Abstract
Many of those who survive a stroke develop a gait disability known as stiff-knee gait (SKG). Characterized by reduced knee flexion angle during swing, people with SKG walk with poor energy efficiency and asymmetry due to the compensatory mechanisms required to clear the foot. Previous modeling studies have shown that knee flexion activity directly before the foot leaves the ground, and this should result in improved knee flexion angle during swing. The goal of this research is to physically test this hypothesis using robotic intervention. We developed a device that is capable of assisting knee flexion torque before swing but feels imperceptible (transparent) for the rest of the gait cycle. This device uses sheathed Bowden cable to control the deflection of a compliant torsional spring in a configuration known as a Series Elastic Remote Knee Actuator (SERKA). In this investigation, we describe the design and evaluation of SERKA, which includes a pilot experiment on stroke subjects. SERKA could supply a substantial torque (12 N· m) in less than 20 ms, with a maximum torque of 41 N·m. The device resisted knee flexion imperceptibly when desired, at less than 1 N·m rms torque during normal gait. With the remote location of the actuator, the user experiences a mass of only 1.2 kg on the knee. We found that the device was capable of increasing both peak knee flexion angle and velocity during gait in stroke subjects. Thus, the SERKA is a valid experimental device that selectively alters knee kinetics and kinematics in gait after stroke.
Index Terms: Compliant actuators, gait, orthotics, Series Elastic Remote Knee Actuator (SERKA), stiff-knee gait (SKG), stroke
I. Introduction
Of the 700 000 people that suffer a stroke in the United States each year [1], many will develop stiff-knee gait (SKG). SKG is broadly defined as reduced knee flexion angle of the affected limb during the swing phase when the foot leaves the ground [2]. Since one foot has difficulty clearing the ground, SKG requires a number of asymmetric gait compensations in order to clear the foot and prevent tripping. Some of these compensations include pelvic tilt and lag, hip circumduction (raising the paretic hip during swing), and premature heel rise of the unaffected foot [3]. This asymmetric gait could lead to biomechanical issues, such as back pain, and affects aesthetics [4], which may play a role in the person’s self-image. Both the increased moment of inertia of the paretic limb [5] and slower cadence [6] reduce energy efficiency and, thus, heightens fatigue.
Despite information indicating that abnormal activity of the knee extensors causes SKG [7], [8], surgical interventions on cerebral palsy patients have produced inconsistent improvements. Treanor used femoral neurectomies and/or release of the rectus femoris (RF) to decrease the effect of this hip flexor/knee extensor muscle but found that only a third of the patients bene-fited from such surgery [9]. Waters et al. performed tenotomies (releasing of the tendon) of the RF and/or vastus intermedius on 32 subjects with SKG, which was found to help only 25% of the patients [10].More recently, Sung and Bang used Lidocaine to block signals from the motor branch innervating the RF [11]. This procedure allowed greater knee flexion angle, but it also caused improper knee flexion angle during stance.
Studies using computer modeling have given additional insight into possible kinematic, kinetic, and muscular mechanisms of SKG. Piazza and Delp found that knee flexion velocity at toe-off contributed the most to peak knee flexion angle in gait [8]. A clinical study by Goldberg et al. examined the limbs of cerebral palsy patients, adding that excessive knee extension torque during stance was the major cause of SKG [12]. Kerrigan et al. examining stroke subjects concluded that hip flexion torque is primarily responsible for peak knee flexion angle in swing [13]. Riley and Kerrigan found that knee angle was more sensitive to torque at the knee than the hip during swing [14]. A later study found that there are different impairments that can cause SKG in each individual [15].Models are limited, however, since problems associated with stroke such as spasticity, contracture, and muscle discoordination have yet to be accurately modeled.
Some of these modeling studies have identified that preswing activity of the knee is a primary contributor to SKG [8], [12], [16], and therefore, we should be able to reduce the negative effects of SKG by selectively altering knee kinetics before the foot leaves the ground. We hypothesize that increasing knee flexion torque in preswing will create greater peak knee flexion during swing, greater toe clearance and, thus, reduce the necessity for energy-consuming gait compensations. While a study on paraplegics by Greene and Granat shows that assisting both ankle and knee motion is necessary to reduce compensations [17], stroke patients have some residual strength in their affected limb, which necessitates the individual joint approach. By controlling knee flexion, we can directly evaluate the importance of preswing activity of the knee in SKG.
Researchers have developed many interesting ways to assist lower limb motion. A number of research groups have developed lower body exoskeletons using motors [18], [19], hydraulics [20], and pneumatics [21], [22]. Hollander et al. created a novel, lightweight system for ankle torque assistance that stores energy in one phase of gait, and then, releases energy when needed [23]. Body-powered orthoses are practical solutions to gait assistance [24] and have been combined with functional electrical stimulation as well [25], yet these examples are meant as solutions to the problem of impaired gait, whereas our goal is to gain a greater understanding of the role of the knee joint in SKG.
We need a device capable of applying torque to the knee during the brief period before toe-off but remains imperceptible during other stages of gait. The device must be as light as possible to reduce both the load on neighboring joints and metabolic cost, but flexible enough to accommodate knee flexion in a variety of user locations on a treadmill. These specific requirements necessitate a flexible, low-impedance, low-weight actuator.
McKibben actuators have many benefits including low weight, high force/weight ratio, and flexibility. They have been attached to an ankle foot orthosis and used effectively to provide plantar flexion assistance during gait [26], [27]. Unfortunately, these actuators have poor bandwidth compared with human capability and difficulty in providing large forces over large ranges of motion [22], [28].
Motors, by contrast, are fast and accurate, yet have a poor force/weight ratio. These issues are dealt with differently in two motorized knee orthoses: the RoboKnee [29] and a “knee perturbator” [30]. The RoboKnee uses a spring in series with a ball screw and motor, which is known as a series elastic actuator [31]. This combination creates a low-weight and low-impedance source of actuation fit for human interaction. The design of the positional knee perturbator places the motor off the leg in a tethered configuration by using sheathed (referred to as Bowden) cable to actuate the joint. Remotely locating its actuator reduces its weight on the leg. The most appropriate design for our application is a modified combination of the two aforementioned knee actuators.
Both the RoboKnee and knee perturbator have nonbackdrivable transmissions but deal with them differently. While the Bowden cable transmission of the position-controlled knee pertubator has numerous advantages, its friction, which is caused by cable moving in its sheath, reduces backdrivability and makes control difficult. To offset this friction, a novel clutch system is activated during walking. The RoboKnee also has a nonback-drivable transmission but avoids control issues by attaching a series elastic component between gearmotor output and the orthosis. In short, a Bowden cable transmission allows for remote actuator placement, and its alignment with a spring in series provides the backdrivability necessary to account for errors due to cable friction [32]. This solution is optimal for a treadmill walking situation requiring torque perturbations. We will refer to this setup as a Series Elastic Remote Knee Actuator (SERKA).
This is not the first introduction of Bowden-cable-driven series elastic actuators for human interaction. For instance, researchers at the University of Twente, Twente, The Netherlands, developed lower extremity powered exoskeleton (LOPES) using a novel configuration of two stiff linear springs around a joint [33]. Another exoskeleton at Sogang University uses linear springs in line with cables and around pulleys to actuate an assistive device for the elderly [34]. However, as we show in this paper, the configuration of SERKA is most suitable for its application.
The purpose of this paper is to introduce and validate an active knee orthosis constructed to selectively assist knee flexion in subjects with SKG. We demonstrate how SERKA’s simple design allows it to exert torque only when needed and has the lowest weight of any active knee brace to our knowledge, with a mass of 1.2 kg. It is capable of exerting up to 41 N·m torque in less than voluntary movement time and has a torque bandwidth beyond human capability. Finally, we show in a pilot experiment that it is capable of increasing peak knee flexion angle and velocity in stroke subjects and discuss its implications for a subsequent experiment. The intervention will help identify impairments and lead toward better treatment, rehabilitation, and assistive technology.
II. Design
Design criteria were centered on a lightweight device capable of assisting knee flexion torque before toe-off, and feeling imperceptible during the remainder of the gait cycle (i.e., transparent). For performance in reflex studies, the device needed to produce substantial torque in less than human reflex latency of 30 ms [35]. In addition, based on unpublished data [36], 40 N·m of flexion torque is needed to bend a paretic knee. The resulting orthosis is shown in Fig. 1.
