Abstract
Distal radius fractures have been a common affliction for millennia, but their treatment is a more recent development as a result of human erudition. While immobilization has served as the only available treatment for most of our history, many advances have been made in the management of distal radius fractures over the last century as the field of orthopedics has grown. Yet, the topic remains hotly contested in the literature, and research continues to focus upon it given the frequency of the injury. In this article, we chronicle the evolution of distal radius fracture treatment in hopes of providing context for the future that lies ahead.
Introduction
The distal radius fracture (DRF) is an injury that predates our species, with a significant milestone in our evolution being the transition to bipedal ambulation by Australopithecus. This elevated posture likely represents a significant risk factor that has played a role in DRFs being the most common fracture treated by physicians.1 This possibility is echoed by the paucity of the injury in our closest evolutionary relative – the chimpanzee.2 As our species gained sophistication, it began to develop treatments of maladies such as fractures in order to minimize morbidity. Though our exploration in the precursors of medicine likely predates the written word, the advances in the treatment of DRFs have a more abbreviated history. There are accounts of fracture splinting that stem back to ancient Egypt, but most of the contributions into the DRF management have been made in the past century.
Today, we have a better understanding of radiocarpal anatomy, wrist biomechanics and bone physiology than ever before, and we continuously strive to refine our surgical techniques to optimize outcomes. Understanding the advances that have been made in DRF treatment provides an appreciation for those who came before us, and a keen perspective of where we have been as we move forward. As one reflects over the history of DRF management, the contributions made to the field can be loosely divided up into three eras with seemingly different goals. In the first era, physicians struggled with the ability to diagnosis fractures in the distal radius. In the second, they had a grasp of the diagnosis but lacked good therapeutic options to address every injury. In the most recent period, surgeons aim to improve their surgical technique and better delineate treatment protocols to maximize functional outcomes and minimize morbidity.
Era of Naiveté (Pre 1895)
The first era in the management of DRF fractures is by far the longest, spanning back much further than our remaining records for us to interpret and understand. The oldest surviving descriptions regarding the management of fractures stem back at least 5,000 years to ancient Egyptian case reports within the Edwin Smith Papyrus.3 The translation of the hieroglyphics amongst these ancient scrolls describes manipulating a fractured arm until it is straight, then applying splints of wood and rolls of linen, which were subsequently hardened with grease and honey to maintain their position. This ancient work represents one of the first surgical texts—an early preliterate civilizatio'ns attempt to preserve medical knowledge for the sake of posterity. Unfortunately, too few cases in these works remain fully-preserved to allow substantial insight into the methods of diagnosis and treatment by the ancient Egyptians.4 Thus, most of the credit regarding the earliest roots of medicine falls to the ancient Greeks.
Often viewed as the father of Western medicine, Hippocrates is ascribed with most of the medical knowledge acquired during the Golden Age of Greece. However, most of the works credited to him are actually an anonymous collection of Greek medical manuscripts from the library of Alexandria.5 Nonetheless, the Hippocratic Corpus represents an aggregate of the medical knowledge of the ancient world. In it lies significant discussion of dislocations and subluxations of the radiocarpal joint along with the prescribed treatment – manual reduction and gentle bandaging.6 However, given the rarity of this injury and the high frequency with which the ancient Greeks described it, it is likely that they misdiagnosed DRFs as radiocarpal dislocations. Millennia of misdiagnosis would pass until the 18th century when Petit and Pouteau would first theorize that Hippocrates had failed to fully conceptualize the injury he was describing and treating.7 Their theories, unfortunately, largely failed to disseminate out of France, leaving them little recognition.
