Abstract
Context:
The surgical removal of impacted mandibular third molar is associated with minor but expected complications like pain, swelling, bruising and trismus. The lingual nerve damage sometimes occurs after the removal of mandibular third molar producing impaired sensation or permanent sensory loss. This complication is usually unexpected and unacceptable for the patients particularly if no prior warning has been given.
Aims:
The aim of the present clinical prospective study was to determine the clinical incidence of lingual nerve injury following mandibular third molar removal and to analyze possible factors for the lingual nerve injury.
Settings and Design:
Clinical prospective study in the Department of Oral Surgery, Punjab Government Dental College and Hospital, Amritsar.
Materials and Methods:
Ninety patients were selected randomly, amongst the patients, who reported to our department from January 2009 to December 2009 for the surgical removal of impacted mandibular third molar. To minimize the risk of lingual nerve injury, the standard terence wards incision was made in all cases and only buccal flap was raised.
Statistical Analysis:
The small number of paraesthesia precluded statistical analysis.
Results:
Out of 90 patients, six patients were diagnosed with lingual nerve paraesthesia. The overall incidence rate of lingual nerve injury was 6.6%.
Conclusions:
It can be concluded that lingual nerve paraesthesia can occur with or without reflection of lingual flap in spite of all the measures taken to protect it. It may be contributed to the fact of anatomical variations of lingual nerve.
Keywords: Lingual nerve, paraesthesia, third molar
INTRODUCTION
The surgical removal of impacted mandibular third molar is associated with minor but expected complications like pain, swelling, bruising and trismus. The lingual nerve damage sometimes occurs after the removal of mandibular third molar producing impaired sensation or permanent sensory loss. This complication is usually unexpected and unacceptable for the patients particularly if no prior warning has been given.[1]
The incidence of lingual nerve injury may occur because of surgeon's inexperience, procedure methodology and certain specific factors such as raising and retracting a lingual mucoperiosteal flap with a Howarth periosteal.[2]
Rood[3] (1983) reported an initial incidence of 6.6% lingual nerve injury, Blackburn and Bramley,[2] 11% and VonArx and Simpson (1997) reported 22%. The exact mechanism of lingual nerve damage during third molar surgery is controversial and amongst the most studies causes are lingual plate perforation and lingual flap trauma during ostectomy or tooth sectioning, usage of lingual flap retractor and supra-crestal incision because the nerve can be located in this region in some cases and may be sectioned. Many researchers (Pogral and Miloro, Kiesselback) have found the intimate relationship between the lingual nerve and mandibular lingual plate around posterior areas. Manson (1988) found no single factor to be causative but the most significant were the depth of impaction, removal of distal bone, elevation of lingual flap and length of operation time.[2]
The aim of the present clinical prospective study was to determine the clinical incidence of lingual nerve injury following mandibular third molar removal and to analyze possible etiologic factors for the lingual nerve injury.
MATERIALS AND METHODS
Ninety patients were selected randomly, amongst the patients, who reported to our department from January 2009 to December 2009 for the surgical removal of impacted mandibular third molar. Medically compromised patients were excluded from this study. Preoperative factors such as depth of impaction, tooth position and bony coverage were considered using orthopantomograph and intraoral periapical radiograph. The impacted mandibular third molars were classified by the “Winter's classification.” Surgical procedure was performed under local anesthesia by the same operator. To minimize the risk of lingual nerve injury the standard Terence Ward's incision was made in all cases and after reflecting the buccal flap, a gutter in the disto-buccal bone was created to expose maximum contour of the tooth. The bone removal was done with the help of motor-driven surgical bur under the constant irrigation of normal saline. Odontectomy or odontotomy procedure was done depending on the path of removal of impacted tooth.
Sensory disturbance was evaluated on 1st and 7th postoperative day and any complaint concerning sensory disturbance of the lingual gingiva and mucosa of the floor of the mouth and tongue was recorded. Assessment of postoperative deficit was carried out by standard questioning, for example: “Do you have normal feeling in your tongue” and pin prick test was used to confirm nerve injury. Patient with any complaint concerning sensory disturbance on postoperative evaluation were advised for regular follow up at the interval of one month and observed up to 6 months, if paraesthesia persisted.
