Abstract
Background
Health care practitioners in jurisdictions around the world are encouraged to work in groups. The extent to which they actually do so, however, is not often measured. The purpose of this paper is to demonstrate the potential for administrative data to measure how practitioners are interconnected through their care of patients. Our example examined the interconnected care provided by family physicians.
Methods
We defined a physician as being “interconnected” with another physician if these 2 physicians provided at least 1% of their clinic visits over a 2-year period to the same patients. We examined a cohort of 2945 primary care physicians in 309 Family Health Networks and Family Health Groups in Ontario, Canada, in 2005/06. In total, 9.3 million physician visits for 2.1 million patients were studied. For each group practice we calculated the number of interconnected physicians.
Results
Physicians had, on average, 2.2 interconnected physician partners (median = 1; 25th and 75th percentile: 0, 3). Physicians saw mainly their own listed patients, and 7.9% (median = 5.9%; 25th and 75th percentile: 2.4%, 11.6%) of their visits were provided to patients of their interconnected partners. The number of interconnected physicians was higher in group practices that had more physicians, but levelled to 2.5 interconnected physicians in practices with 8 or 9 physicians.
Interpretation
Routinely collected administrative data can be used to examine how health care is organized and delivered in groups or networks of practitioners. This study’s concept of interconnected care provided by primary care physicians within groups could be expanded to include other practitioners and, indeed, entire health care systems using more complex network analysis methods.
“Collaborative practice” and “shared care” are among the terms that describe care provided by practitioners working together.1,2 At the centre of most collaborative relationships is the care provided to individual patients. The extent to which providers actually work together to provide care to the same patients—what we define as “interconnected care”—is not often measured or examined. This study sought to examine whether large administrative databases can be used to examine interconnected care.
Studies that examine how health care professionals work together have shown improved patient outcomes, safety and health professional satisfaction.3-6 Intervention studies to improve collaborative practice have shown similar findings.7,8 To date, collaborative practice has been shown to improve outcomes in a variety of specific areas, including geriatrics, emergency department care, adult immunization, hip fracture and neonatal ICU care.
We describe the extent of interconnected care among primary care physicians in Ontario group practices. We recognize that collaboration in health care extends beyond the care provided by physicians; indeed, the recent emphasis on interprofessional care has at its core the concept of two or more health professions working together. Our intention was to demonstrate how administrative data could be used to identify the degree of linkage among primary care physicians, which in turn could serve as a resource for other studies of interprofessional care.
Interconnected care could also provide a building block for the examination of health care delivery from a network perspective. “Network medicine” is a new term that describes health as complex interconnected systems. Advocates of this approach argue that networks will eventually “affect all aspects of medical research and practice,” in large part because networks appear ubiquitous and new perspectives on health emerge once seemingly separate information is mapped together and examined.9 Currently, network medicine has focused on describing disease within 3 linked, interconnected layers: cellular processes; disease development and interaction; and social interaction. Surprisingly, a missing perspective of network medicine is health care delivery. At first glance, health care seems to be well suited to a network approach, by which services are provided through an array of providers and facilities within what is often described as a “complex system.” Having a way to connect the various parts of a system is the most important prerequisite for network analysis, and interconnected patient care is a logical and meaningful way to envision connections in network analysis of health care delivery.
This study, therefore, had three objectives: (1) To demonstrate the feasibility of using administrative data to describe the amount of interconnected care that takes place between primary care physicians. (2) To count the number of “interconnected” physicians in each group practice. (“Interconnection” was defined as 2 physicians in a group who separately provided a defined proportion of their physician–patient visits to the same individual patients.) (3) To examine whether the number of interconnected partners varied according to the number of physicians in the group practice.
Method
Physicians and their practices
The study base included all primary care physicians in Ontario who practised within a Family Health Group (FHG) or Family Health Network (FHN) on 1 September 2005. FHGs and FHNs are groups of physicians who enter into a contractual arrangement with the Ontario Ministry of Health and Long-Term Care to work in teams, develop interdisciplinary practices, and implement a common approach to after-hours and weekend care.10,11 At the time of the study, most FHGs and FHNs represented long-standing group practices that had entered into new formal agreements to become FHGs and FHNs with the Ministry of Health and Long-term Care. FHGs and FHNs eligible to be part of the study cohort had at least 3 but fewer than 49 physicians registered in the group for the period 1 September 2005 to 31 August 2006. We excluded physicians who did not have active patient rosters or who provided fewer than 100 visits to listed patients per year.
Patients and their physician visits
In FHG and FHN groups, patients are listed to individual physicians by means of a signed consent form. The study included all patients who were listed continuously through the study period. All clinic visits to group physicians were included.
