Abstract
Non-Hodgkin's lymphomas are a group of neoplasms that originate from the cells of the lymphoreticular system. Forty percent of non-Hodgkin's lymphomas arise from extra nodal sites. Non-Hodgkin's lymphomas detected primarily in the bone are quite rare, but among jaw lesions, they are more frequently present in the maxilla than in the mandible. There are no classical characteristic clinical features of lymphomas involving the jaw bones. Swelling, ulcer or discomfort may be present in the region of the lymphoma, or it may mimic a periapical pathology or a benign condition. Extranodal non-Hodgkins lymphoma of the maxilla could present as one of the early manifestation of detrimental diseases. Clinically these types of lymphoma can mimic an inflammatory endo-periodontal lesion with symptoms of pain and local discomfort. The greater the delay in diagnosis subsequently worsens the prognosis. A case of maxillary non-Hodgkin's lymphoma with an unusual presentation is discussed.
Keywords: Non-Hodgkin's lymphoma, maxilla, rare entity
INTRODUCTION
Lymphomas are a diverse group of neoplasm's affecting the lympho reticular system. Most of them originate from B lymphocyte. Lymphoma is the second common malignancy of head and neck.[1] Primary non-Hodgkin's lymphoma (NHL) of the bone is rare, accounting for <5%.[2,3] In 1963, the term primary lymphoma of bone was introduced by Ivins and Dahlin.[2] The etiology is unknown even though virus and immuno-suppression are associated. The most common manifestations are pain and swelling in the jaw bone, but it is often clinically diagnosed as a dental infection. Hence, the diagnosis of lymphoma in jaw bone is often delayed. Biopsy is considered when there is a nonhealing extraction wound and if any oral wound is not resolving for a prolong period. We present a case with a chief compliant of mobile teeth, which was later diagnosed as primary NHL of the maxilla.
CASE REPORT
A 30-year-old female patient reported to the department of oral and maxillofacial surgery with complains of growth in the left upper jaw at the site of extraction wound. History revealed she was apparently alright 15 days back; she visited a local dentist for pain in the left upper back teeth, which were found to be mobile and were extracted. Following extraction she noticed a small growth which was insidious in onset and gradually increased to the present size at the site of extraction after 15 days of teeth removal. She revisited the same dentist who referred to our institution. Her medical and family history was not contributory. She was happily housewife with two children. She did not have any abusive habits.
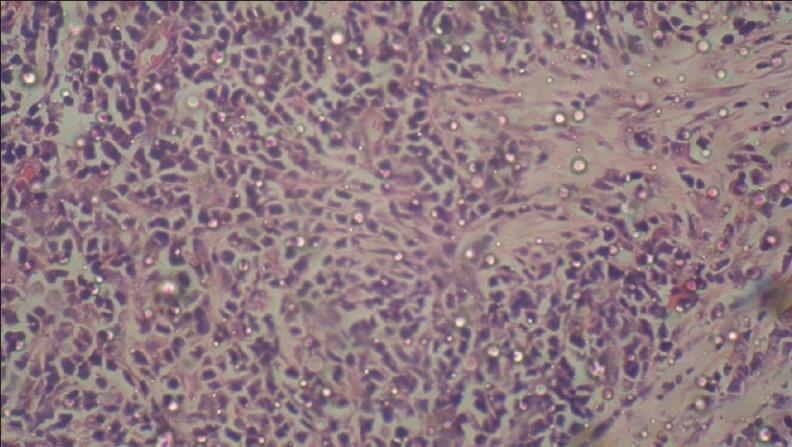
On examination a single, lobulated, sessile pink in color, nonpulsatile lesion was found to be present in 25, 26, 27 regions which extended beyond the occlusal surfaces of teeth both buccally and palatally of approximately 4 cm × 3cm in size [Figure 1]. On palpation, the swelling was fibrous and edematous which was interfering with the occlusion [Figure 2]. There were indentations of the lower teeth on the swelling. There was no regional lymphadenopathy. Differential diagnosis of squamous cell carcinoma and benign tumors were considered. Orthopantomogram (OPG) and PNS view revealed haziness in the left maxillary antrum with radiolucency extending in the alveolus of 25, 26, and 27 regions. Otherwise, her skeletal survey was normal. The CT scan of maxilla [Figures 3–5] revealed break in continuity of buccal, palatal walls, and inferior wall of maxillary antrum. An incisional biopsy was carried out after doing routine blood investigations. Western blot test revealed that patient was HIV positive. The biopsy specimen revealed sheets of abnormally large lymphoid cells with high nucleus: cytoplasmic ratio, coarse chromatin, and inconspicuous nucleoli with abnormal mitotic [Figure 6]. The features were suggestive of large cell lymphoma of B-cell type. Immuno-histochemistry revealed positive CD20, LCA, and CD3, CK were negative, which proved conclusively the lesion to be as a NLM, diffuse large B-cell type. The HIV status was in the fourth stage which superseded non-Hodgkin's lymphoma as per WHO classification. History regarding the HIV-positive status did not reveal any mode of transmission of HIV infection.
Figure 1.

