Abstract
Background and Purpose
Advances in the management of acute ischemic stroke and medical imaging are creating pressure to replace the rigid one-third middle cerebral artery (MCA) and non-contrast-enhanced CT (NCCT) Alberta Stroke Program Early CT Score (ASPECTS) thresholds used for the selection of patients eligible for intravenous thrombolytic therapy. The identification of potentially salvageable ischemic brain tissue lies at the core of this issue. In this study, the role of CT perfusion ASPECTS in the detection of reversible ischemia was analyzed.
Materials and Methods
We retrospectively reviewed the clinical and imaging data of 92 consecutive patients who received intravenous thrombolytic therapy for acute (duration <3 h) ischemic stroke. Most of the patients underwent admission multimodal CT, and all patients had follow-up NCCT at 24 h. ASPECTS was assigned to all modalities and correlated with clinical and imaging parameters. Receiver-operating characteristic curve analysis was performed to determine optimal thresholds for different parameters to predict clinical outcome.
Results
A perfusion defect could be detected in 50% of the patients. ASPECTS correlated inversely with the clinical outcome in the following order: follow-up NCCT > cerebral blood volume (CBV) > mean transit time (MTT) > admission NCCT. The follow-up NCCT and the CBV displayed a statistically significant difference from the admission NCCT, while the MTT did not reach statistical significance. The threshold that best differentiated between good and bad clinical outcome on admission was CBV ASPECTS ≥7. In patients with CT perfusion ASPECTS mismatch, MTT and CBV ASPECTS essentially provided the lower and upper limits for the follow-up NCCT ASPECTS, thus defining the spectrum of possible outcomes. Furthermore, CT perfusion ASPECTS mismatch strongly correlated (r = 0.83) with the mismatch between the tissue at risk and the final infarct, i.e. the amount of salvaged tissue. This finding suggests that the CT perfusion ASPECTS mismatch adequately identifies the amount of potentially salvageable ischemic brain tissue.
Conclusions
Parameters derived from the use of CT perfusion ASPECTS can detect reversible ischemia and are correlated with clinical outcome.
Key Words: ASPECTS, Computed tomography, Perfusion, Stroke, Thrombolytic therapy
Introduction
The role of CT perfusion (CTP) in the decision to administer thrombolytic therapy with intravenous recombinant tissue plasminogen activator (rtPA) remains controversial. Research initiatives have been proposed to establish a sufficient body of evidence that would allow formal clinical guidelines to be composed [1]. At the core of this dilemma lie the detection of the ischemic penumbra and the infarct core and the implications this information should have for clinical decision making. Previous studies suggest that CTP can provide an estimate of the amount of potentially salvageable, acutely ischemic brain tissue and that the resulting CTP parameters provide an independent prognostic factor of the clinical outcome [2, 3, 4, 5, 6]. CTP also seems to increase diagnostic performance in stroke diagnosis and inter- and intraobserver agreement [7].
The Alberta Stroke Program Early CT Score (ASPECTS) is a semiquantitative, weighted scoring system that was developed to overcome the difficulties in the application of the non-contrast-enhanced CT (NCCT) one-third middle cerebral artery (MCA) rule that is used to select patients eligible for intravenous thrombolytic therapy [8]. ASPECTS is predictive of clinical outcome and hemorrhagic complications but is not sufficiently accurate in the triage of thrombolysis candidates [9, 10, 11]. Applying ASPECTS to CTP parametric maps has been suggested to be more reliable in both detecting reversible ischemia and predicting clinical outcome [12, 13, 14, 15].
We retrospectively reviewed the clinical and imaging data of 92 consecutive patients who received intravenous thrombolytic therapy for acute (duration <3 h) ischemic stroke in order to study the potential of CTP ASPECTS in the detection of reversible ischemia. We hypothesized that CTP ASPECTS mismatch [16], the difference between the mean transit time (MTT) and cerebral blood volume (CBV) map scores, might be useful in identifying patients who potentially benefit from thrombolytic therapy.
Materials and Methods
Overview
We retrospectively analyzed the clinical and imaging data of 92 consecutive patients who were admitted to Tampere University Hospital between January 2007 and December 2007 because of acute (duration <3 h) stroke symptoms and who received intravenous rtPA for the treatment of acute ischemic stroke after evaluation. In total, 271 patients suffering from acute ischemic stroke were evaluated as candidates for thrombolytic therapy during this period of time. The initial imaging evaluation of stroke patients consisted of NCCT, CT angiography (CTA) and CTP. The selection of patients eligible for thrombolytic therapy was based on institutional guidelines that did not have CTP or CTA parameters as exclusion or inclusion criteria. Still, we reviewed patient records of 179 patients who did not receive thrombolytic therapy in order to detect possible selection bias caused by CTP studies. The indications to exclude a patient from thrombolytic therapy had been carefully documented. In 1 case, the decision to exclude the patient was based on the results of a CTP study (extremely poor technical quality of the admission NCCT and over one third MCA lesions in the CBV map). In addition, we discovered 3 cases in which the admission NCCT was initially erroneously interpreted as negative and the results were reported orally to the stroke neurologist, followed by a review and a correction after the CTP maps had been calculated and analyzed some minutes later, with the result that the decision to administer thrombolytic therapy was withdrawn.