In 1814, Abraham Colles published his landmark treatise on DRF that led to his eponymous reward. In “On the fracture of the carpal extremity of the radius”, Colles calls to question those who describe all wrist injuries as dislocations, and offers an explanation to why this may have been so.8 He postulates that “the absence of crepitus, and of the other common symptoms of fracture, together with the swelling which instantly arises in this, as in other injuries of the wrist, render the difficulty of ascertaining the real nature of the case very considerable.” He also describes how to reduce the injury and notes the importance of immobilization with a wooden splint to prevent the wrist from falling into dorsal displacement. However, this paper would also receive little attention, and it was the work of Guillaume Dupuytren that brought these fractures to the interest of the surgical world at large.7
Throughout this era, treatment of DRFs changed very little. Casting and splinting was mostly unchanged from the times of the ancient Egyptians and Greeks. Glues, resins and waxes were used to harden bandages in order to immobilize the wrist and forearm. In the 1850s, plaster of Paris gained popularity in Europe as the solidifying agent in casting techniques.9 Results were mixed but overall deemed reasonable due to physicians’ inability to follow-up the anatomic alignment with anything other than physical exam. In 1895, Wilhelm Röntgen would make a discovery that would forever change the landscape of medicine.4 Due to his Nobel prizewinning work on x-rays, the conservative management of DRFs would be called into question for the first time.
Era of Invention (1895-1965)
The advent of roentgenography marked a significant milestone in the evaluation and management of fractures. The information about x-rays disseminated so quickly that within two months of Röntgen's discovery, the first case of using x-rays for clinical diagnosis was published in Lancet.10 This sparked a significant increase in the literature about fractures and their management. For the first time, physicians were able to discuss fractures on the basis of degree of displacement and articular involvement in the live patient, rather than the autopsy specimen. Several authors began publishing on the radiographic findings of DRFs soon afterwards in the late 19th and early 20th centuries.11-15 They called into question the results that had previously been thought adequate and started postulating how to address their concerns.
Throughout this era, management of DRFs remained predominantly nonoperative. Although advances in imaging did allow for better assessment of initial fracture reduction and follow-up, cast immobilization resulted in frequent malunions and residual deformity. It was well-established that DRF frequently resulted in shortening and loss of volar tilt. However, treatment options were limited. Physicians developed complex splints in a wide-variety of wrist positions to attempt to prevent collapse of the fracture fragments over time. Though surgeons began to discuss surgical options to address difficult fractures, it remained a risky endeavor that exposed the patient to infection. The pivotal works in antisepsis by Lister paved the way to make primary surgical fixation a safe and prudent option in the management of fractures.16, 17 Albin Lambotte was the first to attempt controlling the fragments in a DRF by surgical means, building on his experience in other bones of the body. In 1908, he described the use of a percutaneously placed wire through the radial styloid to maintain reduction.18 However, it took more than 40 years before a case series with results using K-wires was published in the literature.19
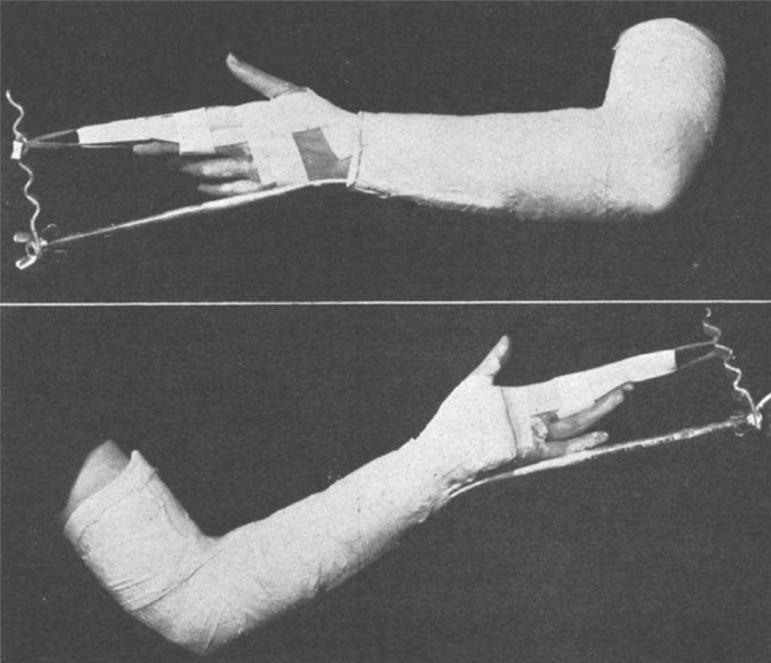
