Abstract
Background/Aims
Gastroesophageal reflux (GER) has been implicated in the pathogenesis of chronic cough. The aims of this study were to evaluate the diagnostic usefulness of multichannel intraluminal impedance combined with pH monitoring (MII/pH monitoring) in patients with suspected symptoms of gastroesophageal reflux disease (GERD) and to assess the correlation between GER symptoms and reflux nature.
Methods
Seventy patients with suspected symptoms of GERD (such as heartburn, acid regurgitation, non-cardiac chest pain, globus and chronic cough) were enrolled. All patients were asked to discontinue medications that would influence esophageal motor function and gastric acid secretion at least one week ago. All subjects underwent MII/pH monitoring.
Results
Forty-five patients (64.3%) were diagnosed with GERD. Among these patients, eleven patients (15.7%) had pathologic acid reflux by pH data and thirty-four patients (48.6%) had pathologic bolus exposure by impedance. Subjects with chronic cough had a higher DeMeester score (p=0.009), percentage of acid exposure time (p=0.007), acid bolus exposure % time (p=0.027), distal acid reflux episodes (p=0.015) and proximal acid reflux episodes (p=0.030) than subjects without chronic cough.
Conclusions
The results of this study showed that the impedance monitoring enhanced diagnostic sensitivity than pH-monitoring alone by 48.6%. In addition, reflux episodes at the distal and proximal esophagus were noted to be important factors associated with chronic cough.
Keywords: Gastroesophageal reflux, Cough, Impedance
INTRODUCTION
Gastroesophageal reflux disease (GERD) has a high prevalence and an increasing incidence. In Western societies, 10% to 20% of the adult population have symptoms of GERD.1,2 Although the frequency of GERD is lower,3,4 the prevalence of GERD is recently is increasing in Asian countries including Korea.5 Apart from the typical symptoms such as heartburn and acid regurgitation, and the atypical or extraesophageal symptoms such as chronic cough, globus sensation in the throat and hoarseness are thought to be caused by pathological reflux of gastric content into the esophagus.6
The significance of the diagnosis and the treatment of atypical manifestations of GERD is still a matter of debate. The assessment of response to empirical treatment with proton pump inhibitors (PPIs) is often the first option of diagnosis. However, patients with atypical gastroesophageal reflux (GER) symptoms usually have a lower response to double dose PPI therapy.7,8
Traditionally, 24-hour ambulatory pH monitoring has been recognized as a standard diagnostic test for GERD. Currently, multichannel intraluminal impedance combined with pH monitoring (MII/pH-monitoring) is considered as the most sensitive tool for the diagnosis and characterization of GERD.9-11 This procedure is used to determine the quantity and quality of weakly alkaline and weakly acidic reflux episodes, apart from acidic reflux events, by the exact determination of the exposure time and the proximal extent of the refluxates.10
The aims of this study were to evaluate the diagnostic usefulness of MII/pH-monitoring in patients with suspected symptoms of GERD and to assess the correlation between GERD symptoms and reflux nature.
MATERIALS AND METHODS
1. Subjects
We performed a prospective study of 70 patients with suspected GERD symptoms who referred to Chonnam National University Hospital between March 2009 and March 2011. The exclusion criteria were subjects with a history of thoracic, esophageal, or gastric surgery; those with primary and/or secondary severe esophageal motility disorders (e.g., achalasia, scleroderma, autonomic or peripheral neuropathy and myopathy); pregnant women; and those with a history of alcohol or drug abuse. Patients were asked to discontinue any medication that would influence esophageal motor function and gastric acid excretion (such as H2 receptor antagonists, PPIs) at least one week before the MII/pH monitoring. The typical GERD symptoms included heartburn and acid regurgitation; atypical GERD symptoms included non-cardiac chest pain (NCCP), globus and chronic cough. Subjects with a chronic cough, not associated with asthma, had a cough lasting longer than 8 weeks, normal spirometry, and a negative methacholine challenge test. The subjects were asked to complete the questionnaires consisted of questions about the patient's symptoms. The questionnaires included severities, durations and frequencies of reflux related symptoms (heart burn, acid regurgitation, chest pain, hoarseness, globus sensation and cough). The severities of reflux related symptoms were recorded by 10 cm visual analogue scales running from 0 (no symptom) to 10 (maximal symptom expression). This study was approved by the Institutional Review Board at Chonnam National University Hospital. All patients provided written informed consent.
