Abstract
Background and Purpose
Persistent deficits in gait speed and spatiotemporal symmetry are prevalent following stroke and can limit the achievement of community mobility goals. Rehabilitation can improve gait speed, but has shown limited ability to improve spatiotemporal symmetry. The incorporation of combined visual and proprioceptive feedback regarding spatiotemporal symmetry has the potential to be effective at improving gait.
Case Description
A 60-year-old man (18 months poststroke) and a 53-year-old woman (21 months poststroke) each participated in gait training to improve gait speed and spatiotemporal symmetry. Each patient performed 18 sessions (6 weeks) of combined treadmill-based gait training followed by overground practice. To assist with relearning spatiotemporal symmetry, treadmill-based training for both patients was augmented with continuous, real-time visual and proprioceptive feedback from an immersive virtual environment and a dual belt treadmill, respectively.
Outcomes
Both patients improved gait speed (patient 1: 0.35 m/s improvement; patient 2: 0.26 m/s improvement) and spatiotemporal symmetry. Patient 1, who trained with step-length symmetry feedback, improved his step-length symmetry ratio, but not his stance-time symmetry ratio. Patient 2, who trained with stance-time symmetry feedback, improved her stance-time symmetry ratio. She had no step-length asymmetry before training.
Discussion
Both patients made improvements in gait speed and spatiotemporal symmetry that exceeded those reported in the literature. Further work is needed to ascertain the role of combined visual and proprioceptive feedback for improving gait speed and spatiotemporal symmetry after chronic stroke.
Following stroke, intensive rehabilitation is used to reduce deficits in gait speed, efficiency, and symmetry. Restoring symmetric gait is important to improve gait efficiency and gait speed1,2 and to decrease the risk of lower-extremity musculoskeletal injury3 and loss of bone mineral density in the paretic limb.4 Although treadmill-based locomotor training programs can improve gait speed during both the subacute and chronic stages poststroke,5 deficits in gait speed persist, whereas spatiotemporal asymmetries remain largely unaltered.6–10 A limitation of treadmills, as a training modality, is that optic flow is eliminated. Optic flow is the visual motion sensed at the eye as the body moves through the environment and is important for controlling gait speed11,12 and stride length.12 Restoring the optic flow of forward motion, by incorporating a virtual environment (VE) into training performed on a treadmill, may increase immersion and motivation,13 making visual information regarding movement relevant and important for improving walking patterns.11
To improve movement patterns during walking, locomotor training is thought to require the production of consistent, “kinematically correct” limb movements.10 In contrast, an assist-as-needed paradigm may promote greater gains,14,15 as the patient is allowed to sense and self-correct his or her own movement errors. Because it is critical that movement errors are perceived with an assist-as-needed paradigm, feedback can be provided in a variety of forms to aid with the relearning process.16 To that end, we coupled an immersive virtual environment to an instrumented dual-belt treadmill to create the Integrated Virtual Environment Rehabilitation Treadmill (IVERT) system.17
The IVERT system17 measures step-by-step symmetry of a given spatiotemporal measure (eg, stance time, step length) and presents real-time feedback: (1) visually through an immersive virtual environment and (2) proprioceptively by adjusting the difference in speeds between the treadmill belts. If the chosen gait parameter becomes more asymmetric, the virtual environment appears to “turn,” much like walking around the curve on a track, and the difference between the left and right treadmill belt speeds becomes greater. As gait symmetry is restored, either within or across sessions, the turning within the VE is reduced, as is the difference in treadmill belt speeds. It is critical, however, for optic flow to match proprioceptive information from the limbs.12 If leg velocity and optic-flow velocity are perceived to be different, gait characteristics will be altered to reduce the mismatch between the competing feedbacks from visual and proprioceptive systems.12 By providing patients with a means of detecting gait asymmetry, our goal is to encourage them to self-correct movement patterns for faster, more efficient, and safer gait.
