Abstract
Objective
Recurrent suicidal behavior is a defining characteristic of BPD. Although most patients achieve remission of suicidal behaviors over time, 3% to 10% die by suicide, raising the question of whether there is a high risk suicidal subtype in BPD. We are conducting the first longitudinal study of suicidal behavior in BPD to identify prospective predictors of suicide attempts, and characterize BPD patients at highest risk for suicide completion.
Method
Demographic, diagnostic, clinical and psychosocial risk factors assessed at baseline were examined for predictive association with medically significant suicide attempts using Cox proportional hazards models. Prospective predictors were defined for subjects completing 6 or more years in the study and compared to earlier intervals.
Results
Among 90 subjects, 25 (27.8%) made at least one suicide attempt in the interval, most occurring in the first two years. Risk of attempt was increased by: a.) low socioeconomic status, b.) poor psychosocial adjustment, c.) a family history of suicide d.) prior psychiatric hospitalization; e.) absence of any outpatient treatment prior to the attempt. Higher global functioning at baseline decreased risk.
Conclusion
Risk factors predictive of suicide attempts change over time. Acute stressors such as MDD were predictive only in the short term (12 mos.), while poor psychosocial functioning had persistent and long term effects on suicide risk. Half of BPD patients have poor psychosocial outcomes despite symptomatic improvement. A social and vocational rehabilitation model of treatment is needed to decrease suicide risk and optimize long term outcomes in BPD.
Introduction
Suicide is a rare event, with an incidence of 11.5 deaths /100,000 population (www.cdc.gov). The rarity of suicide makes it impossible to predict on the basis of known risk factors if or when a given patient will commit suicide (1).While it is impossible to predict individual suicides, suicide rates in the general population may be reduced by systematic physician education on identification and treatment of modifiable risk factors (2). Identifying clinically relevant risk and protective factors requires prospective studies of patients at high risk, using multidimensional assessments, and systematic follow-up. The results of such studies are immediately applicable to clinical assessment and treatment interventions. This is the first such study in subjects with Borderline Personality Disorder.
Why study suicidal behavior in Borderline Personality Disorder (BPD)? BPD is the only DSM-IV diagnosis defined, in part, by recurrent suicidal and self-injurious behaviors (called the “behavioral specialty of the borderline patient” by Gunderson and Ridolfi (2001) (3)). A history of suicide attempts is found in over 70% of consecutively studied inpatients and outpatients with BPD, with an average of 3 or more attempts at time of initial assessment (4). Co-morbidity with BPD increases the likelihood of suicidal behavior in other high risk disorders (5). In population studies, a co-morbid diagnosis of BPD is reported in over one-third of completed suicides (6,7), and half of parasuicidal patients admitted to hospital (8). With a suicide completion rate up to 10%, and a community prevalence estimated in the ECA Study at 2%, BPD is a high risk, clinically relevant model for the study of suicidal behavior (9).
Why study attempters? (Attempters are not completers.) A history of prior attempts is among the most powerful predictors of completed suicide. While only 10–15% of attempters become completers, 30% to 40% of suicide completers have a history of prior attempts (10). Prior attempts increase the likelihood of subsequent attempts (11). Attempters and completers are overlapping populations, with outcome determined, in part, by seriousness of intent and degree of medical lethality (10). High Lethality attempters with BPD share many characteristics of patients who complete suicide, including clinical, psychosocial and biological risk factors (9). Systematic prospective study of such high risk patients using standardized multidimensional methods identifies risk factors for completed suicide.
Following Mann et al. (5,12), we study a stress-diathesis model of suicidal behavior, which predicts an increase in risk of suicide when state stressors, such as acute depression, drug abuse or interpersonal crises, interact with chronic personality traits such as impulsive aggression, pessimism and hopelessness. In a first report from this longitudinal study, we noted a very high rate of interval suicide attempts in the first 2 years of follow-up (24.8% of 133 subjects). An acute stressor, MDD was predictive of interval attempts only in the very short term (e.g. 12 months), while measures of (poor) psychosocial function and illness severity (e.g. hospitalization prior to any interval attempt) were predictive of attempt behavior through the first 2 years (13). A low GAS score at baseline increased risk of suicide attempts in a pooled interval 2 to 5 years following intake, assessed independent of prior attempt experience. A high baseline GAS score was protective. Outpatient treatment was a protective factor which diminished risk of attempt in both short (12 month), and longer term (2–5 year) intervals. This report extends our analysis to an interval of 6 years, and contrasts predictors of suicidal attempts at 1, 2, 4, and 6 year intervals.