2. Esophageal impedance/pH-monitoring
1) MII/pH-monitoring
The MII/pH probe consists of a 2.3 mm polyurethane catheter incorporating six impedance segments (each segment 2 cm long) and one pH-measuring electrode (Sandhill Scientific Inc., Denver, CO, USA). The configuration of this catheter allowed the recording of changes in the intraluminal impedance at 3, 5, 7, 9, 15, and 17 cm above the lower esophageal sphincter (LES). In addition, the pH was monitored at 5 cm above the LES. After defining the LES by using conventional manometry. The MII/pH probe was inserted transnasally and the distal pH probe was positioned 5 cm above the LES. Data from the impedance channels and the pH electrodes were transmitted at frequency of 50 Hz and stored on a portable data recorder (Sleuth; Sandhill Scientific Inc., Highlands Ranch, CO, USA). After 24-hours of recording, data was uploaded onto a personal computer and analyzed by using commercially available software system (Bioview Analysis; Sandhill Scientific Inc., Highlands Ranch, CO, USA). During the recording period, patients were encouraged to participate in regular activities and have routine meals: they were given a personal diary to note meal times, time in the recumrecumbent position, and the timing of any GERD-related symptoms.
2) pH data analysis
Acid reflux episodes were defined as a drop in pH to less than 4 for at least 5 seconds. The acid exposure percent time was calculated as the total time of the acid reflux episodes divided by the monitoring time. The DeMeester score, widely used to evaluate acid reflux, was obtained using 6 different parameters: 1) total percent of time when the pH was <4.0, 2) percent time when the pH was <4.0 during the upright period, 3) percent time when pH was <4.0 during the recumbent period, 4) the total number of acid reflux episodes, 5) the total number of acid reflux episodes longer than 5 minutes, and 6) the duration of the longest acid reflux episodes.12
3) Analysis of MII data
The meal periods were excluded from the analysis. These reflux episodes were classified as acidic if the pH dropped below 4 or as non-acidic if the pH remained above 4 during the episode. A proximal reflux event was considered when the refluxate reached 15 cm of the impedance sensor. The acid exposure percent time was calculated as the total time of acid reflux episodes divided by the monitoring time. The bolus exposure percent time was defined as the sum of the bolus clearance time, of all individual reflux episodes, divided by the monitoring time. The bolus clearance time was defined as the time from a drop in impedance to 50% of the baseline value to recovery of 50% of the baseline value at the most distal impedance channel. The MII/pH monitoring data was analyzed except for reflux episodes that were followed by cough (cough-reflux sequence). The acid exposure percent time of the distal pH probe >4.0% or a DeMeester score >14.7 was defined as acid GERD. The bolus exposure percent time of more than 1.4% without acid GERD was diagnosed as nonacid GERD.
3. Statistical methods
All continuous variables are presented as the median (range) or mean±SD and the proportions expressed as numbers (%). The independent sample t-test, Mann-Whitney U test and chi-square test were used for data analysis. The computer software used for statistical analysis was IBM SPSS version 18.0 (IBM, New York, NY, USA). A p-value of <0.05 was considered statistically significant.
RESULTS
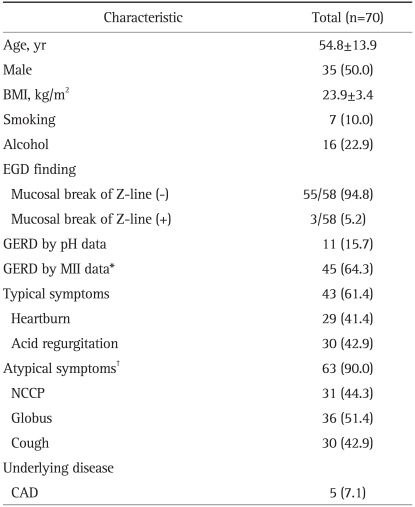
Table 1 summarizes the characteristics of the enrolled subjects. Mean age of subjects was 54.8±13.9 years. There were 35 males (50.0%) and the mean body mass index was 23.9±3.4 kg/m2. There were 43 subjects (61.4%) with typical GER symptoms such as heartburn or acid regurgitation. Sixty-three subjects (90.0%) had atypical GER symptoms such as NCCP, globus and a chronic cough. And thirty-six subjects (51.4%) had both typical & atypical symptoms. The examination was well tolerated by all subjects.
Table 1.
Patient Characteristics
Data are presented as mean±SD or number (%).
BMI, body mass index; EGD, esophagogastroduodenoscopy; GERD, gastroesophageal reflux disease; NCCP, non-cardiac chest pain; CAD, coronary arterial disease.
