Abstract
Background
A simple test of aerobic fitness for patients with traumatic brain injury (TBI) that is valid, reliable, and responsive to change is needed to provide clinicians a functional measure of cardiorespiratory capacity.
Objective
The purpose of this study was to examine the validity and responsiveness to change of the Six-Minute Walk Test (6MWT) in individuals with TBI.
Design
A cohort, pretest-posttest, comparison study was conducted.
Methods
Twenty-one patients performed the 6MWT upon admission to and prior to discharge from a postacute rehabilitation facility. Heart rate and distance traveled were recorded. A physiologic cost index (PCI) (beats per meter) was calculated based on steady-state heart rate. At discharge, all participants were able to perform a graded treadmill exercise test to exhaustion during which peak oxygen consumption (V̇o2) was measured.
Results
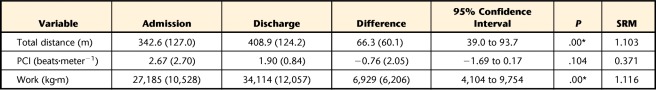
Between admission and discharge, mean total distance increased from 342.6 m (SD=127.0) to 408.9 m (SD=124.2), and work increased from 27,185 kg·m (SD=10,528) to 34,114 kg·m (SD=12,057). The effect size indexes were 1.10 and 1.12 for distance and work, respectively. Correlations (r) between the discharge peak V̇o2 and the discharge 6MWT distance, PCI, and work were .58, −.61, and .47, respectively.
Limitations
Stratification by gait speed may have improved responsiveness, especially for the slow ambulators.
Conclusions
All measures correlated well with peak V̇o2, establishing an acceptable level of criterion-related (concurrent) validity. The addition of heart rate and calculating the PCI was only slightly better at predicting peak V̇o2, albeit nonsignificant, than a simple measure of total distance. The 6MWT provides a good estimate of peak aerobic capacity, and some measures are more responsive to change than others in patients recovering from TBI.
The Centers for Disease Control and Prevention estimates that at least 5.4 million Americans currently have long-term or lifelong need for help in performing activities of daily living as a result of a traumatic brain injury (TBI).1 Associated direct medical costs and indirect costs such as lost productivity totaled approximately $60 billion in the United States in 2000.1 Cognitive and neuropsychologic impairments often accompany the motor impairment, making the assessment of overall physical endurance capacity in patients with TBI a special challenge. A simple test that is sensitive to the physical and cognitive constraints unique to TBI and that is valid, reliable, and responsive to change in the patient's endurance capacity is lacking.
Timed walk/run tests have been in use for more than 50 years, and the first clinical populations studied were patients with pulmonary and cardiovascular disease.2,3 Walk time duration has varied, and it has been suggested that the Six-Minute Walk Test (6MWT) is the best compromise between test duration and ability to discriminate among varying levels of cardiorespiratory fitness.4 In this context, the 6MWT is a measure of functional walking capacity that evaluates the ability of an individual to increase his or her activity level and then maintain a moderate level of physical activity over a period that may be reflective of activities of daily living.5
The 6MWT has since been validated in patients with musculoskeletal impairments,6 other samples of patients with pulmonary pathology,7–9 and patients with cardiovascular disease.10–13 In patients with neurological impairments, the 6MWT has been used and evaluated to determine the functional capacity during recovery from stroke.14–16
In addition to measuring total distance traveled, heart rate response has been incorporated to give an estimate of energy expenditure or physiologic cost.17–21 A physiologic cost index (PCI) offers the advantage of capturing increases in ambulatory and metabolic efficiency that occur when the distance traveled during 6 minutes may not increase, but a lower heart rate is elicited during the task. Eng and colleagues5 recommended that the total distance of a functional walk test be combined with blood pressure and heart rate measurements to better assess the physiologic demand of the activity in patients recovering from stroke. Other authors22,23 have advocated the addition of body weight (estimating total work) to improve the capacity of the 6MWT for predicting endurance.
