Abstract
Background:
Injuries from occupational accidents are associ-ated with agents of biological risk, as they are the gateway to serious and potentially lethal infectious diseases that can be spread by contact between people. Several studies have demonstrated that dental students are among the most vulnerable to blood-borne exposure.
Objectives:
To assess the knowledge, attitude and practice regarding risk of HIV transmission through accidental needlestick injury amongst dental students and providing supportive and proper guidelines regarding needlestick injuries and HIV infection.
Study design:
This was a cross-sectional study done at a dental college attached to a tertiary care hospital, which included third, fourth year students and interns. The results obtained were subjected to statistical analysis using Chi-square test.
Results:
Of the 120 students, 13 (11%) were not even aware that virus could be transmitted through infected needle. A significant proportion of the third year students i.e. 27 (67.5%) were not aware of correct method of disposal of disposable needles and syringes as against interns 17 (42.5%). Around 31 (26%) said that they would promote active bleeding at the site of injury and 37 (30%) said they would take post-exposure prophylaxis.
Conclusion:
Dental professionals are at a risk of occupational acquisition of HIV primarily due to accidental exposure to infected blood and body fluids. There is a need of correcting the existing misconceptions through education programs early in the course and providing supportive and proper guidelines regarding needlestick injuries and HIV infection.
Keywords: HIV transmission, needlestick injury, post exposure propphylaxix
INTRODUCTION
One of the most serious threats dental students face during their clinical training is the possibility of exposure to blood-borne pathogens, with the attendant risk of HIV. Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment. These injuries can occur at any time when people use, disassemble, or dispose of needles.[1] When not disposed of properly, needles can become concealed in linen or garbage and injure other workers who encounter them unexpectedly. AIDS is making new demands on the health service and the competence of health workers. Dental students are exposed to various oral infections or lesions, which may be due to manifestations of AIDS. Dental students share this responsibility especially in the overcrowded hospitals, where they have to perform tooth extractions commonly and dispose/destroy the used needle or syringe.[2]
The risk of accidental needlestick injuries are more during invasive procedure such as giving injection (nerve blocks) and recapping the needle after use. There is confusion regarding correct responses to such accidents both at the administrative levels where policy decisions for institutions are to be made as well as amongst the dental staff and students themselves who are not aware the preventive aspects and of the immediate prophylactic steps to be taken in case of such accidents.[2,3] There should be a well-formulated coordinated approach for the provision of information support, and referral from healthcare workers who sustain occupationally related management of occupational exposures varies between institutions and often reflects the level of staff education and previous experience in areas of infection control and transmission of blood-borne diseases. Despite published guidelines and training programs, needlestick injuries remain an ongoing problem.
Thus the aim of the present study was to assess the knowledge, attitude and practice regarding the risk of HIV infection among dental students after an accidental needlestick injury and to make relevant suggestions.
MATERIAL AND METHODS
There were 120 students attending the dental clinics at our institution. Of these 40, 40 and 40 were in third year, fourth year and Interns, respectively. These students were selected as they are exposed to blood and blood-borne pathogens during their clinical training programs. A cross-sectional study was done amongst the third, fourth year and interns at AME's Dental College Hospital and Research Centre, Raichur, during the academic year of 2010–11 from January 6, 2011 to April 17, 2011. A semi-open self-administered questionnaire with questions pertaining to knowledge, attitude and practice of risk of HIV transmission after needlestick injury was used and the results were subjected to statistical analysis using Chi-square test using SPSS 17.0 version software. To compare the knowledge, attitude and practice among students p < 0.05 was set as statistical significance.
RESULTS
The questionnaires were distributed to all 120 students and the rate of response was 100%. The mean age of students was 19.6±2 years. Of the 120 students, 13 (11%) were not even aware that virus could be transmitted through infected needles; among them 22.5% were third year students. In the present study, 107 (89%) students were aware of possibility of transmission of HIV through infected needles [Table 1, Graph 1].
Table 1.
Knowledge regarding transmission through infected needle
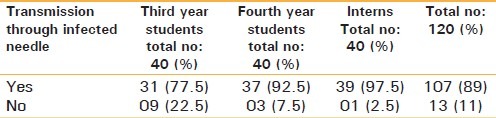
Graph 1.
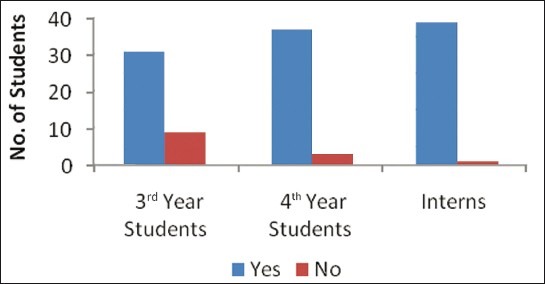
Knowledge regarding transmission through infected needle
In all 26 (22%) said they would recap the used needles, 53 (44%) said they would destroy the needle using needle destroyer, 18 (15%) said they would destroy in puncture-resistant container with disinfectant, 15 (12.5%) said they would throw the needle directly into the dustbin and 8 (7%) said they would bend the needle and through into dustbin [Table 2, Graph 2].