A full multimodal imaging evaluation was successfully completed in 72 of the 92 patients who received thrombolytic therapy. Nine patients were evaluated with NCCT alone and 11 patients with NCCT and CTA because of previously known contrast agent hypersensitivity, chronic renal failure, imminent closure of the 3-hour time window, or movement artifacts that rendered some of the imaging data not evaluable. A standard rtPA administration scheme was used: a total dose of 0.9 mg/kg Actilyse (Boehringer-Ingelheim, Ingelheim, Germany) was administered, with 10% given as a bolus and the remaining 90% as a continuous infusion for 1 h. A follow-up NCCT was performed for all patients 24 h after the administration of the thrombolytic agent. National Institutes of Health Stroke Scale (NIHSS) scores were assessed on admission and 24 h after the thrombolytic therapy. The modified Rankin Scale (mRS) was evaluated preictally and on day 90. The clinical data were stored (prospectively) in the patient records during the hospital stay and on day 90 after the ictus, the latter following a phone interview. These data were collected from the patient records and critically reviewed for errors using the data available from all medical and related disciplines (J.T.S.). The study was approved by the Tampere University Hospital Ethics Committee.
Imaging Parameters
CT scans were obtained using two different multidetector scanners: the General Electrics LightSpeed 16-slice scanner (GE Healthcare, Milwaukee, Wisc., USA) and the Philips Brilliance 64-slice scanner (Philips, Cleveland, Ohio, USA). Brain NCCT was performed using the parameters 120 kV, 430 mA, collimation 12 × 1.25 mm, and rotation 1.5 s (64-slice scanner), or 120 kV, 320 mA, collimation 16 × 1.25 mm, and rotation 1 s (16-slice scanner). Contiguous slices were reconstructed to the thickness of 5 mm in the whole scanning range (64-slice scanner) or to the thickness of 5 mm in the skull base and 7.5 mm in the supratentorial region (16-slice scanner). CTA was performed using a scanning range extending from the C2 vertebra to the vertex of the skull. The imaging parameters were 120 kV, 212 mA (using dynamic tube current modulation), collimation 64 × 0.625 mm, rotation 0.75 s, and pitch factor 0.923 (64-slice scanner), or 120 kV, 160 mA, collimation 16 × 0.625 mm, rotation 0.8 s, and pitch factor 0.938 (16-slice scanner). Contiguous slices were reconstructed to the thickness of 0.9 mm with a 0.45-mm overlap (64-slice scanner) or to the thickness of 1.25 mm (16-slice scanner). The contrast agent (iobitridol 350 mg I/ml; Xenetix, Aulnay-sous-Bois, France) was administered via an antecubital vein with an 18-gauge cannula using a double-piston power injector with a flow rate of 4 ml/s and 70 ml of contrast agent followed by a 50-ml saline flush. Manual bolus triggering was used. CTP was performed using the parameters 80 kV, 200 mA (effective), collimation 32 × 1.25 mm, and rotation 0.4 s (64-slice scanner), or 80 kV, 200 mA, collimation 8 × 2.5 mm, and rotation 1 s (16-slice scanner). 120 slices covering a range of 80 mm were generated in 55 s using an alternating jog protocol, i.e. shuttle mode (64-slice scanner), or 200 slices covering a range of 20 mm were generated in 50 s with a stationary gantry position (16-slice scanner). Contiguous slices were reconstructed to a thickness of 10 mm (64-slice scanner) or 5 mm (16-slice scanner) at even time intervals. The imaging range was positioned so that the ASPECTS planes [8] were always covered. The rest of the 80-mm range (64-slice scanner) was positioned both cranial and caudal to the ASPECTS planes with the exact balancing depending on the clinical presentation. The contrast agent (Xenetix 350 mg I/ml) was administered via an antecubital vein with an 18-gauge cannula using a double-piston power injector with a flow rate of 5 ml/s and 60 ml of contrast agent followed by a 40-ml saline flush.
Image Analysis
NCCT examinations were reviewed using dedicated medical imaging workstations. CTA and CTP images were analyzed, and areas and volumes were measured with Advantage Workstation version 3.2 (GE Healthcare). Parametric perfusion maps – MTT, cerebral blood flow, and CBV – were generated with the CT Perfusion 3 software that uses a deconvolution-based algorithm. CTA images were reviewed by examining both the raw data and maximum intensity projection images.