The gold standard for measuring endurance capacity and cardiorespiratory fitness is a graded exercise test during which oxygen consumption (V̇o2), carbon dioxide production, and pulmonary ventilation are measured. This is an expensive and complex test requiring a great deal of cooperation on the part of the individual being assessed, which can be problematic for patients with TBI, who often have cognitive impairments and motivational challenges. This is a large population of patients, and a simple method to measure endurance capacity that is less burdensome on clinicians and patients recovering from TBI is needed. The 6MWT is a standardized test of endurance capacity that has been shown to be reliable and valid in other patient populations.6–16 When used in rehabilitation settings, an evaluative instrument such as the 6MWT also should be responsive to change. The purpose of this study was to examine the validity and responsiveness to change of the 6MWT in a sample of individuals with TBI. We hypothesized that the total distance, total work, and PCI would be responsive to change over the course of a rehabilitation intervention and would yield results that correlated well with a measure of endurance capacity and cardiorespiratory fitness.
Method
Participants
A total of 21 patients (15 male, 6 female) admitted to a postacute residential rehabilitation center gave written consent to participate in the study. Inclusion criteria were 18 to 60 years of age, no overt cardiovascular disease, the ability to follow 2-step commands, and the ability to ambulate without manual assistance. The participants had a mean age of 30.1 years (SD=11.6, range=16–59) and a mean time since injury of 15.8 months (SD=13.7, range=3–50). Median time since injury was approximately 13 months; 19 participants were between 3 months and 3 years postinjury. Twenty participants had severe injuries (Glasgow Coma Scale [GCS] score=3–8), and 1 participant had a moderate injury (GCS score=10). Motor vehicle accidents were the cause of injury in 18 participants.
As with most samples of patients recovering from TBI, there was large variability in physical and cognitive abilities. All participants followed an individualized program of occupational therapy, physical therapy, speech therapy, therapeutic recreation, and neuropsychotherapy. On average, they attended individual physical therapy treatment sessions 3 to 5 times per week during the time between the pretest and posttest sessions. Each of these sessions was 1 hour in length and consisted of general and specific coordination, strength, and flexibility exercises, depending on the particular impairments of the participant. Depending on the severity of impairment, therapy sessions also included low-intensity aerobic activities. The aerobic component followed established guidelines for frequency, duration, and type (mode) of exercise.24 Depending on the physical and cognitive impairments, the mode of exercise included, but was not limited to, treadmill and elliptical training, semirecumbent reciprocal arm and leg training, stationary and community cycling, and aquatics. However, intensity of training was not optimal and averaged 30% to 50% of heart rate reserve rather than the recommended 60% to 90%.24 Seventy-five percent of the study sample also participated in group exercise activities that primarily consisted of trunk and upper- and lower-extremity active range of motion 2 to 3 times per week.
Qualifications for participating in the study included the ability to ambulate independently with or without an assistive device at a speed of ≥13.41 m/min (0.5 mph) for ≥50 m over level surfaces with minimal supervision. Eleven of the 21 patients studied were unable to perform the peak V̇o2 test on a treadmill upon admission. Performance of the treadmill test included: (1) the ability to walk at least 13.41 m/min (0.5 mph) safely without manual assistance, (2) the ability to safely balance and coordinate stepping on the moving belt, (3) the ability to ambulate at least 7 minutes to allow physiologic and metabolic systems to adjust to changing workloads, and (4) the ability to meet 2 of 3 peak V̇o2 criteria stated below. Also, those individuals who could not adhere to the exhaled gas collection requirements were excluded from the study.
Procedure
The 6MWT was performed upon admission to the facility and just prior to discharge. A chest strap and wristwatch telemetry unit (Polar Vantage XL Heart Rate Monitor, Polar CIC, Port Washington, New York) monitored heart rate continuously throughout the test. Participants were instructed to walk around a rectangular track as many times as possible in 6 minutes. The track was set up in an area that measured approximately 12 m × 6 m. Plastic cones marked the corners of the track, indicating where the participant changed direction, always turning left 90 degrees. Participants were requested to walk around the cones as many times as possible in the 6-minute period at a fast but safe speed. Verbal encouragement was standardized and included the phrase “you are doing fine” after every minute. At minutes 4 and 5, the participants were told they had 2 minutes and 1 minute, respectively, left to walk. The distance traveled was recorded in meters after completion. The total distance walked and the PCI have been shown to have high test-retest reliability for individuals with TBI (intraclass correlation coefficient [ICC 2,1] for distance=.94, ICC [2,1] for PCI=.89).25 Based on these previous data and the desire to minimize the burden of testing on patients and clinicians, no practice trials were included.
