grant numbers: C-A9-240-2 Grant sponsor: In-Sung Foundation for Medical Research.
References
- 1.Ullrich A, Bell JR, Chen EY, Herrera R, Petruzzelli LM, Dull TJ, Gray A, Coussens L, Liao YC, Tsubokawa M, et al. Human insulin receptor and its relationship to the tyrosine kinase family of oncogenes. Nature. 1985;313:756–761. doi: 10.1038/313756a0. [DOI] [PubMed] [Google Scholar]
- 2.Longo N, Wang Y, Smith SA, Langley SD, DiMeglio LA, Giannella-Neto D. Genotype-phenotype correlation in inherited severe insulin resistance. Hum Mol Genet. 2002;11:1465–1475. doi: 10.1093/hmg/11.12.1465. [DOI] [PubMed] [Google Scholar]
- 3.Elsas LJ, Endo F, Strumlauf E, Elders J, Priest JH. Leprechaunism: an inherited defect in a high-affinity insulin receptor. Am J Hum Genet. 1985;37:73–88. [PMC free article] [PubMed] [Google Scholar]
- 4.Longo N, Langley SD, Griffin LD, Elsas LJ. Two mutations in the insulin receptor gene of a patient with leprechaunism: application to prenatal diagnosis. J Clin Endocrinol Metab. 1995;80:1496–1501. doi: 10.1210/jcem.80.5.7538143. [DOI] [PubMed] [Google Scholar]
- 5.Longo N, Langley SD, Griffin LD, Elsas LJ., 2nd Reduced mRNA and a nonsense mutation in the insulin-receptor gene produce heritable severe insulin resistance. Am J Hum Genet. 1992;50:998–1007. [PMC free article] [PubMed] [Google Scholar]
- 6.Park HS, Jin DK, Shin SM, Jang MK, Longo N, Park JW, Bae DS, Bae YS. Impaired generation of reactive oxygen species in leprechaunism through downregulation of Nox4. Diabetes. 2005;54:3175–3181. doi: 10.2337/diabetes.54.11.3175. [DOI] [PubMed] [Google Scholar]
- 7.Thiel CT, Knebel B, Knerr I, Sticht H, Müller-Wieland D, Zenker M, Reis A, Dörr HG, Rauch A. Two novel mutations in the insulin binding subunit of the insulin receptor gene without insulin binding impairment in a patient with Rabson-Mendenhall syndrome. Mol Genet Metab. 2008;94:356–362. doi: 10.1016/j.ymgme.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Longo N, Wang Y, Smith SA, Langley SD, DiMeglio LA, Giannella-Neto D. Genotype-phenotype correlation in inherited severe insulin resistance. Hum Mol Genet. 2002;11:1465–1475. doi: 10.1093/hmg/11.12.1465. [DOI] [PubMed] [Google Scholar]
- 9.Musso C, Cochran E, Moran SA, Skarulis MC, Oral EA, Taylor S, Gorden P. Clinical course of genetic diseases of the insulin receptor (type A and Rabson-Mendenhall syndromes): a 30-year prospective. Medicine (Baltimore) 2004;83:209–222. doi: 10.1097/01.md.0000133625.73570.54. [DOI] [PubMed] [Google Scholar]
- 10.Longo N, Wang Y, Pasquali M. Progressive decline in insulin levels in Rabson-Mendenhall syndrome. J Clin Endocrinol Metab. 1999;84:2623–2629. doi: 10.1210/jcem.84.8.5902. [DOI] [PubMed] [Google Scholar]
- 11.Desbois-Mouthon C, Magré J, Duprey J, Caron M, Blivet-Van Eggelpoel MJ, Daubas C, Gourmelen M, Chevallier B, Rizkalla S, Robert JJ, et al. Major circadian variations of glucose homeostasis in a patient with Rabson-Mendenhall syndrome and primary insulin resistance due to a mutation (Cys284-->Tyr) in the insulin receptor alpha-subunit. Pediatr Res. 1997;42:72–77. doi: 10.1203/00006450-199707000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Krook A, Kumar S, Laing I, Boulton AJ, Wass JA, O'Rahilly S. Molecular scanning of the insulin receptor gene in syndromes of insulin resistance. Diabetes. 1994;43:357–368. doi: 10.2337/diab.43.3.357. [DOI] [PubMed] [Google Scholar]
- 13.Kadowaki T, Kadowaki H, Rechler MM, Serrano-Rios M, Roth J, Gorden P, Taylor SI. Five mutant alleles of the insulin receptor gene in patients with genetic forms of insulin resistance. J Clin Invest. 1990;86:254–264. doi: 10.1172/JCI114693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuthill A, Semple RK, Day R, Soos MA, Sweeney E, Seymour PJ, Didi M, O'Rahilly S. Functional characterization of a novel insulin receptor mutation contributing to Rabson-Mendenhall syndrome. Clin Endocrinol (Oxf) 2007;66:21–26. doi: 10.1111/j.1365-2265.2006.02678.x. [DOI] [PubMed] [Google Scholar]
- 15.Cheatham B, Kahn CR. Insulin action and the insulin signaling network. Endocr Rev. 1995;16:117–142. doi: 10.1210/edrv-16-2-117. [DOI] [PubMed] [Google Scholar]
- 16.Roach P, Zick Y, Formisano P, Accili D, Taylor SI, Gorden P. A novel human insulin receptor gene mutation uniquely inhibits insulin binding without impairing posttranslational processing. Diabetes. 1994;43:1096–1102. doi: 10.2337/diab.43.9.1096. [DOI] [PubMed] [Google Scholar]
- 17.Takata Y, Imamura T, Haruta T, Egawa K, Takada Y, Sawa T, Yang GH, Kobayashi M. Leu 193 mutation in the cysteine rich region of the insulin receptor inhibits the cleavage of the insulin receptor precursor but not insulin binding. Biochem Biophys Res Commun. 1994;203:763–767. doi: 10.1006/bbrc.1994.2248. [DOI] [PubMed] [Google Scholar]
- 18.Kadowaki T, Kadowaki H, Accili D, Yazaki Y, Taylor SI. Substitution of arginine for histidine at position 209 in the alpha-subunit of the human insulin receptor. A mutation that impairs receptor dimerization and transport of receptors to the cell surface. J Biol Chem. 1991;266:21224–21231. [PubMed] [Google Scholar]
- 19.Maassen JA, Van der Vorm ER, Van der Zon GC, Klinkhamer MP, Krans HM, Möller W. A leucine to proline mutation at position 233 in the insulin receptor inhibits cleavage of the proreceptor and transport to the cell surface. Biochemistry. 1991;30:10778–10783. doi: 10.1021/bi00108a024. [DOI] [PubMed] [Google Scholar]
- 20.Maassen JA, Tobias ES, Kayserilli H, Tukel T, Yuksel-Apak M, D'Haens E, Kleijer WJ, Féry F, van der Zon GC. Identification and functional assessment of novel and known insulin receptor mutations in five patients with syndromes of severe insulin resistance. J Clin Endocrinol Metab. 2003;88:4251–4257. doi: 10.1210/jc.2003-030034. [DOI] [PubMed] [Google Scholar]