Previously, visual and proprioceptive feedback have been used separately for altering gait poststroke. Using a VE system in a seated posture, individuals poststroke have enhanced gait speed, endurance, and community participation.18 Other researchers have integrated a treadmill and VE system, although outcomes are not yet available.13 A single patient, using a combination of visual feedback, a robotic exoskeleton, and functional electrical stimulation, was able to improve gait speed and symmetry, although improvements in symmetry were not maintained.19 Other authors have used proprioceptive feedback to adaptively modify step length asymmetry while improving gait speed in a single patient.20 Given these successes, we believe that the combination of proprioceptive and visual feedback during intensive gait training will produce substantial improvements in spatiotemporal symmetry while improving gait speed.
Importantly, feedback from the IVERT system is specific to a single spatiotemporal parameter (eg, stance time, swing time, step length). Thus, it is anticipated that only the parameter for which feedback is provided will change after multiple training sessions. The purpose of this case series is to describe the outcomes associated with long-term training with combined visual and proprioceptive feedback to improve step length and stance time asymmetries in 2 individuals poststroke.
Case Description
Patient 1: History and Systems Review
The first patient was a 60-year-old man diagnosed with left hemiparesis from a stroke to his right carotid artery 18 months before evaluation. His past medical history was unremarkable, except for an irregular heartbeat. Before his stroke, he was physically active, regularly engaging in cycling, golf, and kayaking. After the stroke, he had a 6-week stay in a rehabilitation hospital, during which time he worked on ambulation, transfers, stairs, bed mobility, and management of activities of daily living (ADLs). He was discharged home to live with his supportive wife and continued approximately 6 months of additional outpatient physical therapy. Upon his first visit with us, he expressed an interest in improving his walking and learning to cycle again.
Clinical Impression and Examination
Given his desire to improve his walking, his high level of motivation, and his limited walking ability, he appeared to be a good candidate for intensive gait training.21 Because of his hemiparesis, we were concerned about the possible presence of asymmetric gait and, if present, how to eliminate it to make his gait safer and more efficient.
During his initial evaluation, he stated that he had no pain in his extremities or spine. His left arm appeared flaccid, and he maintained his left hand in a fanny pack strapped around his waist to support the weight of his arm. During his initial evaluation he scored 42/56 on the Berg Balance Scale, 11/34 on the lower-extremity portion of the Fugl-Meyer test, and 12/15 on the Rivermead Mobility Index. Determination of spatiotemporal aspects of his gait were assessed with a GaitRite mat (CIR Systems Inc, Haverton, Pennsylvania), which has been shown to be reliable22 and valid23 for use with individuals poststroke. He performed 3 passes at his comfortable gait speed and 3 passes at the fastest speed he could perform safely. The GaitRite software was used to calculate gait speed, step length, and stance time (Tab. 1). Visually, he was observed to walk slowly, using an articulated ankle-foot orthosis (AFO) on his left leg and a large-base quad cane (LBQC) in his right hand and with his left hand tucked in the fanny pack. Qualitatively, he exhibited genu recurvatum on the left during stance and stiff-knee gait during swing. His hip showed limited extension in late stance, and he rotated his pelvis to the left during stance. We hypothesized that the left pelvic rotation was a means of compensating for his lack of hip extension during stance. Nevertheless, his hip extension passive range of motion (PROM) appeared to be within functional limits when assessed in a prone position.
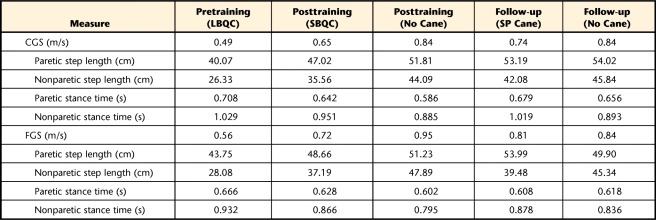
Table 1.
Patient 1: Gait Speed and Spatiotemporal Measuresa
CGS=comfortable gait speed, FGS=fast gait speed, LBQC=large-base quad cane, SBQC=small-base quad cane, SP cane=single-point cane.
