Abstract
Objective
The purpose of this article is to explain how new systems of medical technology, specifically electronic medical records, are playing an increasingly crucial role in the modern health care system. By examining these new developments associated with electronic medical technology and the society-culture-personality model, these aforementioned theoretical frameworks might assist chiropractors in the diagnosis, treatment, and prognosis of their patients.
Discussion
The society-culture-personality model can be used as an organizational instrument for assisting chiropractors in developing a better understanding and appreciation of the interrelationships between electronic medical records technology and the society-culture-personality model. The socially meaningful interaction established through electronic medical records technology may enhance communication between the health care professionals and the patient and thereby could improve the quality of care.
Conclusion
It is essential that future and current chiropractic physicians be aware of the ramifications and changes brought about by electronic medical records technology so that they can integrate, synthesize, and actualize the results to deliver care that involves the ingredients of quality, affordability, availability, accessibility, and continuity for their patients. If these outcomes are examined consistently and well, future chiropractic physicians will be able to transfer the traditions of excellence, dedication, and creativity of the health care profession.
Key indexing terms: Chiropractic; Electronic health records; Technology, medical
Introduction
Electronic medical records (EMRs) or electronic health records (EHRs) have developed rather rapidly over the past several years.1-4 The impact of this new system of technology has influenced the health care institution globally in various forms, such as the professionalization of future practitioners,5,6 the doctor-patient relationship,7,8 and the team approach to health care.9 Indeed, Steven Kraus, DC, recently reminded the chiropractic profession that:
You are going to have to summit with EHR (Electronic Health Records) and digital documentation to stay in practice. Twenty years ago, only 10 percent of chiropractors had computers in their practice, usually for billing purposes. Today, 98 percent use computers on an everyday basis. In 1998, only 5 percent of health professionals had cell phones; today that number is almost 100 percent.10
He further noted that:
Technology is on an exponential curve. It's not going to take another twenty years for your colleagues to move to EHR. Most will be there by 2014, encouraged to do so by Medicare standards if they're not required to do so by their state governments, like in Minnesota. According to my own studies and a survey of over 800 random DCs in the U.S., 74 percent of chiropractors already acknowledge that mandatory EHR's are coming and that they need to adopt it soon. The longer you wait, the quicker this pace is going to be.10
Thus, striking improvements in medical technology are playing an increasingly important role in health care, contributing to improvement in diagnosis, disease management, quality of life, and public health.
The society-culture-personality model in relation to EMRs and chiropractors
We have alluded in previous research that the chiropractic profession is an integral part of the health care institution.11 Therefore, it is important to place the diverse body of descriptive and empirical research on EMR technology and society-culture-personality (SCP) relationships within a constructive type of theoretical framework (Fig 1). This perspective might assist chiropractors nationally and transculturally in the diagnosis, treatment, and prognosis of their future patients in a globalized world. Indeed, globalization, collaboration, economics, technology, and innovation have certainly transformed the landscape of the health care institution in dynamic areas of society, culture, and personality. These transformations have occurred in areas such as the quality of care, the availability of care, the affordability of care, the accessibility of care, and the continuity of care—factors that are intertwined and most essential in the practice of chiropractic medicine (Fig 1).11
Fig 1.
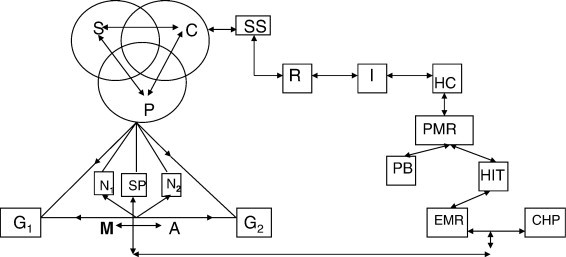
Society-culture-personality (SCP) and EMR in the health care institution. SCP, global village; S, society; C, culture; P, personality; N1, nature or heredity; N2, nurture or environment; G1, gemeinschaft; G2, gesellschaft; M, marginality; A, anomie; SS, social system; R, role; I, institution; HC, health care; SP, socialization process; PMR, patient medical records; PB, paper-based; HIT, health information technology; EMR, electronic medical records; CHP, chiropractic physician.
