This study grows out of the National Institute of Mental Health-funded Sibling Resilience Research Project, an examination of risk and resilience among the siblings of children with severe emotional disturbances (SED; see, e.g., Kilmer, Cook, & Palamaro Munsell, 2010; Kilmer, Cook, Palamaro Munsell, & Salvador Kane, 2010; Kilmer, Cook, Taylor, Kane, & Clark, 2008). The larger project’s specific aims focus largely on the siblings in these families. Extending beyond the siblings, the present study focuses on caregiver physical and psychological well-being, and the degree to which social connections may serve to buffer the effects of caregiver strain on well-being. The study also investigates the relationships among caregiver well-being, family functioning, and child adjustment.
In most families, caregivers attend to basic day-to-day needs of family members and work to ensure that all are safe and well. Thus, caregiver well-being is an essential factor in child adjustment as well as family cohesion and harmony. Indeed, caregiver functioning and well-being can profoundly affect the well-being of family members, especially children in their care (Meadows, Mclanahan, & Brooks-Gunn, 2007; Pilowsky, Wickramaratne, Yoko, & Wiseman, 2006).
Even under ideal circumstances caregiving can bring with it challenges, strain, and stress. For those who parent children with special needs or mental health issues, the strains and stressors may be greater and more complex (Armstrong, Birnie-Lefcovitch, & Ungar, 2005; Baker & McCal, 1995). Caregivers of children with SED experience many of the same concerns as other parents as well as additional challenges. For instance, prior research has indicated that families of children with SED experience considerable adversity (including stressors reflecting turmoil in the family), and, in turn, primary caregivers report substantial levels of strain (Center for Mental Health Services, 2000; Kilmer, Cook, & Palamaro Munsell, 2010). The difficulties faced by these families depend, at least in part, on the child’s problems. Children with SED have been diagnosed with at least one psychiatric disorder, and their difficulties require involvement in more than one service system (e.g., Prange, Greenbaum, Silver, & Freidman, 1992). Because the behaviors associated with SED can be severe, the symptoms experienced by children with SED can be taxing, unpredictable, and disturbing for the entire household. (Yatchmenoff, Koren, Friesen, Gorden, & Kinney, 1998).
Many families who have a child with SED have other children who do not have mental health problems. For caregivers who have children with SED, meeting all family members’ needs may be particularly challenging (Kilmer et al., 2008). In this context, caregivers who are better able to manage the strain and stress associated with caregiving may be more likely to assure that the needs of their families are met (Baker & McCal, 1995). Understanding the nature of the relationship between factors associated with caregivers’ coping may illuminate the broader relationship between caregiver wellness and child and family adjustment. In the sections that follow, we consider relevant theories for framing aspects of this relationship and briefly review selected research regarding (a) caregiver strain, (b) the association between social connections and well-being, (c) links between social support and care giving, and (d) the associations between caregiver well-being and family functioning.
Theoretical Foundations: The Bioecological Model
The bioecological model (e.g., Bronfenbrenner, 1986; Bronfenbrenner & Morris, 2006) is particularly well suited for understanding the multiple influences on child development and adaptation. According to this model, an individual’s various contexts, such as school, home, work, and recreational environments, along with the people associated with these environments, interact with each other and the individual to influence development and well-being (Bronfenbrenner & Morris, 2006). For children, the environment they live in and the relationships they have with their parents are central to their healthy development. Children are dependent on their caregivers for stability and support. Moreover, there is evidence that parental mood, parental coping skills, and overall caregiver wellness are strongly associated with childhood adjustment (Masten, Best, & Garmezy, 1990). Therefore, family is perhaps the most influential environment for a developing individual (Bronfenbrenner, 1986). One of the most crucial interactions within that system is the proximal (i.e., directly influential) relationship between child and parent (McDonald, Gregoire, Poertner, & Early, 1997).
Well-Being
Two major types of well-being have been identified: subjective well-being and psychological well-being (Linley, Maltby, Wood, Osbourne, & Hurling, 2009). Subjective well-being refers to an individual’s assessment of his or her own life satisfaction, whereas psychological well-being reflects aspects of personal growth such as those gained from successfully grappling with existential life questions (Keyes, Shmotkin, & Ryff, 2002). Well-being is associated with an individual’s capacity to effectively cope with life’s challenges. For this study, well-being refers to the combination of caregiver subjective well-being (i.e., satisfaction with life) and the absence of mental and physical symptoms generally attributed to anxiety and depression.
Caregiver Strain
Although there are benefits and rewards associated with caregiving (Taylor-Richardson, Heflinger, & Brown, 2006), there also can be considerable burden. Caregiver strain is multifaceted: Its experience includes, but is not limited to, financial strain, family conflict, and loss of freedom, as well as effects on health (Taylor-Richardson et al., 2006). Some evidence suggests that caregiver strain differs from general life stress (Brannan & Heflinger, 2002). Although psychological distress might be associated with myriad general life stressors, strain is associated specifically with the symptoms and problem behaviors of those for whom one cares (Baker & McCal, 1995).
Although many factors can influence the effects of caregiver strain, child behavior is the strongest predictive factor associated with caregiver strain (e.g., Brannan & Heflinger, 2002). Strain experienced by the caregiver can also profoundly impact child well-being and treatment. For example, higher levels of caregiver strain have been associated with higher levels of service utilization for children with SED, above and beyond what might be accounted for by child symptoms (Brannan, Helfinger, & Foster, 2003).
Social Connections and Well-Being
For this study’s purpose, the broad term social connections is used to encompass such factors as social support, religious connections, and sense of community. Generally defined as a feeling of kinship and a sense of belonging with others (Lee, Draper, & Lee, 2001), social connection refers to a feeling of social acceptance or group membership, as well as the feelings that individuals have for those in their social groups.