Comminuted DRFs remained a significant problem for the treating physician equipped with only cast immobilization. Reduction was impossible to maintain, and shortening of the radius would inevitably develop. The principles of ligamentoaxis were understood in terms of fracture reduction, but in the early 20th century, attempts were made to carry that over to definitive treatment. Lorenz Böhler introduced the use of pins with plaster to treat DRFs much like he had treated lower extremity fractures with traction.20 Donald Murray described the use of an adhesive traction device to maintain radial length during the consolidation phase of bony union (Fig. 5).21 This elaborate contraption distracted the fracture out to length via the radial digits and maintained that alignment while the fracture healed. Skeletal traction via pins and plaster eventually gave way to formal external fixators as we know them today, when in 1944 Anderson and O'Neil's introduced their initial design (Fig. 6).22 Pins were placed in the radius proximally and the index metacarpal distally, and were kept at a length with a simple bar. Thus, surgeons were able to predictably prevent what had previously been considered inevitable radial shortening.
Fig. 5.
Adhesive traction, advanced by surgeons such as Murray, was a precursor to external fixation for comminuted distal radius fractures that was based on the principle of ligamentotaxis. Reprinted with permission from the American Journal of Surgery. Murray DA. Treatment of Fractures of the Carpal End of the Radius by Traction. Am J Surg. 1939:44;135-138
Fig 6.
Anderson and O'Neil were the first to use external fixators on the distal radius in the 1940s, finally providing a surgical option for comminuted intraarticular fractures. Reprinted with permission from the Journal of the American College of Surgeons, formerly Surgery of Gynecology and Obstetrics. Anderson R, O'neil G. Comminuted fractures of the distal end of the radius. Surg Gynec Obstet. 1944;78:434-440
Internal fixation had its earliest proponents in the early 19th century with pioneers like J.K. Rodgers who introduced internal fixation of the skeleton as a treatment for non-unions and pseudoarthroses.23 The only fixation instrument available at the time was surgical wire, which was tightened down after passing it through drill holes in an early cerclage technique. With the dissemination of Lister's advances in antisepsis, surgical management was becoming a safer option, and internal fixation had its first vocal and effective advocates in the early 20th century with men like Sir Arbuthnot Lane and Albin Lambotte.4 Lane's interest in the field was a direct result of his experience with postmortem dissections, where he observed the frequency of malunions and the effect they had on the skeleton and articular surfaces.24 Lane and Lambotte began to treat fresh closed fractures with internal fixation, thus developing the early principles of osteosynthesis. 25-28
Even with some promising results in other long bones, the literature is devoid of any report of a primary open reduction and internal fixation of a DRF prior to 1960. One can speculate as to why that void exists – perhaps the early attempts at ORIF were so poor that they never made it into the literature, or possibly the functional outcomes in DRF at the time were deemed “good enough” that a new surgical option was not explored. Regardless of the cause, there was a significant lag in using plates and screws in DRF in comparison with fractures of other long bones. However, a significant milestone occurred in 1958 when over a dozen Swiss surgeons met to discuss their dissatisfaction with current results in fracture management. This group of visionaries would later serve as the nucleus of the organization we now know as Arbeitsgemeinschaft für Osteosynthesefragen, or AO.29 Soon afterwards, the first two case reports using internal fixation in the distal radius were published in the literature, likely a result of this growing interest in operative management of fractures.30, 31 Yet, ORIF of distal radius fractures remained a rarely used option in the orthopedic surgeon's armamentarium for decades.