Data sources and definitions
Data for this analysis were accessed through a comprehensive agreement with the Ontario Ministry of Health and Long-Term Care. Physicians and their group practices were identified using the Corporate Provider Database, current to March 2007. Physician demographic information was accessed using the Institute for Clinical Evaluative Sciences Physician Database. Patient lists for FHGs and FHNs were identified using Client Agency Program Enrolment tables from 1 Sept. 2005 to 31 Aug. 2006. Ontario’s Registered Persons Database, the province’s health care registry of all persons covered by the Ontario Health Insurance Program (OHIP), was accessed for patient age, sex and place of residence. Physician billing claims to OHIP were extracted to identify services provided in offices, as opposed to other settings such as home and long-term-care facilities.
Prior to data analysis, all patient and provider identifiers were removed and replaced with unique encrypted numbers. The study was approved by the Research Ethics Board of Sunnybrook Health Sciences Centre in Toronto, Ontario.
Analysis
The analysis was performed in 3 steps. First, we determined the number of unique patient–physician visits that took place during the study period. Second, we calculated the number of visits that occurred between a given patient and all of the physicians in the FHG or FHN of which the patient’s family physician was a member. Finally, we looked at how physicians within a FHG or FHN were connected with respect to seeing each other’s patients.
In the first step of our analysis we aggregated our data from billing data into unique physician–patient visits by keeping only one billing per patient per physician per day. This defined our measure of analysis, which was a physician–patient visit.
Step 2 of our analysis summed the total number of patient visits to each physician in the FHG or FHN during the study period. For example, Step 1 might identify a patient who had 10 physician–patient visits to a unique group practice. Step 2 would count the number of visits that patient had with each physician in the practice during the study period. Typically, a patient’s regular primary care physician would provide most of the visits (e.g., 9 of 10 visits were with physician A), and the remaining visits would be provided by others physicians within the group practice (say, 1 of the 10 visits was with physician B).
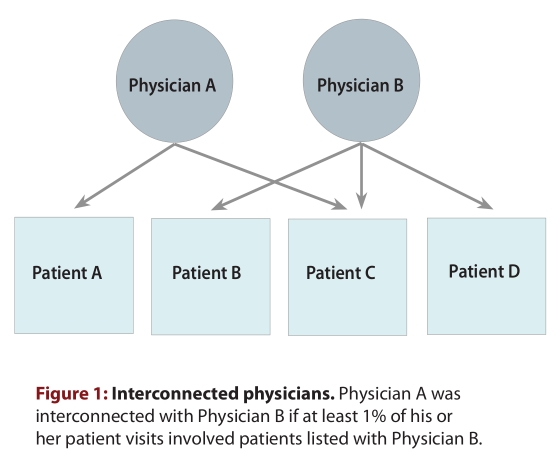
The third step in our analysis counted the number of “interconnected physicians” in each group practice by looking at which physicians in the same group practice had provided a certain proportion of their colleague’s patient’s visits. The threshold for interconnection between 2 physicians was predefined as the provision, on average, of at least 1% of visits to the same patients. That is, in Figure 1, Physicians A and B are interconnected if the care provided to Patient C and other similarly “shared” patients represents at least 1% of the total visits provided by each of Physician A and B. In sensitivity testing, we varied the threshold for interconnectedness from 0.5 to 2.0%.
Figure 1.
Interconnected physicians
Additionally, we assessed the relationship between group size and the number of interconnected physicians within the group by categorizing the FHG and FHN groups according to the number of physicians in each group: 2 or 3, 4 or 5, 6 or 7, 8 or 9, 10 to 14, 15 to 19 and 20 to 48. We calculated the average number of interconnected physicians (using the steps described above) for each group size category to see how practice size influenced the degree of interconnectedness between physicians.