The SCP model (Fig 1) can be used as an organizational device for aiding chiropractors in developing a better understanding and appreciation of the interrelationships between EMR technology and the SCP model as they practice their roles as chiropractic physicians in diverse communities within a gemeinschaft (G1) (rural) and/or gesellschaft (G2) (urban) society (Fig 1).11,12 The purpose of this article is to examine these new developments associated with EMR technology and the SCP model within the health care institution. These areas of development are as follows: (1) changes in the doctor-patient interaction during clinical visits; (2) new patient and chiropractic physician roles and corresponding functions; and (3) new modes of communication between the health care professional and the patient.
New developments associated with EMRs, socially meaningful interaction, and SCP
It is important that health care workers recognize the implications of socially meaningful interaction (SMI) and its subdivisions in terms of diagnosis, treatment, and prognosis of a patient (Fig 2). Bloom13 and Evans14 have elaborated on the importance of SMI between the physician and the patient, and their findings can be applied to the chiropractic physician and the patient. For example, while interacting with the patient, the chiropractic physician should recognize the fact that the patient, although currently in seeming isolation, is a family member, reacting and behaving according to the way the family has influenced his or her understanding and attitudes concerning health and disease (Fig 2).
Fig 2.
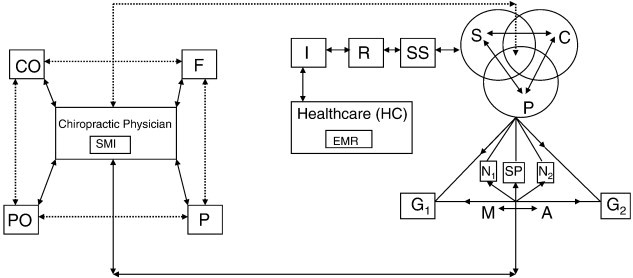
Society-culture-personality (SCP) and SMI in the health care institution. SCP, global village; S, society; C, culture; P, personality; N1, nature or heredity; N2, nurture or environment; G1, gemeinschaft; G2, gesellschaft; M, marginality; A, anomie; SS, social system; R, role; I, institution; HC, health care; SP, socialization process; EMR, electronic medical records; SMI, socially meaningful interaction; F, family; P, patient; PO, professional organization; CO, community organization.
In this manner, the chiropractic physician should be viewed not as an isolated “helper” of the sick but as a member of a larger profession that is part of and functionally linked to other cultural subgroups—hospitals, education, community organizations, professional organizations, and so forth (Fig 2). Indeed, Evans has cogently pointed out that a doctor and the patient “are products of culture—but one in balance, regulated by the familiar principles of homeostasis in which no part or function operates independently of all other parts or functions.”14
Communication, as an element in SMI, is a most relevant concept in health care (Fig 2). Professors Mumford and Skipper asserted that patients desire communication for at least 2 reasons: “First, as a means of obtaining information, and second, as a source of inter-personal contact.”15 They further noted that the patient's education will affect the ease of communication with the health care worker.15
Further research has indicated that the lower the educational attainment of the patient, the greater the probability that fear of the health care worker will be a problem, and the problem is compounded by a limited vocabulary. Explanations may be offered to the patient, but the message does not get through because the patient is unable to interpret the medical vocabulary.16
Electronic medical record technology significantly changes how patients interact with health care workers within a particular society and culture. As a result, chiropractic education must prepare future practitioners for this new type of relationship. In particular, pedagogy must accommodate for 3 key developments: (1) EMRs and the chiropractic physician–patient interaction in the SCP model in the community during clinical visits; (2) EMRs, the SCP model, and new patient and chiropractic physician roles and corresponding functions in the community; and (3) new modes of communication within the SCP model between the chiropractic physician, EMRs, and the patient. The following recommendations address select areas of a formal education curriculum that may necessitate modification based on these 3 new developments associated with EMR technology within the SCP model.