At discharge, all participants could safely perform a graded treadmill exercise test to exhaustion in which peak V̇o2 was measured. Discharge testing was performed 2 to 3 days before or after the discharge 6MWT. During graded exercise testing, the participants' resting and exercise heart rate were monitored by electrocardiography (Cardio Perfect Inc, Atlanta, Georgia). Minute ventilation, V̇o2, and carbon dioxide production during rest and exercise were determined by an automated metabolic cart (Medical Graphics Corp, St Paul, Minnesota). The metabolic cart was calibrated before each test using gases of known concentration. The pneumotach was calibrated with a 3-L syringe. Gas exchange data were averaged over 20-second intervals and used as submaximal and peak values.
Aerobic capacity was measured while ambulating on a treadmill, and participants were allowed to use handholds for balance and safety. Handholds were mandatory for those patients who used an assistive device for overground walking but for balance purposes only. Speed of the treadmill was held constant and dependent on the severity of the participant's gait impairment. Actual treadmill speeds ranged from 18.8 to 88.5 m/min (0.7–3.3 mph), with a mean speed of 67.4 m/min (SD=22.8) (X̅=2.5 mph, SD=0.8). Exhaustion was brought about by 2% increases in slope of the treadmill every minute. Participants were instructed to give their best effort and told that there was no set duration they were expected to walk. This testing protocol is a modification of the Balke stress test,26 and has been used previously in patients with TBI.27,28 Both submaximal and peak responses have been shown to be reliable in this population (ICC [2,1] for peak V̇o2=.92).29 The primary goal of testing was to encourage the participants to give a maximal effort. Quantitative indicators of peak aerobic capacity included: (1) reaching 85% to 90% of age-predicted maximum heart rate, (2) a plateau in V̇o2 with an increase in workload, and (3) a respiratory exchange ratio equal to or greater than 1.10.24 More importantly, the test was stopped if a participant's safety became compromised or if he or she requested to stop. No manual assistance was provided during any of the testing procedures.
Data Analysis
Steady-state heart rate was calculated by averaging the heart rate at the end of minutes 3 through 6 of the 6MWT. The PCI (beats per meter)19 was calculated by dividing heart rate (beats per minute) by gait speed (m/min). Work on the 6MWT was calculated by multiplying total distance by body weight.22,23 Paired-samples t tests were performed on admission and discharge 6MWT results. Furthermore, standardized response means (SRMs)30 were calculated by dividing the mean differences by their respective standard deviations to better characterize responsiveness and the signal-to-noise ratio. Pearson product moment coefficients were calculated correlating peak V̇o2 with: (1) discharge 6MWT total distance, (2) discharge 6MWT PCI, and (3) discharge 6MWT total work. Correlating the discharge data was necessary because not all participants could safely perform the graded treadmill test upon admission or meet the peak criteria stated above. Simple linear regression analyses were performed to develop a prediction equation for each of the 3 predictor variables. Statistical analyses were performed with a desktop statistical analysis program (SPSS version 17.0. SPSS Inc, Chicago, Illinois) at an alpha level of .05 (2-tailed). A Bonferroni adjustment was used to compensate for the multiple comparisons.
Role of the Funding Source
This work was supported by the National Institute of Child Health and Human Development and the Moody Foundation.
Results
Responsiveness
The time between admission and discharge testing ranged from 8 to 25 weeks, with an average follow-up time of 17.7 weeks (SD=4.6). The median duration of treatment was 18 weeks. The values at admission and discharge for the 6MWT are displayed in the Table. Significant differences were found between admission and discharge distance and work outcomes (P<.001). There was a 28% decline in PCI at discharge, but the difference was not significant. However, the tendency for PCI to decrease suggests an increase in efficiency of ambulation was achieved. Three participants used ankle-foot orthoses on both admission and discharge tests. One participant progressed from an elevated forearm support walker to a standard rolling walker. Another participant progressed from a standard rolling walker to a single-point cane. All other participants did not require assistive devices upon admission or discharge.
