Abstract
Aims and Objectives:
Early recognition, aggressive surgical debridement, removal of cause, appropriate antibiotic therapy, improvement of immunocompromised state and dressing of the wound is the treatment of necrotizing cervical fasciitis. There are so many reported cases of burn and some reported cases of necrotizing fasciitis where amniotic membrane has been used as a dressing material, and that encouraged us to use it as a dressing material in our cases.
Materials and Methods:
Six cases of necrotizing cervical fasciitis reported to our department in a span of five years (2005 to 2010). Amniotic membrane taken from placenta of suitable donors had been used as a dressing material in these cases. Data collection included age, sex, medical history of the patients, size of the wound, pain felt by the patient, time taken for granulation tissue formation, total healing time, size of the scar and need for future reconstruction.
Results:
The sample consisted of six patients with a mean age of 45 years. Four of them were male. Etiology was always odontogenic. Five patients were immunocompromised. Three patients were chronic alcoholic. Average size of the wound was 42 square centimeter. Mean time taken for formation of granulation tissue was 22 days; mean total healing time was 36 days. In every case patient reported with pain, which gradually diminished after first application of amniotic membrane. In three cases, pain on fourth day after first application of amniotic membrane was nil (VAS scale). In rest three cases, pain on sixth day after first application of amniotic membrane was nil (VAS scale). Average size of the scar was 9 cm2. Secondary scar revision was required in all six cases.
Conclusion:
Our study concludes that amniotic membrane can be used effectively as a dressing material in necrotizing cervical fasciitis.
Keywords: Amniotic membrane, debridement, granulation tissue, necrotizing cervical fasciitis, scar
INTRODUCTION
Cervical necrotizing fasciitis is a rare, fulminating infection causing extensive necrosis of the subcutaneous tissue and fascial planes with tender, edematous, erythematous overlying skin.[1] It is mostly an odontogenic mixed infection in an immunocompromised patient. It has high mortality rate either due to sepsis and multiorgan failure or due to spread of infection in the mediastinum. On progress the overlying skin becomes pale and then dusky. Overlying skin also loses sensation.
Early recognition, aggressive surgical debridement, removal of cause, appropriate antibiotic therapy and improvement of immunocompromised state is the treatment followed by dressing of the wound.[2] Affected overlying skin is removed and open wound is covered by antiseptic dressing. Dressing is changed regularly similar to that of an extensive burn.[2] Gradually the slough clears and shiny granulation tissue appears. Debridement of the wound is done regularly. Generally the wound is washed and scrubbed regularly by hydrogen peroxide and antiseptics. In our cases we followed the same management protocol but for dressing purpose we used amniotic membrane instead of conventional closed dressing.
Amniotic membrane is the innermost layer of the placenta. It consists of inner single layer of amnion cells fixed to collagen-rich mesenchyme and loosely adhered to chorion. First reported use of amniotic membrane in skin transplantation was by Davis in 1910.[3] Amniotic membrane transplantation promotes re-epithelization, reduces inflammation and fibrosis and modulates angiogenesis.[4] H. Niknejad et al. say that amniotic membrane has anti-inflammatory, anti-fibrosis, anti-scarring antimicrobial properties and it has low antigenicity. It also acts as a scaffold for cell proliferation and differentiation.[3] Many authors said that human amniotic membrane is a good source of stem cells for tissue regeneration and repair.[3,5] In today's world this is widely used in eye surgery and burn cases as a biologic dressing material.[6,7] There are also some reported cases of using this as a dressing material in necrotizing fasciitis involving other parts of the body.[8] Amniotic membrane also had been used as a graft material for vestibuloplasty in a study.[9]
MATERIALS AND METHODS
Six patients having necrotizing cervical fasciitis reported to our department in a span of five years (2005 to 2010) [Figure 1]. Patients were immediately admitted, pus was sent for culture and sensitivity test; intravenous fluid and antibiotic therapy (ceftriaxone+sulbactum and metronidazole) were started and analgesic, antipyretic drugs were given for symptomatic relief.
Figure 1.