Results
There were 260 FHGs and 49 FHNs with 3 to 48 physicians registered in the group from 1 Sept. 2005 to 31 Aug. 2006. This amounted to a total of 4064 physicians. We excluded 1119 physicians (27.5%) who did not have active patient rosters or provided fewer than 100 visits to listed patients per year. The remaining 2945 physicians’ practices were reviewed, representing approximately 30% of all family physicians in Ontario.12
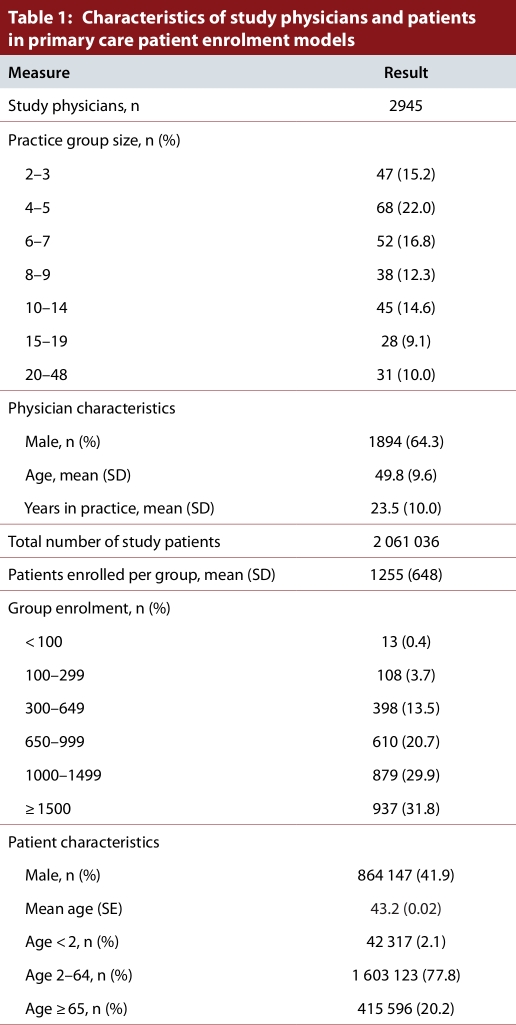
Table 1 summarizes the characteristics of the 2945 physicians and 2 061 036 patients included in the study. There was a considerable range in the number of physicians in the group practices (median = 4; 25th and 75th percentile: 4, 11). Physicians listed an average of 700 patients (median = 646 patients, 25th and 75th percentile: 363, 963). There were 9.3 million unique patient–physician visits throughout the 2-year study period.
Table 1.
Characteristics of study physicians and patients in primary care patient enrolment models
Using threshold of 1% of their visits being with one another’s listed patients, physicians had 2.2 interconnected partners (median = 1; 25th and 75th percentile: 0, 3; see Fig. 2). As expected, decreasing the threshold of common patients increased the number of interconnected physicians, but even using a low threshold of 0.5% for the proportion of visits involving the same patients, the number of interconnected physicians within a group increased to just 3.4 (median = 2; 25th and 75th percentile: 1, 5). Physicians saw mainly their own listed patients, and only 7.9% (median = 5.9%; 25th and 75th percentile: 2.4%, 11.6%) of their visits were provided to patients of their interconnected partners.
Figure 2.
Number of physicians in the group practices
The number of interconnected physicians rose with the size of the practice, but levelled to a mean of 2.5 interconnected physicians for practices with 8 to 19 physicians (Fig. 3). Using a lower threshold of 0.5% for interconnected care, the number of interconnected physicians increased to 4.3 interconnected physicians and was seen in a practice sizes as large as15 to19 physicians (hence accounting for about one quarter of the physicians in the practice). For all thresholds, the number of interconnected physicians decreased in large group practices with 20 to 48 physicians.
Figure 3.
Average number of interconnected physicians, by group size of Family Health Network or Family Health Group.
Discussion
This study examined each pair of physicians in 2 of Ontario’s primary care groups (FHNs and FHGs) and counted how many patients the physicians see in common. We found that physicians provided interconnected care with only a few of their colleagues. Using a threshold of 1% of their visits being with one another’s listed patients, physicians interconnected with only 2.2 other physicians. Despite the wide range in the number of physicians in Ontario’s family practice groups, the size of a group had little association with the extent of interconnected care, beyond groups of 6 or 7 physicians.
The main strength of our study was the use of large linked administrative databases to empirically demonstrate how primary care physicians are connected to each other. We are not aware of other data that can routinely measure the extent to which practitioners work together. Administrative databases are collected for other purposes and so can be used with little additional cost. Other approaches that describe how physicians work together rely on specifically designed surveys or data collection. Surveys of physicians are notoriously challenging with respect to achieving a high, representative response rate.4,5,13
Administrative data are continuously collected for entire populations over time and, as a result, can be used to examine interconnected care in specific contexts (e.g., rural medicine, women’s health, new medical graduates, preventive care, chronic disease management). Furthermore, administrative data in Ontario capture a range of services beyond outpatient care by primary care physicians, including laboratory, diagnostic and therapeutic services and inpatient, institutional and emergency department care.