Table.
Differences Between Admission and Discharge Variables for the Six-Minute Walk Testa
Values at admission and discharge for the Six-Minute Walk Test and for difference between admission and discharge are mean (SD). Asterisk indicates significant difference prior to Bonferroni adjustment (P<.0125). SRM=standardized response mean, PCI=physiologic cost index.
In addition to comparing means, the SRM is shown in the Table. The SRM is reported in order to capture data from all participants regardless of whether they improved, remained stable, or declined in performance. It also differs from the effect size in that it factors in the variability of the change scores rather than the variability of the baseline scores. According to Liang and colleagues,30 it resembles the t statistic but does not factor in sample size. Using Cohen's guidelines31 a value of 0.2 is considered weak, 0.5 is considered moderate, and ≥0.8 is considered a large effect.
Validity
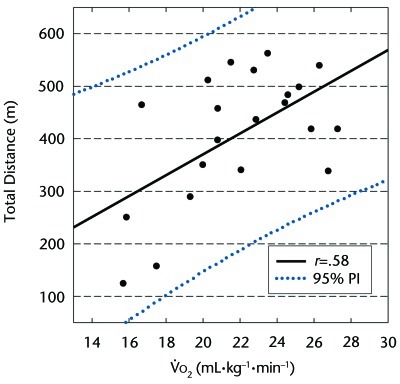
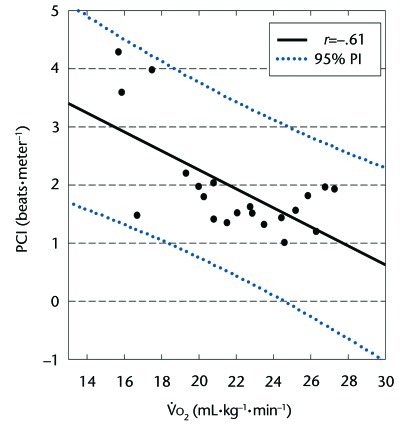
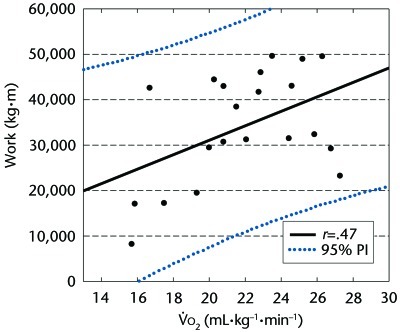
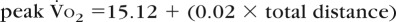
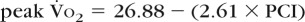
The correlation (r) between the discharge peak V̇o2 on the graded treadmill test and the 6MWT total distance was .58 (Fig. 1). The correlation between peak V̇o2 and PCI was −.61 (Fig. 2). When taking body weight into account and calculating work, the correlation (r) with peak V̇o2 normalized for body weight (mL·kg−1·min−1) was .47 (Fig. 3). Simple regression analyses were performed using 6MWT total distance, PCI, and work as predictors of peak V̇o2. Results were as follows:
- 6MWT total distance as a predictor variable for peak V̇o2 (r=.58, R2=.34, adjusted R2=.30, standard error of the estimate [SEE]=2.98). The prediction equation is as follows (F1,19=9.60, P=.006):
- 6MWT PCI as a predictor variable for peak V̇o2 (r=.61, R2=.38, adjusted R2=.35, SEE=2.88). The prediction equation is as follows (F1,19=11.52, P=.003):
- 6MWT work as a predictor variable for peak V̇o2 (r=.47, R2=.22, adjusted R2=.18, SEE=3.22). The prediction equation is as follows (F1,19=5.38, P=.032):
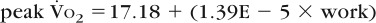
Figure 1.
The peak oxygen consumption (V̇o2) of the 21 participants during graded exercise testing matched with their total distance covered during the Six-Minute Walk Test at discharge. PI=prediction interval.
