Abstract
OBJECTIVE
To compare the effectiveness of group resistance and agility training programs in reducing fall risk in community-dwelling older women with low bone mass.
DESIGN
A randomized, controlled, single-blinded 25-week prospective study with assessments at baseline, midpoint and trial completion.
SETTING
Community centre.
PARTICIPANTS
Community-dwelling women aged 75–85 years with low bone mass.
INTERVENTION
Participants were randomly assigned to one of three groups: Resistance Training (n=32), Agility Training (n=34), and Stretching (sham) exercises (n=32). The exercise classes for each study arm were held twice weekly.
MEASUREMENTS
The primary outcome measure was fall risk (derived from weighted scores from tests of postural sway, reaction time, strength, proprioception, and vision), as measured by a physiological profile assessment (PPA). Secondary outcome measures were ankle dorsiflexion strength, foot reaction time and the Community Balance and Mobility (CB&M) Scale.
RESULTS
Attendance at the exercise sessions for all three groups was excellent: Resistance Training (85.4%), Agility Training (87.3%) and Stretching program (78.8%). At the end of the trial, PPA fall risk scores were reduced by 57.3% and 47.5% in the Resistance and Agility training groups respectively, but by only 20.2% in the Stretching group. In both the Resistance and Agility groups, the reduction in falls risk was mediated primarily by improved postural stability, where sway was reduced by 30.6% and 29.2% respectively. There were no significant differences among the groups for the secondary outcomes measures. Within the Resistance Training group reductions in sway were significantly associated with improved strength as assessed by increased squat load used in the exercise sessions.
CONCLUSION
These findings support the implementation of community-based resistance and agility training programs to reduce fall risk in older women with low bone mass. Such programs may have particular public health benefits as it has been shown that this group are at increased risk of falling as well as sustaining fall-related fractures.
Keywords: Accidental Falls, Fall Risk, Exercise, Aged, Low Bone Mass
INTRODUCTION
Falls are a relatively common event in older people. Approximately 30% of individuals over 65 years of age fall at least once a year, and about half of those do so recurrently. Fall-related injuries and death in older people are a major health care problem worldwide, with the numbers continuing to rise 1. Thus, falls prevention in older people remains a major health care priority.
Falls are not random events 2 and occur, at least in part, due to physiological impairments, such as impaired balance, muscular weakness, and slowed reaction time 3. Exercise can effectively reduce both fall risk factors and falls in older people by ameliorating physiological impairments. For example, Lord et al. 4 demonstrated that a community-based general exercise program improved balance, muscular strength, and reaction time in older women. Furthermore, both Tai Chi Quan 5 and a home-based strength and balance training program 6 have reduced the incidence of falls in community-dwelling older adults. However, exercise comes in many forms, and further research is needed to delineate the specifics of exercise prescription for optimal fall risk and falls reduction. Defining the components of exercise that are effective in reducing fall risk would provide some insight as to the possible underlying mechanisms by which exercise exerts its effect and allow those prescribing exercise to do so more effectively.
Fractures, especially of the hip, are particularly disabling consequences of falling 7. One group of individuals at particularly high risk of sustaining fall-related fractures are those with low bone mass. For example, each standard deviation decrease in femoral neck bone density increases the age-adjusted risk of hip fracture 2.6 times 8. Furthermore, older women with osteoporosis may have a greater risk of falling due to greater impairments in balance and muscular strength compared with age-matched counterparts without osteoporosis 9. Thus, exercise programs aimed at reducing fall risk and falls may be particularly important for older people with low bone mass.
Recently, we conducted a randomized controlled trial that examined the effectiveness of a general exercise program in reducing fall risk in this population 10. This study found that low intensity strength, coordination and balance exercises were effective in improving strength and balance. In this paper we build on this work by conducting a 25-week, single-blinded, randomized controlled trial to compare the effectiveness of two types of community-based exercise programs (high-intensity resistance training and agility training) in reducing fall risk in community-dwelling older women with low bone mass.
METHODS
Study Design
We conducted a randomized, controlled 25-week prospective study with three measurement periods (baseline, midpoint, and trial completion). The assessors were blinded to the participants’ assignments.
Participants
We identified all women aged 75 to 85 years who were residents of greater Vancouver and in whom osteoporosis or osteopenia had been diagnosed at the BC Women’s Hospital and Health Centre (defined as a T-score at the total hip or spine at least 1.0 standard deviations below the young normal sex-matched areal bone mineral density of the Lunar reference database) 11 as potential participants. In addition, the Osteoporosis Society of Canada, BC section, provided a list of individuals with low bone mass who had provided permission to be approached for research studies. Six hundred and eighty-three letters of recruitment were mailed to the women identified from these databases. Local newspaper, radio, and poster advertisements were also used to aid in recruitment. Low bone mass was confirmed in participants recruited in this manner with a dual-energy X-ray absorptiometry (DXA) bone mineral density scan.