Patient 2: History and Systems Review
The second patient was a 53-year-old woman diagnosed with right hemiparesis after an embolic stroke to the left middle cerebral artery 21 months before her evaluation. She stated that the clot causing her stroke resulted from endocarditis, which was brought about by supraventricular tachycardia (SVT) and a mitral valve prolapse (MVP). After 6 weeks of inpatient rehabilitation, she was discharged home to live with her daughter. Four weeks later, she was readmitted to the hospital for cardiovascular surgery to repair her mitral valve. Before her stroke, she was an avid runner and worked as an emergency department nurse, a job she was no longer able to perform due to the diminished function of her right hand. Her goals were to improve her mobility and to eventually return to running and working full time as a nurse.
Clinical Impression and Examination
As with patient 1, we were concerned about the presence of asymmetric gait due to her persistent hemiparesis, but believed that she could improve her gait with intensive gait training. During her initial evaluation, she scored 56/56 on the Berg Balance Scale, 15/15 on the Rivermead Mobility Index, and 29/34 on the lower-extremity portion of the Fugl-Meyer test. Visually, her gait appeared to be slightly slower than normal, and she appeared tentative about placing her right foot on the ground for heel strike. This delay in foot placement appeared to contribute to the stance time asymmetry observed from her GaitRite measures (Tab. 2).
Table 2.
Patient 2: Gait Speed and Spatiotemporal Measuresa
CGS=comfortable gait speed, FGS=fast gait speed.
Intervention
Because both patients had a goal of improving their mobility, we decided to perform intensive gait training,21 with a combination of treadmill-based and overground gait training.24 Because there is evidence that forcing symmetrical gait does not improve symmetry,6 we chose to perform the treadmill-based portion of the gait training on the IVERT system (Fig. 1) to provide accurate feedback regarding step-by-step gait symmetry.
Figure 1.
The Integrated Virtual Environment Rehabilitation Treadmill (IVERT) system17 couples an instrumented dual-belt treadmill with an immersive virtual environment for real-time, congruent proprioceptive and visual feedback of gait asymmetries.
Each patient received feedback about his or her primary spatiotemporal asymmetry deficit. Specifically, patient 1 received feedback regarding his step length asymmetry, whereas patient 2 received feedback regarding stance time asymmetry. Because the real-time feedback is described in detail elsewhere,17 we provide only a brief description here. The IVERT system acquired spatiotemporal gait measures (stance time or step length) from a motorized, instrumented treadmill (Bertec Corp, Columbus, Ohio). Stance time was the time (in milliseconds) that the vertical ground reaction force (Fz) exceeds 10 N, whereas step length was the anteroposterior distance between each foot's center of pressure (COP) at heel-strike.25 Feedback about the respective form of asymmetry (stance time or step length) then was provided visually by “rotating” the virtual environment, with the radius of curvature proportional to each step's spatiotemporal asymmetry. Concurrently, proprioceptive feedback was provided by operating the treadmill belts at different speeds, such that the speed differential was proportional to the current asymmetry. As gait became more symmetric, the belt speed difference decreased, and the trajectory through the VE appeared straighter. To ensure that both patients could attend to the feedback, we used the Star Cancellation Test to rule out unilateral spatial neglect.
Both patients performed a total of 18 sessions over 6 weeks. During each session, the patients performed 20 minutes of walking with the IVERT system, followed by 10 to 15 minutes of overground walking. Rest breaks were given as needed, and each session lasted approximately 60 minutes for patient 1 and 45 minutes for patient 2. Blood pressure was monitored prior to, at mid-training (eg, 10 minutes), and after IVERT walking per American College of Sports Medicine guidelines.26 Because the treadmill speeds are user controlled,17 the intensity of training was dictated by the patient's walking, but was monitored by the therapists (M.D.L. and E.W.). The IVERT system accomplishes user control of the motorized treadmill using a control algorithm that continuously estimates the patient's gait speed in real time from ground reaction force and COP measurements to produce treadmill belt speeds that match the patient's current gait speed.17 The IVERT system calculates gait speed as the product of cadence and step length at the beginning and end of each stance phase (4 times per gait cycle). Thus, the user-control algorithm provides the patient with active, real-time, unencumbered control of the treadmill's speed. Patients were encouraged to walk as quickly as possible, although limits were imposed to maintain their heart rate (HR) between 70% and 75% of estimated maximum. Additional safety limits in the IVERT system ensure that belt speeds are maintained at a safe speed.