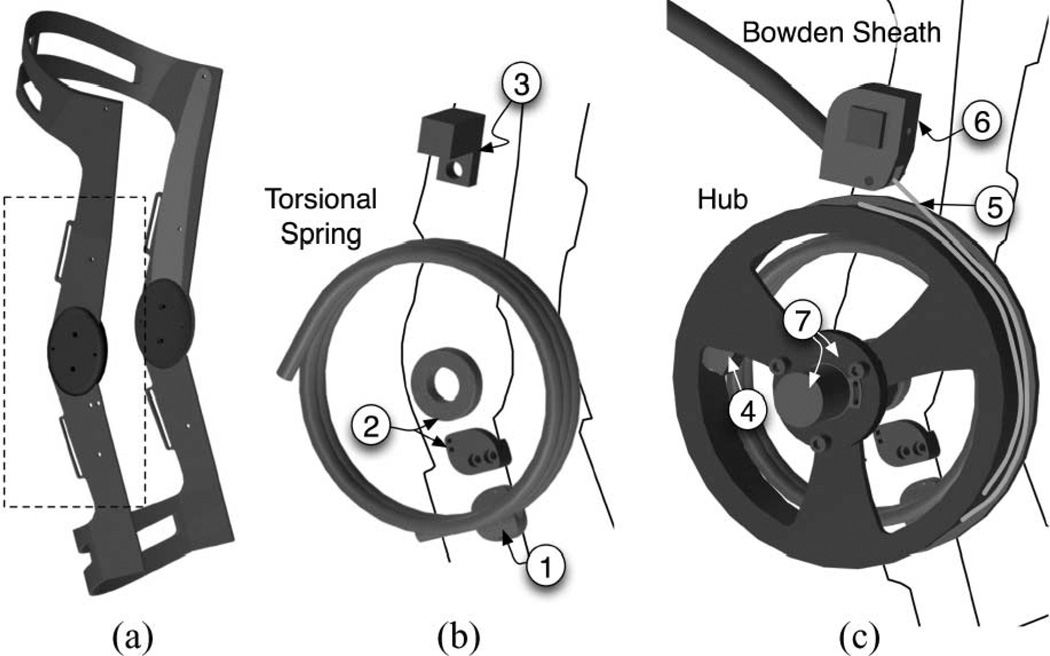
Fig. 1.
(a) Structure of the commercial knee brace without padding or straps. The dashed box indicates the close-up view shown in (b) and (c). (b) Close-up of the torsional spring, along with (1) the spring-brace anchor attached to the shank. (2) A Hall-effect goniometer, composed of an annular magnet fixed and centered on the distal lateral hinge and a hall sensor attached to shank, measures brace angle. Part (3) is the Bowden sheath-brace anchor, which is attached at the thigh. The rest of the device is shown in (c), including the hub with a built-in slot (4) for attachment to the spring. The position of the hub is controlled by excursion of Spectra cable (5) wrapped and anchored to it. The cable passes through Bowden sheath attached to the sheath-brace anchor using a custom-made coupler (6). The hub rotates about a steel shaft (not shown) centered at the distal lateral hinge. The angular displacement of the hub relative to the shaft is measured by an encoder (7) coupled with the hub using a spring-suspension platform. This platform keeps the encoder fixed to the shaft while the spring deformation creates an increase in height (direction along rotation axis) of the hub. Torque exerted by the device is determined by using the difference between the angle measured by the encoder and that of the Hall-effect goniometer.
Design of the SERKA started with the knee brace. We chose to modify an off-the-shelf knee orthosis (Axiom Sport Hi-Impact, Bledsoe Brace Systems, Grand Prarie, TX) that can withstand the 40 N·m torque applied by the actuator. The orthosis weighs approximately 0.5 kg. The superstructure of the orthosis is made from 7075-T6 Aluminum (σYTS = 503 MPa), with a spring steel reinforcement (σYTS = 1590 MPa). Based on the design in Fig. 1, we calculated that the brace would be able to withstand stress with a safety factor of at least 2 in every failure mode.
The design of the orthosis incorporates an anterior shell that prevents the brace from rotating around the leg by gripping on the anteromedial tibia [37]. The superstructure and closed cell foam padding of the orthosis also adequately distribute the forces being applied to leg by the actuator. Zhang and Lee found that the threshold for pressure sensation at the anteromedial tibia is 0.58MPa [38]. Approximately, a 3.22 cm2 surface area would be required to adequately distribute the maximum 40 N·m being applied to the leg; the design of the Axiom Sport Hi-Impact has sufficient surface area to achieve this goal.
The orthosis employs a polycentric hinge, as well as a pivoting strap, to reduce migration [39]. The polycentric hinge is designed to match the instantaneous center of rotation of the knee [40]. A polycentric hinge also reduces the stresses on the internal structures of the knee joint [41]. The antimigration strap fits tightly on the calf muscle and prevents brace slipping. This strap lays over the triceps surae and purchases over the convex shape of this muscle group. The other five straps provide additional friction to reduce distal translation of the orthosis [39]. Modifications to the orthosis have been made to attach the actuator to the distal (lower) lateral hinge.
The position of the knee brace was measured using an annular magnet (Engineered Concepts, Birmingham, AL) centered on the distal lateral hinge and a Hall-effect sensor (Allegro A3515, Worcester, MA) fixed to the shank. Since the brace has geared hinges, measuring the angle at the distal lateral hinge provides enough information for the angle of the entire orthosis. The brace position can be measured to a resolution of 0.2°/bit with an accuracy of 0.41°.
The elastic element we used was a 24N·m/rad torsional spring (Oshkosh Coil Spring, Inc., Oshkosh, WI) made from 6.3 mm (0.25 in) diameter spring steel. The spring was designed to be compliant enough to account for position errors due to Bowden cable friction, and strong enough to bend the knee of a stroke subject during gait (40 N·m) [36]. Spring stiffness was measured using a lever arm and a load cell to measure force and a goniometer to measure angular displacement. The stiffness is far less than the high compliance version of an LOPES joint (63.6 N·m/rad) [33].
One end of this spring is fixed to the shank portion of the knee brace while the other is fixed to an aluminum hub surrounding the 10 cm (4 in) diameter spring. Using a brass journal bearing, the hub rotates around a stainless steel shaft attached through the distal lateral hinge of the orthosis. The position of the hub relative to the shaft is measured by a 5000 counts/revolution optical encoder (Gurley Precision Instruments, Troy, NY). Due to spring deformation, the hub must translate in the direction of the rotation axis during operation, but the encoder cannot translate on the shaft to follow the hub. To account for this problem, we mounted the encoder on a platform suspended by three compression springs and guided by shoulder bolts, thus allowing translation of the hub relative to the encoder, but not allowing relative rotation. In this configuration, the deflection of the torsional spring and, therefore, the torque, is proportional to the difference between the encoder angle and the brace angle.
Spectra cable (1.5 mm diameter, 3.3 kN test strength, Small Parts, Inc., Miramar, FL) wrapping around the hub four times before anchoring to it is used to create deflection in the spring. Spectra is lightweight and soft, has very low friction and is capable of wrapping around small radii [42], but it has also been known to creep [43]. The current version of the SERKA only operates in knee flexion, thus eliminating the need to pretension the cable until use and, thereby, avoiding issues with creep.
The loss of output force due to friction through the Bowden cable exponentially increases with both bending the sheath and friction coefficient. This loss can be quantified through the capstan equation
| (1) |
where To and Ti are the output and input tension, respectively, β is the total angle of bending in the sheath, and μ is the friction coefficient. Thus, keeping the sheath stiff will reduce bending and hence frictional losses. We use a Bowden sheath with a Teflon liner (2.5 mm ID) and steel coil reinforcement for greater stiffness (Motion Pro, Inc., San Carlos, CA). Combined with Spectra, the liner reduces friction considerably when compared with steel–steel contact. Carlson et al. found a coefficient of friction of 0.15 for steel–steel contact and 0.055 for Spectra–Teflon [42]. Through (1), this equates to an 11% reduction in losses due to friction.
The Bowden sheath is anchored to the thigh portion of the brace using a custom-made coupler. The sheath is supported by a sling on the treadmill bar. Together with the brace and unsupported section of Bowden cable, the SERKA has a mass of 1.2 kg.