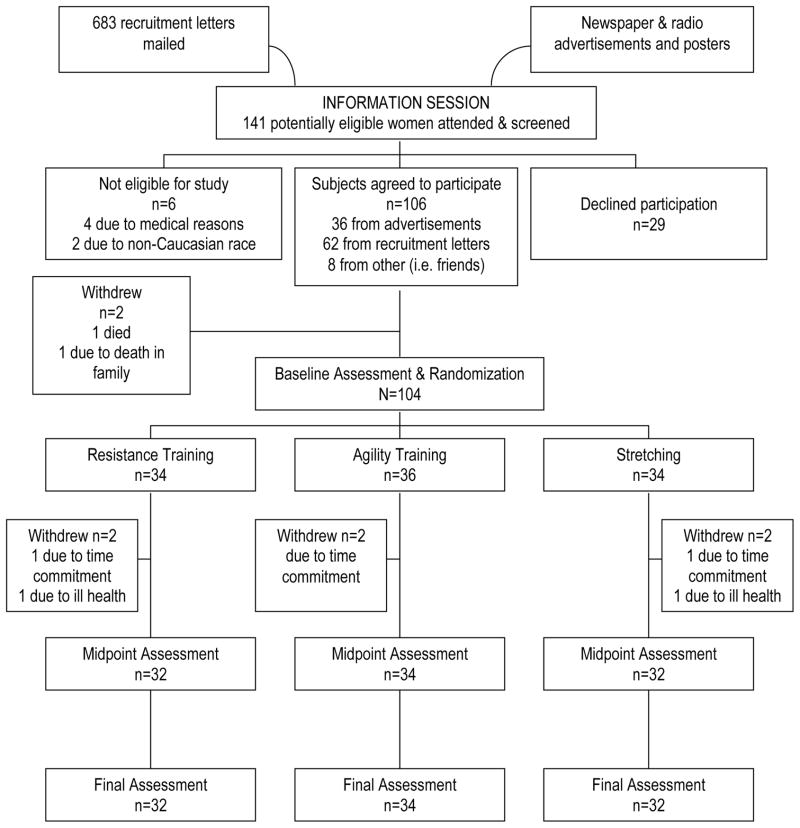
Interested individuals were screened by a standardized telephone interview, which included the revised physical activity readiness (Par-Q) questionnaire 12,13, and were then invited to an information session where a physician (KMK) assessed all potential participants. We excluded women who were: living in care facilities, of non-Caucasian race, regularly exercising twice weekly or more, had a history of illness or a condition that would affect balance (i.e. stroke and Parkinson’s disease), were unable to safely participate in our exercise program, or had a Mini Mental State Examination (MMSE) 14 score of < 23. Figure 1 shows the number of participants in the treatment arms at each the stage of the study (FIGURE 1).
Figure 1.
Flow Chart Outlining Number of Participants in Each Study Arm.
The study was approved by the University of British Columbia Clinical Research Ethics Board and the Research Committee of the Children’s and Women’s Hospital of British Columbia. All participants gave written informed consent prior to participating in the study.
Descriptive Variables
We measured age in years, standing height in centimetres, and mass in kilograms in all participants. General health was assessed with questions from the Canadian Multicentre Osteoporosis Study (CaMOS) questionnaire 15 that relate to current medication use, current supplement use, the presence of medical conditions known to be fall risk factors (such as osteoarthritis), and history of falls. This questionnaire was administered at baseline by trained interviewers. As well, all participants underwent a physician assessment to confirm health status and walking aid use was also recorded.
Cognitive state was assessed using the Mini-Mental State Examination 14. Each participant’s current level of physical activity was determined at the three measurement periods with the Physical Activities Scale for the Elderly (PASE) questionnaire 16,17. Visual acuity, both high and low contrast, was assessed at a test distance of three meters 18. Corrected acuity was determined binocularly and measured in terms of the minimum angle resolvable in minutes of arc. Tactile sensitivity was assessed with a pressure aesthesiometer 18. Filaments of varying thickness were applied to the center of the lateral malleolus and measurements are expressed in logarithms of milligrams pressure.
Adherence with the assigned exercise program was recorded for each participant and expressed as the percentage of the 48 classes (maximum number of classes) attended. All 98 participants were asked to keep a falls diary throughout the intervention period.
Primary Outcome Measure
Participant’s fall risk was assessed at the three measurement periods using the Physiological Profile Assessment (PPA) © 18 (Prince of Wales Medical Research Institute, Randwick, Sydney, NSW, Australia). The PPA is a valid 19,20 and reliable 21 tool for assessing fall risk in older people. Based on the performance of five physiological domains (vision, proprioception, strength, reaction time and balance), the PPA computes a fall risk score (standardized score) for each individual and this measure has a 75% predictive accuracy for falls in older people 19,20. Standardised weightings for each of the five components were derived from a discriminant function for predicting multiple falls from the Randwick Falls and Fractures Study 20. These weightings (canonical correlation coefficients) were −0.33 for edge contrast sensitivity, 0.20 for lower limb proprioception, −0.16 for isometric quadriceps strength, 0.47 for hand reaction time and 0.51 for postural sway on a compliant foam rubber surface. Fall risk scores below 0 indicate a low risk of falling, scores between 0 and 1 indicate a mild risk of falling, scores between 1 and 2 indicate a moderate risk of falling and scores above 2 indicate a high risk of falling. Table 1 describes the tests from the short-form PPA assessment (TABLE 1).