Individuals who feel connected with others are better able to cope, are less prone to anxiety and depression, and have better overall physical health (Lee & Robbins, 1998; Seeman, 1996). Moreover, social connections have been associated with lower disease incidence and severity and faster disease recovery (Seeman, 1996). Conversely, a low sense of social connection is associated with interpersonal behaviors that lead to psychological distress and low self-esteem (Lee et al., 2001). The current study focuses on three forms of social connection: religious participation, sense of community, and social support.
A full consideration of the multifaceted aspects of spirituality, coping, and quality of life, and the extensive literatures regarding each, are beyond the scope of this review. Of particular salience to this study is the potential link between religiosity and social support for families. Although religious participation and religiosity or spirituality are not the same, they appear to be connected (Somalai & Heckman, 2000), and they have implications for families’ experiences of available support. That is, formal religious institutions, such as churches and mosques, offer the potential for a readily available support system.
Conversely, for caregivers of children with SED, religious communities alone may not offer the social inclusion or support they seek. In a qualitative study focusing on the religiosity of caregivers of children with disabilities, Speraw (2006) found that caregivers reported mixed support from faith-based communities. In large part, the feeling of cohesion that caregivers have with their faith community was based on the community’s acceptance or rejection of their child with disabilities. Although these parents perceived a degree of support from their religious communities, they also reported feelings of isolation and rejection when their children were not accepted, supported, and treated as members of the community (Speraw, 2006). These findings suggest that under some circumstances religious connections may serve to compound caregiver strain rather than alleviate it, and that caregivers of children with SED may require social connections beyond those offered by religious institutions.
Sense of community is defined as a sense of belonging within a community in which there is an identified and trusted authority structure and a spirit of shared togetherness and mutual benefit for community members (McMillan, 1996). Findings linking sense of community and well-being are mixed. Obst and White (2005) found that the more individuals feel a sense of belonging in their community, the greater they benefit from these associations. However, Bramston, Pretty, & Chipuer (2002) found that individual factors, such as loneliness, had much stronger associations with individual well-being, and others have reported no association between neighborhood interaction and individual well-being (Farrell, Aubry, & Coulombe, 2004).
Social support is a complex, context-specific construct, and individual needs for support differ based on situation, personality, culture, and expectations (Williams, Barclay, & Schmeid, 2004). Findings are not consistent and not all elements of social support are linked with positive outcomes. However, social support has consistently been associated with mental and physical health and well-being (Armstrong et al., 2005; Lee et al., 2001; Seeman, 1996). Furthermore, the quality of social connections may be of greater importance than simply having someone to confide in during in times of crisis.
Given that social interactions are complex relationships that can have both positive and negative qualities, it is important to note that negative social connections can be associated with poorer adjustment and less adaptive coping (Holahan, Moos, Holahan, & Brennan, 1997). Therefore, the quality of social connections and the responses of those to whom one turns may be of greater importance than simply having someone to confide in during times of crisis. In accordance with this notion, Song and Singer (2006) found that, for caregivers of family members with psychiatric disorders, satisfaction with social support was shown to have buffering effects on stress and depressive symptoms, although social support was not directly associated with caregiver stress relief. In a study of the effects of social support on psychological outcomes and self-esteem, findings indicate that social support may act as a mediator on indicators of well-being (Williams & Galliher, 2006). Others (Quittner, Glueckauf, & Jackson ,1990) have found that buffering models failed to explain the relationship between social support and psychological symptoms for those experiencing stress, but social support mediated the relationship between social support and symptoms of outcomes of anxiety and depression.
Although social support may not have a direct effect on coping, social support appears to be associated with the effects of caregiver strain, and therefore, on coping with strain (Ghate & Hazel, 2002). Regardless of whether social support acts as a mediator or a moderator of the effects of stress on strain, there seem to be some benefits, especially for caregivers. Social support has been found to alleviate caregiver stress, which may contribute to more adaptive coping strategies for dealing with child emotional and behavioral problems (Brannan & Heflinger, 2002)
Social Connections and Caregiving
Meaningful relationships, such as support from friends and family, have been associated with lower reported caregiver stress (Yatchmenoff et al., 1998). Moreover, social connections can also be a key factor in influencing parenting behaviors. For instance, new mothers who reported more social support had more positive interactions with their children and were less anxious in their parenting (Green, Furrer, & McAllistar, 2007). Parents were influenced to change their parenting styles by interactions and feedback in their social environments. However, the burden, and, at times, isolation associated with caring for a child with SED may contribute to difficulty for caregivers in accessing or developing social connections. The very nature of parenting a child with unique and special needs may lead to a disruption of informal supports such as friends and family, as these means of support may not be able to offer the expertise or understanding required (White & Hastings, 2004).
Caregiver Well-Being and Family Functioning
Caregiver well-being can affect children and families deeply, and levels of reported parenting stress have been found to be related to parenting style (Aunos, Goupil, & Feldman, 2008). Research suggests that mothers who report more stress are more likely to be less positive and more hostile toward their children and to use inconsistent or conflicting styles of parenting (Aunos et al., 2008; Luthar, 1999). These inconsistent and hostile parenting styles are associated with a higher frequency of child problem behaviors (Aunos et al., 2008). For parents of children with SED, child behavior and parenting are likely to influence one another (Armstrong et al., 2005; Baker & McCal, 1995). However, some evidence suggests that a change in parenting can lead to changes in child behavior. Green et al. (2007) found that when parents of young children modified their parenting and became less anxious, they were better able to engage their children. In turn, their children responded by exhibiting less disruptive behavior.
Moreover, the effects of parental well-being on child adjustment can be far-reaching. Longitudinal explorations of child well-being reveal that parental depression relates to family discord as well as child anxiety and depression, symptoms of which can continue well into adulthood (Pilowsky et al., 2006). That said, children of parents who report higher levels of family cohesion and well-being are less likely to report signs of anxiety and depression and are less likely to have substance abuse disorders (Pilowsky et al., 2006).