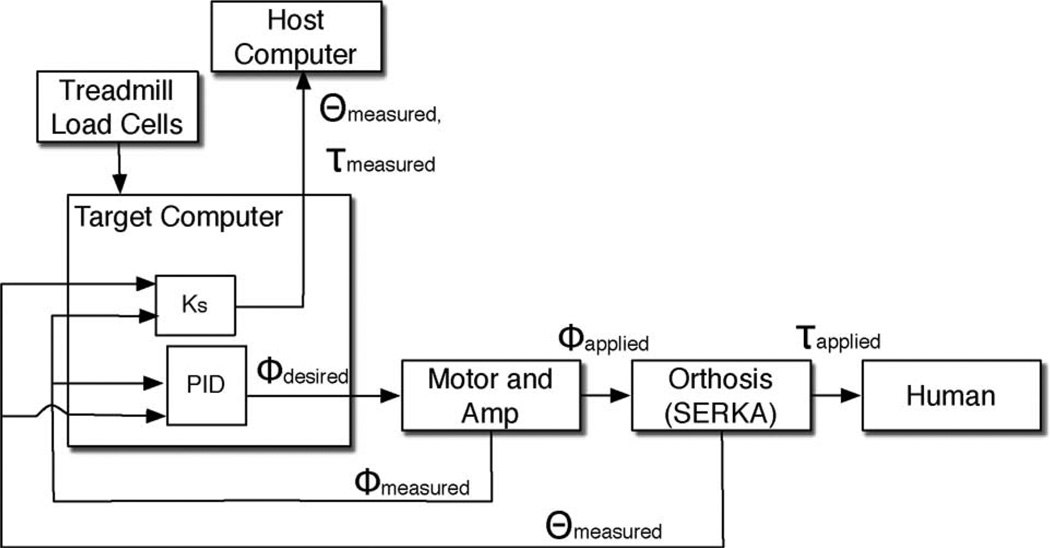
Located away from the user, a 1.4-kW dc servomotor (Moog G413-815, Inc., Blacksburg, VA), with a 5:1 gear reduction (Apex Dynamics, Taiwan) mounted to a fixture, drives a hub that anchors the opposite end of the cable. The motor has a peak torque of 13.6 N·m when operating with three-phase, 230-V power; the gear reduction has a 97% efficiency and 0.08° backlash. Altogether, when connected to 120-V power supply, the calculated peak actuator torque is 45 N·m [44]. This motor/gearbox combination was selected to optimize speed and size while fulfilling the torque requirement. The motor and servoamplifier (Moog T200 Servodrive) are controlled using a custom-assembled PC104 stack containing a PC104 computer, data acquisition card, and other supporting hardware. Control software operates the PC104 target computer from a connected laptop (host) using MATLAB XPC sampling at 1 kHz. The motor, gearbox, amplifier, target, and host computer are all remotely mounted away from the user. A block diagram of the device is shown in Fig. 2.
Fig. 2.
Block diagram of the SERKA. The target computer uses a PID controller to control the displacement of the cable relative to the brace angle.
Flexion torque is exerted on the knee proportional to the deflection of the spring. Contrary to typical series elastic actuators, the SERKA measures spring deflection, but it does not use it for control due to the nonlinear transmission dynamics of the Bowden cable. Instead, the motor operates in torque control, using a PID controller to follow the position of the brace θ, when zero torque is desired (transparent mode).When applying a torque perturbation, the motor changes its position ϕ to an offset (ϕ − θ) corresponding to a desired torque.
Torque is initiated based on contralateral heel strike and ends at ipsilateral toe-off. Since both feet are making contact with the ground during this period, it is known as double support. These events are detected using the load cells from an ADAL split-belt instrumented treadmill (Tecmachine, Andrezieux Boutheon, France). These load cells located in each belt can also be used to detect ground reaction forces of each limb and, when combined with motion capture, to detect joint kinetics and useful data for future experiments.
The SERKA has a number of safety mechanisms. Emergency stops are available to both the subject and experimenter. Software stops prevent the device from exerting torque at the wrong time in the gait cycle. Although the brace actuates only in flexion, the knee brace has a mechanical stop to prevent knee hyperextension. If the cable breaks, the spring returns to equilibrium, and torque on the knee goes to zero.
In summary, we designed the SERKA to exert a torque quickly or to exert no torque at all, depending on the stage of gait. We performed calculations showing that the commercial knee brace is strong enough to withstand the maximum torque while still remaining comfortable. The motor and gear reduction were designed to be strong enough to bend the knee of an affected population, yet were fast and safe. The only weight the user feels is of the elastic element and surrounding structure, thus making the device lightweight and transparent.
III. Performance
The performance of the device is based on exerting a torque quickly and repeatedly, maintaining its orientation on the knee during operation and being transparent enough to be imperceptible while moving.
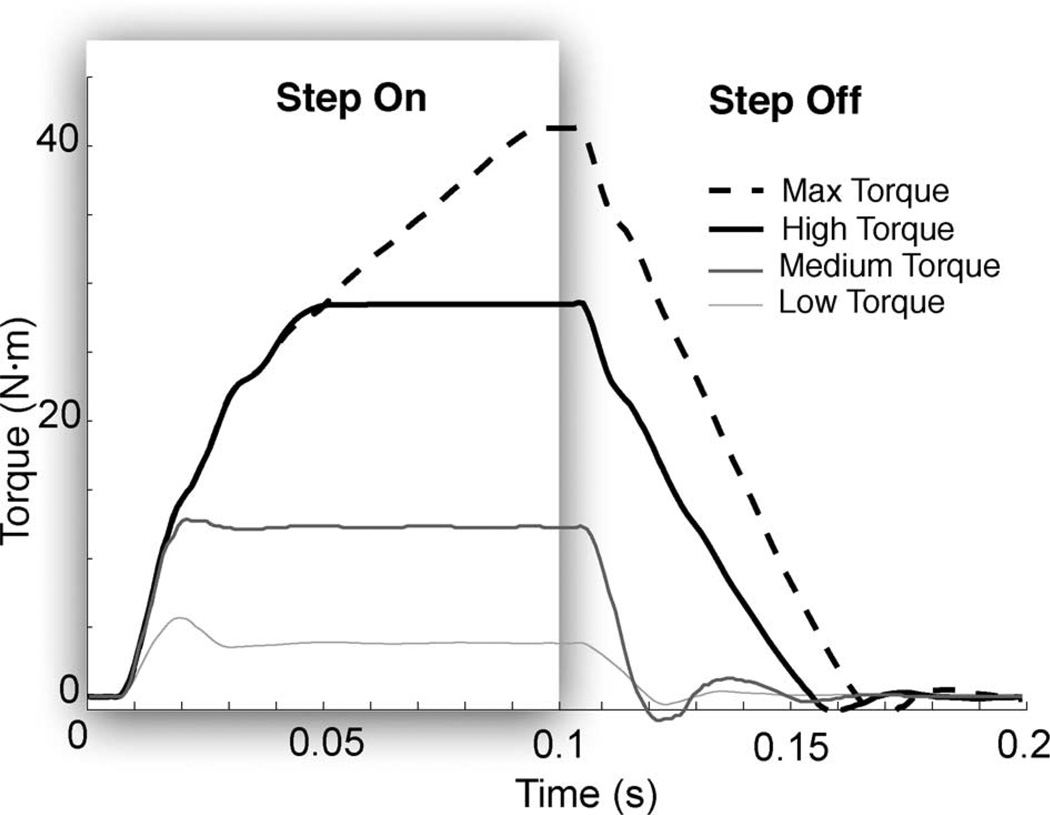
First, we tested how fast the device could exert torque; tests were performed on a rigid plaster model of a leg. We wanted the device to be able to be used to study reflexes; therefore, we needed a small torque bandwidth of 8 Hz and a rise time faster than human reflex latency, i.e., 30 ms [35].We also wanted high assistance torques to be faster than human reaction time thus leading to a bandwidth of 4 Hz and speed faster than 150 ms for large torques [35]. We gave three successive step inputs lasting 100 ms spaced 3 s apart at low, medium, high, and maximum torques. These values were based on what constitutes a small flexion torque (4N·m), peak flexion torque during typical walking (12 N·m), upper level capability of the device (28 N·m), and maximum torque (41 N·m), respectively. Fig. 3 shows the average of the three step inputs for each of the four torque levels. The 90% rise time and 5% settling time for both the increase in torque and the decrease are shown in Table I. As more effort is required of the actuator, rise time increases, with fewer transients due to sheath friction. At low torques, however, we observed 30% overshoot as a result of reduced friction at small cable excursion. Maximum torque can be applied in less than voluntary movement time, and in less than the time it takes for a monosynaptic reflex, the device can exert typical maximum knee flexion torques experienced in gait.
Fig. 3.
Step responses (each curve is the average of three trials) for low, medium, and high torques. In this experiment, we measured torque by the deflection in the spring.
TABLE I.