Table 1.
PPA Short-Form Assessment.
| PPA Task | Description | Measure |
|---|---|---|
| Postural Sway | Individuals were asked to stand as still as possible for 30 seconds on 15cm thick medium-density foam rubber mat with their eyes open, wearing the Lord swaymeter 20. The device consists of a 40-cm long rod with a vertically mounted pen at its end. The rod is attached to the participants by a firm belt and extends posteriorly. The pen records sway on a sheet of millimetre graph paper fastened to the top of an adjustable height table. | Total sway path (mm) was determined from the path traced. |
| Quadriceps Strength | A simple strain gauge was used to assess dominant quadriceps (isometric) strength to the nearest 0.5 kilogram. Participants were seated with the hip and the knee joint at 90 degrees of flexion. | The best of three trials (kg). |
| Hand Reaction Time | Used a light as the stimulus and depression of a switch by the finger as the response. | The average of 10 trials (msec). |
| Proprioception | Seated participants with eyes closed were asked to align the lower limbs on either side of a 60 by 60 cm by 1-cm-thick clear acrylic sheet standing on edge and inscribed with a protractor. | The difference (deg) in matching the great toes. |
| Edge Contrast Sensitivity | The Melbourne Edge Test was used to assess this aspect of visual function. This test presents 20 circular patterns containing edges with reducing contrast. Correct identification of the orientation of the edge on the patches provides a measure of contrast sensitivity in decibel units (dB), where dB=−10log10 contrast. | Number of the last correctly identified circle (dB). |
Secondary Outcome Measures
Secondary outcome measures were included to assess lower limb function in domains not assessed by the short-form PPA as well as a measure of overall general balance and mobility. Isometric ankle dorsiflexion was assessed in a seated position with the foot secured to a footplate and the angle of the knee positioned at 120 degrees. In three trials, the subject attempted maximal dorsiflexion of the ankle and the greatest force was recorded 18. Foot reaction time was assessed with a light as a stimulus and a foot-press as the response 18. General balance and mobility was assessed using the Community Balance and Mobility Scale (CB&M Scale) 22. This scale is a performance-based balance and mobility measure consisting of 12 items each rated at a 5-point scale (85 points maximum). It includes items such as timed single leg stand, tandem walking, and stair mobility. This scale was chosen because present balance and mobility measures do not adequately assess higher levels functioning expected in community-dwelling older people 23,24. Test-retest reliability for the Community Balance Mobility Scale indicates a high agreement between tests with an ICC of 0.98. The internal consistency of the scale is also very high (Cronbach’s alpha=0.96) 22.
Randomization
After baseline measurement, participants were randomly assigned to one of three groups: Resistance Training, Agility Training, and Stretching (sham exercise). Randomization was stratified by baseline performance in postural sway.
Sample Size
The required sample size for this study was estimated based on predictions of 20%, 10%, and 0% change in the PPA’s fall risk score for the Agility Training group, the Resistance Training group, and the Stretching group respectively. Assuming a 30% attrition rate and using an alpha level of < 0.05, 30 participants per group ensured a power of greater than 0.80 to detect a 10% difference between groups.
Exercise Intervention
The exercise intervention began one week after the baseline measures were administered. Participants were required to attend their assigned exercise class twice weekly. All classes were held at a YMCA community centre and led by certified fitness instructors. The classes were 50 minutes in duration, with a 15-minute warm-up, 20 minutes of core content, and a 15-minute cool down. The instructor to participant ratio was 1:2 for the Resistance Training class, 1:3 for the Agility Training class, and 1:4 for the Stretching class. Attendance was recorded daily by the head instructor of each class.
Resistance Training
The protocol for the Resistance Training group was progressive and high-intensity in nature with the aims of increasing muscle strength in the extremities and trunk. Both a Keiser® Pressurized Air system (Keiser Corporation, Fresno, CA, USA) and free weights were used to provide the training stimulus. Participants underwent a 2-week familiarisation period with the equipment and the exercises. The Resistance Training exercises included: biceps curls, triceps extension, seated row, latissmus dorsi pull downs, mini-squats, mini-lunges, hamstring curls, calf raises, and gluteus maximus extensions on a mat.
The intensity of the training stimulus was initially set at 50% to 60% of 1RM (repetition maximum) as determined at week two, with a work range of two sets of 10–15 repetitions and progressed to 75% to 85% of 1RM at a work range of six to eight repetitions (two sets) by week four. The training stimulus was increased using the 7RM method 25, when two sets of six to eight repetitions were completed with proper form and without pain or discomfort. Squats, lunges, and gluteus maximum extensions, however, did not follow the above guideline. These three exercises were performed initially with body weight and loading was increased only when proper form was maintained for two sets of 10 repetitions. The number of sets completed and the load lifted for each exercise were recorded for each participant at every class.