However, an important limitation of administrative data in many jurisdictions is the omission of many types of practitioners from routinely collected data. Existing administrative data in our jurisdiction include mainly physician services (both family physicians and specialists) and, to a very limited degree, services from pharmacists, physiotherapists, chiropractors and dentists. The increasing use of electronic health records (EHR) holds promise for the study of a wider range of practitioners. In our population, EHR data can currently be used within specific organizations (hospitals, primary care groups) to examine most practitioners who contribute care and share common patient information systems. Also, the EHR and administrative data could be combined to examine how interconnected care within specific organizations (with EHR systems that provide a comprehensive range of practitioner data) is related to care within the overall health care system (using administrative data with a limited range of practitioner data).
We envision two main uses of interconnected analyses, both of which provide a methodological approach that can support other studies. The first use supports studies that examine collaborative health care. At the centre of most collaborative relationships is the care provided to individual patients.1,2 Practitioners who provide care to the same patients have the potential for collaboration, whereas practitioners who never provide care to the same patients likely do not have a meaningful collaboration. Accordingly, health care professionals who provide care to many patients in common have a potentially stronger relationship or collaboration than health care professionals who do not share patients. Using patients to link practitioners is referred to as “affiliate analysis” in both social network theory and collaborative care studies.14 Once an affiliation is described it can be used to further examine social structure, relationships and interactions, depending on the strength, direction or other characteristics of the affiliation. Influential policies have encouraged physicians to work together in Ontario. Interconnected care analysis could be used as one approach to help monitor these and other policies.
The second use supports the examination of health care delivery from a network perspective. We performed a very simple network analysis by examining networks of 2 physicians within defined groups. Typical network studies examine the patterns and importance of connections within complex systems, which would simultaneously examine connections within entire health care systems, both within and beyond defined group boundaries. Also, network analysis focuses on how the network structure affects individuals and their relationships, rather than treating individual physicians or patients as discrete unrelated units.
There are also many different ways to examine interconnected care that do not rely on complex network analyses that typify network medicine. We defined a physician as having interconnected care with another physician if 1% of his or her visits were with another physician’s listed patients. Our definition of interconnected care was arbitrary, but increasing or decreasing the threshold of affiliation did not have a large effect on the number of interconnected family physicians. Examples of aspects of interconnected care we did not consider include the “direction” of collaboration (What if Practitioner A sees Practitioner B’s patients, but Practitioner B does not see Practitioners A’s patients?); services provided by networks of practitioners (What if 3 practitioners share patients in common, or Practitioner A and B don’t see each others’ patients but commonly see Practitioner C’s?); absolute measures (such as 50 practitioner–patient visits per year, rather than 1% of visits); care or activities outside the outpatient clinic, such as on-call or hospital care; and interconnected care for specific types of services such as prevention or chronic disease management.
We fully acknowledge that our measure of “interconnected” care is a simplistic way of describing how physicians work together and that many important connections exist between different types of providers. Future studies could compare interconnected care, as measured using routinely collected data, to collaborative care, as measured using more robust methods. Other studies could examine whether interconnected care is associated with improved patient outcomes, which is the primary reason why health professionals have been encouraged to work together. Incorporating interconnected care into quality-of-care studies should be straightforward, because these types of studies are one of the more common uses of routinely collected administrative data.
Conclusions
There is increasing interest in how health care is organized and delivered in groups or networks of practitioners. Routinely collected administrative data can be used for this purpose when they uniquely identify practitioners who provide care and the patients who receive care. We have described a measure of interconnected care that uses these data to measure how practitioners are connected through their provision of care to the same patients, thus applying the concept of “affiliate analysis.” Beyond our study, administrative data can be used in many ways to describe how health providers care for common patients and to evaluate the effect of specific kinds of collaboration on health care services and health outcomes. Network analyses can be performed using the same data to describe how groups of physicians and patients are connected within a larger, complex system.
Biographies
Douglas G. Manuel, MD, MSc, FRCPC, is a Senior Scientist in the Clinical Epidemiology Program at the Ottawa Hospital Research Institute, Associate Professor in the Department of Family Medicine and the Department of Epidemiology and Community Medicine, University of Ottawa, and Adjunct Scientist at the Institute for Clinical Evaluative Sciences (ICES)–uOttawa.
Kelvin Lam, MSc, is an Analyst with the Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada.
Sarah Maaten, MSc, is an Epidemiologist with the Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada.
Julie Klein-Geltink is an Epidemiologist with the Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada.
Footnotes
Competing interests: None declared.
Funding source: This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. DGM holds a Chair in Applied Public Health from the Canadian Institute for Health Research and the Public Health Agency of Canada.
Doug Manuel helped conceive the project and devise the study methodology, oversaw the data collection and the analyses, and was the principal writer of the manuscript. He serves as the study guarantor. Kelvin Lam helped conceive the project and devise the study methodology, performed the data collection and the analyses, and participated in manuscript writing. Sarah Maaten and Julie Klein-Geltink helped conceive the project and devise the study methodology and participated in manuscript writing. All authors approved the final submitted version of the manuscript.