Over the course of the 6 weeks of training, the speed limit was gradually increased to allow them to progress training speed. Patient 1's treadmill speed began at approximately 0.5 m/s during the first session and was approximately 0.9 m/s during the final session. Patient 2's average training speed began at approximately 1.2 m/s for the first session and increased to approximately 1.45 m/s by the last session. During all training sessions, both patients wore a safety harness attached overhead to a custom-designed unweighting system. No unweighting was used with either patient, however, throughout the course of training. Patient 1 wore his AFO during all training sessions, as he only had trace activity in his dorsiflexors, and we believed that he was at risk for an ankle injury if he were to train at high velocities without ankle support.
Both patients held onto the treadmill's handrail at the beginning of training. Patient 1 leaned heavily to the right during his left stance, so that he was bearing a large amount of weight through his right arm. He transitioned from holding on to the handrail to holding the therapist's hand (session 4) for arm support to not holding on to anything (session 6). The therapist's hand, as an intermediate step toward complete removal of arm support, was more compliant (less rigid) than the solid handrail and provided confidence for the patient in overcoming his apprehension regarding walking without arm support. When he was holding the therapist's hand and then when releasing his hold, the speed safety limit on the treadmill was lowered, which forced him to go slower but made him feel more comfortable and develop some confidence that he could walk without holding on. To encourage arm movement with his left arm, he purchased a GivMohr sling (GivMohr Corp, Albuquerque, New Mexico), which allowed shoulder motion and promoted more natural arm swing. Patient 2 was permitted to rest her fingers gently on the handrail to maintain her position in the middle of the treadmill, until letting go completely by session 14.
During each session, we followed the 20 minutes of IVERT walking with overground gait training. During overground training, we worked on speed-intensive training and provided verbal cues similar to those used on the treadmill. After the first 4 sessions, patient 1 did not use his cane during therapy, but continued to use it at home and in the community. He transitioned from a LBQC to a small-base quad cane (SBQC) at session 7 and to a single-point cane at session 15. Both patients performed overground walking practice both indoors and outdoors on level ground and on ramps. Both patients were provided with elastic tubing to perform lower-extremity strengthening exercises at home. Specifically, patient 1 was instructed in standing terminal knee extensions with elastic tubing, seated hamstring muscle curls with his foot on a towel, standing hip flexion and extension against gravity, and active ankle plantar flexion and dorsiflexion against the resistance of the AFO or with the AFO removed. Patient 2 was instructed in squats and ankle plantar flexion and dorsiflexion and inversion and eversion against the resistance of the elastic tubing. Unfortunately, both patients reported that they were not adherent to the home exercise program.
Both patients developed complications during training. At session 5, patient 1 complained of left posterior knee pain and was tender to palpation at the distal biceps femoris tendon. At session 7, he complained of right anterior knee pain, which was reproduced with resisted right knee extension and palpation at the patellar tendon. In both cases, the application of ice after training resolved the knee pain. Patient 2 developed an ingrown toenail on her right big toe, which was resolved after a visit to her podiatrist.