Figure 2.
The peak oxygen consumption (V̇o2) of the 21 participants during graded exercise testing matched with Six-Minute Walk Test physiologic cost index (PCI) at discharge. PI=prediction interval.
Figure 3.
The peak oxygen consumption (V̇o2) of the 21 participants during graded exercise testing matched with Six-Minute Walk Test work at discharge. PI=prediction interval.
Discussion
Prior to this report, there had been no effort to assess the responsiveness and validity of the 6MWT in patients recovering from TBI. We found that responsiveness varied depending on the variable measured, as did the validity (predictability). Total distance and work were the most responsive, whereas physiologic cost (PCI) tended to be a better, albeit not significant, predictor of peak V̇o2. Work tended to have the least predictive ability. Total distance is the variable most often reported in studies utilizing the 6MWT as an outcome variable. The average distance upon admission for patients with TBI in this study was 342 m and was not significantly different from values reported for other patients with neurologic impairments (ie, stroke).14–16
Unfortunately, few studies have investigated the responsiveness of the 6MWT, especially in patients with neurological impairments. Duncan and colleagues32 used the 6MWT to assess changes in endurance in patients with mild to moderate cerebrovascular accident in response to a supervised home exercise program. Change scores were reported for the 6MWT (∼59 m) and are on the same order as those reported here. Unfortunately, standard deviations were not reported, precluding the assessment of responsiveness. Latham and colleagues33 followed patients after hip fracture and found the 6MWT distance to be responsive (SRM=1.11) and on the same order of magnitude as in our patients with TBI. Demers and coworkers34 followed patients with heart failure and examined the responsiveness of the 6MWT to various pharmacologic interventions. They did not find the 6MWT distance to be responsive to change (SRM ranged from −0.009 to 0.269). In another study of patients with heart failure, the 6MWT was found to have an effect size of 0.85.35
Regarding validity, Cooper36 was the first to report on the relationship between a treadmill test performed in the laboratory and a 12-minute walk/run test performed in the field in young US Air Force personnel who were healthy and found a correlation coefficient of .90. In patients with chronic pulmonary disease, McGavin and colleagues2 reported a correlation of .52 when comparing a 12-minute walk test with V̇o2 determined by cycle ergometry. Unfortunately, nearly all validity studies have used the cycle ergometer to measure peak V̇o2. This finding is problematic given that performance on the cycle ergometer usually is limited by quadriceps muscle fatigue, and consequently V̇o2 is significantly less compared with treadmill exercise.37 These same findings were reported in patients with TBI.27 The only study, besides the study by Cooper, that compared a timed walk test distance with treadmill exercise was in patients with rheumatoid arthritis and osteoarthritis and had a correlation coefficient of .87.6 However, that study assessed only 5 patients and used 5-minute walk distance rather than the 6MWT distance.
Other patient populations have been studied extensively, particularly those with pulmonary and cardiovascular disease. Although some authors have found moderate to high correlations with maximum V̇o2, others have found low and insignificant relationships. For patients with cardiovascular accident, correlation coefficients ranged from .37 to .84.14–16 For other patient populations, primarily those with cardiovascular and pulmonary impairments, the coefficients ranged from .36 to .78 (for a review, see Solway et al38). Again, the majority of these studies examined only distance and used a cycle ergometer to measure peak V̇o2.
In addition to studies assessing the validity of total distance measures, there are 2 reports in which 6MWT work has been approximated and correlated to peak V̇o2. Carter and coworkers22 found that total distance alone had a correlation coefficient of .54. When body weight was factored in (distance × weight=work), the correlation improved to .81. Oudiz and colleagues23 utilized a similar method and found the correlation improved from .48 to .76. However, these relationships were based on absolute peak V̇o2 (mL·min−1) and not body weight–normalized peak V̇o2 (mL·kg−1·min−1). Our results were similar when assessing the relationship between the absolute V̇o2 and 6MWT work (r=.47, P=.032 versus r=.70, P<.001). The increase in the relationship is not unexpected, and one should be cautious using absolute V̇o2 because a heavier person has the potential to perform more work and consume more oxygen simply because he or she has more mass. Furthermore, nearly all normative values for peak aerobic capacity are based on weight-normalized V̇o2.