Electronic medical records and the doctor-patient interaction in the SCP model during clinical visits
Chiropractic physicians are trained to be observers. They engage in dialogue with the patient in order to spot postural or verbal cues that help them diagnose and design treatment strategies. The verbal exchange is also an effective tool for assuring the patients of the health care advocacy. In this sense, benefits of the doctor-patient dialogue are not restricted to the doctor. The patient is likewise searching for postural or verbal signs from the chiropractic physician to help the patient to discover important information. Therefore, the doctor-patient dialogue is invaluable to both participants. Consequently, when evaluating the influence of EMR technology on doctor-patient dialogue, analysts should explore how technology affects both the doctor and the patient (Fig 3).
Fig 3.
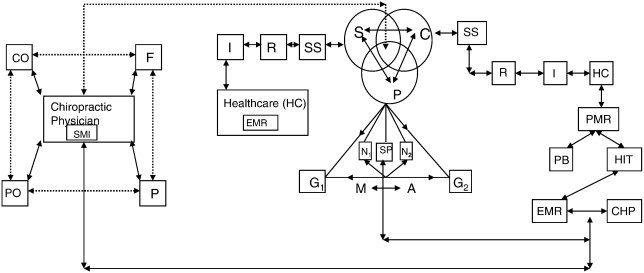
Society-culture-personality (SCP), EMR, and SMI in the health care institution for the new millennium. SCP, global village; S, society; C, culture; P, personality; N1, nature or heredity; N2, nurture or environment; G1, gemeinschaft; G2, gesellschaft; M, marginality; A, anomie; SS, social system; R, role; I, institution; HC, health care; SP, socialization process; EMR, electronic medical records; SMI, social meaningful interaction; F, family; P, patient; PO, professional organization; CO, community organization; PMR, patient medical records; PB, paper-based; HIT, health information technology; CHP, chiropractic physician.
For EMR data to be useful in future encounters, attention to detail during data entry is critical. Hence, chiropractic physicians have very little choice but to devote significant energy to data entry at the point of care. The problem with data entry at the point of care is that computer workstations or tablets require specific body positioning (along with hand and eye movement) that may limit the doctor's ability to concentrate on the patient's movements during the doctor-patient conversation. As a result, EMR technology in the examining room can act as a potential barrier to observation and communication (Fig 3). Lancaster University sociologist John Urry's analysis of copresence further illustrated why EMR technology can obstruct SMI between patient and doctor. He asserts:
Copresence affords particular access to the eyes. Eye contact enables the establishment of intimacy and trust, as well as insincerity and fear, power and control. Simmel considers that the eye is a unique “sociological achievement” as looking at one another is what effects the connections and interactions of individuals. This is the most direct and “purest” interaction. It is the look between people which produces moments of intimacy as: “One cannot take through the eye without at the same time giving”; this produces the “most complete reciprocity” of person-to-person, face-to-face. The look is returned and trust can get established and reproduced.17
Eye contact is a key component of doctor-patient communication at the point of care. The loss of eye contact can therefore lead to the deterioration of trust and damage the doctor-patient relationship. Thus, EMR technology at the point of care can initiate a series of doctor-patient problems stemming from loss of eye contact.
To remedy these problems, chiropractic educators must train future practitioners how to compensate for EMR technology at the point of care. Although data entry cannot be removed from the care process, techniques should be developed that minimize the effect of EMR technology on doctor-patient communication. These techniques should take into account body positioning and reestablish eye contact, which can mitigate some of the copresence problems that stem from computer use during patient interviews. Ultimately, patients cannot feel that they are competing with a computer for a chiropractic physician's attention during clinical visits. Addressing these communication concerns via EMR technology training can make a significant difference in doctor-patient interaction and help establish and reproduce trust (Fig 3).