Method
This study was approved by the University of Pittsburgh Institutional Review Board and funded by the National Institute of Mental Health. Subjects were recruited from inpatient and outpatient services of the Western Psychiatric Institute and Clinic, and by advertisement, from the surrounding community. After complete description of the study to the subjects, written informed consent was obtained. Subjects were assessed by experienced Master’s level clinical raters. Assessments were obtained using semi-structured interviews, standardized self-rated and interviewer-rated measures, conducted in multiple sessions. Diagnoses on Axis I were made using the Structured Clinical Interview for DSM III-R (SCID, (14)). The SCID for DSM IV was used after that revision was introduced. Axis II disorders were diagnosed using the International Personality Disorders Examination (IPDE), which has a lifetime timeframe (15). Subjects were assessed for BPD using the Diagnostic Interview for Borderlines (DIB) (16). The DIB provides BPD diagnoses based on recent symptom severity, with a 3 month to 2 year framework for subsection scores. The Diagnostic Interview for Borderlines – Revised (DIB-R) was added when that version became available (17), and scored concurrently with the DIB to preserve continuity with the longitudinal study. The DIB-R has a 2 year timeframe for all subsections. For inclusion in the study, BPD subjects met criteria for probable or definite BPD on the IPDE, and definite BPD on the DIB (total Scaled Section Score ≥ 7) and DIB-R (total Revised DIB Score ≥ 8). Exclusion criteria included: schizophrenia, delusional (paranoid) disorder, schizoaffective disorder, any bipolar disorder, psychotic depression, CNS pathology (e.g. organic mood disorders, seizure disorder), drug or alcohol dependence (with evidence of withdrawal), physical disorders with known psychiatric consequences (e.g. hypothyroidism), borderline intellectual functioning (IQ < 70 by WAIS). Final diagnoses were determined by consensus of raters, using all available data, including medical records where available.
The pre-defined risk factors included: 1.) demographic variables; 2.) Axis I and II diagnoses; 3.) suicide history including: the Columbia Suicide History (18), the Suicide Intent Scale (SIS) and Scale for Suicidal Ideation (SSI) (19); 4.) state symptoms, including: the Beck Depression Inventory (BDI) (20) Hamilton Rating Scale for Depression-24 item (HamD-24) (21), Beck Hopelessness Scale (22), and Global Assessment Scale (GAS) (23); 5.) personality traits, including: the Barratt Impulsiveness Scale-11 (BIS) (24), Buss-Durkee Hostility Inventory (BDHI) (25), Lifetime History of Aggression (LHA) (26), MMPI_Psychopathic Deviate subscale (27), number of BPD criteria (IPDE), number of SPD criteria (IPDE), and IPDE dimensional scores; 6.) childhood history of physical and/or sexual abuse; 7.) family history of psychiatric disorders and suicide; 8.) social adjustment, including the Social Adjustment Scale-self report version (SAS-sr) (28), and, 9.) the history of psychiatric treatment.
Suicidal behavior was defined as any self-injurious behavior with intent to die. Each suicidal behavior was rated for medical seriousness using the Lethality Rating Scale, which rated medical consequences on a scale from 0 (no consequences) to 8 (death) for 8 forms of suicidal method (18). Subjects were assessed at baseline, 3 month and 12 month intervals in the first year, thereafter annually, supplemented by semi-annual phone assessments. At each assessment, demographic data, clinical diagnoses, suicide histories, and treatment experience were updated for the interval. State and trait symptoms, recent life events and psychosocial adjustment were also re-assessed. Deaths were discovered from systematic monthly searches through the Social Security Death Index and family contact. Death certificates were obtained in all cases to confirm official cause of death. Subjects were paid for all time and effort, including completion of self-rated forms and telephone interviews.