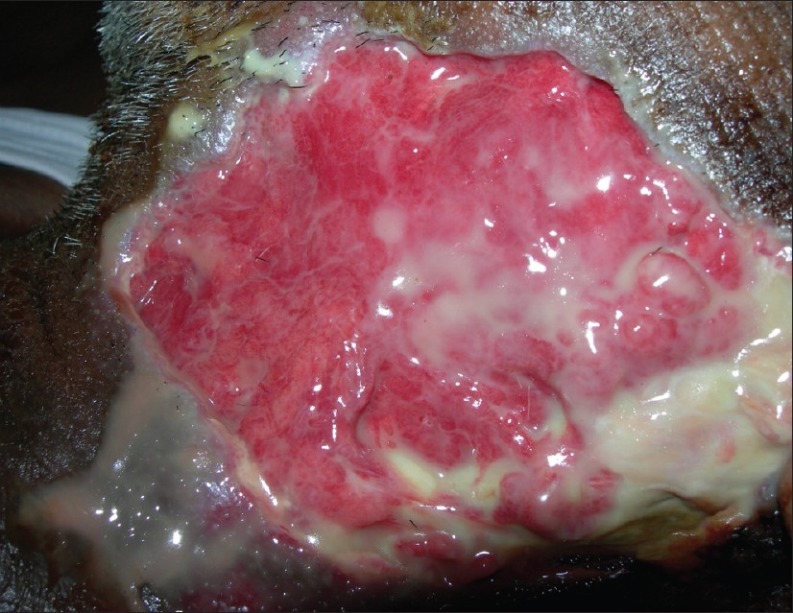
A patient with cervical necrotizing fasciitis
Amniotic membrane used in these cases had been taken from the placenta of the donors after cesarian delivery. Donors were selected after taking prior consent. Donors were medically fit. Blood of the donors were tested six months prior to delivery and few days prior to delivery to exclude the possibility of having diseases like AIDS and hepatitis B.
After completing pre-anesthetic evaluation, thorough surgical debridement, removal of affected overlying skin of the diseased area and extraction of offending teeth was done under general anesthesia [Figure 2]. Amniotic membrane was transplanted to the area to cover the raw wound [Figure 3]. Amniotic membrane source was placenta, obtained after delivery of suitable donor and it was stored at 4°C in 85% glycerol for at least 48 h. Before application, adequate amount of membrane was cut and taken from the stored amniotic membrane and it was well rinsed by normal saline to make it free from glycerol.
Figure 2.
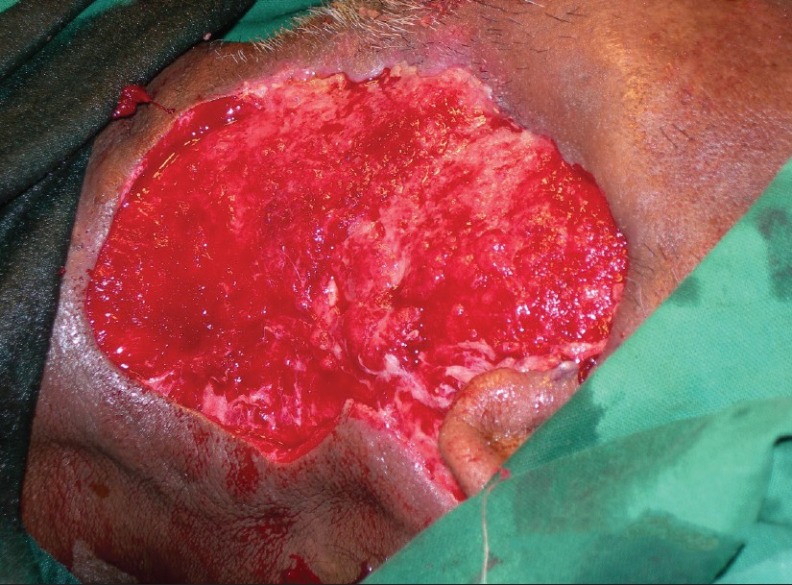
Picture of the wound of the same patient after debridement done under general anesthesia
Figure 3.

Dressing of the wound of the same patient by amniotic membrane
The transplanted membrane was covered by layers of some moist gauze, dry gauze, cotton and bandage. Suitable broad spectrum parenteral antibiotics for 7 days followed by suitable oral antibiotics were prescribed according to the result of the culture and sensitivity test.
We changed dressing regularly at 48-h interval. Change of dressing was done in a clean, sterile dressing room taking all aseptic measures and after taking care of the wound by debridement, scrubbing the wound by antiseptic (povidone-iodine) and washing it by hydrogen peroxide. Before replacing the membrane, the wound had been made reasonably dry by moist compression. This process of dressing change had been carried on until scar developed [Figure 4].
Figure 4.