Era of Refinement (1965-Present)
By the mid 1960s, the forefathers of modern orthopedics had developed the foundations of DRF management that we know today. Operative techniques were introduced in light of the frequent malunions that resulted from the conservative management of fractures, yet as this era began, almost all distal radius fractures continued to be treated nonoperatively.32 The operative indications and benefits were poorly understood by the average practitioner, thus rarely advocated. However, there were some who were dissatisfied with their end results, and many surgeons continued to experiment with new techniques and apply them to their most difficult cases. Thus, this most recent era has seen a refinement of the available techniques and a continuing search to better understand the appropriate indications for each intervention.
Each operative technique has had its proponents over the last several decades – surgeons who innovated the previously described procedures to improve their results, as well as the manufacturers who have improved implant design and materials. Percutaneous pinning was most notably revolutionized by Kapandji, who introduced the concept of intrafocal pinning of the fracture site in the 1970s as a means to buttress the distal segment.33-35 Difficulty with the pins and plaster techniques led to an increase in the use of external fixators in the 1980s.36-38 External fixation devices have been designed to provide surgeons with more options – multiple degrees of freedom to position the wrist in space, as well as the choice of whether to bridge the radiocarpal joint or not.39, 40 However, the use of internal fixation in DRF has probably seen the greatest change in interest and largest increase in operative options over the past 2 decades. With a better understanding of DRF fracture patterns and wrist biomechanics, a multitude of implant systems with a wide variety of designs have been developed. Internal fixation devices have transitioned from stainless steel to titanium alloys, which are lighter and more biocompatible.41, 42 Dorsally applied pi and Forte plates were popularized in the 1990s, but fell quickly out of favor due to the frequent tendon irritations.43-45 Over the last decade, volar locking plates have taken hold as the implant of choice, and operative fixation of DRF is at an all time high.46-50
Most recently, the Journal of the American Medical Association introduced the concept of “evidence-based medicine” into the lexicon of the medical literature, and with it, gave new impetus to research on treatment algorithms for the management of DRFs.51, 52 The notion is that clinical decision-making should reflect the best available evidence from clinical research, rather than heuristics and unsystematic experience.53 However, this concept has had difficulty gaining momentum in the surgical specialties, where clinical questions have a paucity of high-quality evidence, and randomized-controlled trials are few and far between. Often, the surgeon's clinical experience leads to changes in treatment patterns not yet proven superior in the literature. A prime example is the dramatic rise in the use of volar-locking plate for operative fixation over the last decade, with little in the way of comparative studies.46, 47 We must ultimately use outcomes to further elucidate the indications for operative management of DRFs, particularly as we practice medicine in this cost-conscious climate going forward.
Conclusions
Though the injury is older than even our species, most of the advances regarding DRF management have been made over the past century since the advent of x-rays. DRF remains a common ailment and there are more options regarding treatment today than at any previous point in history. Cast immobilization is often used for definitive treatment, but operative management continues to take hold of a larger share of DRFs each year. By reviewing the history of the evolution of DRF management, one gains appreciation for the contributions made thus far in a relatively small window of time. The future in DRF management sees an evolving discussion about the outcomes each treatment option affords and a better understanding of an evidence-based system of practice.
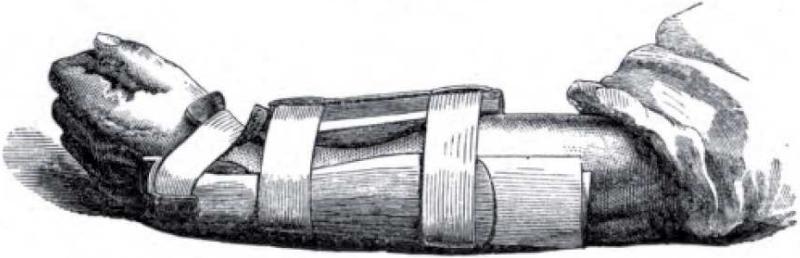
Fig. 1.
An example of functional splinting created to prevent the dorsal collapse of the distal fragment in a Colle's fracture by flexing the wrist and applying pressure to the metacarpal bases and carpal rows. (From Gordon, A. A treatise on the fractures of the lower end of the radius on fractures of the clavicle and on the reduction of the recent inward dislocations of the shoulder joint. London: Churchhill; 1875)
Fig. 2.