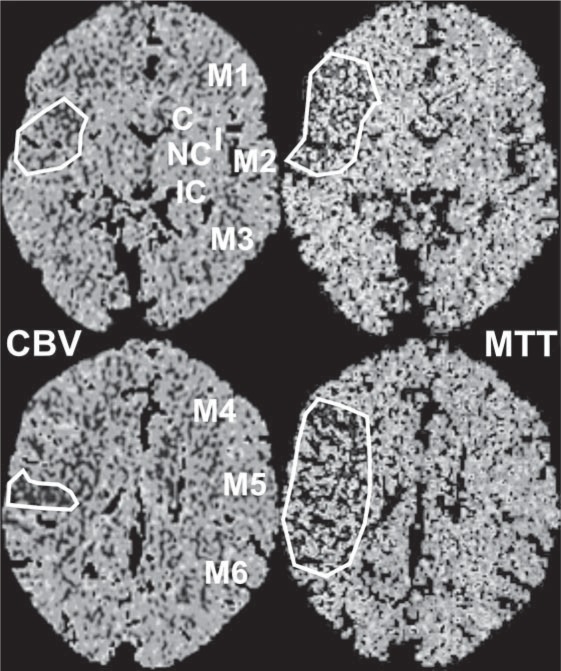
The principles of ASPECTS scoring in NCCT and CTP maps and the evaluation of CTP ASPECTS mismatch have been described in previous studies [8, 12, 15]. In short, each hemisphere is divided into 10 regions in 2 axial planes at the level of the basal ganglia and corona radiata (fig. 1). Each of these regions has a score of 1 point. This point is deducted if that region has ischemic changes. Thus, a negative finding yields a score of 10, and extensive ischemia covering the whole MCA region yields a score of 0.
Fig. 1.
CTP ASPECTS mismatch in a patient suffering from acute ischemia in the right MCA territory. In the CBV maps, ASPECTS areas I, M2, and M5 are affected (CBV ASPECTS = 7), whereas in the MTT maps areas I, M1, M2, M4, M5, and M6 display a perfusion defect (MTT ASPECTS = 4). Thus, CTP ASPECTS mismatch = 3.
MTT maps were used to detect tissue at risk, and CBV maps were used to approximate the infarct core [4]. The calculation of CTP ASPECTS mismatch is described in figure 1. We adopted a semiquantitative approach where the presence of a perfusion defect was determined visually from color-coded maps by comparing the appearance of the affected location with that of the healthy tissue on the contralateral side. In order to increase measurement accuracy and based on theoretical considerations, the area in the visually identified location was required to measure >25 mm2 with a mean MTT >7 s (or mean CBV <2.5 ml/100 g, correspondingly). NCCT and CTP ASPECTS were assigned by two radiologists (N.S. and A.L.). In cases where the scoring differed, a consensus score was agreed on. This score was correlated with the original findings of an experienced neuroradiologist, and if significant discrepancies were present, this neuroradiologist was further consulted. The examinations were reviewed in the order NCCT, CTA, and finally CTP, paralleling that of the clinical work flow. The reviewers were blinded to the clinical data apart from the side and nature of the acute symptoms. Perfusion defect areas and final infarct volumes were measured by one radiologist (N.S.). The boundaries of the affected areas were determined visually, and absolute value thresholds described above were applied. Volume was calculated by multiplying the measured area with the slice thickness. Intraclass correlation coefficients (ICC) between a staff radiologist (N.S.) and an experienced neuroradiologist (J.H.) were calculated for ASPECTS assignments in a test sample (n = 20): ICCNCCT = 0.86, ICCMTT = 0.79, ICCCBV = 0.73, and ICCNCCT 24 h = 0.93. Median interobserver agreement indices for areas and volumes were AreaMTT: 68%, AreaCBV: 90%, and VolumeINFARCT: 80%.
Statistics
Data were analyzed with SPSS version 17 (SPSS Inc., Chicago, Ill., USA). Pearson correlation coefficients and 2-tailed significance levels were calculated in all correlation analyses. Receiver-operating characteristic curves (ROC) were computed and Youden indices were evaluated to select optimal threshold values for imaging parameters to predict dichotomized good clinical outcome. After the dichotomization of the imaging parameters based on the threshold values, the data were cross tabulated and significance levels were calculated using Fisher's exact test. Differences between correlation coefficients and ROC area under the curves (AUCs) were studied with Steiger's Z test and the Hanley-McNeil procedure, respectively. Sensitivity, specificity, and confidence interval calculations were performed using standard procedures. In the text and the illustrations, the following notation is used to denote the level of statistical significance: * p < 0.05, ** p < 0.01 and *** p < 0.001. If p ≥ 0.01, the precise p value is given.