Intra-oral growth extending from 25 to 27 with extension on buccal and palatal side
Figure 2.

Sagittal section of CT showing the extent into the antrum
Figure 3.
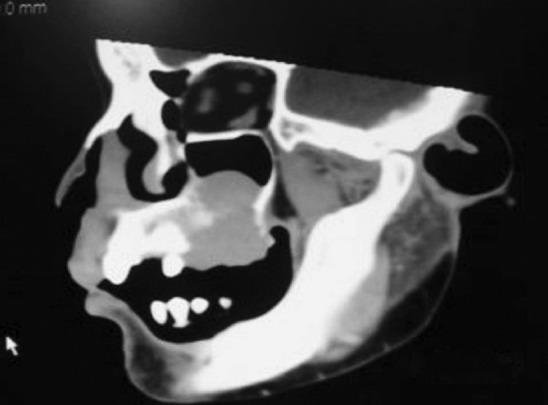
Occlusal view of maxilla in CT showing destruction of maxillary alveolus
Figure 5.

Histopathological examination
Figure 6.
Lesion interfering occlusion
Figure 4.

Coronal CT showing extent of lesion
She was referred to the oncologist. The patient was started on anti-retroviral treatment. Chemotherapy was advised by the oncologist and a total of three cycles were suggested at the gap of every 3 weeks. The treatment regimen followed was that of classical CHOP therapy which comprised of using cyclophosphamide, doxorubicin (hydrodoxorubicin), vincristine (oncovin), and prednisolone. At the end of two cycles the swelling started regressing in size and totally disappeared after three cycles. The growth completely disappeared after chemotherapy [Figure 7]. The patient died 6 months after chemotherapy.
Figure 7.