Including the heart rate response as part of the 6MWT provides the clinician with an estimate of the intensity of the work being performed. By combining heart rate with gait speed, the number of heart beats per meter walked (PCI) can be derived. Because heart rate and V̇o2 are linearly related, the PCI can be used to estimate energy expenditure. Indeed, the simple regressions suggest that PCI was slightly better at predicting peak V̇o2 in this study. However, we did not find it to be the most responsive to change over time. Although there was a tendency for PCI to decline (improvement of 28%) as a result of treatment (increased gait efficiency), the lower responsiveness (SRM) may have been due to the high variability across participants. It also may have been a reflection of the type of treatment the participants received. Emphasis is typically on improving balance, coordination, and strength and not on cardiorespiratory endurance in patients who function at a low level physically. Regardless, clinicians should still be encouraged to include a heart rate response with the 6MWT given the ease with which these data can be collected. If a portable heart rate monitor similar to the one used in this study is not available, clinicians can easily palpate a 10-second recovery pulse at the conclusion of the 6MWT.
Limitations include the small sample size, which did not allow for development of a statistically sound multiple regression model. In addition, future studies should consider stratification of patients into subgroups based on gait speed. Stratification based on gait speed would likely result in less variability within the subsamples and improve responsiveness, but the lower variability may reduce the predictive capacity of a future model. On the other hand, it may reveal that the 6MWT is more or less responsive and valid in certain subgroups of patients. The answer to this question will come when more patients can be studied.
Conclusions
Patients with acquired brain injury commonly complain of fatigue and have decreased functional walking capacity and endurance.27,39,40 It would be helpful to the clinician if there were a responsive and valid measure of endurance capacity. In our study, the total distance and work performed on the 6MWT were found to be responsive to change in a sample of patients with TBI undergoing postacute residential rehabilitation. The observed difference in total distance walked and the lack of significant change in PCI indicate that the participants were able to increase their gait speed at the same level of exertion, suggesting an improvement in ambulatory efficiency. The results suggest that 6MWT PCI is a slightly better predictor of peak V̇o2 than total distance or work. However, accurately measuring heart rate during the walk may be problematic without the right tools, and the addition of some calculations may increase the burden on a busy clinician. Total distance has an advantage from a simplicity standpoint. We do not recommend using work as a predictor of peak V̇o2 because the adjusted R2 value indicates it accounts for only 18% of the variability. Overall, the 6MWT is a good estimate of peak aerobic and endurance capacity in patients in the postacute phase of recovery from TBI. As a measure of endurance capacity, the 6MWT combined with a measure of heart rate response could replace the more sophisticated and complex measure of peak V̇o2 and help assess the effectiveness of cardiopulmonary conditioning programs in a simple and cost-effective way in patients recovering from TBI. Improving cardiorespiratory fitness should be part of a holistic approach to treatment.
The Bottom Line
What do we already know about this topic?
The validity and reliability of the Six-Minute Walk Test (6MWT) has been studied in a variety of patient populations. Very little has been published on this clinical test in patients with traumatic brain injury (TBI).
What new information does this study offer?
In the postacute phase of rehabilitation, the 6MWT administered to patients with TBI is responsive to change and is a good predictor of cardiorespiratory fitness. Adding a measure of heart rate response improves the predictive ability of the test.
If you're a patient, what might these findings mean to you?
The 6MWT is a very simple test to perform and is a good predictor of endurance and aerobic capacity in patients with TBI.
Footnotes
Dr Mossberg provided concept/idea/research design, data analysis, and fund procurement. Both authors provided writing and project management. Ms Fortini provided data collection, participants, facilities/equipment, institutional liaisons, and consultation (including review of manuscript before submission). The authors acknowledge the technical assistance of Paula Skinkis, MEd.
Committees for the protection of human subjects at the Transitional Learning Center and the University of Texas Medical Branch approved the procedures. All HIPAA guidelines were followed.