Picture of the same patient showing wound contraction and scar formation
Data collection included age, sex, medical history of the patients; size of the wound, first evidence of granulation tissue formation, total healing time and need for future reconstruction. Pain felt by the patient was recorded on the reporting day, on the day of first application of amniotic membrane, on the second, fourth, sixth day post first application of amniotic membrane.
RESULTS
Among the six patients, four were male and two were female. Their average age was 45 years [Table 1]. Etiology was always odontogenic (carious lower molar teeth). All patients were weak, moderately febrile with anorexia and dysphagia and were experiencing moderate pain on the day of reporting. Five patients were known immunocompromised; two of them were having Type-2 diabetes and three of them were having compromised liver function due to chronic alcoholism [Table 1].
Table 1.
Table showing nature of wound and course of healing
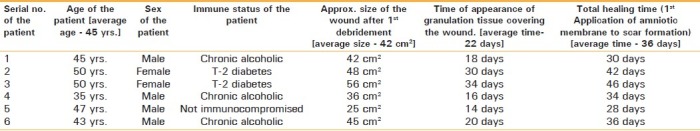
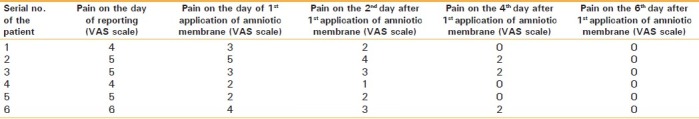
Pain felt by the patient was recorded on the day of reporting, on the day of first application of amniotic membrane, on the second, fourth, sixth day post first application of amniotic membrane. On the day of reporting pain was moderate, and on the day of first application of amniotic membrane pain was mild to moderate. In three cases, pain was absent on and from fourth day post first application of amniotic membrane. In rest three cases, pain was absent on and from sixth day post first application of amniotic membrane [Table 2].
Table 2.
Table showing VAS score for pain during healing
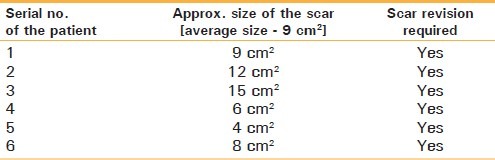
Average size of the raw wound after first debridement and before first application of amniotic membrane was 42 cm2 [Table 1]. Mean time taken for formation of granulation tissue covering the raw wound was 22 days [Table 1]. After average 36 postoperative days sufficient wound contraction and scar formation took place. That period was recorded as total healing time [Table 1]. Average size of the scar was 9 cm2 [Table 3]. Secondary scar revision was required in all six cases, although the patients accepted the scar and refused to go for further surgical intervention.
Table 3.
Table showing the final size of the scar formed
DISCUSSION
In our cases we dealt patients of cervical necrotizing fasciitis, etiology of which was always carious lower molar teeth. Cervical necrotizing fasciitis is mostly of odontogenic origin and there are many such reported cases.[10,11] L. Whitesides et al. said that substance abusers and immunocompromised persons are more prone to cervical necrotizing fasciitis. They used hyperbaric oxygen as adjunctive treatment in their cases and got good result.[11] Five of our patients were immunocompromised; two of them were having diabetes, three of them were having compromised liver function due to chronic alcoholism [Table 1]. Hyperbaric oxygen therapy is costly and rarely available in developing countries.
Niknejad et al recommended proper screening of the donor of the amniotic membrane to exclude any possibility of disease transmission. They advised to repeat the investigations after 6 months to crosscheck ‘window period’ of infection.[3] We followed the protocol.
Ravishankar et al. used 85% glycerol for preservation of amniotic membrane and we did the same thing following their protocol. They told about the advantages of glycerol-preserved amniotic membrane;[12] they are:
Ease of preservation and reconstitution
Low cost
Preservation of morphological structure of the cells
Low antigenicity
Antibacterial and antiviral properties of glycerol so that there is no danger of disease transmission
Provide pain relief and healing
Decreases bacterial count in the wound
Protects wound
Prevents fluid loss
Adhere well to wound
In our study we found all these true. It is easy to procure and preserve amniotic membrane at low cost. It is non-immunogenic; hence no special investigation was required and no rejection of the membrane took place. It seems that amniotic membrane combats infection, promotes healing and relieves pain as we observed in our cases. Mean time for formation of granulation tissue covering the raw wound was 22 days [Table 1], mean total healing time was 36 days [Table 1]. In our experience a healing time of 36 days was quite favorable, also the quantity of the scar was reasonable [Table 3]; however, a comparative study to demonstrate this is needed. Zarutskie and Silverberg. used amniotic membrane as a temporary dressing material in necrotizing fasciitis and they found that it had a better pain control.[8] In all cases patients reported with pain, which gradually diminished after first application of amniotic membrane. In all cases on and from sixth day after first application of amniotic membrane there were no pain [Table 2]. After formation of granulation tissue, split thickness skin grafts could be used in our cases to cover up the wound; however, the donor site morbidity and availability of donor site are its limitations.