Statistical Analyses
Subjects who completed a minimum of 6 years in the study were included in this analysis. Cox proportional hazards regression models were constructed to examine the predictive association between risk factors and suicide attempts. Outcome was defined as a medically significant suicide attempt within the 6 year interval. This designation required a Lethality Rating Scale score ≥ 2, which requires some degree of medical attention. Time-to-event was computed as the difference between the date of baseline assessment to the first suicide attempt in the interval. To assess the effects of the most recent psychiatric treatment interventions on outcome, treatment variables were assessed within the 6 year interval, counting the most recent intervention before any suicide attempt in the interval. To use the entire interval for interval attempters would confound the role of treatment, as most medically significant suicide attempts in our setting are followed by psychiatric treatment. For non-attempters, the entire interval was used.
Estimates of relative risk (RR), and associated 95% confidence intervals were obtained from these models. Missing data resulted in variable sample sizes for some analyses. Data which were missed at predefined assessment points (because of subject unavailability), but obtained at a later date were counted retrospectively in the correct time frame for specific events, using only objective data, e.g. demographic changes (e.g. marriage, divorce, children), suicide attempts, hospitalizations, new onset of major Axis I disorders, and treatment episodes. All analyses were performed using SPSS for Windows Version 17 (Chicago, Ill.).
Results
The longitudinal study has enrolled 252 subjects from inception, of whom 90 subjects have completed six years of follow-up and were included in this analysis. The 6 year sample was 73.3% female, 26.7% male, with a mean (s.d.) age of 29.1(8.3) years. Subjects were 79.8% Caucasian, with a mean SES of 3.4 (0.6) on the Hollingshead Index (Class III). A majority of subjects (62.5%) had never married; though 27.0% had children living with them. Inpatient recruitment yielded 48.9% of subjects, while 21.6% were from outpatient clinics, and 29.5% were non-patients at the time of intake. At baseline, 52.8% of subjects had current DSM III-R diagnoses of MDD, 59.6% had Substance Use Disorders (SUD). The most common Axis II co-morbidity was with Antisocial Personality Disorder, found in 20% of subjects.
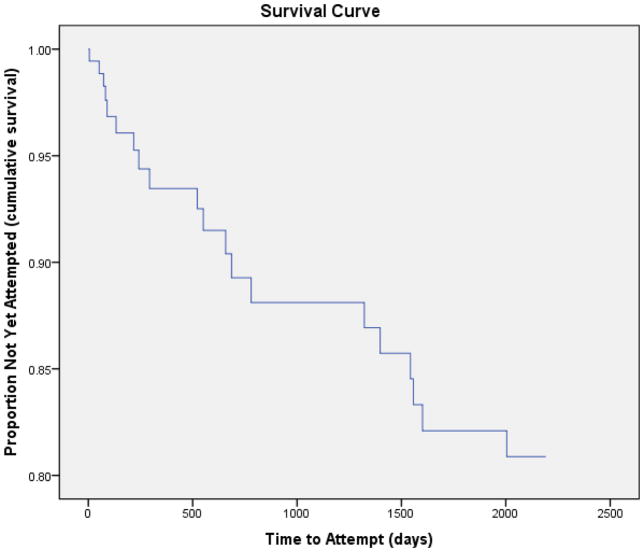
In the six year interval, 25 subjects (27.8%) reported medically significant suicide attempts. The survival curve (Fig. 1) illustrates the fact that most suicidal behaviors occur in the first 2 years of the study (24.8% of 133 subjects at 2 years). Selected bivariate comparisons between groups are presented in Table 1. Interval attempters differed from non-attempters in having significantly lower SES, less education, and poorer social adjustment (SAS-sr) at baseline, (all p<.05), with trend differences (p.<1) for lower baseline GAS. Interval attempters were more likely to report a history of medication use and psychiatric hospitalization prior to the interval attempt. They were also more likely to report a family history of suicide (all p. <.1) (Table 1). There was no significant difference between groups in history of prior attempts at baseline. Among interval attempters, 92% had baseline histories of prior attempts, compared to 81.3% of interval non-attempters. There were no significant differences between groups in Axis I or II co-morbidities, depressive symptoms (BDI, HRDS, Hopelessness), impulsivity or aggression (BIS, LGA, BDHI, MMPI_PD), illness severity (IPDE BPD criteria, DIB section score totals), childhood histories of sexual abuse, age at first hospitalization or total number of prior psychiatric admissions.
Figure 1.
Table 1.