*The patients who were diagnosed as GERD by impedance (pathologic bolus exposure); †Among the 63 patients, 36 patients had both typical and atypical symptoms.
1. Results of MII/pH-monitoring
1) Result of pH data
Eleven out of 70 (15.7%) subjects had diagnosed as pathologic acid reflux because their percent time pH <4.0 was over 4.0% or DeMeester score was over 14.7 point.
2) Result of MII data
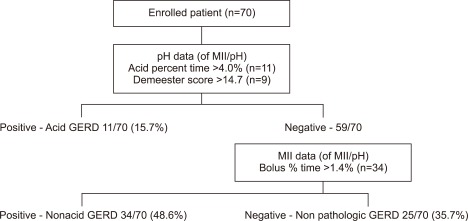
Among 59 subjects that had negative result by pH data, 34 subjects had the result that total bolus reflux percent time was over 1.4%. These subjects were additionally diagnosed with nonacid GERD (Fig. 1).
Fig. 1.
Diagnostic usefulness of MII/pH-monitoring. Forty-five patients (64.3%) are diagnosed with gastroesophageal reflux disease (GERD). Among these patients, 11 patients (15.7%) have acid reflux and 34 patients (48.6%) had non-acid reflux.
2. Clinical characteristics and MII/pH values in subjects with each GER symptoms
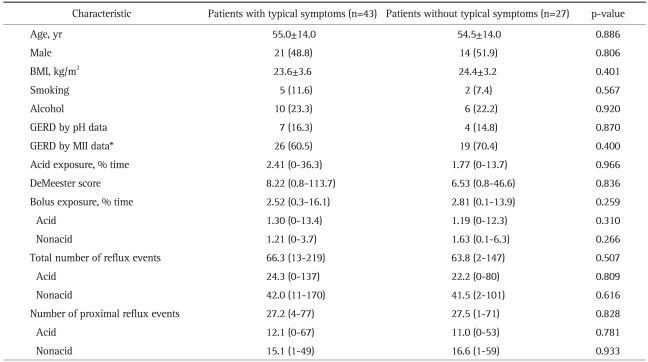
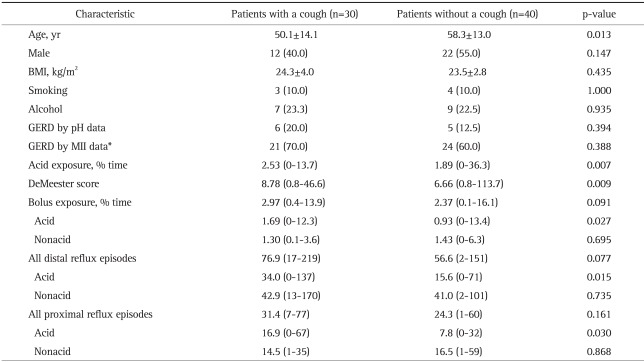
Table 2 shows the clinical characteristics and MII/pH values of subjects with typical GER symptoms and without typical GER symptoms. There was no significant difference in the results of MII/pH values between subjects with typical GER symptoms and subjects without typical GER symptoms. There was no significant difference in the results of the MII/pH values between subjects with NCCP and subjects without NCCP. In addition, there was no significant difference in the results of the MII/pH between patients with globus and patients without globus. However, the subjects with chronic cough had higher DeMeester score, acid exposure percent time, acid bolus exposure percent time, distal acid reflux episodes and proximal acid reflux episodes than patients without chronic cough (p<0.05) (Table 3).
Table 2.
Comparison of Clinical Characteristics and Impedance Data between the Patients with Typical Gastroesophageal Reflux (GER) Symptoms and Patients without Typical GER Symptoms
Data are presented as mean±SD or number (%).
BMI, body mass index; GERD, gastroesophageal reflux disease.
*GERD by MII data, the patients who were diagnosed as GERD by impedance (pathologic bolus exposure).
Table 3.
Comparison of Clinical Characteristics and Impedance Data between the Patients with Chronic Cough and Patients without Chronic Cough
Data are presented as mean±SD or number (%).
BMI, body mass index; GERD, gastroesophageal reflux disease.
*GERD by MII data, the patients who were diagnosed as GERD by impedance (pathologic bolus exposure).