Images of how to properly (A) and improperly (B) don a cravat sling as a treatment of a distal radius fracture. Note how in the proper position (A), the wrist is held in slight flexion, slight supination and ulnar deviation to maintain radial length. (Scudder, CL. The treatment of fractures. Philadelphia: W.B.Saunders, 1902)
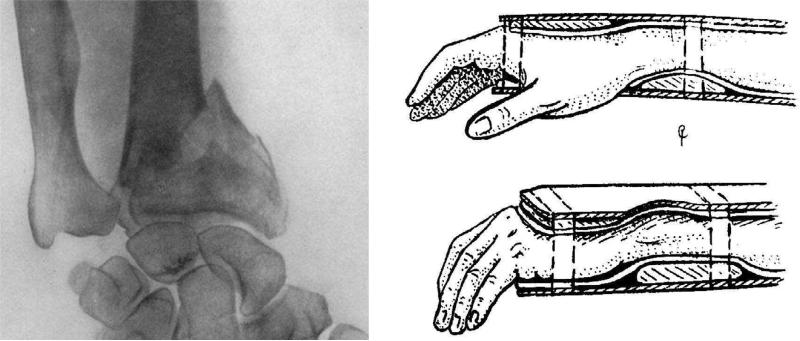
Fig. 3.
X-rays allowed physicians at the turn of the 20th century to better diagnose distal radius fractures, but treatment options were still limited. Even comminuted fractures (A) were treated with splinting (B). (Cotton, F. Fractures of the radius. Ann Surg. 1907; and Cotton, F. Dislocations and Joint Fractures. Philadelphia: W.B. Saunders, 1910)
Fig. 4.
Reduction and plaster immobilization of shortened fractures often required multiple hands to maintain reduction and place a well-fitted cast. Nevertheless, reduction was often lost leaving suboptimal results. Reprinted with permission from Wilhelm Maudrich. Böhler, L. Treatment of Fractures. Vienna, Wilhelm Maudrich, 1929
Acknowledgments
Supported in part by a grant from the National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR062066) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) to Dr. Kevin C. Chung.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–15. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Jurmain R. Trauma, degenerative disease, and other pathologies among the Gombe chimpanzees. Am J Phys Anthropol. 1989;80:229–37. doi: 10.1002/ajpa.1330800211. [DOI] [PubMed] [Google Scholar]
- 3.Breasted JH. The Edwin Smith Surgical Papyrus. Special ed. The Classics of Medicine Library; Birmingham, Ala.: 1984. [Google Scholar]
- 4.Peltier LF. Fractures : a history and iconography of their treatment. Norman Pub.; San Francisco: 1990. [Google Scholar]
- 5.Garrison FH, Wantz GE. An introduction to the history of medicine : with medical chronology, suggestions for study and bibliographic data. Fourth edition W.B. Saunders Co.; Philadelphia ; London: 1929. [Google Scholar]
- 6.Hippocrates, Adams F, Sydenham Society . The genuine works of Hippocrates. Printed for the Sydenham Society; London: 1849. [Google Scholar]
- 7.Peltier LF. Fractures of the distal end of the radius. An historical account. Clin Orthop Relat Res. 1983:18–22. [PubMed] [Google Scholar]
- 8.Colles A. On the fracture of the carpal extremity of the radius. Edinb Med Surg J. 1814;10:181. doi: 10.1097/01.BLO.000020589575491.a8. [DOI] [PubMed] [Google Scholar]
- 9.Rang M. The story of orthopaedics. W.B. Saunders; Philadelphia: 2000. [Google Scholar]
- 10.Jones R, Lodge O. The discovery of a bullet lost in the wrist by the means of Roentgen rays. Lancet. 1896;1:476–7. [Google Scholar]
- 11.Codman E. A study of the x-ray plates of one hundred and forty cases of fracture of the lower end of the radius. Boston Med Surg J. 1900;143:305–9. [Google Scholar]
- 12.Cotton F. The pathology of fracture of the lower extremity of the radius. Ann Surg. 1900;32:194–218. doi: 10.1097/00000658-190007000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pilcher LS. Fractures of the lower extremity or base of the radius. Ann Surg. 1917;65:1–27. doi: 10.1097/00000658-191701000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Destot E. La poignet et les accidents du travail: Étude radiographique et clinique. Vitot Freres; Paris: 1905. [Google Scholar]
- 15.Beck C. Colle's fracture and the Roentgen-rays. Med News. 1898:72. [Google Scholar]