Agility Training
The aims of the Agility Training protocol were to challenge: 1) hand-eye coordination, 2) foot-eye coordination, 3) dynamic balance, 4) standing and leaning balance and 5) psychomotor performance (reaction time). Ball games, relay races, dance movements, and obstacle courses were used to achieve these goals. A logbook was maintained detailing the content of each week’s classes and is available from the first author (TLA). Due to the potential risk of falls in the Agility Training class, participants were given KPH® (Tampere, Finland) hip protectors and all instructors provided very close supervision and ‘spotting’ as in gymnastics training.
Stretching (Sham Exercise)
The content of the Stretching classes consisted of stretching exercises, deep breathing and relaxation techniques, and general posture education. There is no evidence that these exercises reduce fall risk 26. This group served to control for confounding variables such as physical training received by traveling to the community centre for twice-weekly classes, social interaction and changes in lifestyle secondary to study participation.
Adverse Events
After each exercise session, participants were questioned about the presence of any adverse effects, such as musculoskeletal pain or discomfort. Modifications in training program were made on an individual basis as necessary. Any falls that occurred during the classes were recorded. All instructors also monitored participants for symptoms of angina and shortness of breath.
Statistical Analysis
The data were analysed on an intention to treat basis, using SPSS 27 statistical software. Variables that were not normally distributed (sway, hand and foot reaction time) were transformed using natural logarithm before comparisons between the groups were made. Comparisons of group characteristics and baseline scores were undertaken using a Chi Square test for differences in proportions and Students t-tests for differences in means. The falls risk scores, fall risk score components, secondary outcome variables, and PASE scores measured at the 13- and 25-week retests were compared by forced entry multiple linear regression analysis, with baseline scores and experimental group included as independent variables in the models. This analysis procedure provides a more precise indication of the treatment effect than provided by group by time ANOVAs 27. Post hoc analyses were then performed where there were significant main effects use Scheffe corrections. Multivariate analysis of variance (MANOVA) with repeated measures was used to examine whether there were changes in fall risk at the end of the trial compared with baseline and 3-months in the Agility and Resistance Training groups. In these analyses, polynomial contrasts were selected giving measures of linear and quadratic (i.e. non-linear or asymptotic) trends.
Finally, Pearson correlations were computed to determine if changes in the squat load normalized for body weight (load change/weight) between the beginning and at the end of the intervention period was related to reductions in postural sway in the Resistance Training group.
RESULTS
Descriptive Variables, Exercise Adherence and Physical Activity Levels
The mean age of the cohort was 79 (± 3) years. The three groups did not differ in any of the descriptive variables (TABLE 2). In the group as a whole, the adherence to the exercise classes was 83.3%. The Resistance Training group had an average compliance of 85.4%, 87.3% for the Agility Training group, and 78.8% for the Stretching group.
Table 2.
Descriptive Statistics for Descriptor Variables (N = 98).
| Variable* | Resistance (n=32) | Agility (n=34) | Stretching (n=32) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age (yr) | 79.6 (2.1) | 78.9 (2.8) | 79.5 (3.2) |
| Height (cm) | 160.10 (6.02) | 156.96 (6.09) | 158.27 (8.41) |
| Weight (kg) | 59.9 (9.4) | 62.5 (9.3) | 65.2 (12.6) |
| Prescribed Medications | 2.6 (2.3) | 3.2 (2.1) | 4.1 (3.3) |
| High Contrast Acuity† | 1.49 (0.88) | 2.38 (4.42) | 1.54 (0.56 |
| Low Contrast Acuity† | 2.62 (1.55) | 3.77 (4.74 | 2.86 (1.27) |
| Tactile Sensitivity‡ | 4.40 (0.51) | 4.28 (0.49) | 4.12 (0.56) |
| MMSE Score (max 30 points) | 28.7 (1.4) | 28.6 (1.4) | 28.3 (1.9) |
| Number of Classes Attended | 41.0 (9.4) | 41.9 (6.1 | 37.8 (10.1) |
| Baseline PASE | 98.00 (51.78) | 83.29 (35.07) | 76.30 (30.01) |
| Fall in Last 4 Weeks§ | 5 (15.6) | 1 (2.9) | 2 (6.3) |
| Osteoarthritis§ | 11 (34.4) | 13 (38.2) | 17 (53.1) |
| Osteoarthritis of the Knee§ | 5 (15.6) | 6 (17.6) | 6 (18.8) |
| Use of Walking Aid§ | 4 (12.5) | 2 (5.9) | 5 (15.6) |
There were no significant differences among the groups for any measure.
Measured in terms of the minimum angle resolvable in minutes of arc.
Measured in logarithms of milligrams pressure.
Count (%). Count=Number of “yes” cases within each group. % =Percent of “yes” cases within each group.
Physical activity levels (PASE scores) increased during the 25-week intervention period in all three groups (p=0.008). However, these changes did not differ significantly between the groups (p=0.60), and changes in PASE scores were not significantly related with changes in the primary or any secondary outcome measures (r≤0.114, p≥0.266).
