Summary
In many cases, the prognosis for acute cervical carotid artery occlusion is poor. However, a standard treatment for the acute stage is not yet established. We report here the results of eight consecutive patients (mean age 71.5 years old) in which revascularization mainly by suction thrombectomy was performed under proximal protection during the acute phase. The occlusion sites were the intracranial internal carotid artery in five patients, tandem lesions of the internal carotid origin and intracranial vessel in two patients, and the common carotid artery in one patient. In addition, the subjects who received the treatment had an extent of infarction in MRI/DWI that was 1/3 or less of the internal carotid artery territory. The mean time from the onset to treatment commencement was 7.25 hours (2-28 hours). For the endovascular treatment, a guiding catheter with a balloon was used for proximal protection of the carotid artery. Revascularization was performed mainly by suction thrombectomy, and if a stenosed lesion was observed, PTA/stenting was added. Local fibrinolysis was not performed in combination with the above procedure. The treatment results were complete recanalization in three patients and partial recanalization in three patients. However, recanalization was not achieved in two patients. No hyperfusion syndrome or hemorrhagic infarction was observed postoperatively. All four patients in whom thrombi were successfully aspirated had occlusions proximal to the ophthalmic artery branch. In three of these four patients, complete recanalization was achieved. The revascularization procedure using suction thrombectomy under proximal protection was considered effective against the acute cervical carotid occlusions, in particular, those proximal to the ophthalmic artery branch.
Key words: carotid artery, revascularization, suction thrombectomy
Introduction
In general, it is difficult for revascularization procedures to be indicated for acute carotid occlusions. The results of revascularization procedures using conventional thrombolytic agents are poor, and a high rate of hemorrhagic complications has been a problem2,3.
In recent years, reports on revascularization procedures by mechanical thrombectomy have been seen occasionally for acute internal carotid occlusions. The results of such treatment have been good relative to those of thrombolytic agent administration4-9. We report a revascularization procedure mainly by suction thrombectomy performed in eight consecutive patients under proximal protection using a catheter with a balloon.
Methods
The subjects were eight consecutive patients in whom revascularization was performed on acute cervical carotid occlusions at our institution from April 2005 to March 2006. We studied the usefulness of such a treatment on these patients. Treatment was indicated and performed in patients in whom the time from the onset to treatment commencement was 48 hours or less, and whose age was 80 years old or less, and in whom the occlusion was observed in the common or internal carotid artery in the MRA or cerebral angiography, the pretreatment National Institute of Health Stroke Scale (NIHSS) score was between four and 30 points, and the extent of the infarction of the internal carotid artery territory was 1/3 or less in the diffusion-weighted MRI (DWI).
For the endovascular treatment, systemic heparinization was performed under local anesthesia, and an approach via the femoral artery was used. A 9 Fr introducer sheath was placed in the femoral artery. A 9 Fr guiding catheter with a balloon (9 Fr Patlieve: Clinical Supply, Japan) was used as the coaxial system with a 6 Fr inner catheter (CX-JB2) to guide it proximal to the carotid occlusion site. Then the balloon was inflated, and the proximal protection was performed. Suction thrombectomy was performed under the proximal protection. Suction thrombectomy was performed using 6 FrCX-JB2 or a guidance catheter depending on the occlusion site. If residual stenosed lesions were observed after suction thrombectomy, percutaneous transluminal angioplasty (PTA)/stenting was added. If recanalization was not achieved by suction thrombectomy, PTA of the occluded region was performed. Fibrinolytic treatment was not performed concomitantly. Posttreatment, if the occlusion was believed to be from atherothrombosis, argatroban 60 mg/day was administered continuously for 48 hours. Bayaspirin 100 mg or ticlopidine 200 mg, or a combination of the two, was also given orally. If the occlusion was believed to be a cardiogenic cerebral embolism, heparin was continuously administered and then switched to oral warfarin.
Results
Table 1 shows patient backgrounds and treatment results. The mean age of the eight treated patients was 71.5 years (57-79 years), and six were males and two were females. The mean pretreatment NIHSS score was 15.1 points (5-24 points), and the mean time between the onset and treatment commencement was 7.25 hours (2-28 hours). The mechanisms of onset were atherothrombosis in two patients and cardiogenic cerebral embolism in six patients. The occlusion sites were the intracranial internal carotid artery in five patients, tandem lesions of the internal carotid origin and intracranial vessel in two patients, and the common carotid artery in one patient. Thrombus aspiration was successful in four out of eight patients, and complete recanalization was observed in three of these four patients. The occlusion sites were all proximal to the ophthalmic artery branch: C4, C5, common carotid, and internal carotid bifurcation. Residual stenoses were observed after complete recanalization in two patients, one of whom received an additional treatment of PTA only and the other received an additional treatment of PTA/stenting for the stenosed area. At the time of hospital discharge, the modified Rankin scale (mRS) of three patients with complete recanalization was mRS 2 in two patients and mRS 3 in one patient, indicating relatively good results. One other patient had an occlusion of the ICA top. Recanalization could not be achieved, and the patient was mRS 5, indicating poor prognosis. In all four of eight patients in whom suction thrombectomy was not successful, the occlusion sites were distal to the ophthalmic artery branch. PTA was performed for these patients, but complete recanalization was not achieved in any of these patients. Partial recanalization was achieved in three patients, and recanalization was not achieved at all in one patient. At the time of hospital discharge, two of the three patients with partial recanalization had mRS 3. However, one patient had died from a cerebral hernia with extensive cerebral infarction. In addition, another patient, in whom complete recanalization was not achieved, died postoperatively from extensive infarction. A hemorrhagic infarction and hyperfusion syndrome were not observed in either of these patients.