- 16.Lister J. Illustrations of the antiseptic system of treatment in surgery. Lancet. 1867;2:668–9. doi: 10.1580/1080-6032(2000)011[0274:iotaso]2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 17.Lister J. On a new method of treating compound fracture, abscess, with observations on the conditions of suppuration. Lancet. 1867;1:326–9. [Google Scholar]
- 18.Rayhack JM. The history and evolution of percutaneous pinning of displaced distal radius fractures. Orthop Clin North Am. 1993;24:287–300. [PubMed] [Google Scholar]
- 19.Depalma A. Comminuted fractures of the distal end of the radius treat by ulnar pinning. JBJS. 1952;34-A:651. [PubMed] [Google Scholar]
- 20.Bohler L. Treatment of Fractures. Wilhelm Maudrich; Vienna: 1929. [Google Scholar]
- 21.Murray D. Treatment of fractures of the carpal end of the radius by traction. Am J Surg. 1938;44:135–8. [Google Scholar]
- 22.Anderson R, O'Neil G. Comminuted fractures of the distal end of the radius. Surgery, Gynecology and Obstetrics. 1944;78:434–40. [Google Scholar]
- 23.Rodgers J. Case of ununited fracture of the os brachii, successfully treated. New York Med Phys J. 1827;6:521. [Google Scholar]
- 24.Lane W. Some clinical observations on the principles involved in the surgery of fractures. Clin J. 1894;5:392. [Google Scholar]
- 25.Lambotte A. Notes sur l'osteosynthese dans les fractures du poignet. Annales de la Soc de med d'Anvers. 1904 [Google Scholar]
- 26.Lane W. The operative treatment of simple fractures. British Medical Journal. 1905;2:1325. doi: 10.1136/bmj.2.2342.1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lane W. The operative treatment of fractures. Annals of Surgery. 1909;50:1106. doi: 10.1097/00000658-190912000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vrebos J, Dupuis C. From circumferential wiring to miniaturized plates and screws: the history of osteosynthesis of the mandible. Eur J Plast Surg. 2005;28:170–8. [Google Scholar]
- 29.Allgower M, Spiegel PG. Internal fixation of fractures: evolution of concepts. Clin Orthop Relat Res. 1979:26–9. [PubMed] [Google Scholar]
- 30.Cauchoix J, Duparc J, Poral M. Les fractures-luxations marginales anterieures du radius. Revue de Chirurgie Orthopedique. 1960;46:233. [PubMed] [Google Scholar]
- 31.Ellis J. Smith's and Barton's fractures. A method of treatment. J Bone Joint Surg Br. 1965;47:724–7. [PubMed] [Google Scholar]
- 32.Older T, Stabler E, Cassebaum W. Colles fracture: Evaluation and selection of therapy. J Trauma. 1965;5:469–76. [PubMed] [Google Scholar]
- 33.Greatting MD, Bishop AT. Intrafocal (Kapandji) pinning of unstable fractures of the distal radius. Orthop Clin North Am. 1993;24:301–7. [PubMed] [Google Scholar]
- 34.Peyroux LM, Dunaud JL, Caron M, Ben Slamia I, Kharrat M. The Kapandji technique and its evolution in the treatment of fractures of the distal end of the radius. Report on a series of 159 cases. Ann Chir Main. 1987;6:109–22. doi: 10.1016/s0753-9053(87)80023-6. [DOI] [PubMed] [Google Scholar]
- 35.Kapandji A. [Internal fixation by double intrafocal plate. Functional treatment of non articular fractures of the lower end of the radius (author's transl)]. Ann Chir. 1976;30:903–8. [PubMed] [Google Scholar]
- 36.Carrozzella J, Stern PJ. Treatment of comminuted distal radius fractures with pins and plaster. Hand Clin. 1988;4:391–7. [PubMed] [Google Scholar]
- 37.Green DP. Pins and plaster treatment of comminuted fractures of the distal end of the radius. J Bone Joint Surg Am. 1975;57:304–10. [PubMed] [Google Scholar]