References
- 1.Lorenz A D, Mauksch L B, Gawinski B A. Models of collaboration. Prim Care. 1999;26(2):401–410. doi: 10.1016/S0095-4543(08)70013-7. [DOI] [PubMed] [Google Scholar]
- 2.Schmitt M H, Farrell M P, Heinemann G D. Conceptual and methodological problems in studying the effects of interdisciplinary geriatric teams. Gerontologist. 1988;28(6):753–764. doi: 10.1093/geront/28.6.753. http://gerontologist.oxfordjournals.org/cgi/doi/10.1093/geront/28.6.753. [DOI] [PubMed] [Google Scholar]
- 3.Smith Susan M, Allwright Shane, O'Dowd Tom. Does sharing care across the primary-specialty interface improve outcomes in chronic disease? A systematic review. Am J Manag Care. 2008;14(4):213–224. [PubMed] [Google Scholar]
- 4.Hoff Timothy, Jameson Lottie, Hannan Edward, Flink Ellen. A review of the literature examining linkages between organizational factors, medical errors, and patient safety. Med Care Res Rev. 2004;61(1):3–37. doi: 10.1177/1077558703257171. http://www.scholaruniverse.com/ncbi-linkout?id=15035855. [DOI] [PubMed] [Google Scholar]
- 5.Lemieux-Charles Louise, McGuire Wendy L. What do we know about health care team effectiveness? A review of the literature. Med Care Res Rev. 2006;63(3):263–300. doi: 10.1177/1077558706287003. http://www.scholaruniverse.com/ncbi-linkout?id=16651394. [DOI] [PubMed] [Google Scholar]
- 6.Salisbury C, Sampson F, Ridd M, Montgomery A A. How should continuity of care in primary health care be assessed? Br J Gen Pract. 2009;59(561):134–141. doi: 10.3399/bjgp09X420257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zwarenstein Merrick, Reeves Scott, Perrier Laure. Effectiveness of pre-licensure interprofessional education and post-licensure collaborative interventions. J Interprof Care. 2005;19(Suppl 1):148–165. doi: 10.1080/13561820500082800. [DOI] [PubMed] [Google Scholar]
- 8.Zwarenstein Merrick, Goldman Joanne, Reeves Scott. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD000072. doi: 10.1002/14651858.CD000072.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Barabási A L. Network medicine—from obesity to the “diseasome”. N Engl J Med. 2007;357(4):404–407. doi: 10.1056/NEJMe078114. [DOI] [PubMed] [Google Scholar]
- 10.Sarma Sisira, Devlin Rose A, Hogg William. Physician's production of primary care in Ontario, Canada. Health Econ. 2010;19(1):14–30. doi: 10.1002/hec.1447. http://www.scholaruniverse.com/ncbi-linkout?id=19191228. [DOI] [PubMed] [Google Scholar]
- 11.Glazier R H, Klein-Geltink J, Kopp A, Sibley L M. Capitation and enhanced fee-for-service models for primary care reform: a population-based evaluation. CMAJ. 2009;180(11):72–81. doi: 10.1503/cmaj.081316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manuel D G, Maaten S, Thiruchelvam D, Jaakkimainen L, Upshur R. Primary care in the health care system. In: Jaakkimainen L, Upshur R, Klein-Geltink J, Leong A, Maaten S, Schultz S, Wang L, editors. Primary care in Ontario. Toronto: Institute for Clinical Evaluative Sciences; 2006. pp. 1–12. http://www.ices.on.ca/webpage.cfm?site_id=1&org_id=67&morg_id=0&gsec_id=0&item_id=3655&type=atlas. [Google Scholar]
- 13.San Martín-Rodriguez L, Beaulieu M D, D’Amour D, Ferrada-Videla M. The determinants of successful collaboration: a review of theoretical and empirical studies. J Interprof Care. 2005;19(Suppl 1):132–147. doi: 10.1080/13561820500082677. http://informahealthcare.com/doi/abs/10.1080/13561820500082677. [DOI] [PubMed] [Google Scholar]
- 14.Hawe Penelope, Webster Cynthia, Shiell Alan. A glossary of terms for navigating the field of social network analysis. J Epidemiol Community Health. 2004;58(12):971–975. doi: 10.1136/jech.2003.014530. http://www.ncbi.nlm.nih.gov/pmc/articles/pmid/15547054. [DOI] [PMC free article] [PubMed] [Google Scholar]