Outcomes
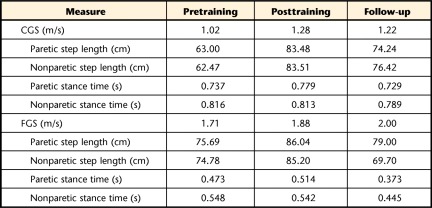
Both patients walked over the GaitRite mat and repeated clinical testing within one week after the last training session, as well as 10 weeks after training ended. Because patient 1 was walking exclusively with a LBQC at the pretraining assessment, we tested him with and without a cane at his posttest visits. All spatiotemporal measures are shown in Table 1 for patient 1 and in Table 2 for patient 2. Patient 1's comfortable gait speed during the posttest was faster without his SBQC (0.84 m/s) compared with walking with the cane (0.65 m/s). Patient 1, who trained to improve step length symmetry, improved his step length symmetry ratio from pretest (1.52) to posttest (1.32) while using a cane (Fig. 2). Without his cane, his symmetry ratio improved even further (1.18). These changes were maintained at 10 weeks after training. Interestingly, his stance time asymmetry, about which he did not receive feedback, did not change from pretraining to posttraining.
Figure 2.
Symmetry ratios for step length (A and C) and stance time (B and D) for patient 1 (A and B) and patient 2 (C and D). Symmetry ratios were calculated as paretic/nonparetic and inverted, if necessary, to be >1.0.1,29 Patient 1 trained to improve his step length symmetry ratio. Symmetry ratios are provided for him at pretraining, posttraining, and 10-week follow-up with (black) and without (white) his cane. Patient 2 trained to improve her stance time symmetry ratio. She walked exclusively without a cane at pretraining, posttraining, and at 10-week follow-up. For both patients, the normal ratio is shaded in gray (step length: 1.00–1.08; stance time: 1.00–1.05).1
Patient 2 also improved her comfortable gait speed from pretraining (1.02 m/s) to posttraining (1.28 m/s). She demonstrated a small improvement in stance time symmetry ratio from pretraining (1.11) to posttraining (1.04), but regressed somewhat by her follow-up (Fig. 2). Her step lengths were symmetrical at pretraining and remained symmetrical at posttraining and follow-up.
Clinical testing following training showed only small improvements for patient 1 (lower-extremity portion of the Fugl-Meyer test: 17/34; Berg Balance Scale: 43/56; Rivermead Mobility Index: 13/15). Patient 2 exhibited a small improvement in her lower-extremity Fugl-Meyer test score (31/34), and the Berg Balance Scale remained at a maximum score (56/56).
After training, patient 1 reported that he did not use his cane routinely at home, although he continued to use it in the community. Importantly, he reported an increase in community activity, with his wife noting that he was willing and able to go grocery shopping with her. With respect to his goal of returning to cycling, he was able to independently mount and dismount a woman's bike mounted to a stationary trainer, although at the conclusion of training he reported that he had not tried cycling. Patient 2 ran through the parking lot successfully, under therapist supervision, during one of our later sessions, but reported at follow-up that she did not feel comfortable running on her own.
Discussion
Our patients were able to use combined visual and proprioceptive feedback of specific spatiotemporal symmetry measures to modify their walking patterns. Both patients increased gait speed and showed greater changes in spatiotemporal symmetry than have been reported generally in the literature.6–8 Recently, however, investigators have sought novel approaches to improve gait speed, while attempting to restore symmetric gait patterns.17,20,27,28 Reisman and colleagues, for example, were able to demonstrate changes in step length symmetry after 4 weeks of split belt walking.20 After 10 sessions of unilateral step training, Kahn and Hornby were unable to demonstrate improvements in step length symmetry at 1 week after training, at a comfortable gait speed, but did show improvements at 2 weeks after training.27 These approaches provide optimism that rehabilitation will be capable of demonstrating robust changes to locomotor patterns after chronic stroke.
