Abstract
Cementoblastoma is a relatively uncommon, benign odontogenic neoplasm of jaws. Mandible is affected more than the maxilla. The lesions are generally diagnosed on a routine radiograph. The localized expansion of cortical plates is observed. Radiographically, it consists of well-defined radiopacity with a radiolucent band. Here is a case report of a female aged 55 years having swelling in the right mandibular angle with an extraoral draining sinus. A panoramic radiograph shows a dense radiopaque mass along the roots of the third molar surrounded by a radiolucent band. Surgical excision was carried out and a histopathological examination was carried out which was suggestive of cementoblastoma.
Keywords: Cementoblastoma, radiopaque mass, infected
INTRODUCTION
Cementoblastoma is a relatively uncommon benign odontogenic neoplasm of the jaws and was first described by Dewey[1] in 1927. It represents less than 1% of all odontogenic tumors.[2,3] The lesion is considered as the true neoplasm of cemental origin.[1,4] The benign cementoblastoma is recognized in the World Health Organization's (WHO's) classification (1971) of periapical odontogenic tumors as one of the four types of cementum-producing disorders. The other three are periapical cemental dysplasia, cementifying fibroma, and gigantiform familial cementoma.[5–7] The WHO defines benign cementoblastoma as “a neoplasm characterized by the formation of sheets of cementum- like tissue containing a large number of reversal lines and a lack of mineralization at the periphery of the mass or in the more active growth area.”[8,9] The WHO has classified benign cementoblastoma and cementifying fibroma as the only true cemental neoplasm.[8,10] Most benign cementoblastomas develop in the mandible. Mandible is affected three times more frequently than the maxilla. The most commonly affected tooth is mandibular first molar.[6,11–13] However, other teeth involved have included mandibular second and third molars, mandibular bicuspids and maxillary bicuspids, and first, second and third molars.[13] True cementoblastoma can be associated with deciduous molars, although this is an uncommon occurrence.[6,14] Lesions generally are discovered in patients younger than 30 years of age, often on a routine radiograph[6,11] although the range has been 10–72 years.[13] Symptoms may be totally absent or when they do occur, they tend to be minor. Pain occurs in some cases. The localized expansion of cortical plates of bone is a typical feature.[8] Radiographically, cementoblastoma typically consists of well-defined radiopacity with a cortical border and then a well-defined radiolucent band just inside the cortical border.[6,15] The outline of the affected root is generally obliterated because of the resorption of the root and fusion of the mass to the tooth.[13] Most teeth affected by the cementoblastoma respond normally to the vitality tests during early stages of the lesion, but necrotic pulp can occur with this entity, usually in later stages.[6]
CASE REPORT
A 55-year-old female reported to the Department of Oral and Maxillofacial Surgery, with complaints of swelling in the right mandibular angle since 1 year and pus discharge in the same region since 2 months. History revealed that the patient had mild swelling with respect to the right mandibular angle since 6 years which underwent a sudden increase in size since a year. No history of fever, paresthesia, and numbness of the lower lip was reported. The past medical history revealed chronic obstructive pulmonary disease in the patient.
An extraoral examination revealed facial asymmetry due to the presence of diffuse swelling and draining sinus with respect to the inferior border of the right mandibular angle. Swelling was firm to hard with no tenderness. An intraoral examination revealed buccal and lingual cortical expansion with third molar. A hard mass was palpable beneath the buccal mucosa and also on the lingual mucosa with respect to the mandibular angle. Provisional diagnosis of cementoblastoma, cement-ossifying fibroma, and complex odontoma was made.
A panoramic radiograph revealed a dense radiopaque mass surrounded by a well-defined radiolucent band with respect to the mandibular angle. The outline of the roots of the third molar was obliterated and the radiopaque mass seemed to be attached to the roots of third molar [Figures 1–5].
Figure 1.

Pre-Operative OPG
Figure 5.

Post operative OPG
Figure 2.
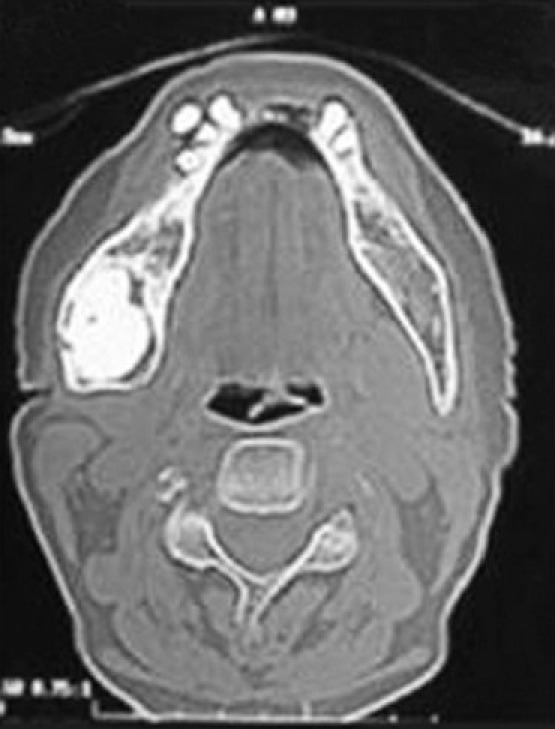
Axial view of lesion on CT scan
Figure 3.