Results
Baseline Characteristics and Validation of the Scoring System
The median age of the patients was 71 years (interquartile range 58–80 years, 42 female). Based on the clinical features and the imaging studies, in 11 of the 92 patients evaluated, the ischemic episode involved the posterior circulation (8 cases of thrombosis of the basilar artery). The rest of the episodes were considered to involve the anterior circulation. The thrombosis could be demonstrated with CTA in 37 cases (45% of the CTA studies and 40% of all patients). In 40 (56%) of the 72 patients evaluated with CTP, a perfusion defect could be detected in the ASPECTS planes. An additional 6 perfusion defects were found outside the ASPECTS planes. A perfusion pattern implying acute ischemia could be detected in half of the cases involving the posterior circulation when CTP was performed. In total, a perfusion defect could be demonstrated in 64% of the CTP studies (50% of all patients). The median NIHSS on admission was 7 points (56.0% had NIHSS <8, 18.7% had NIHSS >15, interquartile range 4–12), and 24 h later the median NIHSS was 2 points. The median mRS was 1 point preictally and 2 points 3 months later. The median change in mRS (ΔmRS) was 1 point. 74.4% of the patients experienced a favorable clinical outcome at 3 months (mRS ≤2). At 24 h, a local hemorrhagic complication (HI1, HI2, PH1, or PH2) was detected in 6 cases (6.5%), and 4 patients (4.4%) had parenchymal hemorrhage distant to the site of the infarct (PHr1 or PHr2). In order to validate the ASPECTS scoring method, we studied the correlations between CTP and NCCT ASPECTS, and the area and the volumetric data acquired from the perfusion maps and the NCCT images. ASPECTS for CBV and MTT were inversely correlated with the perfusion defect areas with r = −0.87*** and r = −0.91***, respectively. The correlation between the CTP ASPECTS mismatch and the measured mismatch area was r = 0.77***. As expected, the infarct volume correlated with ΔmRS (r = 0.54***) as did NIHSS on admission (r = 0.35**).
CTP ASPECTS Parameters Correlate with Final Infarct Volume and Clinical Outcome
In order to assess the prognostic performance, we studied the correlations between different ASPECTS parameters, the final infarct volume, and the clinical outcome, which we measured with ΔmRS. First, we studied the overall performance of the ASPECTS scoring method systematically applied to all patients identified as candidates for thrombolytic therapy based on clinical features, including patients with a subsequently diagnosed posterior circulation stroke (table 1, ‘all patients’). The final infarct volume correlated inversely with all ASPECTS, with the 24-hour follow-up NCCT having the highest correlation, as expected. Also the other scores displayed statistically significant correlations in the order CBV > NCCT0 h > MTT, with NCCT0 h and MTT having close to equal correlation coefficients. This pattern is reflected in the clinical outcome, where the correlations were ordered NCCT24 h > CBV > MTT > NCCT0 h, with CBV having a correlation coefficient almost equal to that of NCCT24 h. In general, the correlations between ASPECTS and ΔmRS were weaker than those between ASPECTS and the infarct volume but still highly statistically significant. This pattern is mostly due to the inclusion of the ischemic events of the posterior circulation in the analysis, as the prognosis of these events is generally worse and ASPECTS is designed to detect disturbances in the anterior circulation. When only anterior circulation events are included in the analysis, the correlations between ASPECTS and ΔmRS are strengthened, while the order remains unchanged (table 1, ‘anterior circulation’).
Table 1.
Correlations between the NCCT and CTP ASPECTS scores and the final infarct volume and the clinical outcome (δmRS) for all patients, patients with anterior circulation ischemia, and patients with CTP ASPECTS mismatch
| Infarct volume |
δmRS |
|||
|---|---|---|---|---|
| corr. coeff. | vs. NCCT0 h | corr. coeff. | vs. NCCT0 h | |
| All patients (n = 92 for NCCT and n = 72 for CTP) | ||||
| NCCT0 h | r = −0.56*** | − | r = −0.25* | − |
| MTT | r = −0.56*** | p = 1.0 | r = −0.34** | p = 0.40 |
| CBV | r = −0.69*** | p = 0.07 | r = −0.48*** | p = 0.01* |
| NCCT24 h | r = −0.82*** | p < 0.001*** | r = −0.49*** | p = 0.01* |
| Anterior circulation (n = 81 for NCCT and n = 66 for CTP) | ||||
| NCCT0 h | r = −0.57*** | − | r = −0.34** | − |
| MTT | r = −0.58*** | p = 0.91 | r = −0.43*** | p = 0.41 |
| CBV | r = −0.70*** | p = 0.08 | r = −0.55*** | p = 0.02* |
| NCCT24 h | r = −0.85*** | p < 0.001*** | r = −0.65*** | p < 0.001*** |
| Patients with CTP ASPECTS mismatch (n = 36) | ||||
| NCCT0 h | r = −0.55** | − | r = −0.39* | − |
| MTT | r = −0.48** | p = 0.63 | r = −0.57*** | p = 0.12 |
| CBV | r = −0.66*** | p = 0.33 | r = −0.69*** | p = 0.01* |
| NCCT24 h | r = −0.84*** | p = 0.003** | r = −0.85*** | p < 0.001*** |
The final infarct volume and the clinical outcome correlated inversely with all ASPECTS scores, with the 24-hour follow-up NCCT having the highest correlation. All the correlation coefficients (corr. coeff.) were statistically significant. The correlations between the MTT and CBV ASPECTS scores and the clinical outcome are stronger than the correlation of the admission NCCT score and the clinical outcome, suggesting that CTP parameters may better classify reversible and non-reversible ischemia. However, only the CBV score displayed a statistically significant difference (p < 0.05) from the admission NCCT score in all the subgroups (vs. the NCCT0 h columns).