Table 2.
Knowledge and awareness regarding methods of disposal of disposable needles and syringes
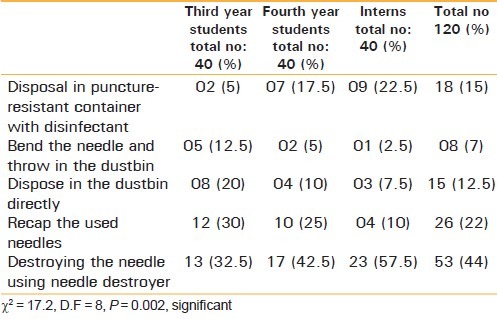
Graph 2.
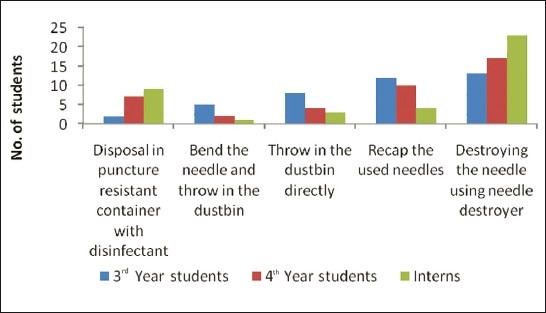
Knowledge and awareness regarding methods of disposal of disposable needles and syringes
When enquired as to what they would do after an accidental needlestick injury, 37 (30%) said they would take post-exposure prophylaxis, 31 (26%) said they would wash the site of injury with surgical spirit or sterilium. Thirty one (26%) said they would promote active bleeding at the site of injury, 14 (12%) said they would wash the site of injury thoroughly with soap and running water and 7 (6%) said they would check HIV status of the patient [Table 3, Graph 3].
Table 3.
Precautions taken after accidental needlestick injury
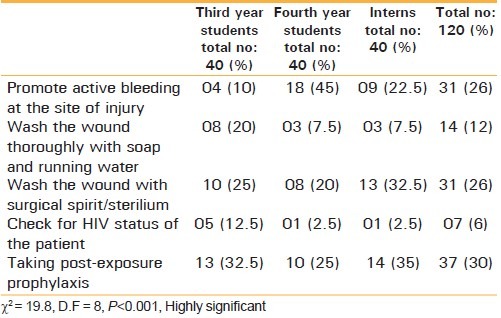
Graph 3.
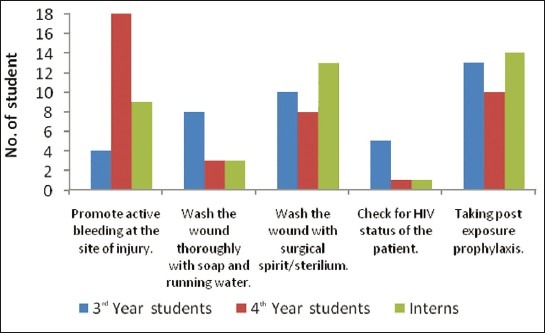
Precautions taken after accidental needlestick injury
DISCUSSION
Needlestick injuries transmit infectious diseases, especially blood-borne viruses. In recent years, concern about AIDS (Acquired Immunodeficiency Syndrome), hepatitis B and hepatitis C has prompted research to find out why these injuries occur and to develop measures to prevent them.[1,2]
Occupational exposure rates have been ex-pressed in terms of examinations for all dental care, persons per year, procedures, and other variations. This may hamper comparisons between results, but allows the evaluation of tendencies. Different studies may include undergraduates, postgraduates, and/or the entire team of professionals in the dental field. The rates found in the present study of 9/10 000 re-ports of percutaneous exposure in relation to the num-ber of procedures performed (83 reports for 93 892 procedures) and 12.8/10 000 consultations (eighty-three reports in 64 414 examinations for all dental care) are similar to findings in a prospective observational study carried out by Cleveland et al. Divergences with other results can be attributed to the methodology employed, as well as other factors. Lower rates were observed in studies based only upon reported accidents, which did not represent the totality of occupational exposure, such as findings by Ramos-Gomez et al. (3.53/10 000 consultations),[1] and Callan et al. (5.24/10 000 consultations).[2] The influ-ence of underreporting has also been demonstrated in studies by Younai et al. and Kotelchuck et al., car-ried out at the same dental school in New York.[2] Despite published guidelines and training programs, needlestick injuries remain an ongoing problem. AIDS imposes on the dental students as lot of stress is associated with a sense of professional and personal inadequacy and fear of becoming infected.[3]
Studies have reported that HIV infection can be acquired through occupational injury during intervention on HIV infected patient. The HIV sequences of the doctor and patient were encoded, analyzed and compared and found to be closely related.[3] Based on data from over 5100 exposures from 26 studies worldwide, the centre for disease control and prevention estimate that the overall risk of infection from accidental exposure is 0.3% if exposure is parental, 0.1% if via mucous membrane. In another study amongst the healthcare workers from over 300 healthcare institutions, the risk of seroconversion following parenteral exposure consistently remained less than 1%.[3]
There are many misconceptions about the risk of transmission through infected needles that need to be corrected. The risk of HIV transmission through accidental needlesticks injury does exist through the risk is low.[4] Universal biosafety precautions if strictly adhered to while working in a healthcare setting reduces the risks further. As per WHO recommendations, needles should not be recapped, bent, broken, removed from disposable syringes or otherwise manipulated by hand as these procedure increase the risk of needlestick injuries.[5,6] These practices should be stopped by introducing educational programs for enhancing the knowledge and skills of the dental students early in the course. As the students lack the necessary skills and training, they may be at more risks of accidental injuries. Hence making them aware of the protective steps and relevant institutional policies regarding such episodes is a necessity.