Torque step response of the serka
| Step On | Step Off | |||
|---|---|---|---|---|
| Torque | 90% Rise Time (s) |
5% Settling Time (s) |
90% Fall Time (s) |
5% Settling Time (s) |
| 4 N·m | 0.013 | 0.035 | 0.019 | 0.027 |
| 12 N·m | 0.017 | 0.018 | 0.016 | 0.047 |
| 28 N·m | 0.040 | 0.044 | 0.047 | 0.050 |
| 41 N·m | 0.078 | 0.089 | 0.057 | 0.060 |
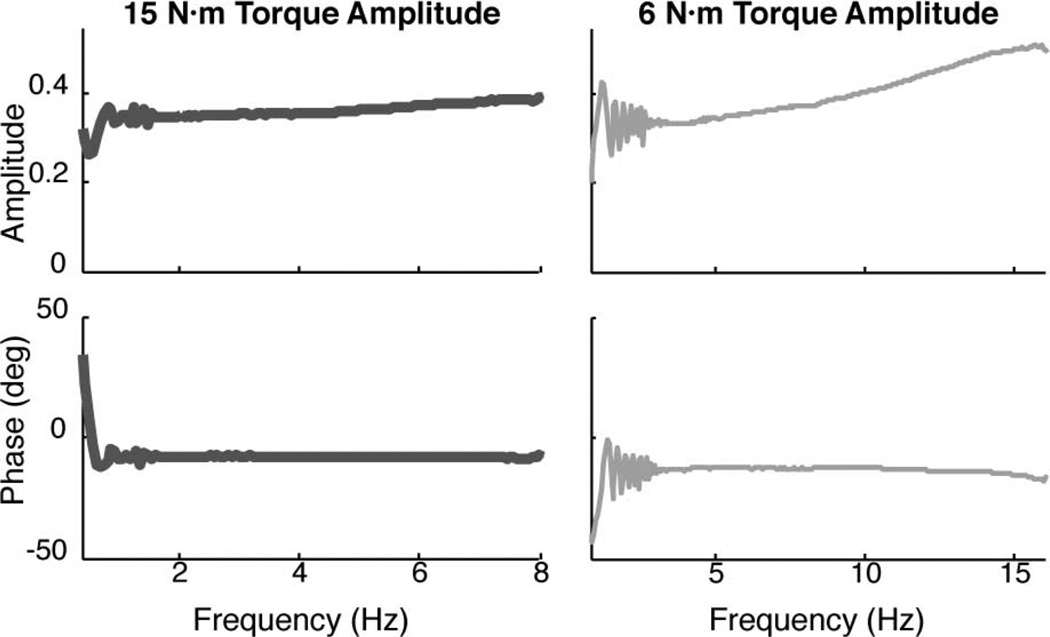
To measure torque bandwidth, we used a chirp torque input applied by the motor. A chirp signal is a sine wave with frequency linearly increasing over time; in this case, it is 60 s. With this slowly increasing frequency input, it was rather straightforward to determine how performance changes in the desired frequency operating range and beyond. We used two different amplitudes: low (6 N·m amplitude, 6 N·m offset) and high amplitudes (15 N·m amplitude, 6 N·m offset). Since the goal for low torque bandwidth was 8 Hz, we tested using a chirp input up to 16 Hz. Likewise, since the goal for high torque bandwidth was 4 Hz, we tested an 8-Hz maximum chirp signal. The SERKA was fully capable of producing torque at the maximum frequency of both tests, as shown in the Bode plots of Fig. 4, comparing desired deflection to measured torque. The noise at low frequency comes from the smaller amount of low-frequency input content in a chirp signal. In both cases, magnitude and phase remain constant throughout the frequency range. Above 8 Hz in the low-torque case, the system gradually approaches a resonance, but the resonant frequency is beyond 16 Hz.
Fig. 4.
Bode plots of high and low torque amplitudes. Note that the output is torque and the input is position (contrary to the more traditional input of torque and output of position) since this is a series elastic actuator.
Transparency is critical in this experiment, and our goal was to create an actuator that feels imperceptible to the knee during movement. One healthy subject gave informed consent. The protocol was approved by the Northwestern University’s Institutional Review Board guidelines. The subject wore the actuator, commanded to exert zero torque, and walked at two speeds to measure transparency. The first speed was 2.0 km/h, which is about the average speed for SKG [15], and 4.0 km/h, which is typical walking speed for a healthy adult. After walking for 60 s, the rms torque on the knee at 2.0 km/h was measured at 0.67 N·m and a value of 0.51 N·m at 4.0 km/h. Average peak torques during these trials were 1.12 and 1.22 N·m for the slow and typical walking speeds, respectively. The subject reported that no resistance was perceived due to the device, meaning that it was sufficiently transparent.
IV. Pilot Experiment
We wanted to evaluate how well the device performs in the field. Therefore, we conducted a pilot test to examine if the brace was strong enough to move the knee of stroke patients during gait. We recruited five chronic stroke subjects with reduced knee flexion during gait and one healthy subject and acquired informed consent in accordance with Northwestern University’s Institutional Review Board guidelines to participate in this study. Subject data are shown in Table II. Inclusion criteria were 1) reduced knee flexion during swing; 2) left-side hemiparesis; 3) ability to ambulate without assistance such as a cane; and 4) ability to provide informed consent.
TABLE II.
Subject Data
| Subject | S1 | S2 | S3 | S4 | S5 | H |
|---|---|---|---|---|---|---|
| Age (yrs.) | 38 | 50 | 43 | 35 | 65 | 28 |
| Gender | M | F | M | M | M | M |
| Years post-stroke | 28 | 3 | 10 | 2 | 27 | N/A |
| Self-selected Speed (m/s) | 0.85 | 0.90 | 0.90 | 1.07 | 0.75 | 1.15 |
| Quad. Resistance (mod. Ashworth) | 1 | 1+ | 1+ | 0 | 2 | N/A |
| Ankle-foot orthosis? | N | Y | N | Y | N | N/A |
Each subject walked on a split-belt treadmill while wearing the device on their paretic limb and a harness to prevent falling (see Fig. 5). Each subject walked for 60 s per trial at 2.0 km/h (for the first 20 s, no forces were applied). The load cell information was fed into the target computer to detect gait events. Torque rose to its desired level upon contralateral heel strike and then returned to zero upon ipsilateral toe-off. Each subject experienced various increasing assistance levels that remained at a constant value within each trial. The amount of assistance was determined by visual inspection of knee flexion angle, thus gradually increasing to try and reach “normal” knee flexion. We measured migration of the brace after each trial and asked each subject for their evaluation of the comfort of the device.
Fig. 5.
Experimental setup where a subject wears a harness to be protected from falls. Cables leading to device are for Bowden actuation and sensors, whose weight is partially supported at the bar.