The Present Study
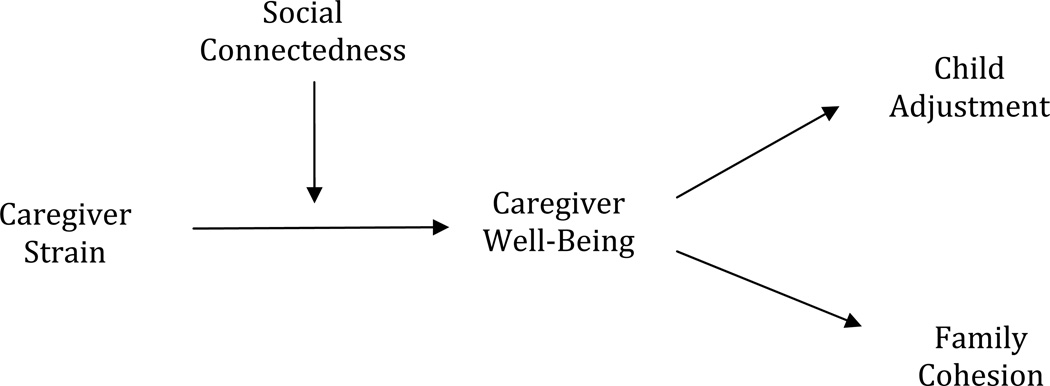
Informed by findings suggesting that parental well-being can have a profound effect on both child behaviors and family relationships, this study seeks to investigate the relationships among caregiver strain, support, and family well-being and to illuminate caregiver factors that contribute to child adjustment. Specifically, as represented in Figure 1, the present study explores the effects of caregiver social connections on the relationship between caregiver strain and well-being. The effects of caregiver well-being on child adjustment and family cohesion are also considered.
Figure 1.
Model of the hypothesized relationships among caregiver strain, social connectedness, and well-being, and child and family adjustment.
Methods
Participant Recruitment and Procedures
Participants were caregivers of families with (a) one child (i.e., diagnosed child) between the ages of 5 and 18 years who meets criteria for SED, and (b) at least one undiagnosed child (i.e., sibling) between the ages of 5 and 10. Multiple recruitment methods were employed. Study personnel spoke to organizations serving children with SED and their families. In addition, electronic versions of flyers were circulated via a national listserv to case management and clinical agencies, as well as parent support groups, by the Federation of Families for Children’s Mental Health, a national parent-run organization that supports families of children diagnosed with mental health disorders.
The participants in this study were self-selected. Those interested in participating in or learning more about the study were directed to contact the project office. Potential participants were screened for eligibility. Consent forms and measures (including standardized indicators of child adjustment, a measure of life stress, and a detailed caregiver questionnaire assessing family relationships, caregiver strain, and other contextual factors) were sent and returned completed via mail. Phone interviews were also conducted, focusing on child development, the caregiver-child relationship, family resources, caregiver connections, caregiver mental health functioning, and the like. Participants received gift cards for their participation.
Participants
One hundred and seventeen caregivers consented to participate in this study. Of those, 76 completed both the survey (T1) measures and the (T1) phone interview. Although scant data were available for those who did not complete the T1 measures and interview, no differences were found between those who participated and those who did not on geographical location of participant or child diagnoses. Only those individuals who completed both the measures and interview were included in the study. Although there was a follow-up 6–8 months later, only T1 data were used here.
Caregiver respondents were predominantly female. Caregivers ranged in age from 24 – 63 years (M = 38.12; SD = 7.48). The number of people in the household ranged from 2 – 16 (M = 4.95; SD = 1.81) with an average number of children per household of 3.00 (SD = 1.07). Yearly family income for participating families varied from less than $5,000 a year to greater than $50,000 (the highest category on the scale used). Twenty-six states were represented in the sample, with the largest number of participant families from North Carolina and Iowa. Beyond this more broad-based geographic representation, the present sample was more diverse socioeconomically than the predominantly poor pilot sample described by Kilmer et al. (2008).
On average, siblings were 7.61 years old (SD = 1.63), and 40% of the sibling sample was female. Siblings were predominantly Caucasian (65%) and African American (16%). The 76 diagnosed children ranged in age from 4 – 17 years with a mean age of 10.99 (SD = 3.19). The most frequent primary diagnoses (available for 86% of children) were attention deficit hyperactivity disorder (49%) and bipolar disorder (26%). Sixty-nine percent of children for whom diagnoses data were available had a secondary diagnosis.
Measures
Caregivers completed multiple measures for the diagnosed child and sibling, as well as scales assessing family and caregiver-specific variables. Selected caregiver report measures from the larger protocol were used for this study. Demographics included family size, income, number of children in household, age, children’s gender and ethnicity and child diagnoses. The Life Events Checklist (LEC), which assesses the stressful life events and circumstances experienced by the family, provided further family context. Items reflect five factors including Family Turmoil, Poverty, Family Separation/Social Services, Illness/Death, and Unsafe/Violent Neighborhood (Kilmer, Cowen, Wyman, Work, & Magnus, 1998).
Three measures were used to assess caregiver social connections. A 19-item measure adapted from the Medical Outcomes Study Social Support Survey (Sherbourne & Stewart, 1991) was used to assess social support. Caregivers used a 5-point scale from 1 (None of the time) to 5 (All of the time) to rate their perceptions of available support across four dimensions including tangible, affectionate, emotional/informational, and positive social interaction. A total score was used here (α = 91). Sense of community was assessed using the 12-item Sense of Community Index (Chavis, Hogge, McMillan, & Wandersman, 1986). On this true/false scale, caregivers responded to items reflecting four factors, including Membership within the Community, Feelings of Influence Upon the Community, Integration and Fulfillment of Needs, and Shared Emotional Connection with Neighbors. Religious Participation and Belonging was developed for the larger project. This 8-item measure utilizes a 4-point scale from 1 (A great deal) to 4 (Not at all) to assess the degree to which the caregiver reported participation in spiritual activities, as well as social connections with his or her faith-based community.