p < 0.05
p < 0.01
p < 0.001
CTP ASPECTS mismatch gives a single-digit estimate of the extent of reversible ischemia (fig. 1). In our data, a mismatch was present in 36 cases (39%). In an additional 4 patients, a perfusion mismatch was present in the ASPECTS planes but not within any ASPECTS subterritory. In the ASPECTS mismatch subgroup, the correlations between ASPECTS and the clinical outcome were higher than in the case of all patients or all anterior circulation events, while the correlations between ASPECTS and infarct volume remained similar (table 1, ‘patients with CTP ASPECTS mismatch’).
Overall, the correlations between the MTT and CBV scores and the clinical outcome are stronger than the correlation of the admission NCCT score and the clinical outcome, suggesting that CTP parameters may better classify reversible and non-reversible ischemia. However, only the CBV score displayed a statistically significant difference (p < 0.05) from the admission NCCT score in all the subgroups studied (table 1).
CTP ASPECTS Mismatch Identifies Potentially Salvageable Ischemic Tissue
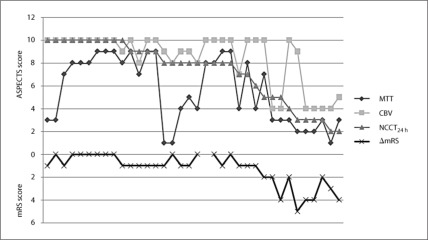
In figure 2, the MTT, CBV, and NCCT24 h ASPECTS scores and ΔmRS are plotted for each of the 36 patients with a CTP ASPECTS mismatch and sorted according to the NCCT24 h ASPECTS in descending order along the x-axis. Essentially, MTT and CBV provide the lower and upper limits for NCCT24 h, thus defining the spectrum of possible outcomes. The ΔmRS curve traces the contour of all the other curves; it lies most closely to the NCCT24 h curve, which can be expected considering the results of the correlation analysis.
Fig. 2.
The MTT, CBV, and NCCT24 h ASPECTS scores and ΔmRS are plotted for each of the 36 patients with a CTP ASPECTS mismatch >0 according to the NCCT24 h ASPECTS in descending order along the x-axis. The ΔmRS curve traces the contour of all the other curves; it lies most closely to the NCCT24 h curve. Essentially, MTT and CBV provide the lower and upper limits for NCCT24 h, thus defining the spectrum of possible outcomes.
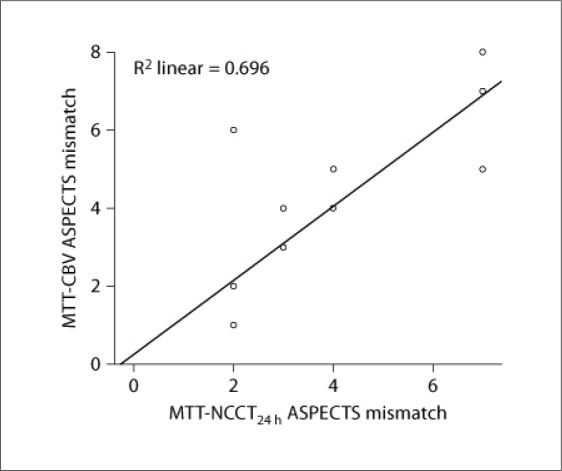
A mismatch between the NCCT24 h and the MTT ASPECTS scores can be used to estimate the amount of tissue salvaged, as MTT gives an estimate on the amount of tissue at risk and NCCT24 h depicts the size of the actual infarct. Thus, this mismatch parameter can be used as a surrogate for vessel recanalization. Dichotomizing ΔmRS with the condition ΔmRS ≤1 to signify good clinical outcome, the lowest statistically significant threshold for the MTT-NCCT24 h ASPECTS mismatch that predicted good clinical outcome was 2 (p = 0.04). Using this threshold as an indicator for total or partial vessel recanalization, in the subgroup of patients with MTT-NCCT24 h ASPECTS mismatch ≥2 (n = 17), this parameter and CTP ASPECTS mismatch are highly correlated (r = 0.83***) and have a strong linear relationship (R2 = 0.70, fig. 3). Overall, these findings suggest that the CTP ASPECTS mismatch adequately predicts the amount of potentially salvageable ischemic brain tissue.
Fig. 3.
The lowest statistically significant threshold for the MTT-NCCT24 h ASPECTS mismatch that predicted good clinical outcome was 2. Using this threshold as a marker indicating total or partial vessel recanalization, in the subgroup of patients with MTT-NCCT24 h ASPECTS mismatch ≥2 (n = 17), this mismatch and CTP ASPECTS mismatch are highly correlated (r = 0.83***) and have a strong linear relationship (R2 = 0.70). In the case of the outlier in the top left corner of the graph, the recanalization was partial or too late, allowing part of the tissue at risk to become infarcted, while the rest of the tissue at risk was salvaged.