RESULT
Out of 90 patients, six patients were diagnosed with lingual nerve paraesthesia on 1st and 7th postoperative day evaluation. The overall incidence rate of lingual nerve injury was 6.6%. One patient with paraesthesia was lost from the study after approximately 3 months of observation due to geographical relocation but this patient had definite sign of return of sensation when he was lost from study. In one patient paraesthesia persisted even after 6 months of follow up in spite of conservative therapy of Cyanocobalamin 1500 unit/day. Other four patients with paraesthesia recovered within 6 months of observation [Table 1].
Table 1.
Number of patients with paraesthesia, tooth position, depth of impaction, state of eruption and time of recovery
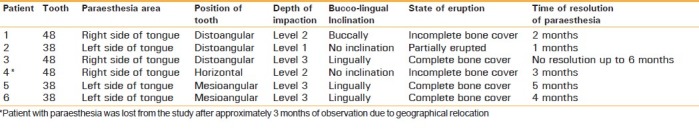
The small number of paraesthesia precluded statistical analysis. However when factors possibly contributing to lingual nerve paraesthesia was analyzed separately and combined, it revealed that paraesthesia were generally associated with horizontal and distoangulation of impaction, impaction with the crown approximating the cemento-enamel junction of second molar, lingual inclination of tooth, state of eruption and duration of surgery.
DISCUSSION
The figure of 6.6% for the lingual nerve injury is higher than expected from clinical experience and accounts in the literature. However it is same as that reported by Rood (1983). This prospective study supports other retrospective reports (David T. Wofford),[4] in noting a possible association between paraesthesia and bony-impacted mandibular third molars, use of bur to remove bone during the surgical extraction, position of impaction and state of eruption. In addition, factors which might be implicated such as the injury due to injection, deep lingual bite while suturing, scar tissue formation were not examined as they were considered difficult to record and analyze.
The causative factors can be discussed under following headings
1. Lingual inclination and lingual flap retraction
In our study, lingual retractor was not used in any case. As reported by Pichler JW, Beirne,[5] lingual nerve injury is 8.8 time more likely to occur in buccal approach with lingual retractor than buccal approach without lingual retractor. Various study reported that the incidence of transient nerve injury is more frequent with lingual flap reflection but it decreases the chance of permanent nerve injury. Pogrel et al[6] and Green wood et al (2004) support the lingual flap reflection and use broader retractors to protect the lingual nerve.[7]
In our study, 15 patients were operated in which third molar was lingually inclined although no attempt was made to raise and retract the lingual flap; the lingual tissue was retracted only to expose the occlusal aspect of tooth.
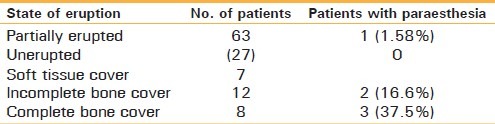
Out of these 15 patients, paraesthesia occurred in 3 patients, paraesthesia of two patients resolved within five months but in one patient paraesthesia did not resolve even within 6 months follow up. Hence the incidence of lingual nerve paraesthesia was more observed with lingually inclined tooth than buccal inclination [Table 2].
Table 2.
Buccolingual inclination and paraesthesia

2. State of eruption
It has been reported by Valmeseda-Castellon[8] that the incidence of lingual nerve paraesthesia was more prone on surgical removal of unerupted mandibular third molar.
Our study also supports Valmeseda-Castellon study and observed more lingual nerve paraesthesia with surgical removal of unerupted mandibular (complete bone cover) third molar [Table 3].
Table 3.
State of eruption and paraesthesia
3. Tooth position
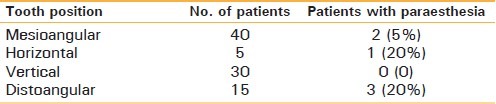
In addition to buccolingual inclination and state of eruption, we also observed the relation of tooth position and incidence of paraesthesia and found more paraesthesia with distoangular and horizontal-impacted third molar [Table 4].
In our study, 5 patients with horizontal-impacted third molar were operated by odontotomy with slight distal bone cutting as needed in these cases and we found postoperative paraesthesia in one patient.
