Americans are continually bombarded with statistics on obesity. The media are filled with news reports celebrating the possible shrinking of our waistlines or lamenting their ongoing expansion. Some recent studies have suggested that U.S. obesity rates are continuing to increase. For example, state- and national-level data from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) of the Centers for Disease Control and Prevention (CDC)1 showed increases between 2007 and 2009 in the reported prevalence of obesity among adults — a 1.1% increase nationally, or an additional 2.4 million or so obese adults. Such data have led some investigators to suggest that by 2050, an enormous percentage of Americans — perhaps approaching 100% — will be overweight (defined in adults as a body mass index [BMI, the weight in kilograms divided by the square of the height in meters] above 25 but below 30) or obese (BMI ≥30). Other reports, however, suggest that the U.S. obesity prevalence, though very high, has stabilized. Results from the CDC's 2007–2008 National Health and Nutrition Examination Survey (NHANES) suggest that the prevalence of obesity among women (35.5%)2 and children 2 to 19 years of age (16.9%)3 has remained stable over the past 10 years and that the prevalence among men (32.2%)2 has not changed significantly since 2003. These conflicting reports have led to confusion regarding the prevalence of, and secular trends for, obesity in the United States.
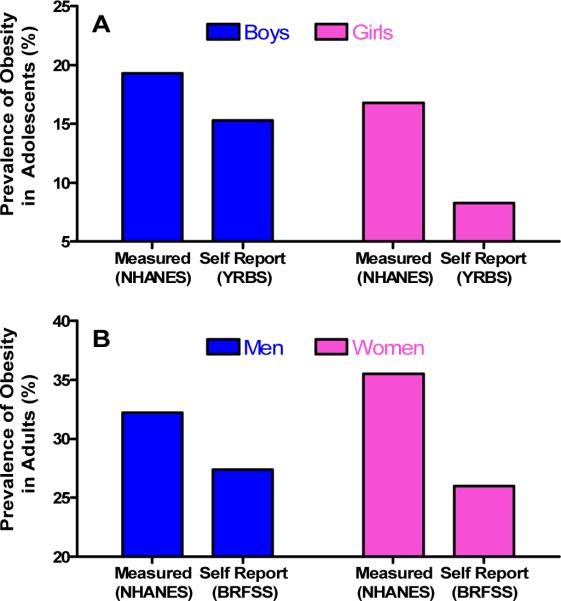
Why do the reported rates vary so markedly (see graphs), even though the data all come from government agencies? If obesity rates are stabilizing, why are they doing so? And what do these trends and prevalence rates mean for the current and future health of the U.S. population?
One key reason for discrepancies among the estimates is a simple difference in data-collection methods. The most frequently quoted data sources are the NHANES studies of adults and children, the BRFSS for adults, and the CDC's Youth Risk Behavior Survey (YRBS)4 for high school students. Although sampling strategies, response rates, age discrepancies, and the wording of survey questions may account for some variability, a major factor is that in calculating the BMI, the BRFSS and YRBS rely on respondents' self-reported heights and weights, whereas the NHANES collects measured (i.e., actual) heights and weights each year, albeit from a considerably smaller sample of the population. Since people often claim to be taller than they are and to weigh less than they actually do,5 we should not be surprised that obesity prevalence figures based on self-reported heights and weights are considerably lower than those based on measured data. Systematic differences between men and women, and potentially among different racial or ethnic groups or different age groups, in misreporting of height and weight in the BRFSS and YRBS could also limit our ability to interpret prevalence rates and trends accurately. In general, then, the estimates from the NHANES seem most likely to reflect the actual prevalence of obesity among adults and children in the United States.
One intriguing question that is raised by the data from self-report surveys — which, despite their inherent limitations, can theoretically allow for reasonably precise (if not entirely accurate) region-specific estimates of obesity prevalence — is why obesity rates that are based on self-reported data continue to increase at the same time that the prevalence of obesity as determined by the actual measurements of NHANES have stabilized. Though this matter may be best addressed by sociologists or psychologists, one possibility is that fewer people are reporting lower-than-accurate weights thanks to increased awareness about obesity on the part of health care professionals and the public at large.