Three dimensional view of lesion on CT scan
Figure 4.
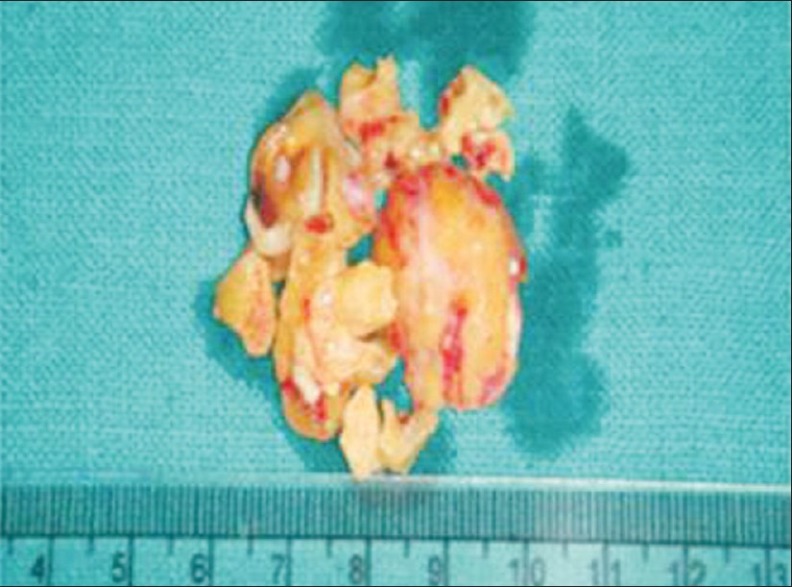
Excised lesion mass
A CT examination of the mandible revealed a large expansile radiopaque mass measuring 2×2 cm in size.
The patient was treated for the COPD first by the physician and simultaneously the patient was put on antibiotics to eradicate the infection from the lesion. After the patient was medically fit, the lesion was surgically excised along with the tooth and the sinus lining was excised. The specimen was submitted for the histological examination. A postsurgical panorogram was obtained.
Histopathologically, the tumor consisted of a calcified mass fused with the roots of third molar with a resultant obliteration of the periodontal ligament. The tumor comprised sheets of calcified tissue with multiple reversal lines and prominent cementoblasts and multinucleated cementoclasts. The peripheral columns showed characteristic radiating columns of the cementum perpendicular to the surface of the lesion. The patient did well postoperatively, with no complications or paresthesia. A postoperative radiograph revealed a complete excision.
DISCUSSION
The cementoblastoma or true cementoma is a slow-growing, benign odontogenic tumor arising from ectomesenchyme.[9] Some authors say that it was described by Dewey.[1] The other class of authors says that it was first described by Norberg.[3,6] Although statistical data suggest that benign cementoblastomas are uncommon, many believe that they occur more often than published account indicates.[15] Cementoblastomas have an unlimited growth potential and endodontic therapy does not eliminate or arrest them.[6] Most patients remain asymptomatic and the lesion is discovered on routine radiographs. Lesions are more common in males than females.[13,15] Lesions commonly occur in the younger age group with people less than 30 years of age.[6] More than 50% of the lesions occur under 20 years of age and the lesion is located in the mandible in more than 70% of cases (with a predominant location at the first molar and second premolar).[3] The expansion of the cortical plates of the bone is the typical feature of cementoblastoma.[6,13,15] The cementoblastoma has a pathognomonic radiographic appearance. It appears as well-defined solitary, circular radiopacity with a radiolucent halo. The lesion is fused to the partly resorbed roots of the associated tooth. The internal structure of the mass may possess a mixed radiolucent–radiopaque quality with a radiating pattern.[10,13,15] The most common lesion to simulate this appearance is a solitary periapical cemental dysplasia. The other differential diagnoses are osteoblastoma, odontome, hypercementosis, and condensing osteitis. A radiolucent band around the benign cementoblastoma is usually better defined and more uniform than with cemental dysplasia.[15] Periapical cemental dysplasia is small in size and shows a progressive change in radiographs from radiolucent to mixed to radiopaque over time.[10] Osteoblastoma and cementoblastoma are closely related lesions that are histologically very similar.[10,16] The cementoblastoma is distinguished from the osteoblastoma by its location in an intimate association with the tooth root. The osteoblastoma arises in the medullary cavity of long bones.[10] The odontome is usually not fused with the tooth root and appears as a more heterogenous radiopacity.[10,13,15] Condensing osteitis lacks a peripheral radiolucent halo.[10] Hypercementosis is a small lesion and does not associate with pain or jaw swelling.