PPA Fall Risk Score, Fall Risk Components and Secondary Outcome Measures
Table 3 shows the baseline, 13-week and 25-week retest results for the fall risk scores, fall risk score components and secondary outcome measures for the three study groups (TABLE 3). The regression analyses revealed a significant difference in one measure only (scores in the CB&M Scale) at the mid-point of the trial. Post-hoc test showed that the Agility Training group showed significant improvements in this measure compared with the other two groups.
Table 3.
Mean Values (SDs) for the Outcome Measures – Baseline, Midpoint, and Final (N = 98).
| Variable* | Baseline | Midpoint | Final |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Resistance (n=32) | |||
| Fall Risk Score | 2.22 (0.70) | 1.39 (0.98) | 0.95 (1.01)‡ |
| Postural Sway (mm) | 230.10 (93.09) | 183.60 (123.19) | 159.61 (81.95)§ |
| Quadriceps Strength (kg) | 17.2 (7.2) | 20.4 (8.4) | 18.9 (8.6) |
| Hand Reaction Time (msec) | 328.3 (44.3) | 284.1 (49.3) | 267.8 (52.3) |
| Proprioception (deg) | 2.2 (2.1) | 1.9 (1.0) | 1.5 (1.2) |
| Edge Contrast (dB) | 17.8 (2.1) | 19.3 (2.0) | 19.2 (2.2) |
| Dorsiflexion Strength (kg) | 6.4 (2.2) | 7.3 (2.6) | 7.6 (2.5) |
| Foot Reaction Time (msec) | 380.5 (81.6) | 320.1 (41.6) | 331.2 (63.9) |
| CB&M Scale (out of 85 points) | 44.6 (21.6) | 49.5 (20.7) | 51.2 (21.9) |
| Agility (n=34) | |||
| Fall Risk Score | 2.40 (0.86) | 1.49 (0.97) | 1.26 (0.93)‡ |
| Postural Sway | 219.20 (80.26) | 179.47 (98.06) | 155.26 (91.15)§ |
| Quadriceps Strength | 17.0 (6.5) | 19.9 (6.2) | 17.2 (7.9) |
| Hand Reaction Time | 337.8 (61.4) | 298.6 (53.6) | 294.9 (55.1) |
| Proprioception | 1.8 (1.2) | 1.8 (1.6) | 1.5 (1.2) |
| Edge Contrast | 17.3 (2.3) | 18.9 (2.1) | 18.7 (2.7) |
| Dorsiflexion Strength | 5.1 (2.6) | 7.3 (1.9) | 6.8 (2.9) |
| Foot Reaction Time | 379.0 (67.8) | 340.2 (68.1) | 353.9 (61.6) |
| CB&M Scale | 39.9 (17.5) | 51.5 (15.5)† | 48.9 (16.4) |
| Stretching (n=32) | |||
| Fall Risk Score | 1.92 (0.83) | 1.50 (0.95) | 1.53 (1.21) |
| Postural Sway | 216.97 (104.72) | 196.60 (122.94) | 217.35 (148.25) |
| Quadriceps Strength | 16.1 (7.2) | 19.2 (7.2) | 17.5 (6.4) |
| Hand Reaction Time | 307.6 (43.1) | 290.5 (49.1) | 280.7 (60.2) |
| Proprioception | 1.7 (0.9) | 2.0 (1.6) | 1.8 (1.2) |
| Edge Contrast | 18.0 (1.5) | 18.8 (1.8) | 18.6 (1.9) |
| Dorsiflexion Strength | 5.4 (2.9) | 6.4 (2.8) | 6.3 (2.4) |
| Foot Reaction Time | 362.8 (57.6) | 332.3 (49.8) | 345.2 (57.5) |
| CB&M Scale | 40.4 (18.3) | 45.8 (17.8) | 45.0(17.4) |
High fall risk scores, high sway values, high reaction time values, low quadriceps strength values, and low edge contrast scores indicate impaired performances. For the CB&M Scale (Community Balance and Mobility Scale), a higher score indicates better physical function.
Significantly different from the Resistance Training and the Stretching group at p<0.05.
Significantly different from the Stretching group at p<0.01.
Significantly different from the Stretching group at p<0.05.
At the end of the trial there were group differences for the fall risk score and postural sway on the compliant foam rubber mat. The groups did not differ on the remaining falls risk component or secondary outcome measures, although for both reaction time tasks, the associations approached statistical significance – hand reaction time (F2,94=2.49, p=0.09) and foot reaction time (F2,94=2.65, p=0.08).