Regression of the lesion
DISCUSSION
Lymphomas are a diverse group of neoplasms affecting the lympho reticular system. Lymphomas have been traditionally divided into Hodgkin's disease and non-Hodgkin's disease. Hodgkin's disease often presents as nodal disease, commonly involving cervical, axillary, and inguinal nodes, whereas non-Hodgkin's disease may develop extra-nodally, outside the lymphoid system and can occur in stomach, salivary glands, and rarely in oral cavity and jaws.[4]
Lymphomas are second only to squamous cell carcinoma in the frequency of malignant neoplasms involving the soft tissues of head and neck region, which usually affects the lymph nodes. NHL are a group of highly diverse malignancies and have great tendency to affect organs and tissues that do not ordinarily contain lymphoid cells. Twenty-thirty percentage of NHL arise from extra-nodal sites.[5]
The head and neck is the second most common region for the extra-nodal lymphoma, the first being the gastro intestinal tract.[5] NHL rarely manifests as a primary malignancy in the head and neck region of >1% and may give an important clue for undiagnosed HIV infection, which accounts for 2% of oral neoplasms in patients with AIDS.[6] Among various head and neck sites, Waldeyers ring, which is the area encompassed by the nasopharynx, tonsil, and base of the tongue, is the most often involved by malignant lymphoma. The nose, para-nasal sinuses, orbit(s), and salivary glands are the other sites affected in head and neck region. Involvement of the oral cavity is not common. The maxilla is affected more commonly than the mandible.[5] Palate and gingiva account for almost 70% of lesions in maxilla[7,8] as seen in our case.
It more commonly affects the middle aged and the elderly (40-80 yrs) with slight male predilection with a male to female ratio of 3:2.[4] There is reversal of the incidence of NHL among young HIV-positive patients. HIV patients are 60 times at risk than the general population and around 3% of HIV-infected people develop lymphomas.[5] In our case, patient was only 30 years old with good health. The gingival and palate regions are commonly affected, while involvement of the alveolus and buccal vestibule, as seen in our patient, is rare. Secondary organ involvement along with the primary in the oral cavity is generally observed.[6]
Primary lymphoma of the bone was first described by Parker and Jackson as primary reticular cell sarcoma of bone.[4] Clinical features of lymphoma of the oral region are not characteristic. They occur as local bony swelling, tooth mobility, painless inflammation of the mucosa with or without ulcerations, and rarely facial or dental pain. Additional observations include trismus, otalgia, gingival ulceration, sinusitis, or cervical lymphadenopathy.[4,5] The oral NHL is more common benign oral and dental pathological conditions.[8] In our case, the patient was aware of the slow growing swelling that was not painful and of short duration which was 15 days following extraction of mobile teeth. Specific and evident radiological signs of bone involvement may be absent in 10-20% of cases. The radiographic findings usually are those of periapical inflammatory processes or osteitis. Diffuse trabecular honeycomb images are occasionally observed. Those may be the images of cortical destruction and invasion of the maxillary sinus.[4,5] Differential diagnosis includes infectious process such as systemic or deep mycosis, dento-alveolar abscess, Wegener's granulomas, midline lethal granulomas, squamous cell carcinomas, metastatic tumors, neoplastic process, wherein very rapid growth is a feature of sarcomas and lympho proliferative disorders.[5]
NHL can be managed by chemotherapy, radiotherapy, and surgery in various combinations. NHL arising in bone is best treated by chemotherapy and may not require radiotherapy.[4] Generally, a combination of chemotherapy (cyclophosphamide, doxorubicin, vincristine, prednisone) and field radiation is recommended for treatment. Monoclonal antibodies directed against antigens or within the lymphoma and injection of interferon have also been used.[6] Survival is excellent in localized disease, whereas disseminated disease seems less favorable.[4]
The prognosis of the disease is good with a maximum of 5-year survival rate in 30% of cases after therapy. The disease may occasionally progress into a diffuse pattern with cutaneous nodules and plaques which undergo blast transformation or rarely turn into leukemia.[6] Currently, the median survival rate of patients with AIDS related to lymphomas after treatment is 5-11 months,[9] as was in our case. In contrast, the response of the non-HIV-positive population to aggressive chemotherapy in the absense of immuno-suppression has highly been effective; 65% to 85% experienced a complete survival response and 50% to 75% attained long-term survival.[9]
CONCLUSION
The main purpose of this article is to develop awareness among dentists as there is an increased risk of oral NHL in the HIV-positive population and to emphasize the importance of including NHL in the differential diagnosis of intra oral soft tissues or ulcerations. This is to stress the importance of early diagnosis to ensure appropriate treatment, to improve prognosis, and quality of life. Prognosis is excellent in localized disease, whereas in disseminated disease, it is less favorable. Lymphomas arising in bone may be effectively managed by chemotherapy alone. Thus, with the rising incidence of extra-nodal lymphomas it has become very important for present age dentists not to take any swellings of the orofacial region at face value but to properly investigate its pathology and treat it judiciously.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Boulaadas M, Benazzou S, Sefiani S, Nazih N, Essakalli L, Kzadri M. Primary extranodal non-Hodgkin's lymphoma of the oral cavity. J Craniofac Surg. 2008;19:1183–5. doi: 10.1097/SCS.0b013e3181764b56. [DOI] [PubMed] [Google Scholar]
- 2.Dinakar J, Priya L, Reddy S. Primary non-Hodgkin's lymphoma of the mandible. J Oral Maxillopath. 2010;14:73–6. doi: 10.4103/0973-029X.72506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frei M, Dubach P, Reichart PA, Schmitt AM, Mueller-Garamvölgyi E, Bornstein MM. Diffuse swelling of the buccal mucosa and palate as first and only manifestation of an extranodal non-Hodgkin ‘double-hit’ lymphoma: report of a case. Oral Maxillofac Surg. 2012;16:69–74. doi: 10.1007/s10006-010-0254-5. [DOI] [PubMed] [Google Scholar]
- 4.Kini R, Saha A, Naik V. Diffuse Large B cell lymphoma of mandible: A case report. Med Oral Patol Oral Cir Bucal. 2009;14:e421–4. [PubMed] [Google Scholar]
- 5.Sankaranarayanan S, Chandrasekar T, Rao P Srinivasa, Rooban T, Ranganathan K. Maxillary Non-Hodgkins lymphoma. J Oral Maxillofac Pathol. 2005;9:34–6. [Google Scholar]
- 6.Pratibha R, Ahmed S, Janaki VR. Primary extranodal non-Hodgkin's lymphoma- A case report. Indian J Dermatol Venereol Leprol. 2004;70:172–4. [PubMed] [Google Scholar]
- 7.Eisenbud L, Scinbba J, Mir R, Sachs SA. Oral presentations in nonHodgkin's Vs lymphoma: A review of thirty one cases. Part I. Data analysis. Oral Surg Oral Pathol. 1984;57:272–80. doi: 10.1016/0030-4220(84)90183-x. [DOI] [PubMed] [Google Scholar]
- 8.Slootweg PJ, Wittkampf AR, Kluin PM, de Wilde PC, van Unnik JA. Extranodal nodal non-Hodgkin's Vs lymphoma of the oral tissues. An analysis of 20 cases. J Maxillofac Surg. 1985;13:85–92. doi: 10.1016/s0301-0503(85)80022-9. [DOI] [PubMed] [Google Scholar]
- 9.Lozada-Nur F, de Sanz S, Silverman S, Jr, Miranda C, Regezi JA. Intra oral non-Hodgkin's lymphoma in seven patients with acquired immunodeficiency syndrome. Oral Surg Oral Med Oral Pathpl Oral Radiol Endod. 1996;82:173–8. doi: 10.1016/s1079-2104(96)80221-6. [DOI] [PubMed] [Google Scholar]