CONCLUSION
Amniotic membrane is easily available at almost no cost especially in a center where delivery cases are done routinely. Sterilization, storage and application are simple.
Considering the properties of amniotic membrane and the easy availability, low cost of procurement and cheap storage makes it appear to be a useful dressing material for cervical necrotizing fasciitis in developing countries where hyperbaric oxygen therapy is costly and rarely available, but potential donors are need to be screened properly to ensure no transmission of disease.
Have we got a faster and better healing with lesser scar? It seems so but we cannot claim scientifically without doing a comparative study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Brook I, Frazier EH. Clinical and microbiological features of necrotizing fasciitis. J Clin Microbiol. 1995;33:2382–7. doi: 10.1128/jcm.33.9.2382-2387.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freischlag JA, Ajalat G, Busuttil RW. Treatment of necrotizing soft tissue infections. The need for a new approach. Am J Surg. 1985;149:751–5. doi: 10.1016/s0002-9610(85)80180-x. [DOI] [PubMed] [Google Scholar]
- 3.Niknejad H, Peirovi H, Jorjani M, Ahmadiani A, Ghanavi J, Seifalian AM. Properties of amniotic membrane for potential use in tissue engineering. Eur Cell Mater. 2008;15:88–99. doi: 10.22203/ecm.v015a07. [DOI] [PubMed] [Google Scholar]
- 4.Solomon A, Wajngarten M, Alviano F. Suppression of inflammatory and fibrotic responses in an invitro model of allergic inflammation by the amniotic membrane stromal matrix. Clin Exp Allergy. 2005;35:941–8. doi: 10.1111/j.1365-2222.2005.02285.x. [DOI] [PubMed] [Google Scholar]
- 5.IIancheran S, Moodley Y, Manuclpillai V. Human fetal membrane-a source of stem cells for tissue regeneration and repair? Placenta. 2009;30:2. doi: 10.1016/j.placenta.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Maral T, Huseyin B, Arsalan H, Demrhan B, Akinbingol G, Haberal M. Effectiveness of human amnion preserved long term in glycerol as a temporary biological dressing. Burns. 1999;25:625–35. doi: 10.1016/s0305-4179(99)00072-8. [DOI] [PubMed] [Google Scholar]
- 7.Solomon A, Meller D, Prabhasawat P, John T, Espana EM, Steuhl KP, et al. Amniotic membrane grafts for nontraumatic corneal perforations, descemetoceles, and deep ulcers. Opthalmology. 2002;109:694–703. doi: 10.1016/s0161-6420(01)01032-6. [DOI] [PubMed] [Google Scholar]
- 8.Zarutskie P, Silverberg F. Amniotic membrane as a temporary wound dressing in necrotizing fasciitis. Obstet Gynecol. 1984;64:284–7. [PubMed] [Google Scholar]
- 9.Samandari MH, Yaghmaei M, Ejalali M, Moshref M, Saffar AS. Use of amnion as a graft material in vestibuloplasty: A preliminary report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:574–8. doi: 10.1016/S107921040400006X. [DOI] [PubMed] [Google Scholar]
- 10.Moss RM, Kunpittaya S, Sonamuchart A. Cervical necrotizing fasciitis-an uncommon sequlae to dental infection. Ann Otol Rhinol Laryngol. 1990;99:643. doi: 10.1177/000348949009900811. [DOI] [PubMed] [Google Scholar]
- 11.Whitesides L, Cotto-Cumba C, Myers RA. Cervical necrotizing fasciitis of odontogenic origin: A case report and review of 12 cases. J Oral Maxillofac Surg. 2000;58:144–52. doi: 10.1016/s0278-2391(00)90327-6. [DOI] [PubMed] [Google Scholar]
- 12.Ravishankar R, Bath AS, Roy R. Amnion Bank-the use of long term giycerol preserved amniotic membranes in the management of superficial and superficial partial thickness burns. Burns. 2003;29:369–74. doi: 10.1016/s0305-4179(02)00304-2. [DOI] [PubMed] [Google Scholar]