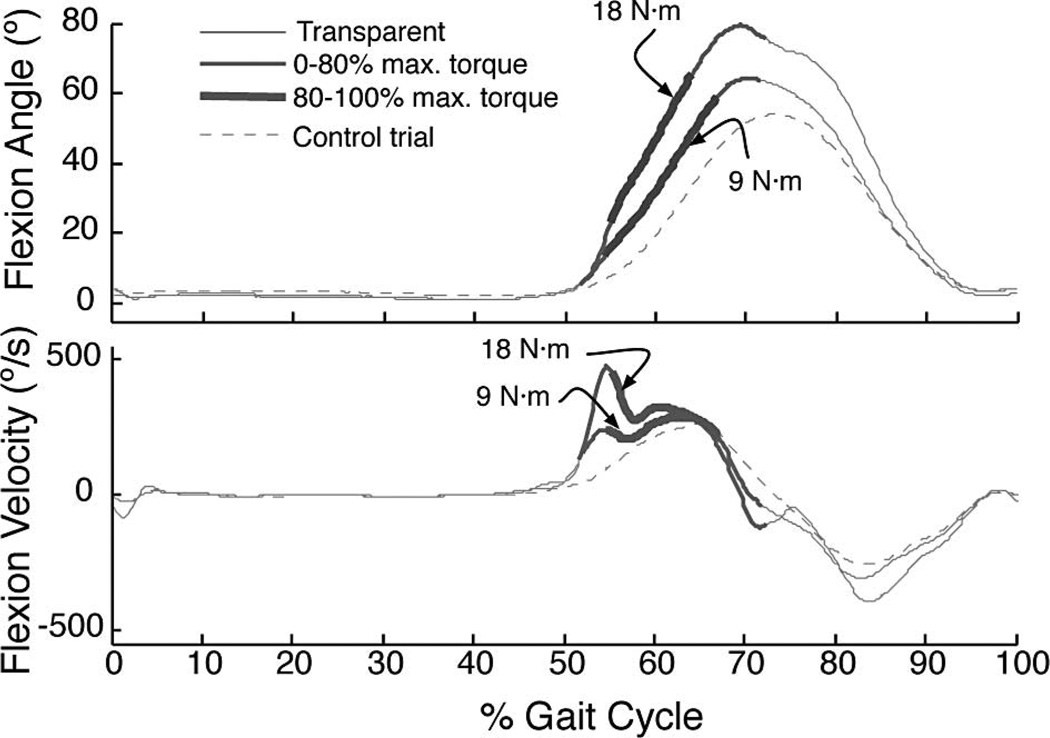
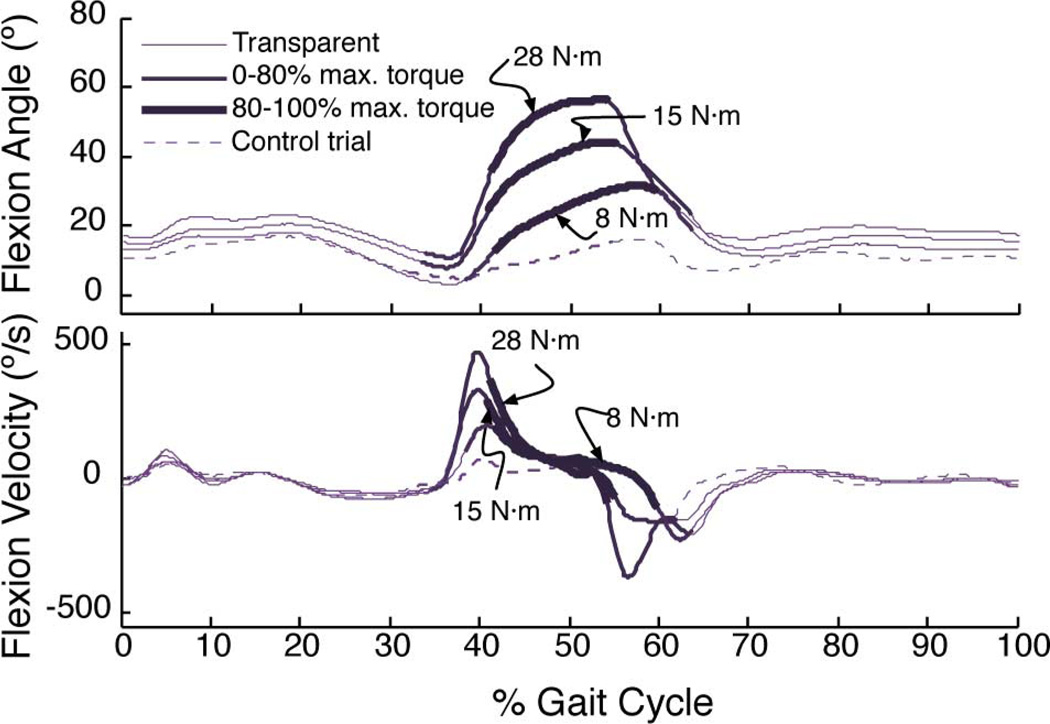
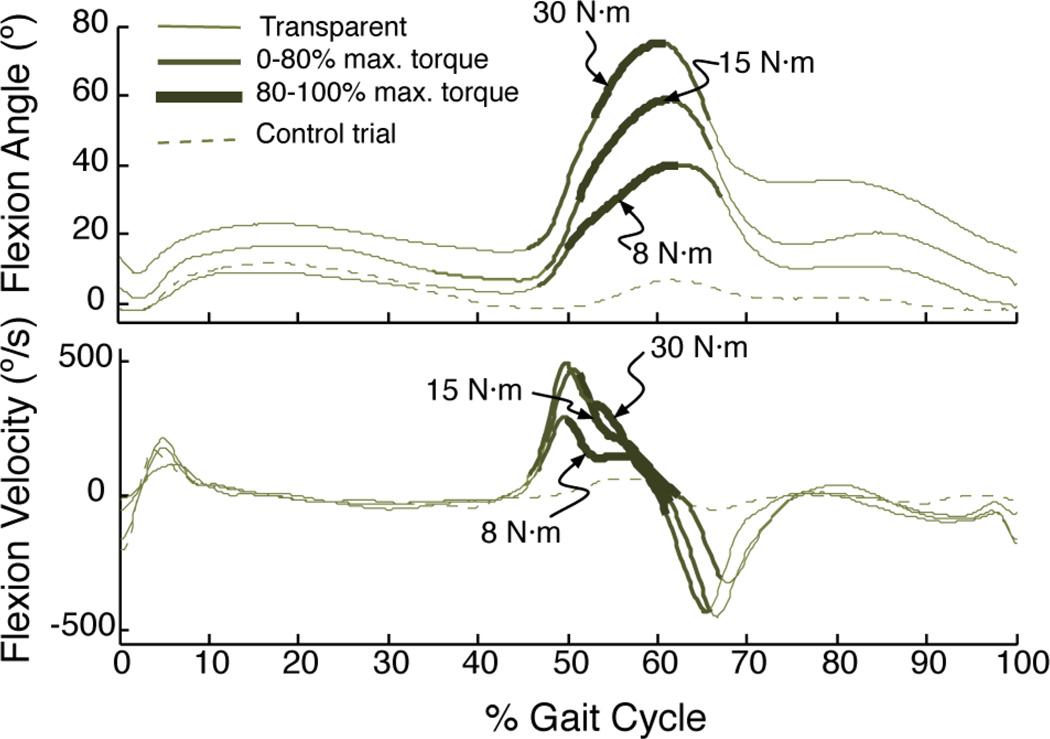
The SERKA was capable of increasing knee flexion angle, but each subject reacted to the assistance differently. Figs. 6–8 illustrate how assistance for the healthy subject and two stroke subjects differ from each other in both knee flexion angle and knee flexion velocity.
Fig. 6.
Flexion assistance increases knee flexion angle and velocity during swing in a healthy subject (H). The thin lines represent when the robot was programmed to behave transparently, and as the thickness increases and the lines darken, the torque rises. The dashed line represents walking without any assistance. Each line is the average of approximately 20 steps. Gait cycle begins and ends at ipsilateral (left) foot strike.
Fig. 8.
In subject S5, knee flexion angle and velocity increase during the assistance, but the kinematics return to their typical values once the assistance stops.
A. Subject H
For the healthy subject (subject H; see Fig. 6), peak knee flexion and knee flexion velocity increased with increasing assistance. Peak knee flexion angle increased 27°, and peak velocity increased 214°/s from the control trial. Knee flexion velocity initially rose with assistance but converged to the control velocity by toe-off. Double support lasted for an average of 17% of the gait cycle.
B. Subject S2
For the stroke subject (subject S2; see Fig. 7), knee flexion angle was affected throughout the gait cycle by the increase in assistance. This subject, who is only three years poststroke, was capable of voluntary knee flexion while seated or standing but only with significant effort. The subject wore a hinged ankle-foot orthosis that permitted only ankle plantar and dorsiflexion.
Fig. 7.
In subject S2, the assistance increased knee flexion angle during swing phase.
The SERKA was successful at increasing knee flexion angle during swing phase in subject S2. Knee flexion angle increased to its greatest extent while torque was being applied, but its effect lasted throughout the swing period. Peak knee flexion angle monotonically increased with torque, which is a total of 72° from the control trial. In addition, knee angle during the entire gait cycle increased a small amount as trials progressed.
Knee flexion velocity increased as torque applied increased (peak flexion velocity increased 435°/s) but not monotonically; 30 N·m assistance resulted in the same velocity profile as 15 N·m assistance. While the assistance increased velocity during preswing, at toe-off the velocity did not change from the control trial. Double support was similar to subject H, i.e., 18%.
C. Subject S5
For subject S5 in Fig. 8, flexion angle and velocity only increased during assistance. This subject, who is 27 years post-stroke, was not able to voluntarily bend his knee whether standing or seated and had increased resistance in his quadriceps (modified Ashworth of 2 out of 4). The subject did not wear an ankle-foot orthosis.
The device was successful at increasing knee flexion angle in subject S5, but this effect did not last beyond the period of assistance. Directly after assistance, the knee position reverted back to the subject’s original gait patterns. As with subject S2 (see Fig. 7), there is a slight offset increase in flexion angle throughout the gait cycle as trials progressed. This offset increase was not seen in any other subjects. Peak knee flexion angle increased 43° from control at maximum assistance.
Knee flexion velocity also increased, and like flexion angle, the effect only lasted during assistance. Peak knee flexion velocity occurred at the same point in gait cycle as the control trial in the beginning of the double support period. Peak flexion velocity increased 437°/s with assistance. Double support period was longer than in any other subjects, which is about 21% of the gait cycle. In this case, the increase in knee flexion velocity preswing did not affect knee flexion angle during swing.
D. All Subjects
Comfort and migration were monitored for all subjects. Throughout the trials, there was no measurable migration. Subjects were repeatedly asked about comfort, and on one occasion, small adjustments were necessary to relieve the tension in the straps, which alleviated any discomfort.
Given the variable bending of the cable sheath during gait, friction could play a role in reducing repeatability. We averaged the standard deviation during torque trials over all subjects and found an average variability of 0.48 N·m, which is an imperceptible value.