In spite of slight distal ostectomy paraesthesia was observed in this patient. The distal ostectomy may be causative factor for paraesthesia in this patient, as supported by Valmeseda-Castellon[8] study.
Table 4.
Tooth position and paraesthesia
4. Depth of impaction
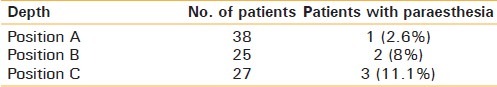
Association of depth of impaction with lingual nerve paraesthesia also observed and found that third molar present below the cementoenamel junction of second molar (level 3) is more significant for paraesthesia [Table 5].
D.A.Mason 2005[9] also reported that the depth of impaction is significantly related with lingual nerve injury.
Table 5.
Depth of impaction and paraesthesia
5. Operation time
In our study paraesthesia in all but one patients resolved within 1to 5 months and paraesthesia in one patient seemed to be “permanent” according to the criteria established by Simpson and Kipp et al.[10] In this patient, the tooth was placed distoangular and completely covered with bone. In comparison to other patient (average time of removal was 20 min), it took more time to remove (almost 40 min). The surgical time may be a contributory factor for lingual nerve injury in this patient as reported by “Valmeseda-Castellon”.[8]
The “Zuniga JR, Blackburn CW[2] reported the incidence of permanent damage of lingual nerve vary between 0.5% to 2%. In our study the incidence of permanent nerve injury was 1.1% which is closer to reported study.
From our study and review of literature, it can be concluded that lingual nerve paraesthesia can occur with or without reflection of lingual flap and in spite of all the measures taken to protect it. It may be contributed to the fact of anatomical variations of lingual nerve. However if on clinical examination or radiographic presentation, it is pre-assessed that lingual nerve can be injured during surgical procedure, it should be well explained to the patient to avoid any legal litigation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Carmichael FA, McGowan DA. Incidence of nerve damage following third molar removal: A West of Scotland Oral Surgery Research Group study. Br J Oral Maxillofac Surg. 1992;30:78–82. doi: 10.1016/0266-4356(92)90074-s. [DOI] [PubMed] [Google Scholar]
- 2.Blackburn CW, Bramley PA. Lingual nerve damage associated with the removal of lower third molars. Br Dent J. 1989;167:103–7. doi: 10.1038/sj.bdj.4806922. [DOI] [PubMed] [Google Scholar]
- 3.Graff-Radford SB, Evans RW. Lingual nerve injury: incidence. [Last accessed on 2011 Mar 26]. Available from: http://www.medscape.com/viewarticle/4620665 .
- 4.Wofford DT. Prospective study of dysesthesia following odontectomy of impacted mandibular third molar. [Last accessed on 1987]. Available from: http://www.linkinghub Valmeseda-Castellon.elsevier.com/retrieve/pii/0278239187900802 . [DOI] [PubMed]
- 5.Pichler JW, Beirne OR. Lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery: A systematic review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:395–401. doi: 10.1067/moe.2001.114154. [DOI] [PubMed] [Google Scholar]
- 6.Pogrel MA, Goldman KE. Lingual flap retraction for third molar removal. J Oral Maxillofac Surg. 2004;62:1125–30. doi: 10.1016/j.joms.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Gomes AC, Vasconcelos BC, de Oliveira e Silva ED, da Silva LC. Lingual nerve damage after mandibular third molar surgery: A randomized clinical trial. J Oral Maxillofac Surg. 2005;63:1443–6. doi: 10.1016/j.joms.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 8.Valmeseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Lingual nerve damage after third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:567–73. doi: 10.1067/moe.2000.110034. [DOI] [PubMed] [Google Scholar]
- 9.Mason DA. Lingual nerve damage following lower third molar surgery. Int J Oral Maxillofac Surg. 1988;17:290–4. doi: 10.1016/s0901-5027(88)80005-5. [DOI] [PubMed] [Google Scholar]
- 10.Kipp DP, Goldstein BH, Weiss WW., Jr Dysesthesia after mandibular third molar surgery: A retrospective study and analysis of 1377 surgical procedures. J Am Dent Assoc. 1980;100:185–92. doi: 10.14219/jada.archive.1980.0074. [DOI] [PubMed] [Google Scholar]