CBV ASPECTS ≥7 Identifies Patients with Good Clinical Outcome
Table 2 demonstrates the thresholds for good clinical outcome (ΔmRS ≤1) for the CTP and NCCT ASPECTS scores derived from ROC. Overall, the most robust predictor of a good clinical outcome was the 24-hour follow-up NCCT score ≥8, which had 94% sensitivity and 65% specificity. However, CBV ≥7 performed well in identifying patients who had good clinical outcome and who potentially benefited from thrombolytic therapy. This threshold had 100% sensitivity, 44% specificity, and no patients with good clinical outcome in the CBV <7 partition. The thresholds MTT ≥4 (AUC = 0.68) and NCCT0 h ≥10 (AUC = 0.66), although statistically robust, were outperformed by CBV ≥7 (AUC = 0.72). The differences between AUCs did not yield statistical significance. However, in the case of MTT and NCCT0 h, the AUCs were below the 0.70 threshold, which is often considered as a cutoff value for an adequately performing diagnostic test. Patients with thrombosis of the basilar artery in the admission CTA were excluded from the analysis.
Table 2.
Threshold values for dichotomized NCCT and CTP ASPECTS parameters that best differentiate between good (ΔmRS ≤1) and bad clinical outcome
| Threshold | Good outcome | p value | RR (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | AUC |
|---|---|---|---|---|---|---|
| CBV ≥7 vs. <7 | 74 vs. 0% | <0.001 | n/a | 1.00 (0.93–1.00) | 0.44 (0.25–0.66) | 0.72 |
| MTT ≥4 vs. <4 | 68 vs. 6% | <0.001 | 11.5 (2.9–45.6) | 0.92 (0.81–0.97) | 0.5 (0.29–0.71) | 0.68 |
| NCCT0 h ≥10vs. <10 | 65 vs. 11% | 0.01 | 6.0 (3.2–11.3) | 0.86 (0.75–0.92) | 0.45 (0.26–0.66) | 0.66 |
| NCCT0 h ≥7vs. <7 | 75 vs. 1% | 0.04 | 62.0 (8.8–436.7) | 0.98 (0.92–1.00) | 0.15 (0.05–0.36) | 0.66 |
| NCCT24 h ≥8vs. <8 | 71 vs. 5% | <0.001 | 27.4 (7.0–107.5) | 0.94 (0.85–0.98) | 0.65 (0.43–0.82) | 0.83 |
ROC were devised to find the optimal threshold values. Overall, the most robust predictor of good clinical outcome was the 24-hour follow-up NCCT score ≥8. CBV ≥7 performed well in identifying patients who had good clinical outcome and who potentially benefited from thrombolytic therapy. The differences between the AUCs did not yield statistical significance for the admission imaging studies (CBV, MTT, and NCCT0 h). Patients with thrombosis of the basilar artery were excluded from the analysis.
RR = Risk ratio; CI = confidence interval; n/a = not available.
Discussion
We set off to study the performance of different quantitative parameters obtained using CTP ASPECTS that potentially have an impact on the choice of treatment in acute stroke. With 16- and 64-slice scanners, the axial dimension of the imaging volume is limited to 20–80 mm depending on the protocol used. This is not enough to cover the whole brain. Further, exact volumetric analysis of the perfusion maps requires user supervision, especially in the case of CBV, and is too slow a procedure to be used in the context of acute stroke imaging, which requires rapid online interpretation of the images. Thus, applying the ASPECTS scoring system to the perfusion images becomes an attractive option [12].
We decided to use the difference between the postictal and the preictal mRS as the indicator of good clinical outcome, as this better reflects the disease load inflicted by the current episode. As expected from the definitions, ΔmRS and 3-month mRS are highly correlated (r = 0.85***). Since poor preictal functional status is essentially a contraindication to thrombolytic therapy, the offset between ΔmRS and 3-month mRS is generally very small or nonexistent. The median preictal mRS in our research population was 1. The threshold for good clinical outcome was chosen to be ΔmRS ≤1 in order to maintain comparability to the traditional 3-month mRS ≤2 threshold.
All patients who received intravenous thrombolytic therapy in a period of 1 year were included in the baseline analysis regardless of the vascular territory affected in order to gain a realistic idea of the performance of the multimodal CT evaluation of stroke in a clinical setting. A perfusion defect could be detected in 50% of these patients, implying that with the technology used, a CT perfusion study could have an impact on half of the positive thrombolytic treatment decisions at the maximum. In total, 87% of the perfusion defects were present in either or both of the two ASPECTS planes. Those located outside the ASPECTS planes were detected by the 64-slice scanner in all but 1 case. The acute ischemic lesions that escape detection by CTP are mostly lacunar processes or are localized infratentorially or cranially to the perfusion study volume [17].