This work was supported by the National Institute of Child Health and Human Development and the Moody Foundation.
References
- 1. Centers for Disease Control and Prevention Injury prevention and control: traumatic brain injury. Available at: http://www.cdc.gov/traumaticbraininjury/tbi_ed.html Accessed March 10, 2011
- 2. McGavin CR, Gupta SP, McHardy GJ. Twelve-minute walking test for assessing disability in chronic bronchitis. Br Med J. 1976;1:822–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923 [PMC free article] [PubMed] [Google Scholar]
- 4. Butland RJ, Pang J, Gross ER, et al. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed). 1982;284:1607–1608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eng JJ, Chu KS, Dawson AS, et al. Functional walk tests in individuals with stroke: relation to perceived exertion and myocardial exertion. Stroke. 2002;33:756–761 [DOI] [PubMed] [Google Scholar]
- 6. Price LG, Hewett JE, Kay DR, Minor MA. Five-minute walking test of aerobic fitness for people with arthritis. Arthritis Rheum. 1988;1:33–37 [Google Scholar]
- 7. Cahalin L, Pappagianopoulos P, Prevost S, et al. The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest. 1995;108:452–459 [DOI] [PubMed] [Google Scholar]
- 8. Nixon PA, Joswiak ML, Fricker FJ. A six-minute walk test for assessing exercise tolerance in severely ill children. J Pediatr. 1996;129:362–366 [DOI] [PubMed] [Google Scholar]
- 9. Eaton T, Young P, Milne D, Wells AU. Six-minute walk, maximal exercise tests: reproducibility in fibrotic interstitial pneumonia. Am J Respir Crit Care Med. 2005;171:1150–1157 [DOI] [PubMed] [Google Scholar]
- 10. Cahalin LP, Mathier MA, Semigram MJ, et al. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;110:325–332 [DOI] [PubMed] [Google Scholar]
- 11. Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46:706–711 [DOI] [PubMed] [Google Scholar]
- 12. Lucas C, Stevenson LW, Johnson W, et al. The 6-min walk and peak oxygen consumption in advanced heart failure: aerobic capacity and survival. Am Heart J. 1999;138(4 pt 1):618–624 [DOI] [PubMed] [Google Scholar]
- 13. Zugck C, Kruger C, Durr S, et al. Is the 6-minute walk test a reliable substitute for peak oxygen uptake in patients with dilated cardiomyopathy? Eur Heart J. 2000;21:540–549 [DOI] [PubMed] [Google Scholar]
- 14. Kelly JO, Kilbreath SL, Davis GM, et al. Cardiorespiratory fitness and walking ability in subacute stroke patients. Arch Phys Med Rehabil. 2003;84:1780–1785 [DOI] [PubMed] [Google Scholar]
- 15. Eng JJ, Dawson AS, Chu KS. Submaximal exercise in persons with stroke: test-retest reliability and concurrent validity with maximal oxygen consumption. Arch Phys Med Rehabil. 2004;85:113–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tang A, Sibley KM, Bayley MT, et al. Do functional walk tests reflect cardiorespiratory fitness in sub-acute stroke? J Neuroeng Rehabil. 2006;3:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Berg K. Heart rate telemetry for evaluation of the energy expenditure of children with cerebral palsy. Am J Clin Nutr. 1971;24:1438–1445 [DOI] [PubMed] [Google Scholar]
- 18. Stallard J, Rose GK, Tait JH, Davies JB. Assessment of orthoses by means of speed and heart rate. J Med Eng Technol. 1978;2:22–24 [DOI] [PubMed] [Google Scholar]
- 19. MacGregor J. The evaluation of patient performance using long-term ambulatory monitoring technique in the domiciliary environment. Physiotherapy. 1981;67:30–33 [PubMed] [Google Scholar]
- 20. Nene AV, Patrick JH. Energy cost of paraplegic locomotion using the ParaWalker: electrical stimulation “hybrid” orthosis. Arch Phys Med Rehabil. 1990;71:116–120 [PubMed] [Google Scholar]