Electronic medical records, SCP, and new patient and chiropractic physician roles and responsibilities in the community
A social system is a patterned relationship of roles (Fig 1). Electronic medical records technology creates a multiplicity of roles and responsibilities throughout the health care system affecting families and communities and professional organizations. More roles and responsibilities can result in more confusion and less quality, unless health care workers and patients come to learn what is expected of themselves and other health care team members. Thus, educating future chiropractic physicians and patients about these new roles is imperative.
Stanford University professor Edward Shortliffe's comments about information technology and health care education are telling. He states:
There is a difference between computer literacy (familiarity with computers and their routine uses in our society) and knowledge of the role that computing and communication technology can and should play in our health-care system. We are generally doing a poor job of training clinicians in the latter area, and are hereby leaving them poorly equipped for the challenges and opportunities they will face in the rapidly changing practice environments that surround them.18
Simply stated, future chiropractic physicians should learn what constitutes illness and health behavior is a health care system that uses information technology such as EMR software and the World Wide Web (WWW). Patients with access to EMR technology and knowledge via the Internet engage in dialogue with their health professional that is far more sophisticated. The patients walk into a chiropractic physician's office after conducting research on their condition and reviewing their own chart. Consequently, “there will need to be a shift in the doctor-patient relationship that focuses on sharing resources and negotiating treatment.”19 Future chiropractic physicians may require further training to accommodate these roles of information sharer and negotiator.
Though this shift will occur for many patients, it will not necessarily occur for those patients who are poorly educated or do not have access to this technology. As a result, chiropractic physicians should also be trained to ask relevant questions for determining the technical competency and educational opportunities of the patient to tailor the communication and treatment strategy accordingly. For those patients that do seek health care information over the Internet, chiropractic physicians should investigate which Web sites these patients are receiving their information from. Chiropractic physicians can then discourage those Web sites that are not industry approved and funnel patients to approved health care information Web sites through the patient's EMR. Essentially, physicians should receive “train the trainer” education that trains them how to teach patients to use EMR technology and Web sites to improve health outcomes. The “train the trainer” approach also encompasses educating patients about the roles and responsibilities of all health care team members, including the patient. As illness behavior is a learned behavior, patients must be taught by chiropractic physicians about their expanded role in the care process as a result of EMR technology and the Internet. Depending upon the willingness of the chiropractic physician to trust patient judgment, this training not only can improve the patient's understanding of personnel roles and responsibilities but also can increase the chance of treatment success.
Electronic medical technology coupled with health care information Web sites is transforming the doctor-patient relationship from an asymmetrical relationship to a more symmetrical relationship. Instead of the chiropractic physician having complete authority and sole access to the repository of health care knowledge, the patient is now empowered to contribute to the healing process. In sum, the role of the patient as a health care team member is more pronounced than ever before, and the chiropractic physician requires training to accommodate for a doctor-patient relationship that is heavily influenced by EMR technology in various societies (Fig 3).
New modes of communication within the SCP model between the chiropractic physician, EMRs, and the patient
Electronic medical records technology allows patients and health care workers to contribute data to the EMR from any location at any time in any society or culture (Fig 3). In addition, all e-mail communication can be captured in the patient's EMR to ensure continuity. Yet, communicating via e-mail or through the patient's EMR requires new rules that should be adhered to by both parties in order for this type of communication to be effective. If a chiropractic physician does not understand the proper use of e-mail or when to release patient information to the patient via the EMR, damage can be inflicted on the doctor-patient relationship. Thus, both the chiropractic physician and the patient should be educated about the proper use of communication made available by EMR technology in a society.