Importantly, the changes exhibited by our patients can be considered meaningful. Recent estimates of minimal detectable change (MDC) for step length (0.15) and stance time (0.09) asymmetry ratios have been reported.29 Patient 1 exceeded the MDC for step length asymmetry ratio, both with and without his cane at posttest and 10-week follow-up. Patient 2 did not exceed the MDC for stance time asymmetry ratio. Nevertheless, the magnitude of change was sufficient to reduce her symmetry ratio below the established threshold for a normal stance time symmetry ratio (1.05) at the posttest.1 Given these changes, the alterations in symmetry ratio are meaningful scientifically, although we are unaware of evidence to support the clinical meaningfulness of these changes. In addition, although the symmetry ratios became more normal, we observed that spatiotemporal measures (step length for patient 1 and stance time for patient 2) of the individual limbs also became more normal.30
We can speculate that the changes in spatiotemporal symmetry are a result of the ability to make and correct errors during training. Walking on a treadmill compared with overground appears to reduce spatiotemporal asymmetry if handrails are used,31 while increasing asymmetry if handrail use is not allowed.32 Unfortunately, training on a conventional treadmill with or without use of a handrail does not appear to consistently alter spatiotemporal asymmetry.6–10 In contrast, novel methods that enhance asymmetry (eg, movement error) are suggested to be beneficial for altering locomotor patterns.20 We believe that the ability to train with movement errors for self-correction contributed to our patients' ability to improve their gait symmetry. Further work, however, is needed to confirm this hypothesis.
Both patients also demonstrated improvements in their comfortable gait speed. The MDC for gait speed in individuals with chronic stroke has been estimated to be 0.20 m/s.29,33 Both patients exceeded this value, with patient 1 exhibiting a change of 0.35 m/s and patient 2 exhibiting a change of 0.26 m/s. Such robust changes in gait speed exceed changes reported typically in the literature.5 It is likely that the progressive nature of the training, coupled with the optic flow from the VE, helped generate substantial improvements in gait speed. A potential limitation is that both patients were prescribed therapeutic exercises to be performed at home, which may confound our interpretation of the effect of our gait training paradigm. Given that adherence to these exercises was so low, however, we feel that the exercises did not substantially contribute to the alterations in gait speed or symmetry in either patient.
At posttest and follow-up, patient 1 walked faster and more symmetrically without the use of his cane. This outcome is in contrast to the notion that use of a cane will improve symmetry.34 Because our goal was to eliminate the use of his cane, patient 1 performed his overground gait practice without his cane. Although the use of a cane in asymmetric individuals who do not typically use canes can improve symmetry,35 it is unknown how individuals who use a cane typically will fare when their cane is taken away. In this single patient, however, his gait improved.
The use of feedback during gait training is certainly not novel.16 In previous studies, visual,18,19,36 auditory,36,37 or proprioceptive20,28 feedback during locomotor training has been used with individuals poststroke. The technique described here, however, combines visual and proprioceptive feedback in a congruent and intuitive manner. In addition, we believe that the use of the self-paced treadmill was beneficial, as it required the patients to remain motivated to walk at a high intensity. That the belts were controlled independently by each limb meant that symmetric gait was not imposed, but rather that continuous proprioceptive feedback was provided regarding the current magnitude of asymmetry. We are encouraged by the outcomes for our patients and believe that the combination of simultaneous visual and proprioceptive feedback of spatiotemporal asymmetry during intensive gait training may be effective at improving gait after chronic stroke. Effectiveness, however, can only be determined through controlled studies.
Footnotes
Dr Lewek, Mr Feasel, Dr Brooks, and Ms Whitton provided concept/idea/project design. Dr Lewek provided writing, data analysis, fund procurement, and patients. Dr Lewek, Mr Feasel, and Ms Wentz provided data collection. Dr Lewek, Dr Brooks, and Ms Whitton provided project management and facilities/equipment. Dr Lewek, Ms Wentz, Dr Brooks, and Ms Whitton provided consultation (including review of manuscript before submission). The authors recognize Laura Kassler, MS, and Zhen Shao for their work on the virtual environment.
Data from this case series were presented at the Combined Sections Meeting of the American Physical Therapy Association; February 8–11, 2012; Chicago, Illinois.
This work was supported by awards from the American Heart Association (09BGIA2210015 to Dr Lewek) and the National Institutes of Health (5P41EB002025 to Rich Superfine, PhD).