Caregiver strain and well-being were assessed using the following measures. Caregiver Strain (CST) is a 13-item yes-no index, which reflects common stressors related to caregiving and taps into multiple dimensions of burden such as physical health and emotional symptoms (Kilmer et al., 2008; Luescher, Dede, Gitten, Fennell, & Maria, 1999). Caregiver symptoms were assessed using The Brief Symptom Inventory (BSI; Derogatis, 2001). This 18-item measure uses a 5-point scale from 0 (Not at all) to 4 (Extremely) to assess symptoms across three factors: Depression, Anxiety, and Somatization. Caregiver Subjective Well-Being (Diener, Emmons, Larsen, & Griffin, 1985) is 5-item measure which assesses global life satisfaction utilizing a 7-point scale from 1 (Strongly disagree) to 7 (Strongly agree).
Youth and family functioning was assessed using the following measures. The true / false 27-item Relationship dimension of the Family Environment Scale (Moos & Moos, 1994) assesses cohesion, expressiveness, and conflict within the family’s relationships. The Behavioral and Emotional Rating Scale- 2 (BERS-2; Epstein, 2004) uses 52 items to assess behavioral and emotional strengths across five subscales (Interpersonal Strength, Family Involvement, Intrapersonal Strength, School Functioning, and Affective Strength) on a 4-point scale from 0 (Statement is not at all like my child) to 3 (Statement is very much like my child). Scores may also be converted into a standardized overall Strength Quotient, which was used in this study. The 39-item Parent-Child Rating Scale (P-CRS; Cowen et al., 1996; Hoyt-Meyers et al., 1995) assesses children’s competencies and problem behaviors using a 5-point scale from1 (Strongly disagree) to 5 (Strongly agree). The final measure of child adjustment utilized in this study was the caregiver-completed Oppositional subscale of the Conner’s Parent Rating Scale-Revised: Short Form (CPRS-R:S; Conners, 2001). On this subscale, caregivers used a 4-point scale from 0 (Not at all true) to 3 (Very much true) to rate items reflecting child oppositionality, which may be particularly associated with the child’s contextual characteristics, including qualities of the caregiver-child relationship and family milieu.
Plan of Analysis
The current sample size precluded the testing of the entire model using methods such as structural equation modeling. Therefore, elements of the model were tested for significance. Specifically, multiple hierarchical regressions were used to ascertain relationships among indicators of social connections, caregiver strain, and caregiver well-being. Additionally, relationships among caregiver well-being and child and family functioning were explored.
Results
Table 1 includes descriptive statistics for key variables of interest. Caregivers reported moderate to high levels of social connections (i.e., social support, sense of community, and religious participation). On average, they reported symptom levels below the clinical range and high levels of subjective well-being. However, a notable proportion experienced some difficulty. For example, 22% of caregivers had BSI Depression scores within the clinical range. Family relationships were reported to be fairly cohesive and expressive with a moderate amount of family conflict. Caregivers endorsed high levels of strain associated with caring for a child with SED. Overall, caregivers reported moderate levels of child strengths and oppositional behaviors and generally positive socio-emotional adjustment in the nondiagnosed siblings.
Table 1.
Descriptive Statistics for Key Variables of Interest
| M (SD) | Scale range | |
|---|---|---|
| Social Support | 68.27 (15.87) | 19–95 |
| Sense of Community Index | 8.80 (2.57) | 0–12 |
| Religious Participation and Connectedness a | 18.42 (7.42) | 7–28 |
| Brief Symptom Inventory b | 17.04 (10.39) | 0–72 |
| Caregiver Subjective Well-Being | 20.21 (6.52) | 5–35 |
| Caregiver Strain | 10.28 (2.60) | 1–13 |
| Family Environment Scale – Relationship Dimension |
15.98 (5.24) | 0–27 |
| Behavioral and Emotional Rating Scale Strength Quotient c |
105.17 (16.77) | 55–155 |
| Parent Child Rating Scale c | 152.32 (21.14) | 94–188 |
| Conners Parent Rating Scale –Oppositional Subscale d |
51.91 (10.66) | 39–89 |
Note. Sample size = 65–71
Lower scores indicate higher levels of participation and connectedness.
Higher scores indicate more symptomatology.
Higher scores indicate higher levels of child strengths / more positive child adjustment.
Higher scores indicate more oppositional behavior.
Bivariate correlations were run to assess the degree to which the indicators of social connections and caregiver strain related to caregiver well-being (see Table 2). Of the social connection measures (i.e., Social Support, Sense of Community Index, and Religious Participation and Belonging) only Social Support was significantly correlated with Caregiver Subjective Well-Being and the BSI. Caregiver Strain was correlated with Caregiver Subjective Well-Being and the BSI.
Table 2.
Correlations Among Social Connectedness Variables and Indicators of Caregiver Well-Being
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Social Support | - | .20 | −.24* | −.30* | .42** | −.45** |
| 2. Sense of Community Index | - | .03 | .13 | .20 | −.23 | |
| 3. Religious Participation | - | .19 | −.18 | .15 | ||
| 4. Caregiver Strain | - | −.32** | .30* | |||
| 5. Caregiver Subjective Well-Being | - | −.54** | ||||
| 6. Brief Symptom Inventory | - |
Note. N=76.
p < .05.
p < .01.
Hierarchical multiple regressions were used to ascertain relationships among the indicators of social connections, caregiver strain, and caregiver well-being. Additionally, relationships among caregiver well-being factors and child and family functioning were explored. As a next step, to allow for parsimonious analyses utilizing a coherent variable reflecting the best model of social connections for this sample, a principal components analysis was run with the three social connections variables. This analysis revealed a two component model (specific results not presented here; see Palamaro Munsell, 2010). Component 1 was used as the social connections variable in subsequent analyses as it best reflected the contribution of each of the three core variables; in other words, unlike Component 2, each social connections variable (i.e., Social Support, Sense of Community, and Religious Participation) contributed meaningfully to Component 1.