DISCUSSION
The combined MII/pH-monitoring is considered as the most sensitive tool for assessing all types of GER (acidic, weakly acidic and weakly alkaline), their composition, proximal extent, duration and clearing.11,13 In this study, 45 patients (64.3%) of the enrolled subjects were diagnosed as GERD by MII/pH-monitoring. Thirty-four patients of them would have been interpreted as having negative findings if tested only by means of conventional pH monitoring. These findings showed the diagnostic usefulness of MII/pH-monitoring in the patients with suspected GERD.
The diagnosis of reflux in patients with atypical symptoms and the establishment of a clear relationship between reflux and atypical GER symptoms can be challenging. Bajbouj et al.14 reported that 63.4% of 'off-PPI' patients with atypical GER symptoms had pathological GER and 61% of patients were diagnosed with GERD by MII/pH-monitoring. Mallhotra et al.15 evaluated patients with suspected extraesophageal GERD who were on or off PPI therapy, and concluded that MII/pH-monitoring was useful for ruling out GERD and redirecting the management of patients. Unlike typical GER symptoms, which often respond well to conventional doses of PPI therapy, atypical GER symptoms require longer periods of therapy and/or higher doses. However, despite the aggressive antisecretory regimens the symptoms often responded poorly. Some studies with MII/pH-monitoring have demonstrated that nonacid reflux persists during PPI therapy.16 Weak acid reflux (pH 4 to 7) may induce symptoms of GERD such as heartburn, regurgitation, and noncardiac chest pain. In the present study, the subjects with chronic cough had more acid reflux episodes at the distal esophagus than subjects without chronic cough. In addition, the results of this study showed that the frequency of acid reflux episodes at the proximal esophagus was significantly higher in the subjects with chronic cough compared to the subjects without chronic cough. Acid reflux is thought to be a common cause of chronic cough, and esophageal instillation of acidic solutions may increase symptoms in selected patients with chronic cough and abnormal pH-monitoring.17 A recent study in GERD-confirmed patients demonstrated that whilst infusion of acid (compared to saline) into the esophagus of those without cough had no effect, the cough reflex becomes significantly sensitized to capsaicin in those with chronic cough.18 However, the results of this study showed the frequency of nonacid reflux episodes at the distal esophagus and proximal esophagus was not different between two groups. The possibility that nonacid reflux events may be important in chronic cough was highlighted by Irwin et al.19 who reported improvements in chronic cough after laparoscopic fundoplication in patients where acid suppression had failed. However, most studies performed to date in patients with chronic cough have not found an increased number of reflux events compared to studies in healthy volunteers but relied on temporal associations between cough and reflux events to suggest a causal relationship.20 And, the control group of this study was not the healthy controls but the subjects with suspected symptoms of GERD except cough. So, this study did not show the difference of the frequency of nonacid reflux.
The limitation of this study included the following; the data did not show the symptom index and symptom association probability. Most studies defined GERD using the symptom index or symptom association probability. Of course, it is important to evaluate whether the symptoms are caused by reflux or not. However, atypical GER symptoms usually persist and do not have a sudden onset easily recognized by the patient.14,21 This characteristic makes it difficult to mark a reflux event at a single point in time; the difficulty of assessment using the symptom index in patients with atypical symptoms makes the diagnosis of GERD with atypical symptoms more confusing than in cases with typical GERD. And also, we could not demonstrate the strict temporal relationship between reflux events documented by MII/pH-monitoring and episodes of cough. Previous studies showed that 23% to 56% had a significant temporal correlation between coughing spells and reflux during MII/pH-monitoring.22
In conclusion, the results of this study showed the diagnostic usefulness of MII/pH-monitoring in patients with suspected GERD. In addition, reflux episodes at the distal and proximal esophagus are important factors associated with chronic cough. Further studies based on large-scale population are needed to provide normal values of MII/pH-monitoring in Asian and more accurate assessment of a causal link between pathological GER and atypical symptoms should be developed.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R Globale Konsensusgruppe. The Montreal definition and classification of gastroesophageal reflux disease: a global, evidence-based consensus paper. Z Gastroenterol. 2007;45:1125–1140. doi: 10.1055/s-2007-963633. [DOI] [PubMed] [Google Scholar]