We hypothesized that CTP ASPECTS parameters predict the clinical outcome of patients who receive intravenous thrombolytic therapy better than the traditional admission NCCT. Correlation analyses with all patients and relevant subgroups support this hypothesis, as the CTP parameters correlate more closely with the clinical outcome when compared to the NCCT findings (table 1). However, only CBV displayed a statistically significant difference from NCCT, while MTT did not reach statistical significance. This is probably due to the heterogeneity introduced by cases in which thrombolytic therapy was effective and the MTT defect was totally or partially reversed. There was no statistically significant difference in the correlations between the admission CTP and NCCT parameters and the total infarct volume. This finding can be expected as the strength of the correlation between the infarct volume and the clinical outcome was only moderate (r = 0.54***), which probably reflects the presence of strategic infarcts that have a relatively small volume but have a considerable impact on the clinical outcome and often escape detection by the follow-up NCCT.
Optimally, the decision of administering thrombolytic therapy is based on the amount of salvageable brain tissue present. In the MCA region, this tissue volume is correlated with CTP ASPECTS mismatch [16]. In total, 39% of the patients presented with such a mismatch. We demonstrated that in patients who received thrombolytic therapy CTP ASPECTS mismatch adequately identifies the amount of potentially salvageable tissue (fig. 2, 3). However, small mismatches are difficult to interpret because of noise introduced by biological heterogeneity and errors in image analysis. In our data, a mismatch ≥2 was linked with good clinical outcome. A larger sample size is needed for a more accurate analysis.
Other notable limitations of this study are its retrospective design and non-excellent interobserver agreement in some imaging parameters, which, however, is comparable to that previously reported [13].
Finally, in the footsteps of previous investigators, we identified threshold values for dichotomized NCCT and CTP ASPECTS parameters that would best differentiate between good and bad clinical outcome. Our approach emphasized the sensitivity of identifying patients with potentially good outcome. While a statistically robust threshold could be devised for all the parameters studied, the threshold that performed best at presentation was CBV ≥7, which is in accordance with previous findings [12, 13, 14, 15]. However, thresholds 6 and 8 performed almost equally well, implying that relying on a single threshold value in decision making is probably ill advised. We also tested the established admission NCCT ASPECTS ≥7 threshold. This threshold proved to be very unspecific (Specificity 15%), which is to be expected as there were only patients who received thrombolytic therapy in our study population.
In conclusion, advances in the management of acute ischemic stroke and medical imaging and the extension of the time window for thrombolytic therapy are creating pressure to replace the rigid one-third MCA rule and non-contrast-enhanced CT ASPECTS thresholds in selecting patients to receive thrombolytic therapy with a shift toward identifying patients with potentially salvageable ischemic brain tissue. Our data suggest that parameters derived using ASPECTS scoring of CT perfusion images, especially the CTP ASPECTS mismatch, can in part answer these demands. Further, on admission, the ASPECTS of the CBV map correlates more strongly with clinical outcome than the NCCT ASPECTS.
Disclosure Statement
The authors have no conflict of interest.
Sources of Funding
This work was supported by the Tampere University Hospital Research Fund and the Oulu University Hospital Research Fund (H.R.).
References
- 1.Wintermark M, Albers GW, Alexandrov AV, Alger JR, Bammer R, Baron JC, Davis S, Demaerschalk BM, Derdeyn CP, Donnan GA, Eastwood JD, Fiebach JB, Fisher M, Furie KL, Goldmakher GV, Hacke W, Kidwell CS, Kloska SP, Köhrmann M, Koroshetz W, Lee TY, Lees KR, Lev MH, Liebeskind DS, Ostergaard L, Powers WJ, Provenzale J, Schellinger P, Silbergleit R, Sorensen AG, Wardlaw J, Wu O, Warach S. Acute stroke imaging research roadmap. AJNR Am J Neuroradiol. 2008;29:e23–e30. doi: 10.1161/STROKEAHA.107.512319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wintermark M, Reichhart M, Thiran JP, Maeder P, Chalaron M, Schnyder P, Bogousslavsky J, Meuli R. Prognostic accuracy of cerebral blood flow measurement by perfusion computed tomography, at the time of emergency room admission, in acute stroke patients. Ann Neurol. 2002;51:417–432. doi: 10.1002/ana.10136. [DOI] [PubMed] [Google Scholar]