A more important question arises when we consider the NHANES data showing that the overall prevalence of obesity among both adults and children appears to have stabilized over the past 5 to 10 years. Why would this be so? A hopeful interpretation is that increasing recognition by health care professionals, researchers, schools, community organizations, industry, and governments of the health effects of obesity has led to changes that reduce the environmental contributors to inappropriate weight gain; some data from communities that track children's BMIs suggest that there may well have been some progress on that front. Alternatively, we may have reached the point where most people who have a strong genetic susceptibility to weight gain are already obese, while a resistant segment remains lean despite our “toxic” environment. Unfortunately, even if that's true, among the susceptible are an ever-increasing number of adults with extreme obesity (BMI ≥40). The distribution of BMI in the United States among adults and children has become increasingly skewed to the right. Indeed, the stabilization of obesity rates among children and adolescents that is revealed in the NHANES data does not appear to extend to the very heaviest boys (those with a BMI at or above the 97th percentile for their age), whose numbers continue to increase.3
It is important to recognize that even if secular trends offer some encouragement, the prevalence of obesity remains unacceptably high, particularly among some racial and ethnic minority populations. The effects of the current obesity epidemic on the physical, psychological, and economic health of our country should not be understated, as the incidence of obesity-related diseases continues to increase among both adults and children.
Perhaps most concerning are the effects of childhood obesity on health in both childhood and adulthood. Growing numbers of children now have diseases once considered to be “adult” conditions, such as type 2 diabetes, nonalcoholic fatty liver disease, and hypertension, and there is evidence that an earlier age of onset of obesity-related diseases may be associated with more severe health consequences in adulthood. In addition, as the incidence of obesity-associated gestational diabetes increases, more fetuses are exposed to a potentially obesogenic intrauterine milieu that may have a significant effect on later risk for obesity, diabetes, and other metabolic disorders, possibly mediated by altered placental uptake of nutrients, which may lead to epigenetic changes and alterations in fetal neural programming. This dynamic, in turn, sets the stage for a vicious cycle of obesity and metabolic disorders that could adversely affect the health of the population for generations. Additional evidence suggests that high rates of weight gain during infancy may increase a person's later risk of obesity. Thus, the trend toward stabilization of obesity rates could be temporary.
There is a need for research to determine how to intervene safely and effectively as early as possible to prevent obesity. We need to develop programs that help women of childbearing age achieve a healthy weight before conception and gain an appropriate amount of weight during pregnancy, as well as interventions targeted to infants and young children that lead to optimal nutritional, activity, and sleep patterns along with appropriate growth and development.
In addition, for the millions of people who are already obese, there is a critical need for safer and more effective treatments to promote and sustain weight loss. Understanding the relationship between obesity and the development of associated medical conditions may also help to improve health independent of weight loss, and a better understanding of the many causal factors that lead to obesity may allow the development of more targeted and effective therapies.
Regardless of current trends in obesity prevalence, we are in trouble. Effective strategies for preventing and treating obesity require a commitment to addressing its causes and consequences at multiple levels — from basic research through community and policy interventions. As increasing recognition of the public health impact of obesity leads to implementation of programs and policies, it is also essential that outcomes be evaluated so that we know what works and what doesn't and can direct our energies and resources toward strategies that are most likely to be successful.
Different Estimates of the Prevalence of Obesity among U.S. Children (Panel A) and Adults (Panel B).
NHANES (2007–2008) data are based on the body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) calculated from measured height and weight among persons 12 to19 years old; the other data are based on the BMI calculated from self-reported height and weight among children in 9th to 12th grade (YRBS 2009) and among adults (BRFSS 2009). For adults (defined as 18 years of age or older in BRFSS and 20 years of age or older in NHANES), obesity is defined as a BMI of at least 30. For children, obesity is defined as a BMI greater than or equal to the age- and sex-specific 95th-percentile standard on the CDC 2000 BMI-for-age growth charts. The CDC 2000 growth charts for children older than 6 years are based on measured heights and weights obtained between 1963 and 1994.
Footnotes
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the National Institutes of Health, the U.S. Public Health Service, or the Department of Health and Human Services.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Vital Signs: State-Specific Obesity Prevalence Among Adults --- United States, 2009 Early Release. MMWR Morb Mortal Wkly Rep. 2010;59(Early Release):1–5. [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 4.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance - United States, 2009. MMWR Surveill Summ. 2010;59(5):1–142. [PubMed] [Google Scholar]
- 5.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8(4):307–26. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]