In comparing reports of occupational exposure and reporting rates among dental students at a U.S. dental school, Peres et al. stated the evident com-bination of some not-yet-fully understood factors intercede between clinical events, identification, and management in the post-exposure protocol established by the school. According to these authors, the psychological constructs that involve the “fear of occupational exposure” and the personal interpreta-tion of the significance of occupational exposure are probably among the factors that influence the belief in reporting.[7]
While the level of occupational risk is low, the consequences of infection with HIV are dire and should not be underrated. Infected healthcare workers have received little support from the profession and the media. There is no effective vaccine available as yet. Through chemoprophylaxis for healthcare workers after accidental HIV exposure is now recommended by international AIDS society, they are not within the reach of many institution.[8] Hence there is a need to improve the knowledge of dental students regarding the risks, the universal biosafety precautions and appropriate responses to accidental injuries early in their course. Including the relevant information in their curriculum could be an important intervention.
There was substantial improvement in compliance with universal precautions in an emergency department following institution of a policy. Healthcare workers who receive injuries need to have confidence that by immediately reporting the injury they will receive appropriate advice and treatment as well as support and encouragement.[9] Thus it is of utmost importance that each institution should have a clear cut and uniform policy regarding prevention of such accidents and the correct steps to be taken after such an episode in the form of referral services. Counseling, chemoprophylactic drugs etc.[10] All healthcare workers should be made aware of these policy and necessary supportive services provided for its implementation.
ACKNOWLEDGEMENT
We thank Dr. Hasan Yakub and all the students of AME'S Dental College Hospital and Research Centre for their participation in the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Ramos-Gomez F, Ellison J, Greenspan D, Bird W, Lowe S, Gerberding JL. Accidental exposures to blood and body fluids among health care workers in dental teaching clinics: A prospective study. J Am Dent Assoc. 1997;128:1253–61. doi: 10.14219/jada.archive.1997.0402. [DOI] [PubMed] [Google Scholar]
- 2.Callan RS, Caughman F, Budd ML. Injury reports in a dental school: A two-year overview. J Dent Educ. 2006;70:1089–97. [PubMed] [Google Scholar]
- 3.Kotelchuck D, Murphy D, Younai F. Impact of underreporting on the management of occupational bloodborne exposures in a dental teaching environment. J Dent Educ. 2004;68:614–22. [PubMed] [Google Scholar]
- 4.Rowe PM. New Guidelines set for occupational HIV Exposure. Lancet. 1996;348:48. doi: 10.1016/s0140-6736(05)64359-0. [DOI] [PubMed] [Google Scholar]
- 5.Marcus R. Health care workers exposed to patients infected with HIV. International conference AIDS. 1989 Jun 4-9;5:63. (Abstract No. WAO.1) [Google Scholar]
- 6.WHO AIDS series 3 guidelines for nursing management of people infected with HIV. Geneva: WHO; 1988. [Google Scholar]
- 7.Garcia LP, Blank VL. Prevalence of occupational exposures to potentially infectious materials among dentists and dental assistants. Cad Saúde Pública. 2006;22:97–108. doi: 10.1590/s0102-311x2006000100011. [DOI] [PubMed] [Google Scholar]
- 8.Erridge P. The right of HIV infected health care workers. BMJ. 1996;347:1042. [Google Scholar]
- 9.Kelen GD, Green GB, Hexter DA, Fortenberry DC, Taylor E, Fleetwood DH, et al. Substantial improvements in compliance with universal precaution in an emergency department following institution of a policy. Arch Intern Med. 1991;151:2051–6. [PubMed] [Google Scholar]
- 10.Kermode M, Jolley D, Langkham B, Thomas M, Crofts N. Occupational exposure to blood and risk of blood borne virus infection among health care workers in rural north Indian settings. Am J Infect Control. 2005;33:34–41. doi: 10.1016/j.ajic.2004.07.015. [DOI] [PubMed] [Google Scholar]