Table 1.
Patients' profiles.
| Case | Age/Sex | NIHSS on admission |
Time from onset to procedure (hr) |
Stroke subtype |
Site of lesion |
Suction Thrombectomy |
Recanali- zation |
Outcom (mRS) |
|---|---|---|---|---|---|---|---|---|
| 1 | 77/M | 5 | 28 | ATBI | ICA(C4 ) | O | CR | 2 |
| 2 | 79/M | 15 | 7 | CE | ICA(C5 ) | O | CR | 3 |
| 3 | 77/M | 17 | 2 | CE | CCA | O | CR | 2 |
| 4 | 70/F | 24 | 4 | CE | ICA orifice+top | O | No | 5 |
| 5 | 63/M | 6 | 9 | CE | ICA top | x | PR | 3 |
| 6 | 79/F | 14 | 3 | CE | ICA orifice+M1 | x | PR | 3 |
| 7 | 57/M | 19 | 3 | ATBI | ICA(C2) | x | PR | 6 |
| 8 | 70/M | 21 | 2 | CE | ICA top | x | No | 6 |
|
M: Male, F: Female, NIHSS: National Institutes of Health Stroke Scale, ATBI: Atherothrombotic brain infarction, CE: Cardiac Embolization, ICA: Internal carotid artery, CCA: Common carotid artery, CR: Complete recanalization, PR: partial recanalization, No: No recanalization, C2: Cisternal segment, C4: Cavenous segment, M1: Middle cerebral artey, Sphenoidal segment, S: modified Rankin scale | ||||||||
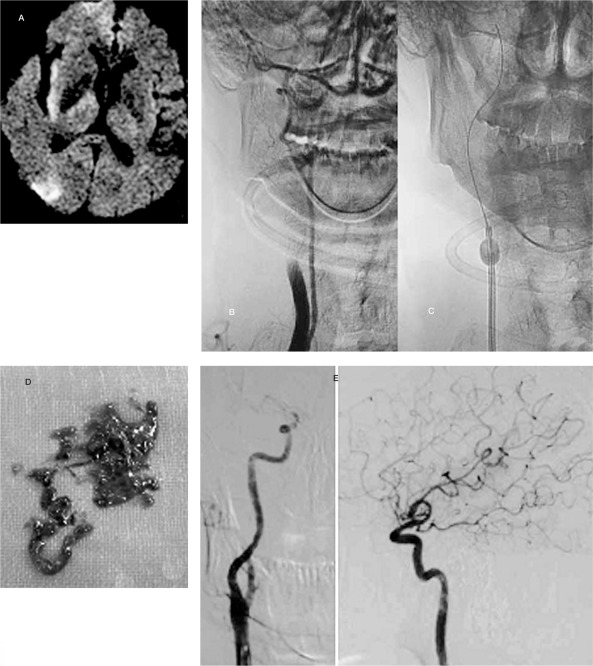
Case Report (Case 3) Figure 1
A 77-year-old male had a history of HCM and Af, and was taking warfarin orally. The patient had an onset of left hemiplegia and his NIHSS was 17 points at the time of admission. In the MRI/MRA, a right carotid occlusion and a diffuse cerebral infarction in a section of the right internal carotid artery territory were observed (A). The revascularization procedure was started 2 hours from the onset. A right common carotid occlusion was observed by cerebral angiography (B). Directly underneath the occluded area, suction thrombectomy was performed under proximal protection by using a 9 Fr Patlieve catheter (C), and complete recanalization was achieved (E). Improvement in symptoms was observed postoperatively. At the time of hospital discharge, the patient was mRS 2.
Figure 1.
Case 3: A) MRI/DWI: Findings of diffuse infarction were obtained in the right ICA area. B) Pretreatment Angiography: Occlusion in rt. CCAG ~CCA immediately before the ICA bifurcation. C) Suction thrombectomy was performed under proximal protection using a 9 Fr Patlieve catheter directly underneath the occluded region. D) Recovered thrombus. E) Posttreatment Angiography: Complete recanalization was achieved.
Discussion
For eight patients with acute internal carotid occlusions, the revascularization procedure was performed centering on suction thrombectomy using a guidance catheter with a balloon. Complete or partial recanalization was achieved in six patients. In four of these patients, functional prognoses were relatively good at the time of hospital discharge. Case reports of revascularization procedures by suction thrombectomy have been seen occasionally4,5. However, our report is the first to suggest that suction thrombectomy is an effective treatment for proximal carotid occlusions.