- 21. Mossberg KA, Linton KA, Friske K. Ankle-foot orthoses: effect on energy expenditure of gait in spastic diplegic children. Arch Phys Med Rehabil. 1990;71:490–494 [PubMed] [Google Scholar]
- 22. Carter R, Holiday DB, Nwasuruba C, et al. 6-minute walk work for assessment of functional capacity in patients with COPD. Chest. 2003;123:1408–1415 [DOI] [PubMed] [Google Scholar]
- 23. Oudiz RJ, Barst RJ, Hansen JE, et al. Cardiopulmonary exercise testing and six-minute walk correlations in pulmonary arterial hypertension. Am J Cardiol. 2006;97:123–126 [DOI] [PubMed] [Google Scholar]
- 24. Thompson WR, ed. ACSM's Guidelines for Exercise Testing and Prescription. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010 [Google Scholar]
- 25. Mossberg KA. Reliability of a timed walk test in persons with acquired brain injury. Am J Phys Med Rehabil. 2003;82:385–390 [DOI] [PubMed] [Google Scholar]
- 26. Balke B, Ware RW. An experimental study of physical fitness of Air Force personnel. US Armed Forces Med J. 1959;10:675–688 [PubMed] [Google Scholar]
- 27. Hunter M, Tomberlin J, Kirkikis C, Kuna ST. Progressive exercise testing in closed head-injured subjects: comparison of exercise apparatus in assessment of a physical conditioning program. Phys Ther. 1990;70:363–371 [DOI] [PubMed] [Google Scholar]
- 28. Mossberg KA, Kuna S, Masel B. Ambulatory efficiency in persons with acquired brain injury after a rehabilitation intervention [erratum in: Brain Inj. 2003;17:266]. Brain Inj. 2002;16:789–797 [DOI] [PubMed] [Google Scholar]
- 29. Mossberg KA, Greene BP. Reliability of graded exercise testing after traumatic brain injury: submaximal and peak responses. Am J Phys Med Rehabil. 2005;84:492–500 [DOI] [PubMed] [Google Scholar]
- 30. Liang MH, Fossel AH, Larson MG. Comparisons of five health status instruments for orthopedic evaluation. Med Care. 1990;28:632–642 [DOI] [PubMed] [Google Scholar]
- 31. Cohen J. A power primer. Psychol Bull. 1992;112:155–159 [DOI] [PubMed] [Google Scholar]
- 32. Duncan P, Richards L, Wallace D, et al. A randomized, controlled pilot study of a home-based exercise program for individuals with mild and moderate stroke. Stroke. 1998;29:2055–2060 [DOI] [PubMed] [Google Scholar]
- 33. Latham NK, Mehta V, Nguyen AM, et al. Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil. 2008;89:2146–2155 [DOI] [PubMed] [Google Scholar]
- 34. Demers C, McKelvie RS, Negassa A, et al. Reliability, validity, and responsiveness of the six-minute walk test in patients with heart failure. Am Heart J. 2001;142:698–703 [DOI] [PubMed] [Google Scholar]
- 35. O'Keeffe ST, Lye M, Donnellan C, Carmichael DN. Reproducibility and responsiveness of quality of life assessment and six minute walk test in elderly heart failure patients. Heart. 1998;80:377–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cooper KH. A means of assessing maximal oxygen intake: correlation between field and treadmill testing. JAMA. 1968;203:201–204 [PubMed] [Google Scholar]
- 37. Hermansen L, Saltin B. Oxygen uptake during maximal treadmill and bicycle exercise. J Appl Physiol. 1969;26:31–37 [DOI] [PubMed] [Google Scholar]
- 38. Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119:256–270 [DOI] [PubMed] [Google Scholar]
- 39. Vitale AE, Jankowski LW, Sullivan SJ. Reliability of a walk/run test to estimate aerobic capacity in a brain-injured population. Brain Inj. 1997;11:67–76 [DOI] [PubMed] [Google Scholar]
- 40. Mossberg KA, Ayala D, Baker T, et al. Aerobic capacity after traumatic brain injury: comparison with a nondisabled cohort. Arch Phys Med Rehabil. 2007;88:315–320 [DOI] [PubMed] [Google Scholar]