- 3.Ezzeddine MA, Lev MH, McDonald CT, Rordorf G, Oliveira-Filho J, Aksoy FG, Farkas J, Segal AZ, Schwamm LH, Gonzalez RG, Koroshetz WJ. CT angiography with whole brain perfused blood volume imaging: added clinical value in the assessment of acute stroke. Stroke. 2002;33:959–966. doi: 10.1161/hs0402.105388. [DOI] [PubMed] [Google Scholar]
- 4.Wintermark M, Flanders AE, Velthuis B, Meuli R, van Leeuwen M, Goldsher D, Pineda C, Serena J, van der Schaaf I, Waaijer A, Anderson J, Nesbit G, Gabriely I, Medina V, Quiles A, Pohlman S, Quist M, Schnyder P, Bogousslavsky J, Dillon WP, Pedraza S. Perfusion-CT assessment of infarct core and penumbra: receiver operating characteristic curve analysis in 130 patients suspected of acute hemispheric stroke. Stroke. 2006;37:979–985. doi: 10.1161/01.STR.0000209238.61459.39. [DOI] [PubMed] [Google Scholar]
- 5.Silvennoinen HM, Hamberg LM, Lindsberg PJ, Valanne L, Hunter GJ. CT perfusion identifies increased salvage of tissue in patients receiving intravenous recombinant tissue plasminogen activator within 3 h of stroke onset. AJNR Am J Neuroradiol. 2008;29:1118–1123. doi: 10.3174/ajnr.A1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim JT, Yoon W, Park MS, Nam TS, Choi SM, Lee SH, Kim BC, Kim MK, Cho KH. Early outcome of combined thrombolysis based on the mismatch on perfusion CT. Cerebrovasc Dis. 2009;28:259–265. doi: 10.1159/000228256. [DOI] [PubMed] [Google Scholar]
- 7.Hopyan J, Ciarallo A, Dowlatshahi D, Howard P, John V, Yeung R, Zhang L, Kim J, MacFarlane G, Lee TY, Aviv RI. Certainty of stroke diagnosis: incremental benefit with CT perfusion over noncontrast CT and CT angiography. Radiology. 2010;255:142–153. doi: 10.1148/radiol.09091021. [DOI] [PubMed] [Google Scholar]
- 8.Pexman JH, Barber PA, Hill MD, Sevick RJ, Demchuk AM, Hudon ME, Hu WY, Buchan AM. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol. 2001;22:1534–1542. [PMC free article] [PubMed] [Google Scholar]
- 9.Dzialowski I, Hill MD, Coutts SB, Demchuk AM, Kent DM, Wunderlich O, von Kummer R. Extent of early ischemic changes on computed tomography (CT) before thrombolysis: prognostic value of the Alberta Stroke Program Early CT Score in ECASS II. Stroke. 2006;37:973–978. doi: 10.1161/01.STR.0000206215.62441.56. [DOI] [PubMed] [Google Scholar]
- 10.Weir NU, Pexman JH, Hill MD, Buchan AM, CASES investigators How well does ASPECTS predict the outcome of acute stroke treated with IV tPA? Neurology. 2006;67:516–518. doi: 10.1212/01.wnl.0000228221.44334.73. [DOI] [PubMed] [Google Scholar]
- 11.Puetz V, Dzialowski I, Hill MD, Demchuk AM. The Alberta Stroke Program Early CT Score in clinical practice: what have we learned? Int J Stroke. 2009;4:354–364. doi: 10.1111/j.1747-4949.2009.00337.x. [DOI] [PubMed] [Google Scholar]
- 12.Parsons MW, Pepper EM, Chan V, Siddique S, Rajaratnam S, Bateman GA, Levi CR. Perfusion computed tomography: prediction of final infarct extent and stroke outcome. Ann Neurol. 2005;58:672–679. doi: 10.1002/ana.20638. [DOI] [PubMed] [Google Scholar]
- 13.Aviv RI, Mandelcorn J, Chakraborty S, Gladstone D, Malham S, Tomlinson G, Fox AJ, Symons S. Alberta Stroke Program Early CT Scoring of CT perfusion in early stroke visualization and assessment. AJNR Am J Neuroradiol. 2007;28:1975–1980. doi: 10.3174/ajnr.A0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kloska SP, Dittrich R, Fischer T, Nabavi DG, Fischbach R, Seidensticker P, Osada N, Ringelstein EB, Heindel W. Perfusion CT in acute stroke: prediction of vessel recanalization and clinical outcome in intravenous thrombolytic therapy. Eur Radiol. 2007;17:2491–2498. doi: 10.1007/s00330-007-0696-9. [DOI] [PubMed] [Google Scholar]
- 15.Lin K, Rapalino O, Law M, Babb JS, Siller KA, Pramanik BK. Accuracy of the Alberta Stroke Program Early CT Score during the first 3 hours of middle cerebral artery stroke: comparison of noncontrast CT, CT angiography source images, and CT perfusion. AJNR Am J Neuroradiol. 2008;29:931–936. doi: 10.3174/ajnr.A0975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin K, Rapalino O, Lee B, Do KG, Sussmann AR, Law M, Pramanik BK. Correlation of volumetric mismatch and mismatch of Alberta Stroke Program Early CT Scores on CT perfusion maps. Neuroradiology. 2009;51:17–23. doi: 10.1007/s00234-008-0454-y. [DOI] [PubMed] [Google Scholar]
- 17.Eckert B, Küsel T, Leppien A, Michels P, Müller-Jensen A, Fiehler J: Clinical outcome and imaging follow-up in acute stroke patients with normal perfusion CT and normal CT angiography. Neuroradiology 2010, E-pub ahead of print. [DOI] [PubMed]