Characteristics of interval attempters and non-attempters.
| Risk Factor | Attempter (n=25) | Non-Attempter (n=65) | Statistic, p-value |
|---|---|---|---|
| Age (mean ± SD) | 29.04 ± 8.55 | 29.02 ± 8.10 | t=0.12, p = ns |
| Sex (% female) | 76.0 | 73.4 | χ2=0.06, p = ns |
| Race (% Caucasian) | 72.0 | 82.8 | χ2=1.30, p = ns |
| SES (% low) | 52.0 | 28.1 | χ2=4.51, p = 0.03 |
| Education (≤ HS diploma) | 52.0 | 28.1 | χ2=4.51, p = 0.03 |
| MDD (% yes) | 44.0 | 56.3 | χ2=1.08, p = ns |
| Substance Abuse (% yes) | 64.0 | 57.8 | χ2=0.29, p = ns |
| Antisocial PD (% yes) | 20.0 | 20.3 | χ2=0.00, p = ns |
| GAS (mean ± SD) | 44.92 ± 9.98 | 54.38 ± 12.92 | t=3.29, p=0.09 |
| Family History of Suicide (% yes) | 8.0 | 0.0 | FET, p = 0.08 |
| SAS-SR Total Score (mean ± SD) | 2.78 ± 0.61 | 2.40 ± 0.64 | t=2.37, p = 0.02 |
| Hospitalization Prior to Attempt * (% yes) | 48.0 | 29.2 | χ2=2.82, p = 0.09 |
| Outpatient Treatment Prior to Attempt* (% yes) | 60.0 | 75.4 | χ2=2.08, p = 0.15 |
| Psychiatric Meds Prior To Attempt* (% yes) | 48.0 | 29.2 | χ2=2.82, p = 0.09 |
| Any Treatment Prior to Attempt* (% yes) | 72.0 | 76.9 | χ2=0.24, p = ns |
NOTE:
Treatment variables: “Prior To Attempt” indicates treatment that occurred in the interval of Baseline – 6 years but prior to the first attempt in the interval. FET: Fisher’s Exact Test.
Cox Regression analyses are presented for all intervals in Table 2, including the current 6 year model. At 6 year follow-up, variables best predictive of increased risk of suicide attempt in the interval included: a.) a family history of suicide, b.) no outpatient treatment (prior to the attempt), c.) low baseline SES, and d.) poor baseline psychosocial functioning (SAS-sr). A high GAS score at baseline was the only variable which diminished risk.
Table 2.
Prospective Predictors at 12 mo, 2 yr, 4 yr, 6 yr.
| Variable | RR | 95% C.I. | p |
|---|---|---|---|
| 12 month: increased risk | |||
| Baseline MDD | 13.23 | 3.38–51.73 | <0.001 |
| Poor social adjustment (*) | 6.08 | 1.68–21.96 | <0.01 |
| Psych. Hospitalization (!) | 2.50 | 0.94–6.61 | 0.06 |
| 12 month: decreased risk | |||
| Any OPD tx (!) | 0.28 | 0.087–0.91 | 0.03 |
| 18–24 month: increased risk | |||
| Psych Hospitalization (!) | 3.58 | 1.55–8.27 | 0.003 |
| Poor social adjustment (*) | 2.59 | 1.23–5.43 | 0.01 |
| 4 year: increased risk | |||
| Family hx of suicide | 13.8 | 2.3–84.2 | 0.005 |
| Psych Hospitalization (!) | 3.39 | 1.29–8.93 | 0.013 |
| 4 year: decreased risk | |||
| (Higher) BL GAS | 1.05 | 0.996–1.100 | 0.07 |
| 6 year: increased risk | |||
| Family hx of suicide | 11.23 | 2.01–62.61 | 0.006 |
| No OPD Treatment (!) | 3.03 | 1.19–7.68 | 0.02 |
| Low SES | 2.63 | 1.05–6.57 | 0.04 |
| Poor social adjustment (*) | 1.88 | 0.96–3.71 | 0.07 |
| 6 year: decreased risk | |||
| (High) GAS | 0.95 | 0.90–0.99 | 0.02 |
SAS-sr, (!) prior to any attempt in the interval
There have been 8 deaths since inception of the study, occurring at a mean age of 41 years, with a range of 25–59 years. As stated on death certificates, causes for the 8 deaths included: 1 suicide (by hanging), 6 accidental, and 1 natural deaths. All accidental deaths were directly or indirectly related to acute or chronic effects of substance abuse (e.g. acute drug toxicity (4), end stage liver disease from alcoholism (1), smoke inhalation (from house fire) while comatose from alcohol (e.g. blood alcohol level at autopsy was 320 mg%). One death, due to pancreatitis, was ruled “natural” but occurred in the context of chronic alcohol dependence.