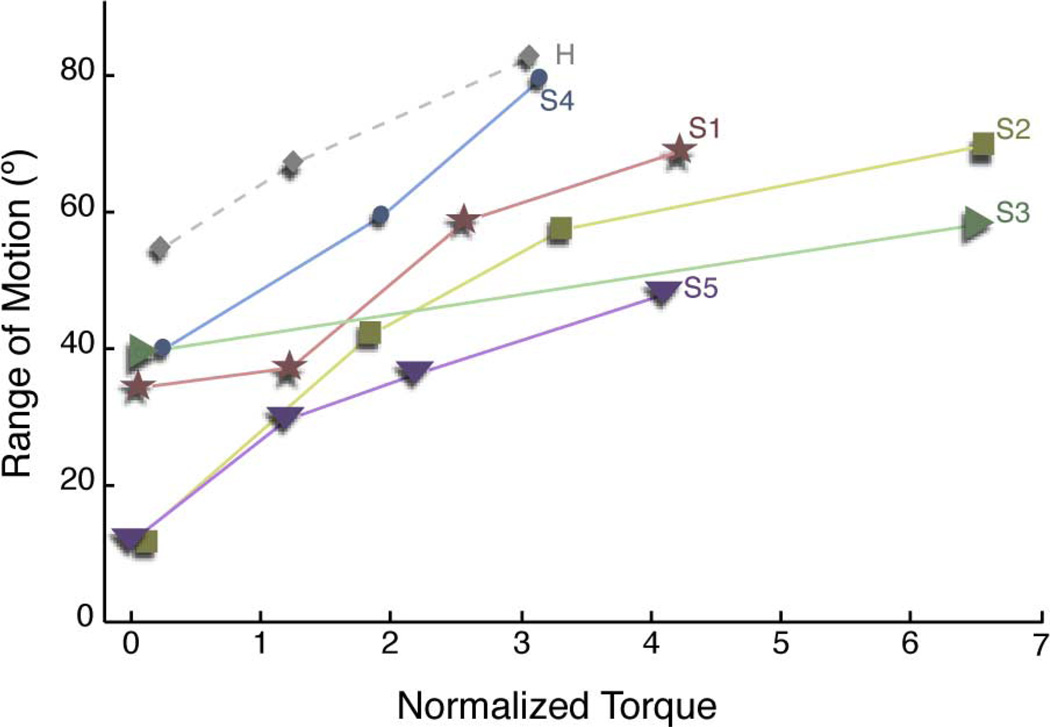
All of the subjects experienced an increase in both knee flexion angle and velocity, despite different reactions to the disturbance. Fig. 9 shows a comparison of knee range of motion, and Fig. 10 shows velocity against the assistance torque, both normalized to the predicted maximum knee flexion torque based on the subjects’ height, weight, and gait speed [45]. For instance, a normalized torque of 2 is twice the predicted knee torque necessary at a given speed. It should be noted that the torque exerted on subject S1 is estimated from previous data since the encoder connection failed during that test.
Fig. 9.
For all stroke subjects, knee flexion assistance increased range of motion. Labels on plot correspond to subject data in Table II. Each data point represents the average peak parameters of about 20 steps. Since each step taken causally affects the following step, observations of peak gait parameters are not independent, and variability such as standard deviation is not useful. Therefore, only averages are given.
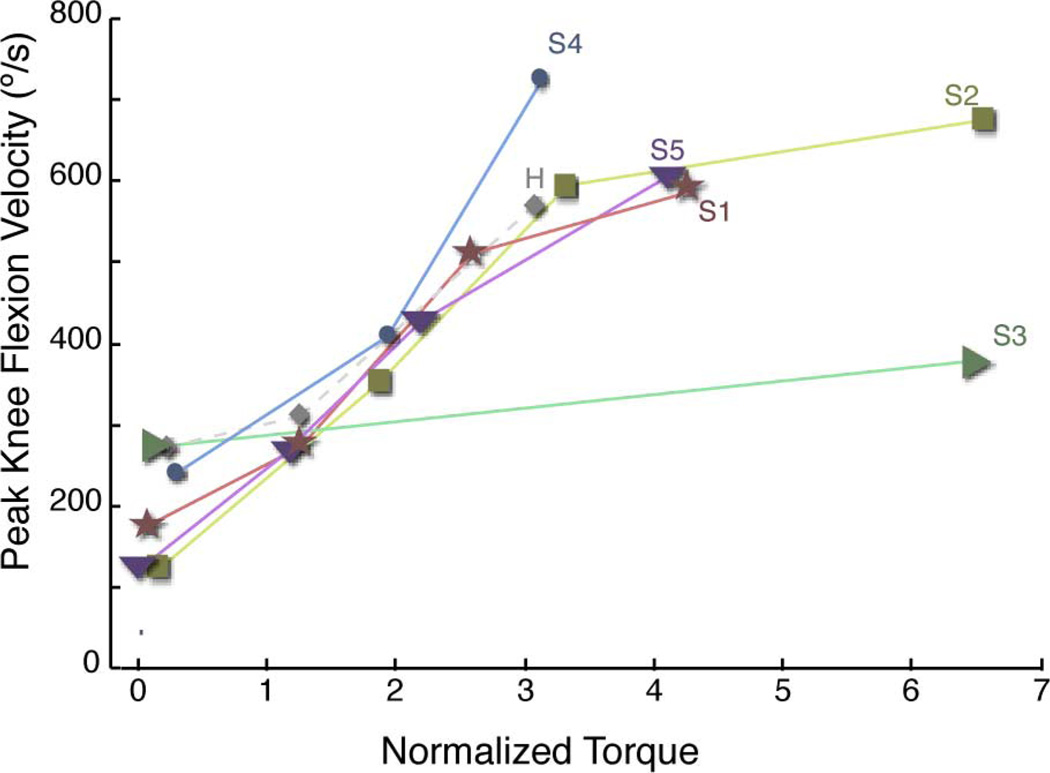
Fig. 10.
For all stroke subjects, knee flexion velocity also increased significantly with increasing torque. Labels on plot correspond to subject data in Table II.
Consistent with the previous three subjects, the knee flexion assistance increased peak knee flexion and, as a result, range of motion during gait. Subject S2 experienced the greatest increase in range of motion, and subject S3 increased the least. Taking all subjects into account, knee flexion angle increases significantly with torque assistance (linear regression, p ≤ 0.005).
Knee flexion velocity also significantly increased in all stroke subjects with flexion torque assistance (p ≤ 0.005) using a linear regression. Similar to range of motion data, subject S3 had the lowest increase in velocity, and subject S2 had the highest increase. However, knee flexion velocity at toe-off did not increase significantly with assistance, nor did knee flexion velocity at toe-off correlate with peak knee flexion during swing (linear regression, p = 0.18). This appears to be contrary to a number of modeling studies [8], [12], [46]. Instead, peak knee flexion velocity occurred approximately half-way into preswing (average of 47% of preswing, standard deviation of 30%).
V. Discussion and Conclusion
The overall goal of the SERKA is use as a scientific tool for understanding SKG. This paper introduces the device, details its performance, and then covers a pilot experiment comparing stroke subjects to a healthy subject.
A. Design and Performance
Given our design considerations, there is no device to our knowledge that is better fit for our application of selectively assisting knee flexion torque during gait. The only weight on the user is the brace, elastic element, and support structure. The compliance of the spring allows transparency that is, measured at less than 1 N·m of rms torque during typical walking. The speed and bandwidth were within design criteria. The commercial knee brace chosen was generally comfortable for subjects and did not migrate on the leg.
The resulting weight of the device was 1.2 kg on the leg. Weight minimization is important; a previous study using an active knee orthosis weighing over 3 kg has shown to affect hip, knee, and ankle kinematics in both limbs of a healthy subject [47]. The effect was most pronounced under asymmetrically loaded conditions. The SERKA’s effect on gait will be examined in future study.
The Bowden sheath and cable design was centered on friction reduction. The Spectra cable and Teflon-lined sheath reduce friction when compared with steel–steel contact. While avoiding sharp bends in the sheath further reduced energy loss due to friction [32], we also learned that minimizing cable angle at exits increased cable life. Using a stiff Bowden sheath can help reduce the number of bends the cable passes through.
Other changes can be made to improve the function of the device. The current version of the SERKA operates only in flexion, but it can be modified to operate in both extension and flexion by using the rotating hub as a capstan. This would require pretensioning, however, which means that the creep-prone Spectra cable would need to be replaced with another material. Weight could potentially be reduced further, perhaps by using a carbon fiber elastic element instead of spring steel [48].
B. Assistance of Knee Flexion in Stroke
Torque assistance in preswing significantly increased both knee flexion angle and velocity in the five stroke subjects and the healthy subject, thus confirming the SERKA’s effectiveness as a scientific tool for research on gait in stroke.
Each subject responded differently to the assistance, which may indicate a different level of impairment. This relationship is most easily summarized in Fig. 9, which compares normalized torque to knee range of motion. The higher the slope of a particular subject, the less their resistance to robotic assistance. This slope does not seem to be correlated with quadriceps resistance to passive stretch (Ashworth), years poststroke, age, or self-selected walking speed, but no conclusions can be made from these few subjects. In two of the subjects (S2 and S5), an increase in knee flexion angle was observed over the entire stride, which could mean that over time, resistance to assistance decreases. We also found that knee flexion velocity during middle of preswing is more indicative of peak knee flexion during swing than knee flexion velocity at toe-off, which is independent of impairment level. Future study will examine the effects of adaptation to assistance.
The timing of the torque pulse, beginning at contralateral heel strike and ending at ipsilateral toe-off, was sufficient for subjects with healthier gait, but as double support time increased, the timing may have prevented greater knee flexion during swing. For example, subject S5 had a longer double support period. Timing the torque pulse at contralateral heel strike may have been premature resulting in the reduced sensitivity to assistance. Subject S1, who responded to the assistance better than S5, felt the timing was “a little off” in his case. However, it is difficult to use subjects’ feedback on timing since they have altered sensation in their paretic limbs.
While migration is a considerable issue for orthotics, at this point there has been no evidence of any problems. Each subject donned the orthosis for about 20 min, while walking with perturbations, without any migration problems. Migration will continue to be monitored in subsequent studies, as trial time will be longer.