- 2.Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Serag HB. Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2007;5:17–26. doi: 10.1016/j.cgh.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 4.Wong BC, Kinoshita Y. Systematic review on epidemiology of gastroesophageal reflux disease in Asia. Clin Gastroenterol Hepatol. 2006;4:398–407. doi: 10.1016/j.cgh.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Jung HK. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil. 2011;17:14–27. doi: 10.5056/jnm.2011.17.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford CN. Evaluation and management of laryngopharyngeal reflux. JAMA. 2005;294:1534–1540. doi: 10.1001/jama.294.12.1534. [DOI] [PubMed] [Google Scholar]
- 7.Vaezi MF, Richter JE, Stasney CR, et al. Treatment of chronic posterior laryngitis with esomeprazole. Laryngoscope. 2006;116:254–260. doi: 10.1097/01.mlg.0000192173.00498.ba. [DOI] [PubMed] [Google Scholar]
- 8.Steward DL, Wilson KM, Kelly DH, et al. Proton pump inhibitor therapy for chronic laryngo-pharyngitis: a randomized placebo-control trial. Otolaryngol Head Neck Surg. 2004;131:342–350. doi: 10.1016/j.otohns.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 9.Lee BE, Kim GH, Ryu DY, et al. Combined dual channel impedance/pH-metry in patients with suspected laryngopharyngeal reflux. J Neurogastroenterol Motil. 2010;16:157–165. doi: 10.5056/jnm.2010.16.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anandasabapathy S, Jaffin BW. Multichannel intraluminal impedance in the evaluation of patients with persistent globus on proton pump inhibitor therapy. Ann Otol Rhinol Laryngol. 2006;115:563–570. doi: 10.1177/000348940611500801. [DOI] [PubMed] [Google Scholar]
- 11.Cho YK, Kim GH, Kim JH, Jung HY, Lee JS, Kim NY. Diagnosis of gastroesophageal reflux disease: a systematic review. Korean J Gastroenterol. 2010;55:279–295. doi: 10.4166/kjg.2010.55.5.279. [DOI] [PubMed] [Google Scholar]
- 12.Johnson LF, DeMeester TR. Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol. 1986;8(Suppl 1):52–58. doi: 10.1097/00004836-198606001-00008. [DOI] [PubMed] [Google Scholar]
- 13.Cho YK. How to interpret esophageal impedance pH monitoring. J Neurogastroenterol Motil. 2010;16:327–330. doi: 10.5056/jnm.2010.16.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bajbouj M, Becker V, Neuber M, Schmid RM, Meining A. Combined pH-metry/impedance monitoring increases the diagnostic yield in patients with atypical gastroesophageal reflux symptoms. Digestion. 2007;76:223–228. doi: 10.1159/000112728. [DOI] [PubMed] [Google Scholar]
- 15.Malhotra A, Freston JW, Aziz K. Use of pH-impedance testing to evaluate patients with suspected extraesophageal manifestations of gastroesophageal reflux disease. J Clin Gastroenterol. 2008;42:271–278. doi: 10.1097/MCG.0b013e31802b64f3. [DOI] [PubMed] [Google Scholar]
- 16.Tamhankar AP, Peters JH, Portale G, et al. Omeprazole does not reduce gastroesophageal reflux: new insights using multichannel intraluminal impedance technology. J Gastrointest Surg. 2004;8:890–897. doi: 10.1016/j.gassur.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449–454. doi: 10.1136/gut.2004.055418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Javorkova N, Varechova S, Pecova R, et al. Acidification of the oesophagus acutely increases the cough sensitivity in patients with gastro-oesophageal reflux and chronic cough. Neurogastroenterol Motil. 2008;20:119–124. doi: 10.1111/j.1365-2982.2007.01020.x. [DOI] [PubMed] [Google Scholar]
- 19.Irwin RS, Zawacki JK, Wilson MM, French CT, Callery MP. Chronic cough due to gastroesophageal reflux disease: failure to resolve despite total/near-total elimination of esophageal acid. Chest. 2002;121:1132–1140. doi: 10.1378/chest.121.4.1132. [DOI] [PubMed] [Google Scholar]
- 20.Smith J, Woodcock A, Houghton L. New developments in reflux-associated cough. Lung. 2010;188(Suppl 1):S81–S86. doi: 10.1007/s00408-009-9210-2. [DOI] [PubMed] [Google Scholar]
- 21.Zerbib F, Stoll D. Management of laryngopharyngeal reflux: an unmet medical need. Neurogastroenterol Motil. 2010;22:109–112. doi: 10.1111/j.1365-2982.2009.01437.x. [DOI] [PubMed] [Google Scholar]
- 22.Smith JA, Decalmer S, Kelsall A, et al. Acoustic cough-reflux associations in chronic cough: potential triggers and mechanisms. Gastroenterology. 2010;139:754–762. doi: 10.1053/j.gastro.2010.06.050. [DOI] [PubMed] [Google Scholar]