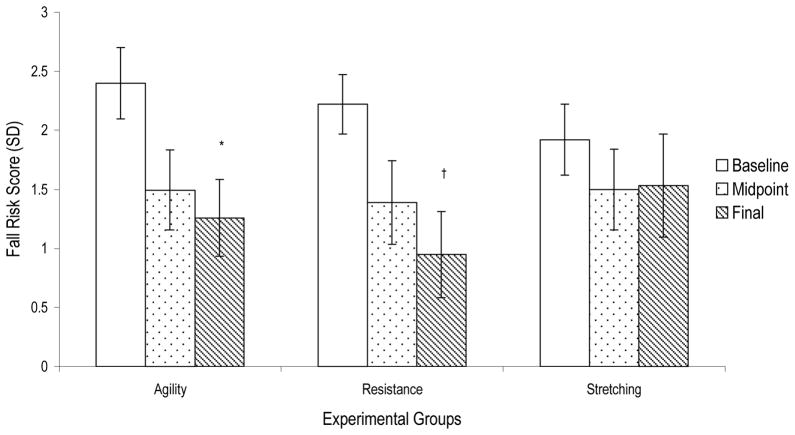
Post-hoc analyses indicated that both Resistance Training and Agility Training had significantly reduced fall risk scores compared with the Stretching group at the end of the intervention period. PPA fall risk scores were reduced by 57.3% and 47.5% in the Resistance and Agility Training groups respectively, but by only 20.2% in the stretching group. In both the Resistance and Agility groups, the reduction in falls risk was mediated primarily by improved postural stability, where sway was reduced by 30.6% and 29.2% respectively. In contrast, sway showed no significant change in the Stretching group (0.0%)
The Agility and Resistance training groups showed continued improvements in fall risk throughout the intervention period (FIGURE 2). The repeated measure MANOVA analysis indicated a significant linear contrast (p<0.001) and an insignificant quadratic contrast (p=0.15) for change in fall risk in the Resistance Training group. In the Agility Training group, there were significant linear (p<0.001) and quadratic contrasts (p<0.05), indicating that improvement beyond the mid-point of the trial was less marked.
Figure 2. Fall Risk Score.
*Significantly different from the Stretching group, p=0.005.
†Significantly different from the Stretching group, p=0.001.
Error bars represent 95% confidence intervals.
Changes in Squat Load and Sway in the Resistance Training Group
Over the trial period, squat load normalized to body weight (load (kg)/weight (kg)) used in the exercise regime for the Resistance Training group increased by 16.5% (± 5.2). Increases in squat load were significantly associated with reductions in postural sway scores (r=−0.45, p<0.01).
Adverse Events
Musculoskeletal complaints (e.g. sore neck, bursitis of the hip) developed in 10 women in the Resistance Training group, three in the Agility Training group, and two in the Stretching group. All musculoskeletal complaints either resolved or diminished within 3 weeks of onset and none required a physician’s attention. Four participants in the Agility Training group experienced shortness of breath that required them to desist from participating for 5 minutes before continuing. There were two trips (one participant) and six falls (four participants) in the Agility Training group. None of the falls in class resulted in injuries requiring medical attention.
Falls
Based on the falls diaries, which excluded falls that occurred in classes, there were 18 falls in the Resistance Training group (one subject fell seven times), 11 falls in the Agility Training group, and 10 falls in the Stretching group during the 25-week intervention period. There were 10 frequent fallers, defined as women having more than one fall during the intervention period; three in Resistance Training group, five in the Agility Training group and two in the Stretching group.
DISCUSSION
We found that both high-intensity resistance training and agility training were effective in reducing fall risk compared with a stretching program in older community-dwelling women with low bone mass. After 25 weeks of intervention, Resistance Training and Agility Training significantly reduced the fall risk score by 57% and 48%, respectively, compared with only a 20% reduction in the Stretching group. Based on normative data from the Randwick Falls and Fractures Study 20, these changes represent a reduction in the risk of falling over 12 months from over 80% to 50–55%.
Of the five components that contribute to the calculation of the fall risk score, we hypothesized that postural sway, quadriceps strength, and hand reaction time would be amenable to change by the intervention programs. We found that both Resistance Training and Agility Training significantly improved postural stability compared with the Stretching group, but that the groups did not differ significantly in the tests of strength and reaction time at the end of the trial. This indicates that for both groups the reduction in fall risk scores was primarily mediated via improved postural stability.
The finding that Agility Training improved postural stability is consistent with previous investigations in other populations of older people 4,28,29. However, the finding that Resistance Training improved postural stability contrasts with some previous studies 30,31. The inconsistencies in the findings here may relate to differences in the intensity of the resistance training programs used across studies. For example, the current study and the study by Nelson et al. 32 used high-intensity resistance training programs - 75% to 85% of 1RM, two sets of six to eight repetitions; and 85% of 1RM, three sets of eight repetitions respectively. In contrast, studies with lower intensity interventions such as 70% to 75% of 1RM, 13 repetition maximum 30, or home-based lower extremity resistance training program using therabands or body weight 31 have not been found to be effective in improving balance.
Although not reflected by the seated isometric knee extension test, the Resistance Training group significantly increased the squat load used in the exercise program. The lack of significant improvement in the strength outcome measure may reflect the specificity of training (standing squats) that differed from the conditions for testing (seated knee extension). The lack of generalization across strength measures has also been reported by Murphy and Wilson 33, who found that in athletes who trained with standing squats, significant strength gains were demonstrated in a 1 RM standing squat test but not in a seated knee extension test. Increases in squat load were significantly associated with reductions in sway scores on the compliant foam rubber mat, and this interesting association may indicate how resistance training is related to improved balance and reduced falls risk.