The team approach to health care involves communication, SMI, and EMR technology within the SCP model. Health care practitioners giving information on the patient's EMR must be taught what types of information are suitable for the particular patient. For instance, sensitive data, such as bad test results, should not be accessible to the patient electronically until the chiropractic physician and the patient have met to discuss the diagnosis. The education of health care practitioners regarding electronic communication and the release of information to the patient, via EMR technology, is composed of 2 distinct parts. The first part involves the health care practitioner learning to strike a balance between information suitable to be “pushed” and information that is “pulled” or demanded by consumers/patients.20 This includes instruction in proper e-mail etiquette and how to restrict access to specific sections of the EMR to the chiropractic physician only. The second part entails the training of the technologists to educate the patient about the patient's responsibilities pertaining to e-mail communication. The patient can be unsure at times about what e-mail communication is appropriate. It is the physician's responsibility to set the guidelines to avoid confusion or life-threatening situations irrespective of the society and/or culture concerned (Fig 3).
Besides the managed care, mass media, and malpractice stressors that have negatively affected the trust between the patient and the health care professional, patient privacy is a new stressor that can be addressed by the health care worker's education. Patient fears about their health information being made available to unintended parties is one of the biggest concerns of health care professionals transitioning to EMR technology. Patient perception regarding lack of confidentiality can constrict the flow of information between the patient and the practitioner, negatively impacting the ability of the chiropractic physician to diagnose and treat the patient. In order for chiropractic physicians to calm patient fears and educate them about security measures, some educational background in network security is necessary. Through training, the chiropractic physician will be able to confidently relay information through body and verbal language that adequate security measures are in place that ensure patient privacy and foster trust.
Though these recommendations pertaining to the training of health care practitioners may seem obvious to technically savvy health care workers, they do address important issues when dealing with new modes of communication. Nonetheless, chiropractic schools cannot assume that chiropractic and other health care workers already have obtained these skills. The doctor-patient communication is an organizational concern because the team approach to health care requires all team members to be on the same page regarding appropriate electronic communication. Time dedicated toward educating health care workers about electronic communication rules will ensure continuity and improve the quality of patient care and thus influence the availability of care, the affordability of care, and the continuity of care.
Conclusion
We have examined some select issues for the use of EMRs and the patient-practitioner relationship within the SCP model so that future chiropractic physicians can benefit from them. We have focused on (1) EMR and the doctor-patient interaction in the SCP model during clinical visits; (2) EMRs, the SCP model, new patient and chiropractic physician roles and responsibilities; and (3) new modes of communication within the SCP model, the chiropractic physician, EMRs, and the patient. It is hoped that current and future chiropractic physicians will internalize and make use of these select concepts and issues in their future roles as practitioners. In the SCP model, we have noted the impact of EMRs on the patient–chiropractic physician relationship, SMI, and the communication of a patient. In the SMI process, we have noted the interrelationships of the chiropractic physician within the family, the community, and the professional organization. Indeed, the family is the unit of health because it is the unit of living.
Implicit in our analysis is the focus that future and current chiropractic physicians be aware of the ramifications and changes brought about by EMR technology so that they can integrate, synthesize, and actualize the results to deliver care that involves the ingredients of quality, affordability, availability, accessibility, and continuity for their patients. If these outcomes are examined consistently and well, future chiropractic physicians will be able to transfer the traditions of excellence, dedication, and creativity of the health care profession.
On balance, in the analysis of EMRs it is essential that chiropractic physicians recognize the implications of the SCP system for the diagnosis, treatment, and prognosis of a patient. To be understood properly, beliefs and attitudes toward health and illness must be examined in a societal and cultural context.8 Such a concern for care epitomizes the dictum promulgated by Professor Francis Weld Peabody of Harvard Medical School; namely, “the secret of the care of the patient is in the caring for the patient.”21
Funding sources and potential conflicts of interest
The authors reported no funding sources or conflicts of interest for this study.
Acknowledgments
The authors thank all those who contributed to this research project: Loyola University Chicago, Harvard Medical School, Northeastern Illinois University, and members of Loyola University Chicago's Jesuit community. Tamil Selvi Chakrapani assisted in converting the diagrams into a digitized format. Dr. Marcel Fredericks thanks the Health Service Research Training Committee of the National Institutes of Health for the Public Health Service Fellowship at Harvard University Medical School.