Discussion
Suicide attempts occurred most frequently in the first two years of follow-up (e.g. 19% of 137 subjects in the first 12 months, 24.8% of 133 subjects by the second year). Thereafter, the number of new attempts decreased rapidly with time. Prospective predictors changed dramatically over time. In the shortest interval (12 months), attempts were predicted by MDD, an acute stressor. Thereafter, no acute clinical stressors predicted interval attempts. Both of these results may be attributable to illness severity and inpatient recruitment for nearly half of this sample. Frequency of repeat suicide attempts in the year following hospitalization for an index attempt has been reported at 17%, independent of diagnosis (29). The Collaborative Longitudinal Personality Disorders Study (CLPS), a prospective study of 4 PDs, including BPD, found that 20.5% of treatment seeking BPD patients attempted suicide during the first 2 years of study (30). Worsening of MDD predicted suicide attempts in the following month in their pooled PD sample. Suicide attempt following hospitalization, (and predicted by MDD), strongly suggests persisting depression. Similarly, illness severity, marked by psychiatric hospitalizations in the follow-up interval (but preceding any attempt), was predictive of subsequent attempt through the 4th year of follow-up. It is noteworthy that any OPD treatment in the 12 month interval diminished the suicide risk, and suggests this is due to successful treatment of MDD or decreased illness severity. Importantly, absence of OPD treatment remained a predictor of suicide risk to the 6 year follow-up.
The most consistent predictors of suicide attempts across all time intervals were measures of psychosocial and global function. Poor psychosocial function (assessed by SAS-sr) predicted increased risk of suicidal behavior at 12 months, 2 years and 6 years, while high baseline GAS was protective at 4 and 6 year intervals. By year 6, low SES was also a predictor of high risk. Poor psychosocial function at year 6 was most significant in the family, social and vocational subscales of the SAS-sr. Good social support is a known protective factor against suicide, buffering the adverse effects of negative life events, which are prominent in the lives of patients with BPD (31). Negative life events among patients in the CLPS (especially in matters of love and marriage, or crime and legal events), predicted suicidal behavior in the month during and preceding the adverse events (32). Poor baseline GAF scores and poor family relationships were among the significant predictors of poor psychosocial outcomes (low GAF scores) in BPD patients followed for 2 years in the CLPS study (33). Functional impairment in social relationships changed little in BPD patients in this time frame despite improvement in diagnostic criteria (34). The McLean Study of Adult Development found that half of BPD subjects failed to achieve social and vocational recovery at 10 year follow-up despite symptomatic remission of BPD diagnostic criteria in 93% (35). Vocational failure contributed most to poor psychosocial functioning in this study. Suicidal and self-injurious behaviors remitted early in the course of the McLean study (35); however, symptomatic improvement did not prevent poor psychosocial outcome in the long term. If the majority of BPD subjects can expect symptomatic remission in time, who dies by suicide?
Our interval attempters are characterized by low SES, low educational achievement and poor psychosocial adjustment. Across many studies, poor psychosocial function (defined by SES, social relationships, educational and vocational achievement) is a predictor of attempt behavior independent of diagnoses (5), of high lethality attempts, and suicide completion in some, though not all, studies of BPD (9), and in non-clinical populations. Community subjects with personality disorders (PD), including BPD, who complete suicide, have more problems with loss of relationships, jobs, unemployment and family compared to suicides with no PD. (9). Community subjects with BPD have lower educational and vocational achievement than subjects with other PDs, and are more likely to be receiving disability payments compared to other Axis II patients (36).