It has been postulated that regular exercise may maintain the reactive capacity of older people by delaying the deterioration of the dopamine systems, enhancing cerebral circulation integrity, and having trophic influence on the neurons that supply the muscle fibers 34. There were strong trends that indicated that the agility and resistance training groups had faster reaction times at the end of the trial for both a finger and foot-press response, but these differences did not reach statistical significance. Significant improvements may have been evident with a longer duration of the intervention period or with increased power with a slightly larger sample 4.
At the study mid-point (13 weeks), there were few differences among the groups. However, for both the Resistance and Agility groups further improvements occurred in the second period of the trial, so that significant differences were apparent for the fall risk and postural sway measures. This would indicate that trials of six-month duration or more are necessary to obtain maximal beneficial intervention effects. Improvement in general balance and mobility (CB&M scores) was apparent in the Agility Training group at 13 weeks, but the relative improvement over the other groups was not maintained at the study endpoint. This may be due to the lack of established protocols and appropriate safe environment for progressing an agility training program, compared with a resistance training program. Further, all three groups showed improvements in this measure at the end of the trial, which may reflect direct participation in the programs, indirect activity associated with attending the classes and increased activity outside the program as indicated by the changes in PASE scores.
Both the Resistance and Agility exercise programs were feasible for older adults with low bone mass. However, the Agility Training program carried a higher risk of falls compared with the Resistance Training. Our Agility Training program required considerable planning and many safety precautions. Furthermore, the progression of an agility training program, unlike a resistance training program, is not well defined in both the clinical and research setting. Although adverse effects also occurred in the Resistance Training group, we contend that short-term musculoskeletal complaints are less disabling than sustaining a hip fracture from a fall. Thus, we consider that a community-based agility program is more complex to deliver outside of the research setting than is a resistance training program. On the other hand, it was clear that the Agility Training participants found the program particularly enjoyable, and this may enhance long-term compliance.
We acknowledge that the study has certain limitations. First, the interventions were staff intensive and their availability in the health system may be limited by cost. Second, the primary study outcome was fall risk, as opposed to falls. Thus, future research using falls as the primary outcome measure is needed to confirm the role of resistance training and agility training in falls prevention in those with low bone mass. It would be also be useful to contrast the interventions against proven fall prevention interventions.
In conclusion, we found that both high-intensity resistance training and agility training significantly reduced fall risk in older women with low bone mass compared with a stretching program. Furthermore, this study demonstrated that this group have the capacity to participate in demanding exercise programs with acceptable risk. These exercise programs may have particular public health benefits as it has been shown that older women with low bone mass are at increased risk of falling as well as sustaining fall-related fractures.
Acknowledgments
The authors thank the Vancouver Foundation (BCMSF, Operating Grant) and the BC Women’s Hospital Osteoporosis Program, the Vancouver South Slope YMCA management and members who enthusiastically supported the study by allowing free access to participants for the training intervention, and the Osteoporosis Society of Canada, BC Branch, for support with recruitment of participants. The authors are indebted to Ms Connie Waterman, Director of the BC Women’s Hospital Osteofit Program for her help in designing and implementing the training interventions and Dr. Lynda Thayer for the medical assessments. We thank the instructors for their commitment to the participants’ health and safety. Drs. Khan, Eng and Janssen are Canadian Institutes of Health Research New Investigators. Dr. Eng received a salary support from Canadian Institutes of Health Research (MSH-63617). Drs. McKay, Eng and Janssen are Michael Smith Foundation for Health Research (MSFHR) Career Scholars. Ms. Liu-Ambrose is a MSFHR Doctoral Trainee, a Killam Pre-Doctoral Fellow, and a MSFHR Post-doctoral Trainee. The Peter Wall Institute for Advanced Studies at UBC funded the Exploratory Workshop related to this study. The Canada Foundation for Innovation funded essential infrastructure used in this study (New Opportunities Fund).