References
- 1. Patterson KK, Gage WH, Brooks D, et al. Evaluation of gait symmetry after stroke: a comparison of current methods and recommendations for standardization. Gait Posture. 2010;31:241–246 [DOI] [PubMed] [Google Scholar]
- 2. Titianova EB, Peurala SH, Pitkanen K, Tarkka IM. Gait reveals bilateral adaptation of motor control in patients with chronic unilateral stroke. Aging Clin Exp Res. 2008;20:131–138 [DOI] [PubMed] [Google Scholar]
- 3. Norvell DC, Czerniecki JM, Reiber GE, et al. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch Phys Med Rehabil. 2005;86:487–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jorgensen L, Crabtree NJ, Reeve J, Jacobsen BK. Ambulatory level and asymmetrical weight bearing after stroke affects bone loss in the upper and lower part of the femoral neck differently: bone adaptation after decreased mechanical loading. Bone. 2000;27:701–707 [DOI] [PubMed] [Google Scholar]
- 5. Duncan PW, Sullivan KJ, Behrman AL, et al. Body-weight-supported treadmill rehabilitation after stroke. N Engl J Med. 2011;364:2026–2036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hornby TG, Campbell DD, Kahn JH, et al. Enhanced gait-related improvements after therapist- versus robotic-assisted locomotor training in subjects with chronic stroke: a randomized controlled study. Stroke. 2008;39:1786–1792 [DOI] [PubMed] [Google Scholar]
- 7. Patterson SL, Rodgers MM, Macko RF, Forrester LW. Effect of treadmill exercise training on spatial and temporal gait parameters in subjects with chronic stroke: a preliminary report. J Rehabil Res Dev. 2008;45:221–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Silver KH, Macko RF, Forrester LW, et al. Effects of aerobic treadmill training on gait velocity, cadence, and gait symmetry in chronic hemiparetic stroke: a preliminary report. Neurorehabil Neural Repair. 2000;14:65–71 [DOI] [PubMed] [Google Scholar]
- 9. Plummer P, Behrman AL, Duncan PW, et al. Effects of stroke severity and training duration on locomotor recovery after stroke: a pilot study. Neurorehabil Neural Repair. 2007;21:137–151 [DOI] [PubMed] [Google Scholar]
- 10. Westlake KP, Patten C. Pilot study of Lokomat versus manual-assisted treadmill training for locomotor recovery post-stroke. J Neuroeng Rehabil. 2009;6:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lamontagne A, Fung J, McFadyen BJ, Faubert J. Modulation of walking speed by changing optic flow in persons with stroke. J Neuroeng Rehabil. 2007;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Prokop T, Schubert M, Berger W. Visual influence on human locomotion. Modulation to changes in optic flow. Exp Brain Res. 1997;114:63–70 [DOI] [PubMed] [Google Scholar]
- 13. Fung J, Richards CL, Malouin F, et al. A treadmill and motion coupled virtual reality system for gait training post-stroke. Cyberpsychol Behav. 2006;9:157–162 [DOI] [PubMed] [Google Scholar]
- 14. Cai LL, Fong AJ, Otoshi CK, et al. Implications of assist-as-needed robotic step training after a complete spinal cord injury on intrinsic strategies of motor learning. J Neurosci. 2006;26:10564–10568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lewek MD, Cruz TH, Moore JL, et al. Allowing intralimb kinematic variability during locomotor training poststroke improves kinematic consistency: a subgroup analysis from a randomized clinical trial. Phys Ther. 2009;89:829–839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tate JJ, Milner CE. Real-time kinematic, temporospatial, and kinetic biofeedback during gait retraining in patients: a systematic review. Phys Ther. 2010;90:1123–1134 [DOI] [PubMed] [Google Scholar]
- 17. Feasel J, Whitton MC, Kassler L, et al. The integrated virtual environment rehabilitation treadmill system. IEEE Trans Neural Syst Rehabil Eng. 2011;19:290–297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mirelman A, Bonato P, Deutsch JE. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke. 2009;40:169–174 [DOI] [PubMed] [Google Scholar]