Recurrent suicidal behaviors early in the course of BPD are often characterized by impulsive, angry acts in response to acute stressors, such as perceived rejection. These are “communicative gestures,” i.e. impulsive behaviors with little lethal intent, objective planning or medical consequences. Impulsivity in BPD is significantly associated with number of suicide attempts but not degree of medical lethality (9). The McLean Study found that “manipulative suicide efforts” diminished rapidly with time, from 56.4% of subjects at year 2 to 16.4% at 6 years of follow-up, and 4.2% by year 10 (37). Completed suicide in BPD may occur after many years of illness, failed treatment, loss of supportive relationships, and social isolation. In their 27 year naturalistic follow-up study, Paris & Zweig-Frank (2001) (38) found that BPD patients who completed suicide had “burned out” their social supports and were no longer involved in active treatment. The average age at death was 37 years. This suggests that there may be a poor prognosis, high lethality subgroup of BPD patients who are at greater risk over time.
To identify subjects who had increasing degrees of medical lethality with recurrent attempts, we recently reported a trajectory analysis of Lethality Rating Scale scores in BPD subjects who had 3 or more suicide attempts. Two distinct patterns were identified: a low lethality group of subjects with recurrent but minimally lethal behaviors, and a high lethality group with increasing medical lethality scores with recurrent attempts (39). Subjects with the high lethality trajectory were characterized by inpatient recruitment (a severity marker), and poor psychosocial function, while the low lethality group had more negativism, substance use disorders, histrionic and/or narcissistic co-morbidity.
Our sample is still young (mean age 29 years) and early in the suicidal process. However, after 6 years of follow-up, low SES, poor psychosocial adjustment and absence of OPD treatment are predictors of suicidal behavior. We suggest that these are characteristics of a poor prognosis subtype. By 4 and 6 years of follow-up, a family history of suicide is a prominent risk variable. This risk factor includes heritable biological traits which increase the vulnerability to suicidal behavior. The poor prognosis subtype may include a biologic diathesis to suicidal behavior.
We did not find any predictive associations between risk factors such as impulsivity or aggression (BIS, LHA), co-morbidity with ASPD, histories of childhood maltreatment, and interval suicidal attempts, although each of these factors has been associated with suicidal behavior in BPD in cross-diagnostic studies (9). Impulsivity is a diagnostic criterion for BPD, and is associated with number of suicide attempts, but not with medical lethality. Impulsive-aggression is an endophenotypic trait of temperament, mediated by diminished central serotonergic function, and associated with suicidal behavior in BPD and across diagnoses (12). This heritable trait may be represented in our study by the family history of suicide.
Acute symptoms are unlikely to have predictive value for suicidal behavior in the long term course. The McLean study showed that acute symptoms remitted early in the course of BPD (i.e. remission rate exceeding 60% by 6 years) (37). In the CLPS, suicide attempts were predicted by childhood sexual abuse (40). Childhood sexual abuse is a known risk factor for suicidal behavior in BPD, and is associated with neurobiologic changes, including chronic dysregulation of the HPA, volume loss in areas of prefrontal cortex, hippocampus and amygdala, and diminished central serotonergic function (measured by the prolactin response to serotonergic pharmacologic challenge.) The increased frequency of suicidal behavior in sexually abused females with BPD, compared to non-abused BPD controls may be related to the effects of this altered neurobiology on behavior, including a diathesis to impulsivity, aggression, PTSD, and MDD.
Our mortality experience suggests that Substance Use Disorders (SUD), are a risk factor for premature death in subjects with BPD. Substance Use Disorders are ubiquitous in this sample (59.6%). Although the diagnosis does not distinguish interval attempters (64%) from non-attempters (57.8%), or prospectively predict suicide attempts, the mortality associated with SUD in our sample is a strong argument for early diagnosis and intervention for this co-morbid condition.
Finally, our data suggest that early OPD treatment directed at enhancing family, social and vocational functioning would decrease long term suicide risk in BPD. Current treatment modalities for BPD (e.g. DBT, pharmacotherapy) are focused on symptomatic relief. Efforts to increase overall psychosocial function may be more relevant to long term prognosis. A rehabilitation model of treatment (as in the treatment of schizophrenia) may be required to optimize outcome in BPD.
Acknowledgments
Supported by a grant from the National Institute of Mental Health (RO1 MH 048463) to Dr. Soloff
Footnotes
Paper presented at the 2011 Annual Meeting of the American Psychiatric Association, 14-18 May, 2011 Honolulu, Hawaii
Dr. Soloff and Mrs. Chiappetta report no competing interests.