References
- 1.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 2.Grimely-Evans J. Fallers, non-fallers and Poisson. Age Ageing. 1990;19:268–269. doi: 10.1093/ageing/19.4.268. [DOI] [PubMed] [Google Scholar]
- 3.Carter ND, Kannus P, Khan KM. Exercise in the prevention of falls in older people: a systematic literature review examining the rationale and the evidence. Sports Med. 2001;31(6):427–438. doi: 10.2165/00007256-200131060-00003. [DOI] [PubMed] [Google Scholar]
- 4.Lord S, Ward J, Williams P, et al. The effect of a 12-month exercise trial on balance, strength, and falls in older women: A randomized trial. J Am Geriatr Soc. 1995;43:1198–1206. doi: 10.1111/j.1532-5415.1995.tb07394.x. [DOI] [PubMed] [Google Scholar]
- 5.Wolf S, Barnhart H, Kutner N, et al. Reducing frailty and falls in older persons: An investigation of Tai Chi and computerized balance training. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 6.Campbell J, Robertson M, Gardner M, et al. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–1069. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 8.Cummings S, Black D, Nevitt M, et al. Bone density at various sites for prediction of hip fractures. Lancet. 1993;341:72–75. doi: 10.1016/0140-6736(93)92555-8. [DOI] [PubMed] [Google Scholar]
- 9.Liu-Ambrose T, Eng J, Khan K, et al. Older women with osteoporosis have increased postural sway and weaker quadriceps strength than counterparts with normal bone mass: Overlooked determinants of fracture risk? J Gerontol. 2003:000–000. doi: 10.1093/gerona/58.9.m862. In Press. [DOI] [PubMed] [Google Scholar]
- 10.Carter ND, Khan KM, McKay HA, et al. Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. Can Med Assoc J. 2002;167(9):997–1004. [PMC free article] [PubMed] [Google Scholar]
- 11.WHO Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Geneva: World Health Organization, WHO Technical Report Series; 1994. [PubMed] [Google Scholar]
- 12.Chisholm D, Collins M, Kulak L, et al. Physical activity readiness. Br Col Med J. 1975;17:375–378. [Google Scholar]
- 13.Canadian Society for Exercise Physiology. Par-Q and You. Gloucester, Ontario, Canada: Canadian Society of Exercise Physiology; 1994. pp. 1–2. [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 15.Krieger N, Tenenhouse A, Joseph L, et al. The Canadian Multicentre Osteoporosis Study. Can J Aging. 1999;18:376–387. [Google Scholar]
- 16.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 17.Washburn RA, McAuley E, Katula J, et al. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52(7):643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 18.Lord S, Sherrington C, Menz H. Risk factors and strategies for prevention. Cambridge: Cambridge University Press; 2001. A physiological profile approach for falls prevention. Falls in older people; pp. 221–238. [Google Scholar]
- 19.Lord S, Clark R, Webster I. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. 1991;39:1194–1200. doi: 10.1111/j.1532-5415.1991.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 20.Lord S, Ward J, Williams P, et al. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42:1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 21.Lord S, Castell S. Physical activity program for older people: Effect on balance, strength, neuromuscular control, and reaction time. Arch Phys Med Rehabil. 1994;75:648–652. doi: 10.1016/0003-9993(94)90187-2. [DOI] [PubMed] [Google Scholar]
- 22.Howe J, Inness E, Verrier M, et al. Development of the Community Balance and Mobility Scale (CB&M) for the Traumatic Brain Injury (TBI). American Congress of Rehabilitation Medicine; 1999. [Google Scholar]
- 23.Wallmann H. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limit of stability. J Gerontol. 2001;56A(9):M580–583. doi: 10.1093/gerona/56.9.m580. [DOI] [PubMed] [Google Scholar]
- 24.Briggs R, Gossman M, Birch R, et al. Balance performance among noninstitutionalized elderly women. Physical Activity. 1989;69(9):748–756. doi: 10.1093/ptj/69.9.748. [DOI] [PubMed] [Google Scholar]
- 25.Braith RW, Graves JE, Leggett SH, et al. Effect of training on the relationship between maximal and submaximal strength. Med Sci Sports Exerc. 1993;25(1):132–138. doi: 10.1249/00005768-199301000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Province MA, Hadley EC, Hornbrook MC, et al. The effects of exercise on falls in elderly patients. A preplanned meta- analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA. 1995;273(17):1341–1347. [PubMed] [Google Scholar]
- 27.SPSS. SPSS Base 8.0, Applications Guide. Chicago: SPSS Inc; 1992. [Google Scholar]
- 28.Ledin T, Kronhed A, Moller C, et al. Effects of balance training in elderly evaluated by clinical tests and dynamic posturography. J Vestib Res. 1991;1:129–138. [PubMed] [Google Scholar]
- 29.Lord S, Caplan G, Ward J. Balance, reaction time, and muscle strength in exercising and nonexercising older women: A pilot study. Arch Phys Med Rehabil. 1993;74(8):837–839. doi: 10.1016/0003-9993(93)90010-8. [DOI] [PubMed] [Google Scholar]
- 30.Wolfson L, Whipple R, Derby C, et al. Balance and strength training in older adults: Intervention gains and Tai Chi maintenance. J Am Geriatr Soc. 1996;44:498–506. doi: 10.1111/j.1532-5415.1996.tb01433.x. [DOI] [PubMed] [Google Scholar]
- 31.Chandler J, Duncan P, Kochersberger G, et al. Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community-dwelling elders? Arch Phys Med Rehabil. 1998;79:24–30. doi: 10.1016/s0003-9993(98)90202-7. [DOI] [PubMed] [Google Scholar]
- 32.Nelson ME, Fiatarone MA, Morganti CM, et al. Effects of high-intensity strength training on multiple risk factors for osteoporotic fractures. A randomized controlled trial. JAMA. 1994;272(24):1909–1914. doi: 10.1001/jama.1994.03520240037038. [DOI] [PubMed] [Google Scholar]
- 33.Murphy A, Wilson G. The ability of tests of muscular function to reflect training-induced changes in performance. Journal of Sports Sciences. 1997;15(2):191–201. doi: 10.1080/026404197367461. [DOI] [PubMed] [Google Scholar]
- 34.Spirduso W. Physical fitness in realtion to motor aging. In: Mortim J, Pirozzolo F, Maletta G, editors. The aging motor system. New York: Praeger; 1982. [Google Scholar]