The clinical course of an acute internal carotid occlusion is known for poor prognosis 1. In addition, the treatment results are poor for internal carotid occlusions by transvenous or transarterial administration of a thrombolytic agent2,3. According to the International Management of Stroke Study (IMS), when acute internal carotid occlusions were treated by only intravenous tPA administration, recanalization was observed only in 10% of the occluded arteries. When a combination of transvenous and local selective intraarterial administration was used, complications of hemorrhage became a problem. The hemorrhage rate was high at 71%3. In the MERCI trial (2005, Stroke) in which a recanalization procedure was performed using a clot retriever, tPA intraarterial administration was performed in 51 patients after the usage of the retriever. Complications of hemorrhage tended to occur at a higher rate for the group with concomitant tPA usage compared to the group in which a retriever alone was used 9. In our series of patients, we performed PTA/stenting after the aspiration. However, thrombolytic agent administration was not combined with the procedure. As a result, we did not observe hemorrhagic complications. We believe hemorrhage can be avoided by avoiding the use of a thrombolytic agent for recanalization of an acute carotid occlusion.
In recent years, relatively good results for mechanical thrombectomy have been reported occasionally as an acute-stage revascularization method for internal carotid occlusions 4-9. In the MERCI trial, the recanalization rate was 53% in 47 patients with internal artery occlusions. The mortality rate was 51% and symptomatic hemorrhage was seen in 15% of the patients8. In the present report, complete recanalization was observed in 37.5% of the occluded arteries. The percentage was 75.5% when partial recanalization was included. The mortality rate was 25%. We considered our results more favorable relative to those from the IMS and MERCI studies.
In our study, the occlusion sites for four patients in whom the thrombi were aspirated were all proximal to the ophthalmic artery branch, and we were able to guide the suction catheter directly underneath the occluded region. Previous literature described similar resuits for recanalization procedures by suction thrombectomy 4,5. When suction thrombectomy was performed far away from the occluded region because the suction catheter could not be guided immediately underneath the site· none of the thrombi was aspirated.
For internal carotid occlusions distal to the ophthalmic artery branch· it was difficult to achieve recanalization using a combined treatment of suction thrombectomy and PTA. For such occlusions· there have been reports on mechanical thrombectomy using a clot retriever or microsnare6-9, and future progress is expected.
Conclusions
For an acute carotid occlusion, a revascularization procedure was performed in eight consecutive patients. This procedure was performed by mainly suction thrombectomy under proximal protection using a guidance catheter with a balloon. The usefulness of such a treatment was examined. The recanalization rate was 75%, hemorrhage rate was 0%, and the treatment was considered feasible. In particular, the treatment was considered effective for occlusions proximal to the ophthalmic artery branch.
References
- 1.Meyer FB, Sundt TM, Jr, et al. Emergency carotid endarterectomy for patients with acute carotid occlusion and profound neurological deficit. Ann Surg. 1986;203(1):8289. doi: 10.1097/00000658-198601000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The IMS. Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke. Stroke. 2004;35:904–911. doi: 10.1161/01.STR.0000121641.77121.98. [DOI] [PubMed] [Google Scholar]
- 3.The IMS. Hemorrhage in the Interventional Management of Stroke Study. Stroke. 2006;37(3):847–851. doi: 10.1161/01.STR.0000202586.69525.ae. [DOI] [PubMed] [Google Scholar]
- 4.Helmi L, Wayne M, et al. Intraarterial suction thrombectomy in acute stroke. Am J Neuroradiol. 2002;23:783–786. [PMC free article] [PubMed] [Google Scholar]
- 5.Xu GF, Suh DC, et al. Aspiration thrombectomy of acute complete carotid bulb occlusion. J Vasc Interv Radiol. 2005;16(4):539–542. doi: 10.1097/01.RVI.0000150925.36365.8E. [DOI] [PubMed] [Google Scholar]
- 6.Hilario M, Gregg H, et al. Mechanical thrombectomy of the internal carotid artery and middle cerebral arteries for acute stroke by using the retriever device. Am J Neuroradiol. 2004;25(10):1812–1815. [PMC free article] [PubMed] [Google Scholar]
- 7.Gunnar W. Transarterial embolectomy in acute stroke. Am J Neuroradiol. 2003;24:892–894. [PMC free article] [PubMed] [Google Scholar]
- 8.Imai K, Mori T, et al. Successful thrombectomy in acute terminal internal carotid occlusion using a basket type microsnare in conjunction with temporary proximal occlusion: a case report. Am J Neuroradiol. 2005;26:1395–1398. [PMC free article] [PubMed] [Google Scholar]
- 9.Smith WS, et al. Safety and Efficacy of Mechanical Embolectomy in Acute Ischemic Stroke. Result of the MERCI Trial. Stroke. 2005;36:1432–1440. doi: 10.1161/01.STR.0000171066.25248.1d. [DOI] [PubMed] [Google Scholar]