Then, to explore the degree to which social connections influence the effect of caregiver strain on caregiver well-being, two separate two-step hierarchical regressions were run with the well-being variables, Caregiver Subjective Well-Being and the BSI, as the dependent variables. To prepare for the regressions and facilitate interpretation of results, each independent variable was centered. Caregiver Strain and Social Connections were entered in Step 1 of each regression to illustrate the degree to which Caregiver Strain and Social Connections together contribute to the variance in caregiver well-being. In Step 2, the interaction term reflecting the joint effects of Caregiver Strain and Social Connections was added to assess the degree to which the joint effect of Caregiver Strain and Social Connections uniquely contributes to caregiver well-being over and above the effects of the individual variables.
In the model predicting Caregiver Subjective Well-Being (see Table 3), Step 1 of the model was significant, with Caregiver Strain and Social Connections accounting for 25 % of the variance in Caregiver Subjective Well-Being; Social Connections and Caregiver Strain each were significantly associated with Caregiver Subjective Well-being. However, the interaction reflecting the joint effect of Caregiver Strain and Social Connections did not contribute significantly to the model; there was no significant interaction effect.
Table 3.
Summary of Hierarchical Multiple Regression Testing the Joint Effects of Social Connectedness and Caregiver Strain on Caregiver Subjective Well-Being
| Model | b | S.E. | ΔR2 | F | |
|---|---|---|---|---|---|
| Step 1 | .25** | 10.66 | |||
| (Intercept) | 20.19** | .72 | |||
| Caregiver Strain (centered) | −.66* | .28 | |||
| Social Connectedness Component (centered) |
2.57** | .74 | |||
| Step 2 | .00 | .04 | |||
| (Intercept) | 20.17** | .73 | |||
| Caregiver Strain (centered) | −.66* | .28 | |||
| Social Connectedness Component (centered) |
2.54** | .76 | |||
| Interaction | −.04 | .20 |
Note. N = 76. b = unstandardized beta.
p < .05.
p < .01.
In the model predicting caregiver symptoms as reflected by the BSI, Step 1 was significant, with Caregiver Strain and Social Connections accounting for 26% of the variance in BSI scores. Both Social Connections (b = −4.20, p < .01) and Caregiver Strain (b =. 95, p < .05) were significantly associated with the BSI. However, in Step 2, the interaction (i.e., joint effect of Caregiver Strain and Social Connections) did not contribute significantly to the model, indicating that there was no significant interaction effect of Strain and Social Connections on caregiver symptoms.
In summary, the regression results indicate that caregiver strain and social connections both contributed significantly to variance in the two indicators of caregiver well-being. However, there was not a significant joint effect of caregiver strain and caregiver social connections found for either caregiver well-being variable. Because no interaction effect was found, no further test for moderation was warranted.
To explore the degree to which caregiver well-being is associated with family functioning and child adjustment and to assess which of these variables are most strongly associated with caregiver well-being, bivariate correlations (see Table 4) were run for the caregiver well-being variables, Caregiver Subjective Well-Being and the BSI, as well as the variables reflecting family relationships and child adjustment, the Relationship Dimension of the Family Environment Scale (FES), the Behavioral and Emotional Rating Scale (BERS-2), the Parent Child Rating Scale (PCRS), and the Oppositional Scale of the Connors Parent Rating Scale – Revised: Short Form (CPRS-R: S). Caregiver Subjective Well-being was significantly associated with the FES and the BERS, but not with the PCRS or the CPRS Oppositional Scale. The BSI was significantly associated with the BERS and PCRS but not with CPRS Oppositional scores.
Table 4.
Correlations Among Indicators of Caregiver Well-Being and Indicators of Child and Family Functioning
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Caregiver Subjective Well-Being | - | −.54** | .45** | .34** | .13 | −.07 |
| 2. Brief Symptom Inventory a | - | −.30* | −.38** | −.28* | .18 | |
| 3. FES Relationship Dimension | - | .34** | .08 | −.27* | ||
| 4. Behavioral and Emotional Rating Scale Strength Quotientb |
- | .69** | −.53** | |||
| 5. Parent Child Rating Scaleb | - | −.44** | ||||
| 6. CPRS Oppositional Subscale c | - |
Note. N=76.
Higher scores indicate more symptomatology.
Higher scores indicate higher levels of child strengths / more positive child adjustment.
Higher scores indicate more oppositional behavior.
p<.05.
p<.01.
In the next set of analyses, those variables that were significantly associated with caregiver well-being - the FES, the BERS and the PCRS - were regressed onto Caregiver Subjective Well-Being and the BSI. In all three regressions, Caregiver Subjective Well-Being and the BSI were entered together in one step to ascertain the degree in which caregiver well-being variables collectively contributed to the variance in child or family functioning.
The model testing the effects of caregiver well-being on family relationships was significant, with caregiver well-being accounting for 20% of the variance in the FES; Caregiver Subjective Well-Being contributed significantly to the model (b = .33, p < .01), but the BSI did not. The model testing the effects of caregiver well-being on BERS Strength Quotient scores was also significant; although neither single variable was a significant contributor, the two caregiver well-being factors together accounted for 16% of the variance in BERS scores. The model testing the effects of caregiver well-being on the PCRS scores was not significant.
Discussion
This study tested elements of a model of the relationships among social connections, strain, caregiver well-being, and family functioning in families of children with SED. The study’s most basic findings are as follows. Caregiver social connections and caregiver strain (i.e., strain directly related to parenting a child with SED) were significantly associated with caregiver well-being. However, there was no significant interaction effect of social support and caregiver strain, and therefore, no buffering effect of social support on the effects of caregiver strain on caregiver well-being. In addition, indicators of caregiver well-being were significantly associated with family relationships and positive child adjustment. These results indicate that when parents are more strained, the children in their care fare less well and families may experience more conflict. However, not all indicators of child adjustment were significantly related to caregiver well-being; child oppositional behavior was not found to be a significant correlate of caregiver well-being.