References
- 1.American Psychiatric Association. Practice Guideline for the Assessment and Treatment of Patients with Suicidal Behaviors. 2003. [PubMed] [Google Scholar]
- 2.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 3.Gunderson JG, Ridolfi ME. Borderline personality disorder: suicidality and self-mutilation. Ann N Y Acad Sci. 2001;932:61–77. [PubMed] [Google Scholar]
- 4.Soloff PH, Lynch KG, Kelly TM, Malone KM, Mann JJ. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: A comparative study. Am J Psychiatry. 2000;157:601–608. doi: 10.1176/appi.ajp.157.4.601. [DOI] [PubMed] [Google Scholar]
- 5.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 6.Isomesta ET, Henriksson MM, Heikkinen ME, Aro HM, Marttunen MJ, Kuoppasalmi KI, Lonnqvist JK. Suicide among subjects with personality disorders. Am J Psychiatry. 1996;153:667–673. doi: 10.1176/ajp.153.5.667. [DOI] [PubMed] [Google Scholar]
- 7.Runeson B. Mental disorder in youth suicide. Acta Psychiatr Scand. 1989;79:490–497. doi: 10.1111/j.1600-0447.1989.tb10292.x. [DOI] [PubMed] [Google Scholar]
- 8.Soderberg S. Personality disorders in parasuicide. Nordic Journal of Psychiatry. 2001;55:163–167. doi: 10.1080/08039480152036038. [DOI] [PubMed] [Google Scholar]
- 9.Soloff PH. Risk factors for suicidal behavior in borderline personality disorder: a review and update. In: Zanarini MC, editor. Borderline Personality Disorder. Boca Raton, Fl: Taylor & Francis; 2005. pp. 333–365. [Google Scholar]
- 10.Maris RW, Berman AL, Silverman MM. Comprehensive Textbook of Suicidology. New York: The Guilford Press; 2000. p. 19. [Google Scholar]
- 11.Leon AC, Friedman RA, Sweeney JA, Brown RP, Mann JJ. Statistical issues in the identification of risk factors for suicidal behavior: the application of survival analysis. Psychiatry Res. 1990;31:99–108. doi: 10.1016/0165-1781(90)90112-i. [DOI] [PubMed] [Google Scholar]
- 12.Mann JJ. Neurobiology of suicidal behavior. Nat Rev Neurosci. 2003;4:819–827. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 13.Soloff PH, Fabio A. Prospective predictors of suicide attempts in borderline personality disorder at one, two, and two-to-five year follow-up. J Pers Disord. 2008;22(2):123–134. doi: 10.1521/pedi.2008.22.2.123. [DOI] [PubMed] [Google Scholar]
- 14.Spitzer RL, Williams JBW, Gibbon M, First MB. Instruction manual for the structured clinical interview for DSM-III-R. New York: Biometrics Research Department, New York State Psychiatric Inst; 1988. [Google Scholar]
- 15.Loranger AW, Janca A, Sartorius N. Assessment and diagnosis of personality disorder: the ICD-10 international personality disorder examination (IPDE) Cambridge: Cambridge University Press; 1997. [Google Scholar]
- 16.Gunderson JG, Kolb JE, Austin V. The diagnostic interview for borderlines. Am J Psychiatry. 1981;38:896–903. doi: 10.1176/ajp.138.7.896. [DOI] [PubMed] [Google Scholar]
- 17.Zanarini M, Gunderson JG, Frankenburg FR, Chauncey DL. The revised diagnostic interview for borderlines: discriminating BPD from other Axis II disorders. J Pers Disor. 1989;3(1):10–18. [Google Scholar]
- 18.Oquendo MA, Halberstam B, Mann JJ. Risk factors for suicidal behavior. Review of Psychiatry. 2003;22:103–129. [Google Scholar]
- 19.Beck AT, Schuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnick HLP, Lettiem D, editors. The Prediction of Suicide. Bowie, MD: Charles Press; 1974. pp. 45–56. [Google Scholar]
- 20.Beck AT, Ward CH, Mendelson M, Mosk J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 21.Guy W. ECDEU Assessment Manual of Psychopharmacology-Revised (DHEW Publ. No ADM 76–338) Rockville, MD: U.S. Department of Health Education and Welfare, Public Health Service, Alcohol, Drug Abuse and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976. [Google Scholar]
- 22.Beck AT, Steer RA. Manual for the Beck Hopelessness Scale. San Antonio, TX: Psychological Corp; 1988. [Google Scholar]