- 38.Seitz WH, Jr., Froimson AI, Leb R, Shapiro JD. Augmented external fixation of unstable distal radius fractures. J Hand Surg Am. 1991;16:1010–6. doi: 10.1016/s0363-5023(10)80060-7. [DOI] [PubMed] [Google Scholar]
- 39.Zanotti RM, Louis DS. Intra-articular fractures of the distal end of the radius treated with an adjustable fixator system. J Hand Surg Am. 1997;22:428–40. doi: 10.1016/S0363-5023(97)80009-3. [DOI] [PubMed] [Google Scholar]
- 40.Atroshi I, Brogren E, Larsson GU, Kloow J, Hofer M, Berggren AM. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77:445–53. doi: 10.1080/17453670610046389. [DOI] [PubMed] [Google Scholar]
- 41.Pennekamp PH, Wimmer MA, Eschbach L, Burian B, Koch P, Kraft CN. Microvasculatory reaction of skeletal muscle to Ti-15Mo in comparison to well-established titanium alloys. J Mater Sci Mater Med. 2007;18:2053–60. doi: 10.1007/s10856-007-3116-4. [DOI] [PubMed] [Google Scholar]
- 42.Dennison DG. Distal radius fractures and titanium volar plates: should we take the plates out? J Hand Surg Am. 2010;35:141–3. doi: 10.1016/j.jhsa.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 43.Ring D, Jupiter JB, Brennwald J, Buchler U, Hastings H., 2nd Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg Am. 1997;22:777–84. doi: 10.1016/S0363-5023(97)80069-X. [DOI] [PubMed] [Google Scholar]
- 44.Carter PR, Frederick HA, Laseter GF. Open reduction and internal fixation of unstable distal radius fractures with a low-profile plate: a multicenter study of 73 fractures. J Hand Surg Am. 1998;23:300–7. doi: 10.1016/S0363-5023(98)80131-7. [DOI] [PubMed] [Google Scholar]
- 45.Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg Am. 2003;85-A:1956–60. doi: 10.2106/00004623-200310000-00014. [DOI] [PubMed] [Google Scholar]
- 46.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–73. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koval KJ, Harrast JJ, Anglen JO, Weinstein JN. Fractures of the distal part of the radius. The evolution of practice over time. Where's the evidence? J Bone Joint Surg Am. 2008;90:1855–61. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 48.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29:96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 49.Sammer DM, Fuller DS, Kim HM, Chung KC. A comparative study of fragment-specific versus volar plate fixation of distal radius fractures. Plast Reconstr Surg. 2008;122:1441–50. doi: 10.1097/PRS.0b013e3181891677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chung KC, Squitieri L, Kim HM. Comparative outcomes study using the volar locking plating system for distal radius fractures in both young adults and adults older than 60 years. J Hand Surg Am. 2008;33:809–19. doi: 10.1016/j.jhsa.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Handoll HH, Madhok R. From evidence to best practice in the management of fractures of the distal radius in adults: working towards a research agenda. BMC Musculoskelet Disord. 2003;4:27. doi: 10.1186/1471-2474-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lichtman DM, Bindra RR, Boyer MI, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of distal radius fractures. J Bone Joint Surg Am. 2011;93:775–8. doi: 10.2106/JBJS.938ebo. [DOI] [PubMed] [Google Scholar]
- 53.Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268:2420–5. doi: 10.1001/jama.1992.03490170092032. [DOI] [PubMed] [Google Scholar]