Limitations
Before considering the study’s findings and contributions, it is important to note several limitations. Most significantly, the relatively small sample size limited statistical power and restricted the ability to test the entire proposed model. Because participants were self-selected, it is impossible to compare the characteristics of the sample with the full range of caregivers and families who received information about the study. There is no way to know whether those caregivers who chose to participate differed significantly in terms of strain or concern from those who chose not to participate, or whether participants tended to be parents of children who were more or less well adjusted. Therefore, this sample may not be representative of all families of children with SED.
Past explorations of families with children with SED have focused on those with limited resources (i.e., lower SES; Center for Mental Health Services, 2000; Cook & Kilmer, 2010a; Kilmer et al., 2008). Because the participants in the current study were self-selected, it may be that this far more economically diverse sample is not reflective of those caregivers most in need of social connection. In other words, study families might be faring well relative to the general population of families of children with SED. Therefore, some study families may be experiencing relatively lower levels of strain and life stressors than their less financially stable counterparts. That said, prior work with this same sample documented the extremely high levels of adversity experienced by this sample (e.g., Kilmer et al., 2010).
Moreover, the current study relied solely on caregiver reports of all study variables, including family functioning and child adjustment. Youth views on the family situation and their own adjustment may have revealed associations not found in study results. Furthermore, it is important to note that the parent study was not designed specifically as an exploration of social connections and well-being. That is, it may be that measures designed particularly for this purpose and this population might have been more sensitive to such relationships. Thus, issues of measurement may account for some of the null findings. For instance, given the importance of context in influencing one’s needs for support and its potential benefits, as well as the multiple dimensions that may affect the degree to which perceived support relates to well-being, including the match between support needs and the type of support received (see, e.g., Cutrona & Russell, 1990; Haber, Cohen, Lucas, & Baltes, 2007), it may be that the social support scale used here did not sufficiently capture the aspects of support most pertinent to these caregivers.
In a similar vein, this study’s analyses - utilizing the specific measures available in the parent study - failed to yield significant correlations between some key social connections variables (i.e., religious participation and sense of community) and caregiver well-being. Although past findings linking religious participation and sense of community to strain reduction and well-being have been mixed (e.g., Bramston et al., 2002; Farrell et al., 2004; Obst & White 2005; Somlai & Heckman 2000; Speraw, 2006; Yatchmenoff et al., 1998), a more detailed religious participation measure or one designed to tap into perceived social connection via religious participation may have revealed an association between religious participation, strain, and well-being and contributed more strongly to the social connections principal component. Likewise, a more sensitive sense of community scale designed to measure the aspects of community most salient to parents of children with SED may have better reflected the aspects of community of greatest salience to these families. In addition, information about family strain and caregiver coping may have helped to create a more accurate portrait of these caregivers and their characteristics and contexts.
The data collected in the larger study were longitudinal; however, the current study drew from one time point only. Relationships among social connections, caregiver strain, and well-being are likely complex. It may well be that future longitudinal explorations that take into account changes in family strain, stress exposure, child needs, and caregiver demands over time reveal additional aspects regarding the nature of the relationships among these variables.
Conclusions and Future Directions
Despite the limitations, several study findings warrant discussion. This study explored the relationships among well-being and social connections in caregivers of children with SED, a relatively understudied population. In fact, although multiple studies have assessed caregiver strain in these families, few studies (see, e.g., Brannan & Heflinger, 2002, and Brannan et al., 2003 as exceptions) have examined the factors associated with this strain and its potential effect on the family system. More broadly, although much of the literature addresses the clinical needs and treatment options for the system-identified children, relatively few studies have explored the effects of caregiver well-being on other family members or the effect of strain associated with caring for a child with SED on the nondiagnosed children in the family. This study can serve as a foundation for future studies as findings here suggest that strain experienced by the caregiver can profoundly affect the rest of the family, particularly those children who otherwise might be doing well.
Although the failure to detect an interaction between social connections and caregiver strain might suggest that social connections do not affect strain or stress, it is essential to note that those caregivers reporting social connections with their neighborhoods and communities also reported fewer symptoms and a greater sense of life satisfaction. This suggests that parents who were more connected to their communities may be more likely to experience positive states of being regardless of level of strain (Lee et al., 2001; Lee & Robbins, 1998; Seeman, 1996). In support of this notion, there is much evidence to suggest the benefits of social connections for caregivers of children with SED (see Cook & Kilmer, 2010b).
The present study did not directly examine coping variables. Given the unpredictable nature of the symptoms associated with SED, it may be that for parents of children with SED, social connections facilitate one’s coping and adaptation in the face of strain but do not necessarily decrease strain meaningfully. Therefore, future studies might explore the ways in which professionals who serve children with SED may attend to family needs. For instance, helping to connect caregivers with prospects for building relationships with others, such as support groups or parent support organizations, may help to ease the effect of stress and strain felt by the entire family (see, e.g., Cook & Kilmer, 2010a, 2010b). Future studies might explore the effects of respite care for caregivers, family support programming, or support groups for parents of children with SED.
Although not all indicators of child adjustment were associated with caregiver well-being, there was a notable and significant association between caregiver well-being and child strengths. This finding warrants further investigation. It may be that when caregivers recognize their children’s strengths, such as positive peer interaction or academic achievement, children may be more likely to experience greater well-being. Focusing on child symptoms such as oppositionality may result in more negative experiences for both child and parent, such as conflict, nonoptimal parenting, or other adversities. This would be consistent with past findings that suggest that emotionally responsive and nurturing caregiving is associated with child socio-emotional strengths (Egeland, Carlson, & Sroufe, 1993). These findings begin to highlight specific ways in which caregiver wellness can affect child adjustment.