[10] Due to benign but a locally aggressive nature of the lesion,[9] the treatment of choice is a complete removal of the lesion along with the associated tooth. A more conservative approach to retain the associated tooth and removal of the lesion using a surgical endodontic technique has been reported.[6,10,17,18] It can be used for small lesions in strategic teeth in which the lesion can be excised without injuring adjacent teeth and if a sufficient crown-to-root ratio remains after apicoectomy. Recurrence after the excision is rare; if it recurs, it is because of an inadequate excision of the lesion.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Dewey KW. Osteoma of molar. Dent Cosmos. 1927;69:1143–9. [Google Scholar]
- 2.Regezi JA, Kerr DA, Courtney RM. Odontogenic tumors: An analysis of 706 cases. J Oral Surg. 1978;36:771–8. [PubMed] [Google Scholar]
- 3.Ahrens A, Bressi T. True cementoma (Benign Cementoblastoma): A case report. Rivista Scientifica Europea. 2005;2:1–4. [Google Scholar]
- 4.Lu Y, Xaun M, Takata T, Wang C, He Z, Zhou Z, et al. Odontogenic tomours. A demographic study of 759 cases in a chinese population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:707–14. doi: 10.1016/s1079-2104(98)90208-6. [DOI] [PubMed] [Google Scholar]
- 5.Pindborg JJ, Kramer IRH, Torloni H. Histological typing of odontogenic tumors, jaw cysts, and allied lesions. Geneva: Presented at a meeting of World Health Organization; 1971. [Google Scholar]
- 6.Biggs TJ, Benenati WF. Surgically treating a benign cementoblastoma while retaining the involved tooth. J Am Dent Assoc. 1995;126:1288–90. doi: 10.14219/jada.archive.1995.0365. [DOI] [PubMed] [Google Scholar]
- 7.Ghandour K. Cementomas. Den News. 1997;4:1. [Google Scholar]
- 8.Kramer IR, Pindborg JJ, Shear M. World Health Organization, International Histological Classification of Tumors. New York: Springer-Verlag; 1992. Histological typing of odontogenic tumors; p. 23. [Google Scholar]
- 9.Schafer ET, Singh B, Myers RD. Cementoblastoma associated with a primary tooth: A rare pediatric lesion. Pediatr Dent. 2001;23:351–3. [PubMed] [Google Scholar]
- 10.Pynn RB, Sands DT, Bradley G. Benign cementoblastoma: A case report. J Can Dent Assoc. 2001;67:260–2. [PubMed] [Google Scholar]
- 11.Zachariades N, Skordalaki A, Papanicolaou S, Androulakakis E, Bournias M. Cementoblastoma: Review of the literature and report of a case in a 7-year old girl. Br J Oral Maxillofac Surg. 1985;23:456–61. doi: 10.1016/0266-4356(85)90031-2. [DOI] [PubMed] [Google Scholar]
- 12.Piatelli A, D’Addom A, Piatelli M. Benign Cementoblastoma: Review of literature and report of a case of an unusual location. Acta Stomatol Belg. 1990;8:209–15. [PubMed] [Google Scholar]
- 13.Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. 4th ed. Philadelphia: W.B. Saunders; 1993. pp. 301–3. [Google Scholar]
- 14.Cannel H. Cementoma of a deciduous tooth. Oral Surg Oral Med Oral Pathol. 1991;71:648. doi: 10.1016/0030-4220(91)90379-q. [DOI] [PubMed] [Google Scholar]
- 15.White, Pharoh . Oral Radiology principles and interpretation. 5th ed. Missouri: Mosby; 2009. pp. 434–8. [Google Scholar]
- 16.Slootweg PJ. Cementoblastoma and Osteoblastomaa comparison of histologic features. J Oral Pathol Med. 1992;219:385–9. doi: 10.1111/j.1600-0714.1992.tb01024.x. [DOI] [PubMed] [Google Scholar]
- 17.Georig AC, Fay JT, King E. Endodontic treatment of cementoblastoma. Oral Surg. 1984;58:133–6. doi: 10.1016/0030-4220(84)90125-7. [DOI] [PubMed] [Google Scholar]
- 18.Keyes G, Hilferbrand K. Successful surgical endodontics for benign cementoblastoma. J Endod. 1987;13:566–9. doi: 10.1016/s0099-2399(87)80007-9. [DOI] [PubMed] [Google Scholar]