It is surprising that increased knee flexion velocity at toe-off was not necessary for increased peak knee flexion angle in swing, whether or not the subject was impaired. Instead, peak knee velocity in the middle of preswing was a more-accurate indicator of knee flexion angle during swing. This result is consistent with a modeling study, which concluded that RF activity in preswing is a better indicator of peak knee flexion angle than RF activity in early swing [49]. This does not claim that knee flexion velocity at toe-off is not important, but rather increasing knee flexion velocity before toe-off can also improve knee flexion angle during swing.
Future work will take advantage of more measurements and longer training periods. It is important to note that the knee positions and velocities are not of the knee itself but of the knee brace. The brace was tightly secured to the knee, but compliance of the brace and the soft tissue leaves some error in the results. These inaccuracies can be accounted for using a redundant measurement system, such as motion capture, as will be employed in future. This will also allow calculation of joint torques in the hip and ankle. Electromyography (EMG) of selected muscles in the affected limb will reveal potential muscle discoordination or spastic reflexes. Longer walking times will allow subjects to adapt and deadapt to the assistance, thus providing time to observe expected changes in gait compensations.
In this investigation, we reviewed the performance and experimental evaluation of a novel actuator intended to determine the causes associated with SKG. The SERKA performs to specifications, and a subsequent experiment validated its use as a tool for altering joint kinetics and kinematics. Using this device, we plan on examining the role of the knee in SKG, thus applying knee flexion torque to help better identify the impairments associated with the disability. From this information, we will be able to understand what is necessary to restore a healthier gait, thus leading toward a blueprint for assistive devices and better rehabilitation strategies.
Acknowledgment
The authors would like to thank a number of investigators for their help: Dr. Y. Dhaher, Dr. G. Hornby, Dr. K. Gordon, and Dr. R. Bogey, D.O., all at the Rehabilitation Institute of Chicago, and Dr. E. Colgate at Northwestern University.
This work was supported in part by the American Heart Association, in part by the Department of Veterans Affairs, in part by the National Institutes of Health, National Institute of Neurological Disorders and Stroke under R01 NS053606, and in part by the Davee Foundation.
Biographies

James S. Sulzer received the B.S. degree in mechanical engineering from Ohio State University, Columbus, in 2002 and the M.S. degree in mechanical engineering from Northwestern University, Evanston, IL, in 2006. He is currently working toward the Ph.D. degree with Northwestern University and the Rehabilitation Institute of Chicago, Chicago, IL.

Ronald A. Roiz received the B.S. degree in cybernetics from the University of California, Los Angeles, in 2004 and the M.S. degree in prosthetics and orthotics from the Georgia Institute of Technology, Atlanta, TX, in 2007.
In 2008, he completed the orthotics residency at the Rehabilitation Institute of Chicago, Chicago, IL. He is now enrolled as a medical student at the University of Illinois-Chicago.

Michael A. Peshkin (M’85) received the Ph.D. degree from Carnegie Mellon University, Pittsburgh, PA, in 1988.
He is currently a Professor of mechanical engineering at Northwestern University, Evanston, IL. He is an inventor of cobots (collaborative robots) and has been engaged in the field of human-interactive aspects of robotics for many years. He is a founder of three companies in image-guided surgery (Mako Surgical), materials handling (Cobotics), and rehabilitation robotics (Kinea Design). His current research interests include exercise robotics, haptic communication between people, and electromagnetic sensors.

James L. Patton (M’98) received two B.Sc. degrees in mechanical engineering and engineering science/bioengineering from the University of Michigan, Ann Arbor, in 1989, the M.Sc. degree in theoretical mechanics from Michigan State University, East Lansing, in 1993, and the Ph.D. degree in biomedical engineering from Northwestern University, Evanston, IL, in 1998.
He is currently the Associate Director of the Center for Rehabilitation Robotics, Rehabilitation Institute of Chicago, Chicago, IL. He is also an Associate Professor of bioengineering at the University of Illinois at Chicago. He also holds Adjunct appointments in physical medicine and rehabilitation and mechanical and biomedical engineering at Northwestern University. He was engaged in research on haptics, modeling the human–machine interface, robotic teaching, and robotic facilitation of recovery from a brain injury. His current research interests include modeling of human–machine interactions and how to use these predictors to exploit the nervous systems’ adaptive capacities for teaching new movements.
Dr. Patton is a member of the IEEE Robotics and Automation and Engineering in Medicine Biology Societies, as well as the Society for Neuroscience. He is a reviewer of the IEEE TRANSACTIONS ON BIOMEDICAL ENGINEERING, the IEEE Engineering in Medicine Biology Magazine, and the IEEE TRANSACTIONS ON ROBOTICS AND AUTOMATION. He is the Chair of the IEEE-EMBS Technical Committee on Biomedical Robotics.
Footnotes
Color versions of one or more of the figures in this paper are available online at http://ieeexplore.ieee.org.
Contributor Information
James S. Sulzer, Department of Mechanical Engineering, Northwestern University, Evanston, IL 60208 USA, and also with the Sensory Motor Performance Program, Rehabilitation Institute of Chicago, Chicago, IL 60611 USA (JamesSulzer2009@u.northwestern.edu)
Ronald A. Roiz, Department of Prosthetics and Orthotics, Rehabilitation Institute of Chicago, Chicago, IL 60611 USA. He is now with the University of Illinois-Chicago, Chicago, IL 60607 (ronaldroiz@gmail.com)
Michael A. Peshkin, Department of Mechanical Engineering, Northwestern University, Evanston, IL 60208 USA (peshkin@northwestern.edu).
James L. Patton, Department of Bioengineering, University of Illinois at Chicago, Chicago, IL 60680 USA, and also with the Rehabilitation Institute of Chicago, Chicago, IL 60611 USA (pattonj@uic.edu).
References
- 1.Tech. Rep. Dallas, TX: Amer. Heart Assoc.; 2007. Heart disease and stroke statistics. [Google Scholar]
- 2.Perry J. Gait Analysis: Normal and Pathological Function. Thorofare, NJ: Slack; 1992. [Google Scholar]
- 3.Sutherland DH, Davids J. Common gait abnormalities of the knee in cerebral palsy. Clin. Orthop. 1993;vol. 288:139–147. [PubMed] [Google Scholar]
- 4.Hsu A, Tang P, Jan M. Analysis of impairments influencing gait velocity and asymmetry of hemiplegic patients after mild to moderate stroke. Arch. Phys. Med. Rehabil. 2003;vol. 84(no. 8):1185–1193. doi: 10.1016/s0003-9993(03)00030-3. [DOI] [PubMed] [Google Scholar]
- 5.Royer TD, Martin PE. Manipulations of leg mass and moment of inertia: Effects on energy cost of walking. Med. Sci. Sports Exerc. 2005;vol. 37(no. 4):649–656. doi: 10.1249/01.mss.0000159007.56083.96. [DOI] [PubMed] [Google Scholar]
- 6.Doke J, Donelan JM, Kuo AD. Mechanics and energetics of swinging the human leg. J. Exp. Biol. 2005;vol. 208(no. 3):439–445. doi: 10.1242/jeb.01408. [DOI] [PubMed] [Google Scholar]
- 7.Kerrigan DC, Gronley J, Perry J. Stiff-legged gait in spastic paresis. A study of quadriceps and hamstrings muscle activity. Amer. J. Phys. Med. Rehabil. 1991;vol. 70(no. 6):294–300. [PubMed] [Google Scholar]
- 8.Piazza S, Delp S. The influence of muscles on knee flexion during the swing phase of gait. J. Biomech. 1996;vol. 29(no. 6):723–733. doi: 10.1016/0021-9290(95)00144-1. [DOI] [PubMed] [Google Scholar]
- 9.Treanor J. The role of physical medicine treatment in stroke rehabilitation. Clin. Orthop. 1969;vol. 63:14–22. [PubMed] [Google Scholar]