Children depend on their parents and caregivers for stability, safety, support, and assistance in helping them make sense of adverse events and life challenges (Masten et al., 1990). Nurturing, patient parenting is essential for children with SED who oftentimes have difficulties regulating their emotional and behavioral responses. In contrast, a caregiver who is overwhelmed or who has limited resources might lash out in frustration or anger. When the caregiver is under a great deal of pressure or is not well, he or she will be less able to be available, accessible, and responsive to the child’s needs, and that can contribute to greater difficulty adjusting and coping for the children. Given that many youngsters with SED experience challenges in emotional and behavioral regulation, adult caregivers who are emotionally stable and whose resources are not overly taxed may be essential. By strengthening community support and attending to parent and caregiver needs and well-being, family-serving professionals will be doing their utmost to ensure that the children with SED and their families thrive.
Acknowledgments
This research was supported by National Institute of Mental Health Award 1R03MH065596-01A2 to Kilmer and Cook.
References
- Armstrong MI, Birnie-Lefcovitch S, Ungar MT. Pathways between social support, family well being, quality of parenting, and child resilience: What we know. Journal of Child and Family Studies. 2005;14:269–281. [Google Scholar]
- Aunos M, Goupil G, Feldman M. Mothers with intellectual disabilities who do or do not have custody of their children. Journal on Developmental Disabilities. 2008;10:65–79. [Google Scholar]
- Baker DB, McCal K. Parenting stress in parents of children with attention-deficit hyperactivity disorder and parents of children with learning disabilities. Journal of Child and Family Studies. 1995;4:57–68. [Google Scholar]
- Bramston P, Pretty G, Chipuer H. Unraveling subjective quality of life: An investigation of individual and community determinants. Social Indicators Research. 2002;59:261–274. [Google Scholar]
- Brannan AM, Heflinger CA. Distinguishing caregiver strain from psychological distress: Modeling the relationships among child, family and caregiver variables. Journal of Child and Family Studies. 2002;10:405–418. [Google Scholar]
- Brannan AM, Heflinger CA, Foster EM. The role of caregiver strain and other family variables in determining children’s use of mental health services. Journal of Emotional and Behavioral Disorders. 2003;11:77–91. [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- Bronfenbrenner U, Morris PA. Theoretical models of human development. In: Lerner RM, Damon W, editors. Handbook of child psychology. Hoboken, NJ: John Wiley & Sons Inc.; 2006. pp. 793–828. [Google Scholar]
- Center for Mental Health Services. Annual Report To Congress on the Evaluation of the Comprehensive Community Mental Health Services for Children and Their Families Program , 2000. Atlanta, GA: ORC Macro; 2000. [Google Scholar]
- Chavis DM, Hogge JH, McMillan DW, Wandersman A. Sense of community through Brunswik’s lens: A first look. Journal of Community Psychology. 1986;14:24–40. [Google Scholar]
- Conners CK. Conners’ Rating Scales-Revised (CRS-R): Technical manual. North Tonawanda, NY: Multi-Health Systems, Inc.; 2001. [Google Scholar]
- Cook JR, Kilmer RP. Defining the scope of systems of care: An ecological perspective. Evaluation and Program Planning. 2010a;33:18–20. doi: 10.1016/j.evalprogplan.2009.05.006. [DOI] [PubMed] [Google Scholar]
- Cook JR, Kilmer RP. The importance of context in fostering responsive community systems: Supports for families in systems of care. American Journal of Orthopsychiatry. 2010b;80:115–123. doi: 10.1111/j.1939-0025.2010.01014.x. [DOI] [PubMed] [Google Scholar]
- Cowen EL, Hightower AD, Pedro-Carroll JL, Work WC, Wyman PA, Haffey WG. School-based prevention for children at risk: The Primary Mental Health Project. Washington, DC: American Psychological Association; 1996. [Google Scholar]
- Cutrona CE, Russell DW. Type of social support and specific stress: Toward a theory of optimal matching. In: Sarason BR, Sarason IG, Pierce GR, editors. Social support: An interactional view. New York, NY: John Wiley; 1990. pp. 319–366. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory (BSI-18): Administration, scoring, and procedures manual. Minneapolis, MN: NCS Pearson, Inc.; 2001. [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Egeland B, Carlson E, Sroufe L. Resilience as process. Development and Psychopathology. 1993;5:517–528. [Google Scholar]
- Epstein MH. BERS-2: Behavioral and Emotional Rating Scale examiners manual. 2nd ed. Austin, TX: Pro-Ed.; 2004. [Google Scholar]
- Farrell SJ, Aubry T, Coulombe D. Neighborhoods and neighbors: Do they contribute to personal well-being? Journal of Community Psychology. 2004;32:9–25. [Google Scholar]
- Green BL, Furrer C, McAllistar C. How do relationships support parenting? Effects of attachment style and social support on parenting behavior in an at-risk population. American Journal of Community Psychology. 2007;40:96–108. doi: 10.1007/s10464-007-9127-y. [DOI] [PubMed] [Google Scholar]
- Haber MG, Cohen JL, Lucas T, Baltes BB. The relationship between self-reported received and perceived social support: A meta-analytic review. American Journal of Community Psychology. 2007;39:133–144. doi: 10.1007/s10464-007-9100-9. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Brennan P. Social context, coping strategies, and depressive symptoms: An expanded model with cardiac patients. Journal of Personality and Social Psychology. 1997;72:918–928. doi: 10.1037//0022-3514.72.4.918. [DOI] [PubMed] [Google Scholar]
- Hoyt-Meyers LA, Cowen EL, Work WC, Wyman PA, Magnus KB, Fagen DB, Lotyczewski BS. Test correlates of resilient outcomes among highly stressed 2nd and 3rd grade urban children. Journal of Community Psychology. 1995;23:326–338. [Google Scholar]
- Keyes CLM, Shmotkin D, Ryff CD. Optimizing well-being: The empirical encounter of two traditions. Journal of Personality and Social Psychology. 2002;82:1007–1022. [PubMed] [Google Scholar]