- 19. Krishnamoorthy V, Hsu WL, Kesar TM, et al. Gait training after stroke: a pilot study combining a gravity-balanced orthosis, functional electrical stimulation, and visual feedback. J Neurol Phys Ther. 2008;32:192–202 [DOI] [PubMed] [Google Scholar]
- 20. Reisman DS, McLean H, Bastian AJ. Split-belt treadmill training poststroke: a case study. J Neurol Phys Ther. 2010;34:202–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moore JL, Roth EJ, Killian C, Hornby TG. Locomotor training improves daily stepping activity and gait efficiency in individuals poststroke who have reached a “plateau” in recovery. Stroke. 2010;41:129–135 [DOI] [PubMed] [Google Scholar]
- 22. Ng SS, Hui-Chan CW. The timed up & go test: its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch Phys Med Rehabil. 2005;86:1641–1647 [DOI] [PubMed] [Google Scholar]
- 23. Stokic DS, Horn TS, Ramshur JM, Chow JW. Agreement between temporospatial gait parameters of an electronic walkway and a motion capture system in healthy and chronic stroke populations. Am J Phys Med Rehabil. 2009;88:437–444 [DOI] [PubMed] [Google Scholar]
- 24. Duncan PW, Sullivan KJ, Behrman AL, et al. Protocol for the Locomotor Experience Applied Post-stroke (LEAPS) trial: a randomized controlled trial. BMC Neurol. 2007;7:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Noble JW, Prentice SD. Adaptation to unilateral change in lower limb mechanical properties during human walking. Exp Brain Res. 2006;169:482–495 [DOI] [PubMed] [Google Scholar]
- 26. American College of Sports Medicine ACSM's Guidelines for Exercise Testing and Prescription. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005 [Google Scholar]
- 27. Kahn JH, Hornby TG. Rapid and long-term adaptations in gait symmetry following unilateral step training in people with hemiparesis. Phys Ther. 2009;89:474–483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lam T, Luttmann K, Houldin A, Chan C. Treadmill-based locomotor training with leg weights to enhance functional ambulation in people with chronic stroke: a pilot study. J Neurol Phys Ther. 2009;33:129–135 [DOI] [PubMed] [Google Scholar]
- 29. Lewek MD, Randall EP. Reliability of spatiotemporal asymmetry during overground walking for individuals following chronic stroke. J Neurol Phys Ther. 2011;35:116–121 [DOI] [PubMed] [Google Scholar]
- 30. Lewek MD. The influence of body weight support on ankle mechanics during treadmill walking. J Biomech. 2011;44:128–133 [DOI] [PubMed] [Google Scholar]
- 31. Harris-Love ML, Forrester LW, Macko RF, et al. Hemiparetic gait parameters in overground versus treadmill walking. Neurorehabil Neural Repair. 2001;15:105–112 [DOI] [PubMed] [Google Scholar]
- 32. Kautz SA, Bowden MG, Clark DJ, Neptune RR. Comparison of motor control deficits during treadmill and overground walking poststroke. Neurorehabil Neural Repair. 2011;25:756–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Flansbjer UB, Holmback AM, Downham D, et al. Reliability of gait performance tests in men and women with hemiparesis after stroke. J Rehabil Med. 2005;37:75–82 [DOI] [PubMed] [Google Scholar]
- 34. Patterson KK. Clinician's commentary. Physiother Can. 2009;61:161–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Beauchamp MK, Skrela M, Southmayd D, et al. Immediate effects of cane use on gait symmetry in individuals with subacute stroke. Physiother Can. 2009;61:154–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Montoya R, Dupui P, Pages B, Bessou P. Step-length biofeedback device for walk rehabilitation. Med Biol Eng Comput. 1994;32:416–420 [DOI] [PubMed] [Google Scholar]
- 37. Hogue RE, McCandless S. Genu recurvatum: auditory biofeedback treatment for adult patients with stroke or head injuries. Arch Phys Med Rehabil. 1983;64:368–370 [PubMed] [Google Scholar]