- 10.Waters R, Garland D, Perry J, Habig T, Slabaugh P. Stiff-legged gait in hemiplegia: Surgical correction. J. Bone Joint Surg. Amer. 1979;vol. 61:927–933. [PubMed] [Google Scholar]
- 11.Sung D, Bang H. Motor branch block of the rectus femoris: Its effectiveness in stiff-legged gait in spastic paresis. Arch. Phys. Med. Rehabil. 2000;vol. 81:910–915. doi: 10.1053/apmr.2000.5615. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg SR, Ounpuu S, Delp SL. The importance of swing-phase initial conditions in stiff-knee gait. J. Biomech. 2003;vol. 36(no. 8):1111–1116. doi: 10.1016/s0021-9290(03)00106-4. [DOI] [PubMed] [Google Scholar]
- 13.Kerrigan DC, Roth RS, Riley PO. The modelling of adult spastic paretic stiff-legged gait swing period based on actual kinematic data. Gait Posture. 1998;vol. 7(no. 2):117–124. doi: 10.1016/s0966-6362(97)00040-4. [DOI] [PubMed] [Google Scholar]
- 14.Riley PO, Kerrigan DC. Torque action of two-joint muscles in the swing period of stiff-legged gait: A forward dynamic model analysis. J. Biomech. 1998;vol. 31(no. 9):835–840. doi: 10.1016/s0021-9290(98)00107-9. [DOI] [PubMed] [Google Scholar]
- 15.Kerrigan DC, Karvosky ME, Riley PO. Spastic paretic stiff-legged gait: Joint kinetics. Amer. J. Phys. Med. Rehabil. 2001;vol. 80(no. 4):244–249. doi: 10.1097/00002060-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Anderson FC, Goldberg SR, Pandy MG, Delp SL. Contributions of muscle forces and toe-off kinematics to peak knee flexion during the swing phase of normal gait: An induced position analysis. J. Biomech. 2004;vol. 37:731–737. doi: 10.1016/j.jbiomech.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 17.Greene P, Granat M. A knee and ankle flexing hybrid orthosis for paraplegic ambulation. Med. Eng. Phys. 2003;vol. 25(no. 7):539–545. doi: 10.1016/s1350-4533(03)00072-9. [DOI] [PubMed] [Google Scholar]
- 18.Kasaoka K, Sankai Y. Predictive control estimating operator’s intention for stepping-upmotion by exo-skeleton type power assist system HAL. Proc. IEEE/RSJ Int. Conf. Intell. Robots Syst. 2001;vol. 3:1578–1583. [Google Scholar]
- 19.Blaya J, Herr H. Adaptive control of a variable-impedance ankle-foot orthosis to assist drop-foot gait. IEEE Trans. Neural Syst. Rehabil. Eng. 2004 Mar.vol. 12(no. 1):24–31. doi: 10.1109/TNSRE.2003.823266. [DOI] [PubMed] [Google Scholar]
- 20.Chu A, Kazerooni H, Zoss A. On the biomimetic design of the berkeley lower extremity exoskeleton (BLEEX); Proc. IEEE Int. Conf. Robot. Autom; 2005. pp. 4345–4352. [Google Scholar]
- 21.Costa N, Bezdicek M, Brown M, Gray J, Caldwell D, Hutchins S. Joint motion control of a powered lower limb orthosis for rehabilitation. Int. J. Autom. Comput. 2006;vol. 3(no. 3):271–281. [Google Scholar]
- 22.Gordon KE, Sawicki GS, Ferris DP. Mechanical performance of artificial pneumatic muscles to power an ankle-foot orthosis. J. Biomech. 2006;vol. 39(no. 10):1832–1841. doi: 10.1016/j.jbiomech.2005.05.018. [DOI] [PubMed] [Google Scholar]
- 23.Hollander K, Sugar T, Herring D. Adjustable robotic tendon using a ‘jack spring,’. presented at the Int. Conf. Rehabil. Robot.; Chicago, IL. 2005. [Google Scholar]
- 24.Winchester P, Carollo J, Parekh R, Lutz L, Aston J., Jr A comparison of paraplegic gait performance using two types of reciprocating gait orthoses. Prosthet. Orthot. Int. 1993;vol. 17(no. 2):101–106. doi: 10.3109/03093649309164364. [DOI] [PubMed] [Google Scholar]
- 25.Andrews B, Baxendale R, Barnett R, Phillips G, Yamazaki T, Paul J, Freeman P. Hybrid FES orthosis incorporating closed loop control and sensory feedback. J. Biomed. Eng. 1988;vol. 10(no. 2):189–195. doi: 10.1016/0141-5425(88)90099-4. [DOI] [PubMed] [Google Scholar]
- 26.Ferris D, Czerniecki J, Hannaford B. An ankle-foot orthosis powered by artificial pneumatic muscles. J. Appl. Biomech. 2005;vol. 21(no. 2):189–197. doi: 10.1123/jab.21.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gordon KE, Ferris DP. Learning to walk with a robotic ankle exoskeleton. J. Biomech. 2007;vol. 40(no. 12):2636–2644. doi: 10.1016/j.jbiomech.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 28.Davis S, Tsagarakis N, Canderle J, Caldwell DG. Enhanced modelling and performance in braided pneumatic muscle actuators. Int. J. Robot. Res. 2003;vol. 22(no. 3/4):213–227. [Google Scholar]
- 29.Pratt JE, Krupp BT, Morse CJ, Collins SH. The roboknee: An exoskeleton for enhancing strength and endurance during walking. Proc. IEEE Int. Conf. Robot. Autom. 2004;vol. 3:2430–2435. [Google Scholar]
- 30.Andersen J, Sinkjaer T. Mobile ankle and knee perturbator. IEEE Trans. Biomed. Eng. 2003 Oct.vol. 50(no. 10):1208–1211. doi: 10.1109/TBME.2003.816073. [DOI] [PubMed] [Google Scholar]
- 31.Pratt GA, Williamson MM. Series elastic actuators. Proc. IEEE/RSJ Int. Conf. Intell. Robots Syst. 1995;vol. 1:399–406. [Google Scholar]
- 32.Townsend W, Salisbury J., Jr The effect of coulomb friction and stiction on force control. Proc. IEEE Int. Conf. Robot. Autom. 1987;vol. 4:883–889. [Google Scholar]
- 33.Veneman J, Ekkelenkamp R, Kruidhof R, Helm FVd, Kooij HVd. A series elastic- and Bowden cable-based actuation system for use as torque actuator in exoskeleton-type robots. Int. J. Robot. Res. 2006;vol. 25(no. 3):261–281. [Google Scholar]
- 34.Kong K, Jeon D. Design and control of an exoskeleton for the elderly and patients. IEEE/ASME Trans. Mechatron. 2006 Aug.vol. 11(no. 4):428–432. [Google Scholar]
- 35.Winter DA. Biomechanics and Motor Control of Human Movement. New York: Wiley; 1990. [Google Scholar]
- 36.Hornby T. Torque in spastic quadriceps. 2007 (unpublished data) [Google Scholar]
- 37.Bledsoe 2007 [Online]. Available: www.bledsoebrace.com. [Google Scholar]
- 38.Zhang M, Lee WC. Quantifying the regional load-bearing ability of trans-tibial stumps. Prosthet. Orthot. Int. 2006;vol. 30(no. 1):25–34. doi: 10.1080/03093640500468074. [DOI] [PubMed] [Google Scholar]
- 39.van Leerdam N. Academy of American Orthotists and Prosthetists. Chicago, IL: AAOP; 2006. The genux a new knee brace with an innovative non-slip system. [Online]. Available: http://www.oandp.org/publications/jop/2006/2006-42.asp. [Google Scholar]
- 40.Winter D, Ishac M, Scott S. Instantaneous centre of rotation of the knee during human gait; Proc. 12th Int. Cong. Biomech; 1989. [Google Scholar]
- 41.Walker P, Rovick J, Robertson D. The effects of knee brace hinge design and placement on joint mechanics. J. Biomech. 1988;vol. 21(no. 11):965–974. doi: 10.1016/0021-9290(88)90135-2. [DOI] [PubMed] [Google Scholar]
- 42.Carlson L, Veatch B, Frey D. Efficiency of prosthetic cable and housing. J. Prosthet. Orthot. 1995;vol. 7(no. 3):96–99. [Google Scholar]
- 43.Deng M, Latour RA, Ogale AA, Shalaby SW. Study of creep behavior of ultra-high-molecular-weight polyethylene systems. J. Biomed. Mater. Res. 1998;vol. 40:214–223. doi: 10.1002/(sici)1097-4636(199805)40:2<214::aid-jbm6>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 44.Moog T200 Programmable Servo Drive Manual. Blacksburg, VA: Moog, Inc; 2003. [Google Scholar]
- 45.Lelas JL, Merriman GJ, Riley PO, Kerrigan DC. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture. 2003;vol. 17(no. 2):106–112. doi: 10.1016/s0966-6362(02)00060-7. [DOI] [PubMed] [Google Scholar]
- 46.Goldberg S, Ounpuu S, Arnold A, Gage J, Delp S. Kinematic and kinetic factors that correlate with improved knee flexion following treatment for stiff-knee gait. J. Biomech. 2006;vol. 39(no. 4):689–698. doi: 10.1016/j.jbiomech.2005.01.015. [DOI] [PubMed] [Google Scholar]
- 47.Weinberg B, Nikitczuk J, Patel S, Patritti B, Mavroidis C, Bonato P, Canavan P. Design, control and human testing of an active knee rehabilitation orthotic device; Proc. IEEE Int. Conf. Robot. Autom; 2007. pp. 4126–4133. [Google Scholar]
- 48.Cherry MS, Choi DJ, Deng KJ, Kota S, Ferris DP. Design and fabrication of an elastic knee orthosis: Preliminary results. presented at the Int. Design Eng. Tech. Conf. Comput. Inf. Eng. Conf.; Philadelphia, PA. 2006. [Google Scholar]
- 49.Reinbolt J, Fox M, Arnold A, Ounpuu S, Delp S. Importance of preswing rectus femoris activity in stiff-knee gait. J. Biomech. 2008;vol. 41(no. 11):2362–2369. doi: 10.1016/j.jbiomech.2008.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]