- 23.Spitzer RL, Gibbon M, Endicott J. The Global Assessment Scale: A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- 24.Barratt ES. Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep. 1965;16:547–554. doi: 10.2466/pr0.1965.16.2.547. [DOI] [PubMed] [Google Scholar]
- 25.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Clin Psychol. 1959;21:343–349. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- 26.Brown GL, Goodwin FK. Cerebrospinal fluid correlates of suicide attempts and aggression. Ann N Y Acad Sci. 1986;487:175–188. doi: 10.1111/j.1749-6632.1986.tb27897.x. [DOI] [PubMed] [Google Scholar]
- 27.Hathaway SR, Mehl PE. The Atlas for the Clinical Use of the MMPI. Minneapolis, MN: University of Minnesota Press; 1951. [Google Scholar]
- 28.Weissman MM, Bothwell S. Assessment of social adjustment by patient self report. Arch Gen Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 29.Cedereke M, Ojehagen A. Prediction of repeat parasuicide after 1–12 months. Eur Psychiatry. 2005;20:101–109. doi: 10.1016/j.eurpsy.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Yen S, Shea MT, Pagano M, Sanislow CA, Grilo CM, McGlashan TH, Skodol AE, Bender DS, Zanarini MC, Gunderson JG, Morey LC. Axis I and Axis II disorders as predictors of prospective suicide attempts: findings from the Collaborative Longitudinal Personality Disorders Study. J Abnorm Psychol. 2003;112(3):375–381. doi: 10.1037/0021-843x.112.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pagano ME, Skodol AE, Stout RL, Shea MT, Yen S, Grilo CM, Sanislow CA, Bender DS, McGlashan TH, Zanarini MC, Gunderson JG. Stressful life events as predictors of functioning: Findings from the Collaborative Longitudinal Personality Disorders Study. Acta Psychiatr Scand. 2004;110:421–429. doi: 10.1111/j.1600-0447.2004.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yen S, Shea MT, Pagano ME, Shea TM, Grilo CM, Gunderson JG, Skodol AE, McGlashan TH, Sanislow CA, Bender DS, Zanarini MC. Recent life events preceding suicide attempts in a personality disorder sample: findings from the Collaborative Longitudinal Personality Disorders Study. J Consult Clin Psychol. 2005;73:99–105. doi: 10.1037/0022-006X.73.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gunderson JG, Daversa MT, Grilo CM, McGlashen TH, Zanarini MC, Shea MT, Skodol AE, Yen S, Sanislow CA. Predictors of 2 year outcome for patients with borderline personality disorder. Am J Psychiatry. 2006;163:822–826. doi: 10.1176/ajp.2006.163.5.822. [DOI] [PubMed] [Google Scholar]
- 34.Skodol AE, Pagano ME, Bender DS, Shea TM, Gunderson JG, Yen S, Stout RL, Morey LC, Sanislow CA, Grilo CM, Zanarini MC, McGlashan TH. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med. 2004;35:443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10 year prospective follow-up study. Am J Psychiatry. 2010;167:663–667. doi: 10.1176/appi.ajp.2009.09081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zanarini MC, Frankenburg FR, Hennen J, Reich B, Silk KR. Psychosocial functioning of borderline patients and Axis II comparison subjects followed prospectively for six years. J Pers Disord. 2005;19:19–29. doi: 10.1521/pedi.19.1.19.62178. [DOI] [PubMed] [Google Scholar]
- 37.Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: a 10 year follow-up study. Am J Psychiatry. 2007;164:929–935. doi: 10.1176/ajp.2007.164.6.929. [DOI] [PubMed] [Google Scholar]
- 38.Paris J, Zweig-Frank H. A 27 year follow-up of patients with borderline personality disorder. Compr Psychiatry. 2001;42:482–487. doi: 10.1053/comp.2001.26271. [DOI] [PubMed] [Google Scholar]
- 39.Soloff PH, Chiappetta L. Subtyping borderline personality disorder by suicidal behavior. J Pers Disord. doi: 10.1521/pedi.2012.26.3.468. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, McGlashan TH, Zanarini MC, Morey LC. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. Am J Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]