- Kilmer RP, Cook JR, Palamaro Munsell E. Moving from principles to practice: Recommended policy changes to promote family-centered care. American Journal of Community Psychology. 2010;46:332–341. doi: 10.1007/s10464-010-9350-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer RP, Cook JR, Palamaro Munsell E, Kane Salvador S. Factors associated with positive adjustment in siblings of children with severe emotional disturbance: The roles of family resources and community life. American Journal of Orthopsychiatry. 2010;80(4):473–481. doi: 10.1111/j.1939-0025.2010.01050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer RP, Cook JR, Taylor C, Kane SR, Clark LY. Siblings of children with severe emotional disturbances: Risks, resources, and adaptation. American Journal of Orthopsychiatry. 2008;78:1–10. doi: 10.1037/0002-9432.78.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilmer RP, Cowen EL, Wyman PA, Work WC, Magnus KM. Differences in stressors experienced by urban African American, White, and Hispanic children. Journal of Community Psychology. 1998;26:415–428. [Google Scholar]
- Lee RM, Draper M, Lee S. Social connectedness, dysfunctional interpersonal behaviors and psychological distress: Testing a mediator model. Journal of Counseling Psychology. 2001;48:310–318. [Google Scholar]
- Lee RM, Robbins SB. The relationship between social connectedness and anxiety, self-esteem and social identity. Journal of Counseling Psychology. 1998;45:338–345. [Google Scholar]
- Linley PA, Matby J, Wood AM, Osbourne G, Hurling R. Measuring happiness: The higher order factor structure of subjective and psychological well-being measures. Personality and Individual Differences. 2009;49:878–884. [Google Scholar]
- Luescher JL, Dede DE, Gitten JC, Fennell E, Maria BL. Parental burden, coping, and family functioning in primary caregivers of children with Joubert Syndrome. Journal of Child Neurology. 1999;14:642–648. doi: 10.1177/088307389901401004. [DOI] [PubMed] [Google Scholar]
- Luthar SS. Poverty and children’s adjustment. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Masten AS, Best KM, Garmezy N. Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology. 1990;2:425–444. [Google Scholar]
- McDonald TP, Gregoire TK, Poertner J, Early TJ. Building a model of family caregiving for children with emotional disorders. Journal of Emotional and Behavioral Disorders. 1997;5:138–148. [Google Scholar]
- McMillan DW. Sense of community. Journal of Community Psychology. 1996;24:315–325. doi: 10.1002/jcop.22406. [DOI] [PubMed] [Google Scholar]
- Meadows SO, McLanahan SS, Brooks-Gunn J. Parental depression and anxiety and early childhood behavior problems across family types. Journal of Marriage and Family. 2007;69:1162–1177. [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale manual. 3rd Ed. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- Obst PL, White KM. An exploration of the interplay between psychological sense of community, social identification and salience. Journal of Community and Applied Social Psychology. 2005;15:127–135. [Google Scholar]
- Palamaro-Munsell E. The effects of caregiver social connectedness on caregiver, child and family well-being (Unpublished master’s thesis) Charlotte, NC: University of North Carolina at Charlotte; 2010. [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Yoko N, Weissman MM. Family discord, parental depression and psychopathology in offspring: 20 year follow-up. American Academy of Child and Adolescent Psychiatry. 2006;45:452–460. doi: 10.1097/01.chi.0000198592.23078.8d. [DOI] [PubMed] [Google Scholar]
- Powell LH, Shahabi L, Thorenson CE. Religion and spirituality: Linkages to physical health. American Psychologist. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- Prange ME, Greenbaum PE, Silver SE, Freidman RM. Family functioning and psychopathology among adolescents with severe emotional disturbances. Journal of Abnormal Child Psychology. 1992;20:83–102. doi: 10.1007/BF00927118. [DOI] [PubMed] [Google Scholar]
- Quittner AL, Glueckauf RL, Jackson DN. Chronic parenting stress: Moderating versus mediating effects of social support. Journal of Personality and Social Psychology. 1990;59:1266–1278. doi: 10.1037//0022-3514.59.6.1266. [DOI] [PubMed] [Google Scholar]
- Seeman TE. Social ties and health: The benefits of social integration. Annals of Epidemiology. 1996;6:442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Somlai AM, Heckman TG. Correlates of spirituality and well-being in a community sample of people living with HIV disease. Mental Health, Religion & Culture. 2000;3:57–70. [Google Scholar]
- Song L, Singer M. Life stress, social support, coping and depressive symptoms: A comparison between the general population and family caregivers. International Journal of Social Welfare. 2006;15:172–180. [Google Scholar]
- Speraw S. Spiritual experiences of parents and caregivers who have children with disabilities or special needs. Issues in Mental Health Nursing. 2006;27:213–230. doi: 10.1080/01612840500436974. [DOI] [PubMed] [Google Scholar]
- Taylor-Richardson KD, Heflinger CA, Brown TN. Experience of strain among types of caregivers responsible for children with serious emotional and behavioral disorders. Journal of Emotional and Behavioral Disorders. 2006;14:157–168. [Google Scholar]
- White N, Hastings RP. Social and professional support for parents of adolescents with severe intellectual disabilities. Journal of Applied Research in Intellectual Disabilities. 2004;17:181–190. [Google Scholar]
- Williams P, Barclay L, Schmeid V. Defining social support in context: A necessary step in improving research, intervention, and practice. Qualitative Health Research. 2004;14:942–960. doi: 10.1177/1049732304266997. [DOI] [PubMed] [Google Scholar]
- Yatchmenoff DK, Koren PE, Friesen BJ, Gordon LJ, Kinney RF. Enrichment and stress in families caring for a child with a serious emotional disorder. Journal of Child and Family Studies. 1998;7:129–145. [Google Scholar]