References
- 1.Amatayakul M. 2nd ed. American Health Information Management Association; Chicago (Ill): 2004. Electronic health records: a practical guide for professionals and organizations; pp. 1–23. [Google Scholar]
- 2.Bates D., Mark E., Gotlieb E., Zapp J., Mullins H.C. A proposal for electronic medical records in U.S. primary care. J Am Med Inform Assoc. 2003;10:1–10. doi: 10.1197/jamia.M1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berkowitz L.L. Physician adoption strategies. In: Carter J.H., editor. 2nd ed. vol. 10. American College of Physicians; Philadelphia (Pa): 2008. pp. 231–252. (Electronic health records). [Google Scholar]
- 4.Carter J. American College of Physicians; Stanford (Calif): 2001. Electronic medical records: a guide for clinicians and administrators. [Google Scholar]
- 5.Fredericks M., Miller S., Odiet J., Fredericks J. Toward an understanding of cellular sociology and its relationships to cellular biology. Education. 2003;124:237–256. [Google Scholar]
- 6.Fredericks M. McFarland and Company; Jefferson (NC): 1980. Dental care in society: the sociology of dental health. [Google Scholar]
- 7.Fredericks M., Mundy P. Loyola University Press; Chicago (Ill): 1976. The making of a physician. [Google Scholar]
- 8.Fredericks M., Odiet J., Miller S., Fredericks J. Toward a conceptual re-examination of the patient-physician relationship in the health care institution for the new millennium. J Natl Med Assoc. 2006;98(3):378–385. [PMC free article] [PubMed] [Google Scholar]
- 9.Fredericks M. Social backgrounds and some selected attitudes of clinical students in a medical school. J Natl Med Assoc. 1968;60:201–206. [PMC free article] [PubMed] [Google Scholar]
- 10.Kraus S. Going paperless, part 2: lessons from the summit. Dynamic Chiropractic. 2008:18–23. [Google Scholar]
- 11.Fredericks M., Hang L., Ross M., Fredericks J., Lyons L. Chiropractic physicians: toward a synthesis of electronic medical records and the society, culture, personality model in the new millennium. J Chiropr Humanit. 2008;15:2–4. [Google Scholar]
- 12.Lyons L., Lam H., Ross M., Fredericks J., Fredericks M. Chiropractic physicians: a functional conceptualization of electronic medical records technology and the society, culture, and personality model in the delivery of health care. J Chiropr Humanit. 2008;15:10–18. [Google Scholar]
- 13.Bloom S.W. Russel Sage Foundation; New York (NY): 1963. The doctor and his patient. [Google Scholar]
- 14.Evans L.J. The University of Michigan Press; Ann Arbor (Mich): 1964. The crisis in medical education. [Google Scholar]
- 15.Skipper J.K., Mumford E. Harper and Row; New York (NY): 1967. Sociology in hospital care. [Google Scholar]
- 16.Koos E.L. 3rd ed. McGraw-Hill; New York (NY): 1959. The sociology of the patient. [Google Scholar]
- 17.Urry J. Connections. Environ Plan D. 2004;22:27–37. [Google Scholar]
- 18.Shortliffe E. The evolution of electronic medical records. Acad Med. 1999;74:414–419. doi: 10.1097/00001888-199904000-00038. [DOI] [PubMed] [Google Scholar]
- 19.Carlile S., Sefton A. Healthcare and the information age: implications for medical education. Med J Aust. 1998;168:340–343. doi: 10.5694/j.1326-5377.1998.tb138963.x. [DOI] [PubMed] [Google Scholar]
- 20.Nissen S., Abdulla A., Khandheria B., Kienzie M., Zaher C. The role of technology to enhance clinical and educational efficiency. J Am Coll Cardiol. 2004;44:256–260. doi: 10.1016/j.jacc.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 21.Peabody F.W. The case of the patient. JAMA. 1927;88:877–882. [Google Scholar]


